Abstract
AIM: To study the alterations in p53 gene among Indian gastric cancer patients and to correlate them with the various clinicopathological parameters.
METHODS: A total of 103 gastric cancer patients were included in this study. The p53 alterations were studied by both immunohistochemical method as well as polymerase chain reaction (PCR)-single strand conformation polymorphism (SSCP) analysis. We only studied four (exon 5, 6, 7, and 8) of the 11 p53 exons. The alterations in p53 were also correlated with respect to various clinicopathological parameters.
RESULTS: Among 103 cases, p53 over-expression and alteration were detected in 37 (35.92%) and 19 (18.44%) cases, respectively. Most of the p53 alterations were found at exon 5 (31.54%), followed by exon 6 (26.31%), exon 7 (21.04%) and exon 8 (21.04%). A significant correlation of p53 over-expression was found with p53 alteration (P = 0.000). Concordance between p53 alteration (as detected by SSCP) and over-expression [as detected by immunohistochemistry (IHC)] was found in 75% cases. We found that IHC-positive/SSCP-negative cases accounted for 21% of cases and IHC-negative/SSCP-positive cases accounted for remaining 4% cases.
CONCLUSION: Our results show that p53 gene mutations are significantly correlated with p53 protein over-expression, with 75% concordance in over-expression and alteration in the p53 gene, but 25% disconcordance also cautions against the assumption that p53 over-expression is always associated with a gene mutation. There may be other mechanisms responsible for stabilization and accumulation of p53 protein with no evidence of gene mutation that reflect an accumulation of a non-mutated protein, or a false negative SSCP result.
Keywords: Gastric cancer, p53, Single strand conformation polymorphism, Gene mutation, Immunohistochemistry
INTRODUCTION
Gastric cancer is a common disease worldwide[1] and also one of the leading causes of cancer death (5th in male and 6th in female) in India[2]. Its pattern and incidence vary widely between different parts of the world. Costa Rica and Japan have the first and second highest rate in the world with a death rate of 77.7 and 50.5 per 100000, respectively[1,3]. In the United States, 12100 deaths from gastric cancer were expected during 2003 with a death rate of 6.8 per 100000[4]. The overall age-adjusted incidence (world population) of gastric cancer in Jordan is 5.8 per 100000[5]. The burden of new cancer cases has been estimated in the year 2002 based on the National Cancer Registry Programme in India. The number of new digestive tract cancer cases was estimated to be approximately 145000; out of which stomach cancer comprised 23785 cases in men and 11890 in women[6]. Although aggressive surgical resection has improved the overall outcome of patients with this carcinoma, results of surgical resection for advanced cancer are still poor, and the search for predictors of disease survival and response to therapy is therefore mandatory[7]. The molecular biology of gastric cancer has been widely studied in the developed world, particularly in Japan[8–11]. However, only a few scattered reports from the developing world have been published[12–16], and there are no similar published data reported from India. The molecular events leading to the development of gastric cancer are largely unknown, but there is now enough evidence to suggest that the functional inactivation of p53 gene through allelic loss and point mutation plays an important part[17,18].
Several genetic alterations have been shown to play a significant role in tumorigenesis. By and large, the most frequently observed molecular changes occur in the p53 gene[19]. The p53 gene encodes a protein involved in control of the cell cycle and acts as a negative regulator in the cell’s response to damaged DNA[20]. Functional alteration of p53 protein can occur through several mechanisms: point mutations, deletions, rearrangements in the p53 gene, binding with viral proteins, binding with cellular proteins, and oligomerization[21]. Wild-type p53 protein has a very short half-life, whereas mutated p53 is stable and can accumulate at high concentration in the nuclei of tumor cells. As a consequence, immunohistochemical staining with specific antibodies can be used to detect mutant p53 protein. Detecting the precise alteration occurring at the genetic level is much more laborious and costly. The most widely used molecular approach is single strand conformation polymorphism (SSCP) analysis of DNA fragment amplified by polymerase chain reaction (PCR)[22], with subsequent sequence analysis. The sensitivity of SSCP is influenced by the experimental conditions, and by the length of the amplified fragment under study.
The aim of present study was to determine p53 status in Indian gastric cancer patients, who have undergone gastrectomy, and correlate it with various clinicopathological parameters. This study also correlated immunohistochemical staining of p53 protein with SSCP analysis of the PCR-amplified DNA.
