Abstract
Introduction:
Although recent research indicates that many Latino smokers are nondaily smokers or daily smokers who smoke at a low level (≤5 cigarettes/day), almost no research has investigated the characteristics of low-level smokers because such individuals are typically excluded from clinical trial research.
Methods:
The present study examined the associations of daily smoking level and demographics, tobacco dependence, withdrawal, and abstinence during a specific quit attempt among 280 Spanish-speaking Latino smokers (54% male) who participated in a clinical trial of a telephone counseling intervention. Daily smokers were classified as low-level (1–5 cigarettes/day; n = 81), light (6–10 cigarettes/day; n = 99), or moderate/heavy smokers (≥11 cigarettes/day; n = 100). Data were collected prior to the quit attempt and at 5 and 12 weeks postquit.
Results:
Results yielded three key findings. First, smoking level was positively associated with the total score and 12 of 13 subscale scores on a comprehensive, multidimensional measure of tobacco dependence. Low-level smokers consistently reported the least dependence, and moderate/heavy smokers reported the most dependence on tobacco. Second, low-level smokers reported the least craving in pre- to postcessation longitudinal analyses. Third, despite significant differences on dependence and craving, low-level smoking was not associated with abstinence. Smoking level was not associated with demographic variables.
Discussion:
This is a preliminary step in understanding factors influencing tobacco dependence and smoking cessation among low-level Spanish-speaking Latino smokers, a subgroup with high prevalence in the Latino population.
Introduction
According to 2005 data from the U.S. Bureau of the Census, Latinos now comprise over 14% of the nation's population and are the largest and fastest growing minority group in the United States (Bernstein, 2006). Although the prevalence of smoking is lower among Latinos than the general population (15.2% vs. 20.8%), the adverse consequences of tobacco use on Latino health are severe (Centers for Disease Control and Prevention [CDC], 2007). For example, three of the four leading causes of death among Latinos are related to smoking (cancer, heart disease, and stroke), and lung cancer is the leading cause of cancer death among Latino men and the second leading cause among Latino women (National Cancer Institute [NCI], 2005). Moreover, Latinos experience tobacco-related disparities associated with access to treatment, tobacco marketing, cultural and language barriers (Bolen, Rhodes, Powell-Griner, Bland, & Holtzman, 1997), and receipt of physician advice to quit smoking (CDC, 2000). Thus, research addressing tobacco use and dependence among minority groups such as Latinos has been identified as a major public health priority (Fiore et al., 2000; U.S. Department of Health and Human Services, 2001).
Latino smokers may be relatively unique among racial/ethnic groups with respect to nondaily, low-level daily (i.e., 1–5 cigarettes/day), or light daily smoking (i.e., 6–10 cigarettes/day; Fagan, Moolchan, Lawrence, Fernander, & Ponder, 2007; Okuyemi et al., 2002; S. H. Zhu, Pulvers, Zhuang, & Baezconde-Garbanati, 2007). Data from the National Household Survey on Drug Abuse (1991–1993) indicated that 27.4% of Latinos were low-level daily smokers, as compared with 18.4% of Black and 9.3% of White smokers (Kandel & Chen, 2000). Unfortunately, low-level smokers have typically been excluded from randomized clinical trials of smoking cessation interventions, perhaps due to perceptions of increased need for research among those with higher levels of tobacco consumption (S. H. Zhu et al., 2007). However, because low-level smokers are at elevated risk of negative health outcomes when compared with former or never-smokers (NCI, 1998), understanding the associations of low-level smoking with tobacco dependence, withdrawal, and cessation is an important public health aim and could lead to specific treatment approaches targeted at these smokers.
Research suggests that cigarette consumption may be a proxy for physical dependence on tobacco, such that low-level smokers demonstrate less dependence than heavier smokers (Kandel & Chen, 2000). As a result, low-level smokers are more likely to attempt to quit, to experience less withdrawal (Shiffman, Paty, Gnys, Kassel, & Elash, 1995), and to maintain abstinence than are heavier smokers (cf., S. H. Zhu, Sun, Hawkins, Pierce, & Cummins, 2003). Likewise, research supports a comparative lack of withdrawal symptoms in low-level daily smokers attempting to quit (Shiffman et al., 1995), as well as different smoking motives among low-level smokers (e.g., situational factors or a desire for positive reinforcement), as compared with heavier smokers (i.e., withdrawal avoidance; Shiffman & Paty, 2006). However, little is known about how tobacco dependence and withdrawal differ between low-level and light smokers during a specific quit attempt or how these relationships might operate among Latino smokers, who harbor a higher relative proportion of low-level smokers than do other racial/ethnic groups.