MATERIALS AND METHODS
Tumor specimens
From April 2002 to February 2007, cancerous and normal mucosa samples taken from 128 consecutive patients with suspected gastric cancer were enrolled for the study. Cancerous and normal mucosa samples collected from various hospitals after gastrectomy were aliquoted into two sterile tubes. The aliquots for histological and immunohistochemical studies were stored at 4°C in 10% buffered formalin. On the other hand, aliquots for PCR-SSCP studies were stored at -20°C in 1X PBS until DNA extraction. The tissue specimen for SSCP analysis was taken from the center of the tumor mass. No patients had undergone previous chemotherapy or radiotherapy. All the clinicopathological data were collected prospectively and registered in the database. A detailed histopathological examination was performed to determine the depth of invasion on the gastric wall and the extent of metastases within regional lymph nodes. Among 128 cases, 25 were found to be histopathologically negative for gastric cancer and thus were excluded from the study. The remaining 103 cases were from West Bengal (n = 60), Jammu & Kashmir (n = 30) and New Delhi (n = 13). Patients included males (n = 78) and females (n = 25) with a mean age of 56 years (range 25-71 years). The clinical stage was determined by the tumor, node, metastasis (TNM) system[23] and histological diagnosis was made according to the classification of Lauren[24].
Immunohistochemical staining
For immunohistochemical analysis of p53 protein, 4-μm-thick tissue sections were cut and stained with anti-p53 monoclonal antibody (DO7, Biogenex Laboratories, San Ramon, USA) by streptavidin-biotin immunoperoxidase technique (LSAB) using the standard avidin-biotin-complex (ABC) method, followed by antigen retrieval by microwave technique as previously described[25,26]. Briefly, 4-μm-thick sections were first mounted on glass slides, treated with methanol (with 4% H2O2) for 30 min, and incubated with anti-p53 monoclonal antibody (1:100 dilution; DO1 and DO7, Biogenex Laboratories, San Ramon, USA) overnight at 4°C in a humid chamber. After washing thrice with PBS, slides were incubated with biotinylated anti-mouse IgG antibody (DAKO-LSAB kit, Peroxidase, M/s Dakopatts, Denmark) for 30 min at room temperature and developed using HRP-streptavidin and diaminobenzidine tetra hydrochloride (Sigma, St. Louis, USA). The slides were incubated at room temperature for 5-10 min under microscopic control till the optimum development of brown-colored product. Finally, sections were counterstained with Harris hematoxylin and mounted in DPX. The reaction was considered as positive when a strong coloration of the cell nucleus was evident. Sections with nuclear staining in less than 10% of the tumor cells were regarded as negative. Positive p53 nuclear staining was categorized into three patterns as follows: (+), only a few scattered positively stained cells (10%-25% of all tumor cells); (++), localized aggregation of positively stained cells (26%-70% of all tumor cells); and (+++), diffuse aggregation of positively stained cells (more than 70% of all tumor cells). Over-expression of the p53 protein was defined when a (++) or (+++) staining pattern was observed. Negative control sections were processed immunohistochemically without incubating with the primary antibody and positive control sections were from a breast cancer tissue known to express high level of p53.
Genomic DNA isolation and PCR amplification of the p53 exons
Genomic DNA was isolated from tissues of gastric cancer patients by a modified proteinase K digestion and phenol/chloroform extraction technique. All four exons (5, 6, 7 and 8) were amplified separately and details of the primers and PCR cycling parameters used are mentioned in Table 1. The standard PCR reaction contained 0.5 μg genomic DNA, 200 μmol/L dNTPs, 1X PCR buffer, 1.5 mmol/L MgCl2, 1 U of Taq DNA polymerase and 0.3 μmol/L of each primer. Each PCR reaction contained negative controls, where only water was added in place of genomic DNA. The PCR products were electrophoresed on a 20 g/L agarose gel to check the amplification. Samples with positive amplifications were processed for SSCP analysis.
Table 1.
Detail of the primers and cycling parameters
| p53 exons | Sequence (5’-3’) | Cycling parameters1 | PCR product (bp) |
| 5 | Sp5F: TGTTCACTTGTGCCCTGACT | 45 s denaturation at 94°C, 30 s annealing at 54°C, 1 min extension at 72°C | 266 |
| Sp5R: CAGCCCTGTCGTCTCTCCAG | |||
| 6 | Sp6F: GCCTCTGATTCCTCACTGAT | 45 s denaturation at 94°C, 30 s annealing at 53°C, 1 min extension at 72°C | 160 |
| Sp6R: TTAACCCCTCCTCCCAGAGA | |||
| 7 | Sp7F: ACTGGCCTCATCTTGGGCCT | 45 s denaturation at 94°C, 30 s annealing at 56°C, 1 min extension at 72°C | 180 |
| Sp7R: TGTGCAGGGTGGCAAGTGGC | |||
| 8 | Sp8F: TAAATGGGACAGGTAGGACC | 45 s denaturation at 94°C, 30 s annealing at 54°C, 1 min extension at 72°C | 230 |
| Sp8R: TCCACCGCTTCTTGTCCTGC |
Initial denaturation of 10 min at 94°C and final extension of 10 min at 72°C were used in all amplifications. Number of cycles in all amplifications was 35.
SSCP analysis
Non-radioactive SSCP was performed as described previously[27] with slight modification. A 2-μL volume of PCR product was denatured in 5 μL of formamide loading buffer by boiling for 10 min. Denatured samples were loaded onto 120 g/L acrylamide non-denaturation gel and electrophoresed at a constant 100 V for 4-6 h. Images of the ethidium-bromide-stained gels were captured using the BioRad Gel Documentation system. Samples with mobility shifts were verified by a second independent PCR-SSCP where silver staining was done for the same.
Statistical analysis
Descriptive statistics i.e. mean, standard deviation and frequency distribution were calculated for all the variables in the study. According to the different categories for the categorized variables, χ2 test was used to estimate the significance level of the association among them. Student’s t-test, Pearson correlation and analysis of variance were applied for the continuous variables according to the categories, wherever applicable. P < 0.05 was considered statistically significant. SPSS.60 software (SPSS Inc, Chicago, USA) was used for these calculations.
RESULTS
Detection of p53 gene mutation by SSCP analysis
The p53 exons 5, 6, 7 and 8 were successfully amplified from all 103 cases which gave expected PCR fragments of 266 bp, 160 bp, 180 bp, and 230 bp, respectively. After SSCP analysis, altered p53 was identified by the presence of one or two extra bands migrating above or below the normal single-stranded products (Figure 1). Occasionally, mutant bands were also detected between the single and double-strand bands that may have been caused by formation of normal-mutant heterodimers. However, normal p53 banding pattern was also observed among all cases. SSCP data showed that 17.47% (19/103) of the cases were harboring altered p53 (Table 2). Out of these 19 cases, six showed alterations in exon 5, five in exon 6, four in exon 7 and four in exon 8. We further observed that the positivity for p53 mutations was relatively higher in intestinal-type carcinoma (22.44%, 11/49) as compared to diffuse-type (15.66%, 7/45) adenocarcinoma[28] (Table 3).
Figure 1.
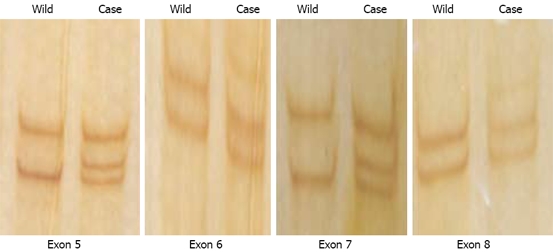
SSCP analysis of exons 5, 6, 7 and 8 of p53 gene. Wild-type and one tumor sample containing mutation are shown for each exon. Only single-strand DNA bands are shown. Heterodimers and double-stranded bands have been omitted.
Table 2.
Relationship between p53 protein over-expression detected by IHC and p53 gene mutation detected by SSCP analysis of 103 gastric carcinomas n (%)
| IHC status | SSCP-negative | SSCP-positive | Total | P |
| IHC-negative | 62 (60) | 4 (4) | 66 (64) | 0.000 |
| IHC over-expression | 22 (21) | 15 (15) | 37 (36) | |
| Total | 84 (81) | 19 (19) | 103 (100) |
Table 3.
Correlation between clinicopathological characteristics and p53 genetic alteration in patients with gastric adenocarcinoma
| Factors |
p53 alteration |
n (%) | P1 | |
| Negative (%) | Positive (%) | |||
| Age | ||||
| < 40 yr | 12 (14.29) | 1 (5.26) | 13 (12.62) | 0.533 |
| 40-65 yr | 55 (65.48) | 15 (78.95) | 70 (67.96) | |
| > 65 yr | 17 (20.23) | 3 (15.79) | 20 (19.42) | |
| Gender | 0.407 | |||
| Male | 62 (73.81) | 16 (84.21) | 78 (75.73) | |
| Female | 22 (26.19) | 3 (15.79) | 25 (24.27) | |
| Cell differentiation | 0.462 | |||
| Well | 9 (10.72) | 2 (10.53) | 11 (10.68) | |
| Moderately | 31 (36.90) | 8 (42.11) | 39 (37.86) | |
| Poorly | 44 (52.38) | 9 (47.37) | 53 (51.46) | |
| Histology | 0.522 | |||
| Intestinal | 35 (41.67) | 10 (52.63) | 45 (43.69) | |
| Diffused | 41 (48.81) | 8 (42.11) | 49 (47.57) | |
| Undiff/mixed | 8 (9.52) | 1 (5.26) | 9 (8.74) | |
| Site | 0.606 | |||
| Cardiac | 19 (22.62) | 2 (10.53) | 21 (20.39) | |
| Fundus | 14 (16.67) | 2 (10.53) | 16 (15.53) | |
| Body | 18 (21.43) | 5 (26.32) | 23 (22.33) | |
| Antrum | 33 (39.29) | 10 (52.63) | 43 (41.75) | |
| Stage | 0.813 | |||
| I | 26 (30.95) | 6 (31.58) | 32 (31.07) | |
| II | 32 (38.10) | 6 (31.58) | 38 (36.89) | |
| III | 21 (25.00) | 6 (31.58) | 27 (26.21) | |
| IV | 5 (5.95) | 1 (5.26) | 6 (5.83) | |
χ2 test with Fisher’s test were used to test the frequency distribution of p53 alteration.