The relatively high proportion of Latino low-level smokers also has implications for treatment. The current guidelines for smoking cessation intervention (Fiore et al., 2008) recommend pharmacotherapy and behavioral counseling. However, given that low-level smokers may be less physically dependent on tobacco, pharmacotherapy might be less effective or ineffective. Moreover, little research has focused on the efficacy of behavioral smoking cessation interventions among Latinos, and only a few studies have demonstrated a significant treatment effect (Lawrence, Graber, Mills, Meissner, & Warnecke, 2003; Wetter et al., 2007). Thus, more research on the development of efficacious smoking cessation treatments for Latino smokers is needed, and information about dependence, withdrawal, and other smoking-related constructs can help to inform and direct the focus of those interventions.
Given the uniquely high prevalence of low-level smoking among Latino smokers, the present study examined the associations of daily smoking level with demographics, tobacco dependence, withdrawal, and abstinence during a specific quit attempt among Spanish-speaking Latino smokers.
Methods
Source of data
Data were from Adiós al Fumar, a two-group randomized clinical trial evaluating the efficacy of a culturally sensitive, proactive, behavioral treatment program for Spanish-speaking Latino smokers (Wetter et al., 2007). Self-identified Latino adult smokers residing in Texas who called the National Cancer Institute's Cancer Information Service (CIS South Central office) to request Spanish-language smoking cessation assistance were eligible for enrollment in this study. Participants were recruited from several locations in Texas (e.g., Houston, San Antonio, El Paso, and the Rio Grande Valley) via paid media (television, radio, newspaper, and direct mailings).
Participants were enrolled from August 2002 to March 2004. There were 355 eligible callers during the study period. Of the 355 callers, 297 consented to participate (84%). Of the 58 callers who did not participate, 28 declined, 3 were ineligible, 19 were unreachable, and 8 provided incomplete data. Of the 297 participants enrolled in the original clinical trial, daily smoking level was undeterminable for 17 individuals and they were excluded from the current study, yielding a final sample size of 280 participants.
Callers agreeing to participate in the study were contacted by project staff within 1 week of their initial call to the CIS to complete a verbal, audiotaped informed consent, and a baseline assessment. Follow-up assessment calls were conducted 5 and 12 weeks after the baseline assessment. Participants were randomly assigned to receive one of two telephone-based counseling protocols as part of the clinical trial (standard vs. enhanced). Standard counseling consisted of the single CIS counseling session that had been delivered during the initial call to the CIS, plus an offer of Spanish-language self-help materials that would be mailed to the participant if preferred. The content of counseling, session length, and treatment duration were based on evidence presented in the U.S. Public Health Service's Treating Tobacco Use and Dependence Clinical Practice Guideline (Fiore et al., 2000). Enhanced counseling consisted of the original CIS call and three additional calls scheduled through postquit week 4, which incorporated motivational enhancement techniques (Miller & Rollnick, 2002) into the guideline-based approach (Fiore et al., 2000). Assessment and counseling calls were conducted in Spanish. Detailed information about the treatment protocol and outcome is available elsewhere (Wetter et al., 2007).
Measures and variables of interest
Smoking level.
Smoking level was assessed at baseline and defined by self-reported cigarettes smoked per day. Smoking level classification was informed by S. H. Zhu et al. (2007): low-level (1–5 cigarettes/day), light (6–10 cigarettes/day), and moderate/heavy smokers (≥11 cigarettes/day). The separation of low-level and light smokers allowed for a detailed examination of potential differences in withdrawal, dependence, and abstinence among this particularly understudied end of the smoking-level spectrum.
Demographic variables.
Demographic measures collected at baseline included age, gender, educational achievement, marital status, annual household income, ethnicity, time in the United States, and language spoken at home. Several variables were dichotomized: marital status (married vs. not married), household income (≤US$20,000 vs. >$20,000), ethnicity (Mexican vs. other), time in the United States (≤10 years or >10 years), and language spoken at home (only Spanish vs. not only Spanish).
Tobacco dependence.