Undiff: Undifferentiated.
Detection of p53 protein over-expression by immunohistochemistry (IHC)
We used DO-7 to detect p53 over-expression by IHC staining. Overall, 35.92% (37/103) of gastric carcinomas exhibited positive nuclear staining (Figure 2). The concordance of results between SSCP and IHC (i.e. both positive and negative) was 75% (Table 2). In addition, 21% of carcinomas (22/103) stained positively by IHC but failed to display any mutation by SSCP, while the remaining 4% (4/103) displayed mutant bands by SSCP but showed no staining by IHC.
Figure 2.
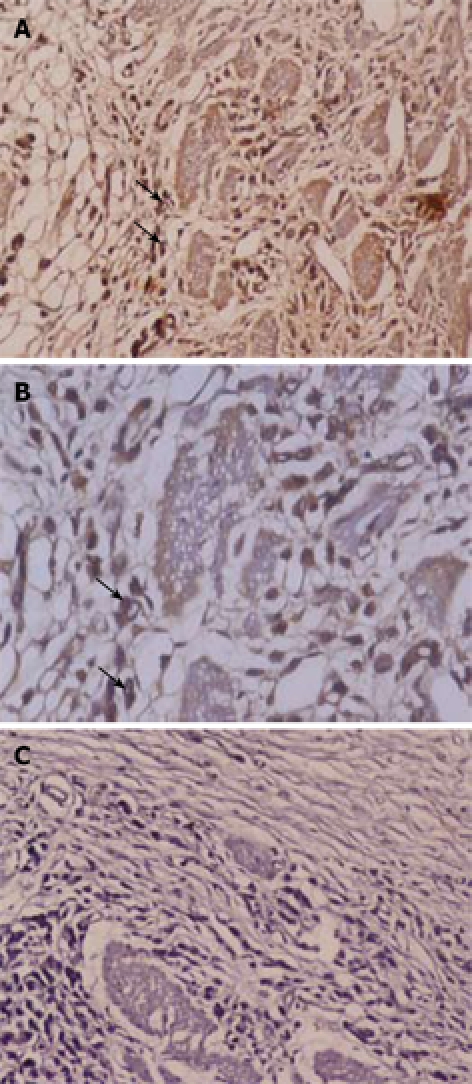
Immunohistochemical staining of p53 protein in diffused type-poorly differentiated gastric cancer. p53 protein over-expression is seen primarily on cell nucleus. A: Positive nuclear staining (× 200); B: Positive nuclear staining (× 400); C: Negative control (× 200).
DISCUSSION
The present study describes the status of p53 gene mutation and over-expression in Indian gastric cancer patients. The association between p53 abnormalities and pathological characteristics of tumor was also assessed. Mutations of the p53 gene are the most common genetic alteration, known to occur in a wide range of human cancers[19]. A number of studies have reported the frequency of p53 alteration in gastric cancer, showing p53 mutation in 18%-58%[18,29,30] and p53 protein over-expression in 26%-65% of gastric adenocarcinoma[31,32]. Under normal conditions, wild-type p53 protein is rapidly degraded but in carcinomas, the acquisition of a mutant genotype is thought to increase the half-life of the mutant protein , which leads to accumulation and detection by immunohistochemical techniques, an indirect method of screening tumors for mutation within the p53 gene. However, a number of discordant results have been reported[33,34]. p53 over-expression can also reflect the accumulation of wild-type protein, which is stabilized via a mechanism other than mutation-for example, by binding with SV40 T antigen, which greatly increases the half-life of the protein[35]. In the present study, we have attempted to address this issue by comparing p53 gene mutation and protein over-expression in a large number of gastric tumors. We analyzed here only exons 5 to 8; because most of the p53 mutations have previously been found to be clustered in the highly conserved domains that roughly correspond to exons 5-8[36]. Although approximately 90% of the p53 point mutations have been reported from exons 5-8, the individual incidence rate of p53 mutations in these exons is not known[37,38]. Although our study is primarily focused on exons 5 to 8, mutations in other exons (13%-22%) could account for some negative SSCP cases[39,40].
Several studies have addressed the relationship between p53 protein accumulation and p53 alteration in different tumor types[41–43]. The concordance rates between IHC staining and SSCP (both negative and positive) fall within a relatively wide range (50% to 80%), but this probably depends on differences both in methodology and tumor type. In the present study, for establishing a relationship between p53 gene mutation and p53 protein accumulation, gastric carcinomas were analyzed for exons 5, 6, 7 and 8 of the p53 gene. We found that p53 protein was over-expressed in 35.92% cases and p53 gene was mutated in 17.47% of cases. A comparison of PCR-SSCP and immunohistochemical findings showed concordant (i.e. both positive and negative) results in 75% of the cases. In particular, 15 (78.94%) of the 19 cases showing a p53 gene mutation were also positive for p53 protein accumulation on IHC, while 22 (26%) of the 84 cases without mutation were positive on IHC. In 26 (25%) cases, the immunohistochemical and SSCP results were discordant; negative IHC/positive SSCP in four and positive IHC/negative SSCP in 22. The presence of p53 gene mutations was significantly correlated with p53 protein over-expression (P = 0.000).
Accumulation of p53 protein with no evidence of gene mutation may either reflect an accumulation of a non-mutated protein, or a false-negative SSCP result. The sensitivity of SSCP analysis is still a matter of debate; not only does it depend on the experimental conditions (i.e. temperature, ionic strength and presence or absence of glycerol), but also on the length of the amplified fragment being analyzed[44]. Sheffield et al[45] reported that SSCP sensitivity dramatically decreased with increasing fragment size; the percentage of single base substitution detected by SSCP was 90% when the amplified fragment was 135 bp, 70% when it was 200 bp, and 67% as fragment size exceeded 300 bp[46]. As the amplified fragment length we analyzed was 266 bp for exon 5, 160 bp for exon 6, 180 bp for exon 7 and 230 bp for exon 8, SSCP sensitivity for exon 5 and 8 might have been less than 70%. Although our study focused on exons 5 to 8, where the majority of the mutations are thought to be localized[38], mutations in other exons (13%-22%) could account for some negative SSCP cases[39,40]. A false-negative SSCP result may also occur when the tissue is not sufficiently represented in tissue from which the DNA is extracted. The search for p53 gene mutation by molecular assays is important for defining the functional alterations that are derived from the different mutations. In this regard, it might be advisable to study all of the exons of the p53 gene. We can justify the inconsistent cases of SSCP and IHC by some possible explanations: first, there may be mutations in exons other than those we examined; second, binding of wild-type p53 protein to a cellular oncogene might have led to an elongated half-life; and third, the proportion of alleles containing p53 mutations may be relatively low, and not shown up in the analysis[47].
It was reported that wild-type p53 proteins could combine with viral oncoproteins or cellular oncoproteins to enhance their stability and prolong their half-life, leading to p53 protein accumulation in cells. In such cells, IHC staining was still positive even without p53 gene mutations; furthermore, about 10% of p53 gene mutations could take place outside of exons 5-8. Therefore, the positive rate of PCR-SSCP targeting only exons 5-8 was usually lower than that of IHC[20,47–49].
In conclusion, PCR-SSCP is a simple and rapid method for the evaluation of p53 gene mutations and its association with immunohistochemical analysis of the p53 protein expression might provide a more precise use of p53 as a prognostic marker in gastric cancer.
COMMENTS
Background
Gastric cancer is a common disease worldwide, including India. The molecular events leading to the development of gastric cancer are largely unknown, but various lines of evidence suggests that the functional inactivation of the p53 gene plays an important role. The p53 protein is involved in control of the cell cycle. Wild-type p53 protein has a very short half-life, whereas mutated p53 is stable and can accumulate at high concentration in the nuclei of tumor cells, and is detected by immunohistochemical staining with specific antibodies. Polymerase chain reaction (PCR)-single strand conformation polymorphism (SSCP) analysis was done to screen and detect the presence of any point mutation in p53 gene.
Research frontiers
In general, the present study is a part of cancer research that is aimed at mutational analysis of the p53 gene among gastric cancer patients. To the best of our knowledge, this is the first study where an attempt has been made to correlate the p53 gene mutation with various clinicopathological features among Indian gastric cancer patients.
Innovations and breakthroughs
Authors have analyzed the status of p53 protein expression by immunohistochemistry (IHC) and p53 gene mutation by PCR-SSCP among gastric cancer cases. This study also provides a significant correlation between immunohistochemical staining of p53 protein and SSCP analysis of the PCR amplified DNA.
Applications
PCR-SSCP in association with IHC of the p53 protein may provide a more precise use of p53 as a prognostic marker for gastric cancer.
Terminology
SSCP is a technique used to screen and detect the mutational change at the single nucleotide level. Additional bands of DNA is an indication of gene alteratio. IHC is a technique used to detect the mutated p53 protein in the nucleus of cancer cells. Mutation in the p53 gene leads to increased half-life and accumulation of p53 protein in the nucleus.
Peer review
The paper describes p53 alterations among gastric cancer patients in India. The alterations were studied by IHC and PCR-SSCP analyses. A significant correlation of p53 over-expression and alteration in p53 gene detected by SSCP was found. It is an interesting study and this is also the first such study from an Indian population, including a large sample from a long research period.