Tobacco dependence was measured at baseline with the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68; Piper et al., 2004) and with single-item dependence variables (i.e., number of years smoked and dichotomized time to first cigarette of the day [≤5 min or >5 min after waking]). The WISDM-68 is a comprehensive, multidimensional measure of dependence that yields an overall smoking dependence score as well as subscale scores for critical dimensions of dependence, including nonphysical indices of dependence (e.g., affiliative attachment, automaticity, and social/environmental goads; Piper et al., 2004).
Tobacco withdrawal.
Tobacco withdrawal was measured at baseline and the 5- and 12-week postquit assessments with the Wisconsin Smoking Withdrawal Scale (WSWS). The WSWS includes subscales for anger, anxiety, sadness, concentration difficulty, craving, hunger, and sleep (Welsch et al., 1999).
Smoking abstinence.
Abstinence was defined as a self-report of no smoking during the previous 7 days at the 5- and 12-week assessments. Biochemical verification of abstinence was not performed due to the telephonic nature of the clinical trial.
Data analyses
Initial analyses investigated the associations of smoking level with demographic variables and single-item tobacco dependence variables. Chi-square tests were used for analyses involving categorical variables, and analyses of variance were used for continuous variables. Multivariate regression analyses were used to investigate the association of smoking level with tobacco dependence as measured with the WISDM-68. Both unadjusted and adjusted analyses were performed. Demographic covariates in the adjusted model included age, gender, educational achievement, marital status, annual household income, ethnicity, time in the United States, and language spoken at home.
Generalized linear mixed model (GLMM) regressions (McCulloch & Searle, 2001) were conducted to assess the longitudinal association of smoking level with withdrawal (WSWS) from 5 to 12 weeks postquit, controlling for treatment group, demographic variables, abstinence, and baseline withdrawal.
Finally, the associations between smoking level and abstinence were assessed at static postquit timepoints using logistic regressions and controlling for treatment group, age, gender, educational achievement, marital status, annual household income, ethnicity, time in the United States, and language spoken at home. Results were examined using both completer-only (missing data from dropouts were maintained) and intent-to-treat (dropouts categorized as smokers) analyses. The completer-only analysis included 84% of the low-level, 83% of the light, and 83% of the moderate/heavy smokers included in the intent-to-treat analyses. The association between smoking level and abstinence over time was assessed using GLMM regressions.
Results
Participant characteristics
Participants (n = 280) were generally of low socioeconomic status. More than 50% reported less than $20,000 in total household income per year, and approximately 50% reported less than a high school education. Almost two-thirds of participants reported that Spanish was the only language spoken at home, and slightly less than half resided in the United States for 10 years or less. We found no significant relationships between smoking level and demographic variables (Table 1).
Table 1.
Participant characteristics at baseline
| Low-level smokers: 1–5 cigarettes/day (n = 81) | Light smokers: 6–10 cigarettes/day (n = 99) | Moderate/heavy smokers: ≥11 cigarettes/day (n = 100) | p value | |
| Demographic variable | ||||
| Age, years (SD) | 40.7 (13.0) | 40.9 (9.8) | 43.1 (11.3) | .265 |
| Gender (percent male) | 53.1 | 50.5 | 59.0 | .469 |
| Education (percent) | ||||
| <High school | 43.2 | 49.5 | 56.0 | |
| ≥High school to some college | 39.5 | 42.4 | 35.0 | |
| ≥College | 17.3 | 8.31 | 9.0 | .185 |
| Marital status (percent married) | 73.8 | 62.6 | 70.0 | .258 |
| Household income (percent <US$20,000) | 58.0 | 59.4 | 46.4 | .143 |
| Ethnicity (percent Mexican origin) | 59.3 | 69.7 | 70.0 | .233 |
| Time in the United States (percent >10 years) | 51.9 | 59.6 | 64.0 | .252 |
| Language spoken at home (percent Spanish only) | 64.2 | 63.6 | 59.0 | .719 |
| Single-item tobacco-dependence variable | ||||
| Average number of cigarettes/day (SD) | 3.4 (1.4) | 8.6 (1.6) | 19.7 (7.8) | <.001 |
| Number of years smoked (SD) | 19.5 (11.0) | 21.7 (9.1) | 24.5 (1.08) | .005 |
| Time to first cigarette (percent ≤5 min) | 6.2 | 12.1 | 28.3 | <.001 |
| Treatment group (percent enhanced) | 46.9 | 53.5 | 50.0 | .674 |
Note. The p values for continuous variables are based on analysis of variance tests for differences between groups based on smoking level; p values for categorical variables are based on chi-square tests for differences between groups based on smoking level.