Acknowledgments
The authors would like to thank Dr. P Sahni (Department of Gastroenterology Surgery, AIIMS, New Delhi), Dr. A Roy (Roy & Trivedi Diagnostics, Kolkata) and Dr. SA Zargar (Govt. Medical College, Srinagar) for providing surgical specimens. We thank Dr. S Saxena (Director, Institute of Pathology, ICMR, New Delhi) for providing clinicopathological facilities. We also acknowledge Dr. Shahina Begum, Dr. Md Tauqeer Alam, Chandra Prakash, Gulrooh Barha, and Zeenat Mirza for fruitful discussion while writing the manuscript.
Peer reviewer: Minna Nyström, PhD, Department of Biological and Environmental Sciences, PO Box 56 (Viikinkaari 5 D), University of Helsinki, Helsinki FI-00014, Finland
S- Editor Li DL L- Editor Kumar M E- Editor Lin YP
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Rao DN, Ganesh B, Dinshaw KA, Mohandas KM. A case-control study of stomach cancer in Mumbai, India. Int J Cancer. 2002;99:727–731. doi: 10.1002/ijc.10339. [DOI] [PubMed] [Google Scholar]
- 3.Sasagawa T, Solano H, Mena F. Gastric cancer in Costa Rica. Gastrointest Endosc. 1999;50:594–595; discussion 595-596. [PubMed] [Google Scholar]
- 4.Jemal A, Murray T, Samuels A, Ghafoor A, Ward E, Thun MJ. Cancer statistics, 2003. CA Cancer J Clin. 2003;53:5–26. doi: 10.3322/canjclin.53.1.5. [DOI] [PubMed] [Google Scholar]
- 5.Bani-Hani KE, Yaghan RJ, Heis HA, Shatnawi NJ, Matalka II, Bani-Hani AM, Gharaibeh KA. Gastric malignancies in Northern Jordan with special emphasis on descriptive epidemiology. World J Gastroenterol. 2004;10:2174–2178. doi: 10.3748/wjg.v10.i15.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mohandas KM, Jagannath P. Epidemiology of digestive tract cancers in India. VI. Projected burden in the new millennium and the need for primary prevention. Indian J Gastroenterol. 2000;19:74–78. [PubMed] [Google Scholar]
- 7.Lee WJ, Lee WC, Houng SJ, Shun CT, Houng RL, Lee PH, Chang KJ, Wei TC, Chen KM. Survival after resection of gastric cancer and prognostic relevance of systematic lymph node dissection: twenty years experience in Taiwan. World J Surg. 1995;19:707–713. doi: 10.1007/BF00295910. [DOI] [PubMed] [Google Scholar]
- 8.Tahara E, Semba S, Tahara H. Molecular biological observations in gastric cancer. Semin Oncol. 1996;23:307–315. [PubMed] [Google Scholar]
- 9.Wu M, Semba S, Li D, Yokozaki H. Molecular pathological analysis of mucinous adenocarcinomas of the stomach. Pathobiology. 2004;71:201–210. doi: 10.1159/000078674. [DOI] [PubMed] [Google Scholar]
- 10.Yasui W, Yokozaki H, Fujimoto J, Naka K, Kuniyasu H, Tahara E. Genetic and epigenetic alterations in multistep carcinogenesis of the stomach. J Gastroenterol. 2000;35 Suppl 12:111–115. [PubMed] [Google Scholar]
- 11.Werner M, Becker KF, Keller G, Hofler H. Gastric adenocarcinoma: pathomorphology and molecular pathology. J Cancer Res Clin Oncol. 2001;127:207–216. doi: 10.1007/s004320000195. [DOI] [PubMed] [Google Scholar]
- 12.Johnson O, Ersumo T, Ali A. Gastric carcinoma at Tikur Anbessa Hospital, Addis Ababa. East Afr Med J. 2000;77:27–30. [PubMed] [Google Scholar]
- 13.Hamdi J, Morad NA. Gastric cancer in southern Saudi Arabia. Ann Saudi Med. 1994;14:195–197. doi: 10.5144/0256-4947.1994.195. [DOI] [PubMed] [Google Scholar]
- 14.Al-Mofleh IA. Gastric cancer in upper gastrointestinal endoscopy population: Prevalence and clinicopathological characteristics. Ann Saudi Med. 1992;12:548–551. doi: 10.5144/0256-4947.1992.548. [DOI] [PubMed] [Google Scholar]
- 15.Mohar A, Suchil-Bernal L, Hernandez-Guerrero A, Podolsky-Rapoport I, Herrera-Goepfert R, Mora-Tiscareno A, Aiello-Crocifoglio V. Intestinal type: diffuse type ratio of gastric carcinoma in a Mexican population. J Exp Clin Cancer Res. 1997;16:189–194. [PubMed] [Google Scholar]
- 16.Wu CW, Tsay SH, Hsieh MC, Lo SS, Lui WY, P'eng FK. Clinicopathological significance of intestinal and diffuse types of gastric carcinoma in Taiwan Chinese. J Gastroenterol Hepatol. 1996;11:1083–1088. doi: 10.1111/j.1440-1746.1996.tb00041.x. [DOI] [PubMed] [Google Scholar]
- 17.Tamura G, Kihana T, Nomura K, Terada M, Sugimura T, Hirohashi S. Detection of frequent p53 gene mutations in primary gastric cancer by cell sorting and polymerase chain reaction single-strand conformation polymorphism analysis. Cancer Res. 1991;51:3056–3058. [PubMed] [Google Scholar]
- 18.Renault B, van den Broek M, Fodde R, Wijnen J, Pellegata NS, Amadori D, Khan PM, Ranzani GN. Base transitions are the most frequent genetic changes at P53 in gastric cancer. Cancer Res. 1993;53:2614–2617. [PubMed] [Google Scholar]
- 19.Hollstein M, Sidransky D, Vogelstein B, Harris CC. p53 mutations in human cancers. Science. 1991;253:49–53. doi: 10.1126/science.1905840. [DOI] [PubMed] [Google Scholar]
- 20.Kastan MB, Onyekwere O, Sidransky D, Vogelstein B, Craig RW. Participation of p53 protein in the cellular response to DNA damage. Cancer Res. 1991;51:6304–6311. [PubMed] [Google Scholar]
- 21.Prokocimer M, Rotter V. Structure and function of p53 in normal cells and their aberrations in cancer cells: projection on the hematologic cell lineages. Blood. 1994;84:2391–411. [PubMed] [Google Scholar]
- 22.Orita M, Suzuki Y, Sekiya T, Hayashi K. Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics. 1989;5:874–879. doi: 10.1016/0888-7543(89)90129-8. [DOI] [PubMed] [Google Scholar]
- 23.Aurello P, D'Angelo F, Rossi S, Bellagamba R, Cicchini C, Nigri G, Ercolani G, De Angelis R, Ramacciato G. Classification of lymph node metastases from gastric cancer: comparison between N-site and N-number systems. Our experience and review of the literature. Am Surg. 2007;73:359–366. [PubMed] [Google Scholar]
- 24.Lauren P. The two histological main types of gastric carcinoma, diffuse and so-called intestinal-types carcinoma. An attempt at histochemical classification. Acta Pathol Microbiol Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 25.Campani D, Cecchetti D, Bevilacqua G. Immunocy-tochemical p53 detection by microwave oven heating of routinely formalin-fixed paraffin sections. J Pathol. 1993;171:151–152. doi: 10.1002/path.1711710213. [DOI] [PubMed] [Google Scholar]
- 26.Baas IO, Mulder JW, Offerhaus GJ, Vogelstein B, Hamilton SR. An evaluation of six antibodies for immunohistochemistry of mutant p53 gene product in archival colorectal neoplasms. J Pathol. 1994;172:5–12. doi: 10.1002/path.1711720104. [DOI] [PubMed] [Google Scholar]
- 27.Braggio E, Bonvicino CR, Vargas FR, Ferman S, Eisenberg AL, Seuanez HN. Identification of three novel RB1 mutations in Brazilian patients with retinoblastoma by "exon by exon" PCR mediated SSCP analysis. J Clin Pathol. 2004;57:585–590. doi: 10.1136/jcp.2003.014423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tahara E. Molecular mechanism of stomach carcinogenesis. J Cancer Res Clin Oncol. 1993;119:265–272. doi: 10.1007/BF01212724. [DOI] [PubMed] [Google Scholar]
- 29.Seruca R, David L, Castedo S, Veiga I, Borresen AL, Sobrinho-Simoes M. p53 alterations in gastric carcinoma: a study of 56 primary tumors and 204 nodal metastases. Cancer Genet Cytogenet. 1994;75:45–50. doi: 10.1016/0165-4608(94)90214-3. [DOI] [PubMed] [Google Scholar]
- 30.Poremba C, Yandell DW, Huang Q, Little JB, Mellin W, Schmid KW, Bocker W, Dockhorn-Dworniczak B. Frequency and spectrum of p53 mutations in gastric cancer--a molecular genetic and immunohistochemical study. Virchows Arch. 1995;426:447–455. doi: 10.1007/BF00193167. [DOI] [PubMed] [Google Scholar]
- 31.Monig SP, Eidt S, Zirbes TK, Stippel D, Baldus SE, Pichlmaier H. p53 expression in gastric cancer: clinicopathological correlation and prognostic significance. Dig Dis Sci. 1997;42:2463–2467. doi: 10.1023/a:1018844008068. [DOI] [PubMed] [Google Scholar]