Tobacco dependence
Low-level, light, and moderate/heavy smokers differed with regard to single-item tobacco-dependence variables (see Table 1). Low-level smokers smoked for fewer years and were more likely to wait longer to smoke the first cigarette of the day. Similarly, smoking level was strongly associated with dependence measured by the WISDM-68 (Table 2). As the pattern of results in unadjusted and adjusted analyses was similar, only adjusted analyses are reported. Results indicated that smoking level was associated with the WISDM-68 total score and 12 of 13 subscale scores (see Table 2). Smoking level was not, however, associated with scores on the social/environmental goads subscale. Low-level and light smokers, respectively, reported significantly less dependence than moderate/heavy smokers on all 12 of the significant subscales and on the total score. Low-level smokers reported significantly less dependence than light smokers on eight subscales, as well as the WISDM-68 total score.
Table 2.
Wisconsin Inventory of Smoking Dependence Motives total and subscale means by smoking level and significant differences between smoking levels in adjusted regression analyses
| Score (SD) by smoking level |
p value |
||||||
| Low-level | Light | Moderate/heavy | Low-level versus light | Low-level versus moderate/heavy | Light versus moderate/heavy | Overall | |
| WISDM-68 subscale | |||||||
| Affiliative attachment | 2.66 (1.70) | 3.80 (1.96) | 4.72 (1.81) | >.0001 | >.0001 | .0003 | >.0001 |
| Automaticity | 3.67 (1.84) | 4.22 (1.85) | 5.57 (1.36) | .01 | >.0001 | >.0001 | >.0001 |
| Behavioral choice/melioration | 2.98 (1.71) | 4.24 (1.78) | 5.22 (1.66) | .0009 | >.0001 | .0004 | >.0001 |
| Cognitive enhancement | 2.79 (1.37) | 3.55 (1.42) | 4.26 (1.59) | ns | >.0001 | >.0001 | >.0001 |
| Craving | 2.63 (1.65) | 2.93 (1.67) | 3.86 (1.82) | >.0001 | >.0001 | .0011 | >.0001 |
| Cue exposure/associative processes | 3.39 (1.61) | 4.85 (1.55) | 5.54 (1.45) | .0016 | >.0001 | .004 | >.0001 |
| Loss of control | 3.87 (1.27) | 4.49 (1.31) | 5.00 (1.31) | >.0001 | >.0001 | >.0001 | >.0001 |
| Negative reinforcement | 4.04 (1.65) | 4.40 (1.61) | 5.15 (1.66) | ns | >.0001 | .0006 | >.0001 |
| Positive reinforcement | 3.50 (1.63) | 4.09 (1.81) | 4.72 (1.78) | ns | >.0001 | .0045 | >.0001 |
| Social/environmental goads | 3.63 (2.04) | 3.88 (1.88) | 4.00 (2.08) | ns | ns | ns | ns |
| Taste/sensory processes | 3.55 (1.49) | 4.18 (1.55) | 4.91 (1.51) | .0135 | >.0001 | .0005 | >.0001 |
| Tolerance | 3.00 (1.64) | 4.30 (1.62) | 5.37 (1.31) | >.0001 | >.0001 | >.0001 | >.0001 |
| Weight control | 2.57 (1.64) | 2.94 (1.67) | 3.42 (1.92) | ns | .0019 | .0520 | .0076 |
| WISDM-68 total | 42.29 (15.67) | 52.08 (15.21) | 61.74 (15.55) | .0001 | >.0001 | >.0001 | >.0001 |
Withdrawal
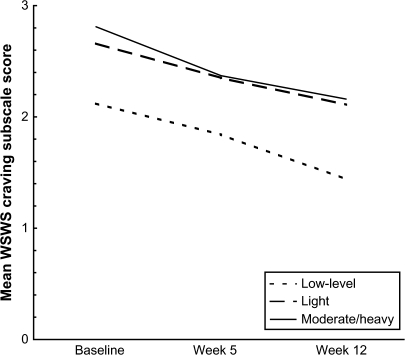
In longitudinal analyses of withdrawal, smoking level was strongly associated with craving, F(2, 221) = 6.19, p = .0024, but not with other withdrawal symptoms. The low-level smoking group reported less craving than other groups at baseline and both postquit timepoints (Figure 1).
Figure 1.
Comparison of unadjusted Wisconsin Smoking Withdrawal Scale craving subscale mean scores by smoking level from baseline through 12 weeks postquit.
Abstinence
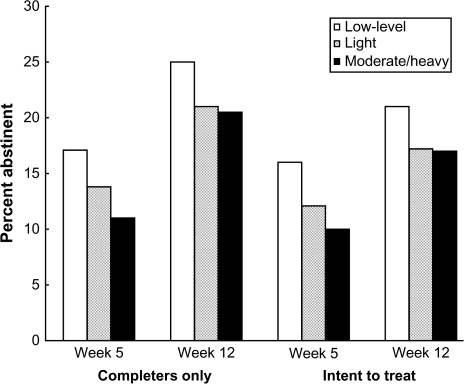
Smoking level was not significantly associated with abstinence in logistic regressions conducted at static timepoints (i.e., 5 and 12 weeks postquit), regardless of method of analysis (i.e., completer-only or intent-to-treat; Figure 2). Similarly, smoking level was not significantly associated with abstinence in longitudinal analyses.
Figure 2.
Abstinence by smoking level at 5 and 12 weeks postquit.
Discussion
The present study was the first to examine the associations of smoking level with demographics, tobacco dependence, withdrawal, and abstinence among Spanish-speaking Latinos during a specific quit attempt. Three key findings emerged regarding low-level smokers, who were of particular interest due to their uniquely high prevalence among Latino smokers. First, smoking level was strongly linked to the total score and 12 of 13 subscale scores on a comprehensive, multidimensional measure of tobacco dependence (i.e., WISDM-68) as well as single-item tobacco-dependence variables. In each case, low-level smokers reported the least dependence and moderate/heavy smokers reported the greatest dependence on tobacco. Second, in withdrawal analyses (i.e., WSWS), smoking level was associated with craving longitudinally from prequit to 12 weeks postquit, but not with other withdrawal symptoms. Low-level smokers reported the least craving and moderate/heavy smokers the most craving at all points in time. Finally, smoking level was not significantly associated with abstinence at static postquit timepoints or longitudinally. Thus, despite less dependence and fewer cravings, low-level smokers were not more likely than heavier smokers to quit smoking.
The lesser levels of tobacco dependence reported by low-level smokers complement previous findings about “chippers” (nondaily and low-level smokers) who manifest less (or no) dependence on nicotine, as compared with heavier smokers (for a review of research, see Shiffman & Paty, 2006). However, the present study extends that research to Latinos. Low-level and light smokers differed significantly in self-reported tobacco dependence; low-level smokers reported less dependence than their light smoking counterparts. This finding highlights the importance of examining low-level and light smokers separately, at least among Spanish-speaking Latino smokers.
Given that smoking level was associated with 12 of the 13 subscales of the WISDM-68, the lack of association with the remaining subscale, social/environmental goads, is of particular interest. Social/environmental goads assess contextual influences on smoking (e.g., social motives for smoking, smoking in the presence of other smokers), and the lack of association suggests that low-level smokers may be as motivated as light and moderate/heavy smokers to smoke in response to environmental cues and social motives. These results complement findings that chippers smoke for social reasons, or to enhance the enjoyment of activities, rather than in response to physiological withdrawal symptoms (Shiffman, Kassel, Paty, Gnys, & Zettler-Segal, 1994; Shiffman & Paty, 2006). Moreover, low-level smokers reported significantly less craving, both at baseline and during the quit attempt, than did light or moderate/heavy smokers, but they did not differ on any other withdrawal symptoms. Thus, results suggest that interventions for low-level Latino smokers need to be weighted more toward building the skills to combat smoking in response to social situations and activities, as well as altering environmental features to facilitate abstinence, rather than tolerating physiological dependence and craving. The potential efficacy of pharmacotherapy among low-level Latino smokers deserves serious study given the reduced tobacco dependence and craving among this segment of smokers.
Smoking level was not associated with abstinence during the quit attempt. This finding is notable because previous research indicates that low-level smokers are more likely than heavier smokers to maintain abstinence when quitting, perhaps due to reduced levels of, or the absence of, dependence on tobacco (cf. S. H. Zhu et al., 2003). Although low-level smokers were less dependent on tobacco and experienced less craving during the quit attempt than did light or moderate/heavy smokers, this did not translate into higher cessation rates. However, as shown in Figure 2, there was a suggestion, albeit nonsignificant, that low-level smokers might be more likely to quit successfully, and the present study may have simply lacked sufficient power to detect the effect of smoking level on abstinence. Future research should prospectively investigate the relationship between smoking level and biochemically confirmed abstinence with larger samples of Spanish-speaking Latino smokers.
The present study has several strengths. First, the focus was on Spanish-speaking Latino smokers, a historically underserved racial/ethnic group that has been grossly understudied (Fagan et al., 2007). Second, the sample allowed a detailed examination of the low end of the smoking-level spectrum because low-level and light smokers were included, unlike the majority of smoking-related randomized clinical trials that include only those who smoke at least 10 cigarettes/day (cf. Okuyemi et al., 2002). Further, the sample allowed us to distinguish between low-level and light smokers in our exploration of dependence, withdrawal, and abstinence, which is particularly relevant among Latino smokers, given the smoking levels demonstrated here and in previous research (Kandel & Chen, 2000; S. H. Zhu et al., 2007). Finally, the present study was unique in its examination of low-level smoking because of its comprehensive assessment of tobacco dependence using the WISDM-68.
A notable limitation of the present study is the lack of biochemical verification of abstinence. However, biochemical verification of the results would likely alter the pattern of results only if there was a systematic bias for misreporting that was dependent on smoking level, which is unlikely. The participants in this study were treatment-seeking, Spanish-speaking Latinos from Texas, two-thirds of whom were of Mexican heritage; therefore, results may not generalize to other Latino population groups. Whether participants modified their smoking level prior to baseline data collection in anticipation of a quit attempt was unknown, and future studies with similar designs should account for this possibility.
To the best of our knowledge, this study was the first to examine tobacco dependence, withdrawal, and abstinence during a specific quit attempt among low-level, Spanish-speaking Latino smokers. Results indicated that low-level smokers were less dependent on tobacco and manifested less craving relative to light and moderate/heavy smoking groups. However, we found no differences between groups in abstinence during the quit attempt. This study represents a preliminary step in understanding the factors influencing tobacco dependence and smoking cessation among low-level Spanish-speaking Latino smokers, a subgroup with high prevalence in the Latino population, and is important in its focus on an understudied and underserved group.
Funding
Minority Health Research and Education Program of the Texas Higher Education Coordinating Board; National Cancer Institute (R01 CA94826, R01 CA89350, R25 CA57730); and Centers for Disease Control and Prevention (K01DP001120, K01DP000086).
Declaration of Interests
None declared.
Supplementary Material
Acknowledgments
The authors thank the National Cancer Institute's Cancer Information Service for their contributions to the original research project, Adiós al Fumar, from which our data were derived.
References
- Bernstein R. Nation's population one-third minority. 2006. Retrieved 8 November 2007, from http://www.census.gov/Press-Release/www/releases/archives/population/006808.html. [Google Scholar]
- Bolen JC, Rhodes L, Powell-Griner EE, Bland SD, Holtzman D. State-specific prevalence of selected health behaviors, by race and ethnicity—Behavioral Risk Factor Surveillance System. MMWR Morbidity and Mortality Weekly Report. 1997;49:1–60. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Receipt of advice to quit smoking in Medicare managed care—United States 1988. MMWR Morbidity and Mortality Weekly Report. 2000;49:797–801. [Google Scholar]
- Centers for Disease Control and Prevention. Cigarette smoking among adults—United States 2006. MMWR Morbidity and Mortality Weekly Report. 2007;56:1157–1161. [PubMed] [Google Scholar]
- Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007;102(Suppl. 2):5–29. doi: 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Treating tobacco use and dependence. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services Public Health Service; 2000. [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008 Update. Clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services Public Health Service; 2008. Retrieved May 2008, from http://www.surgeongeneral.gov/tobacco/default.htm. [Google Scholar]
- Kandel DB, Chen K. Extent of smoking and nicotine dependence in the United States: 1991–1993. Nicotine & Tobacco Research. 2000;2:263–274. doi: 10.1080/14622200050147538. [DOI] [PubMed] [Google Scholar]
- Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in U.S. racial/ethnic minority populations: An assessment of the literature. Preventive Medicine. 2003;36:204–216. doi: 10.1016/s0091-7435(02)00023-3. [DOI] [PubMed] [Google Scholar]
- McCulloch C, Searle S. Generalized, linear, and mixed models. New York: Wiley; 2001. [Google Scholar]
- Miller W, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. 2nd ed. New York: Guilford; 2002. [Google Scholar]
- National Cancer