- 32.Gomyo Y, Ikeda M, Osaki M, Tatebe S, Tsujitani S, Ikeguchi M, Kaibara N, Ito H. Expression of p21 (waf1/cip1/sdi1), but not p53 protein, is a factor in the survival of patients with advanced gastric carcinoma. Cancer. 1997;79:2067–2072. doi: 10.1002/(sici)1097-0142(19970601)79:11<2067::aid-cncr3>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 33.Wynford-Thomas D. P53 in tumour pathology: can we trust immunocytochemistry? J Pathol. 1992;166:329–330. doi: 10.1002/path.1711660402. [DOI] [PubMed] [Google Scholar]
- 34.Kohler MF, Nishii H, Humphrey PA, Saski H, Marks J, Bast RC, Clarke-Pearson DL, Boyd J, Berchuck A. Mutation of the p53 tumor-suppressor gene is not a feature of endometrial hyperplasias. Am J Obstet Gynecol. 1993;169:690–694. doi: 10.1016/0002-9378(93)90644-x. [DOI] [PubMed] [Google Scholar]
- 35.Sarnow P, Ho YS, Williams J, Levine AJ. Adenovirus E1b-58kd tumor antigen and SV40 large tumor antigen are physically associated with the same 54 kd cellular protein in transformed cells. Cell. 1982;28:387–394. doi: 10.1016/0092-8674(82)90356-7. [DOI] [PubMed] [Google Scholar]
- 36.Nigro JM, Baker SJ, Preisinger AC, Jessup JM, Hostetter R, Cleary K, Bigner SH, Davidson N, Baylin S, Devilee P. Mutations in the p53 gene occur in diverse human tumour types. Nature. 1989;342:705–708. doi: 10.1038/342705a0. [DOI] [PubMed] [Google Scholar]
- 37.Soussi T. The p53 tumor suppressor gene: from molecular biology to clinical investigation. Ann N Y Acad Sci. 2000;910:121–137; discussion 137-139. doi: 10.1111/j.1749-6632.2000.tb06705.x. [DOI] [PubMed] [Google Scholar]
- 38.Caron de Fromentel C, Soussi T. TP53 tumor suppressor gene: a model for investigating human mutagenesis. Genes Chromosomes Cancer. 1992;4:1–15. doi: 10.1002/gcc.2870040102. [DOI] [PubMed] [Google Scholar]
- 39.Greenblatt MS, Bennett WP, Hollstein M, Harris CC. Mutations in the p53 tumor suppressor gene: clues to cancer etiology and molecular pathogenesis. Cancer Res. 1994;54:4855–4878. [PubMed] [Google Scholar]
- 40.Hartmann A, Blaszyk H, McGovern RM, Schroeder JJ, Cunningham J, De Vries EM, Kovach JS, Sommer SS. p53 gene mutations inside and outside of exons 5-8: the patterns differ in breast and other cancers. Oncogene. 1995;10:681–688. [PubMed] [Google Scholar]
- 41.Dix B, Robbins P, Carrello S, House A, Iacopetta B. Comparison of p53 gene mutation and protein overexpression in colorectal carcinomas. Br J Cancer. 1994;70:585–590. doi: 10.1038/bjc.1994.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang LD, Zhou Q, Hong JY, Qiu SL, Yang CS. p53 protein accumulation and gene mutations in multifocal esophageal precancerous lesions from symptom free subjects in a high incidence area for esophageal carcinoma in Henan, China. Cancer. 1996;77:1244–1249. [PubMed] [Google Scholar]
- 43.Hong SI, Hong WS, Jang JJ, Lee DS, Cho NS, Jung ME, Kim HB, Ha GW, Park IC, Cho DS. Alterations of p53 gene in primary gastric cancer tissues. Anticancer Res. 1994;14:1251–1255. [PubMed] [Google Scholar]
- 44.Hayashi K, Yandell DW. How sensitive is PCR-SSCP? Hum Mutat. 1993;2:338–346. doi: 10.1002/humu.1380020503. [DOI] [PubMed] [Google Scholar]
- 45.Sheffield VC, Beck JS, Kwitek AE, Sandstrom DW, Stone EM. The sensitivity of single-strand conformation polymorphism analysis for the detection of single base substitutions. Genomics. 1993;16:325–332. doi: 10.1006/geno.1993.1193. [DOI] [PubMed] [Google Scholar]
- 46.Hayashi K. PCR-SSCP: a simple and sensitive method for detection of mutations in the genomic DNA. PCR Methods Appl. 1991;1:34–38. doi: 10.1101/gr.1.1.34. [DOI] [PubMed] [Google Scholar]
- 47.Hall PA, Lane DP. p53 in tumour pathology: can we trust immunohistochemistry?--Revisited! J Pathol. 1994;172:1–4. doi: 10.1002/path.1711720103. [DOI] [PubMed] [Google Scholar]
- 48.Fearon ER, Hamilton SR, Vogelstein B. Clonal analysis of human colorectal tumors. Science. 1987;238:193–197. doi: 10.1126/science.2889267. [DOI] [PubMed] [Google Scholar]
- 49.Scott N, Quirke P. Molecular biology of colorectal neoplasia. Gut. 1993;34:289–292. doi: 10.1136/gut.34.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]


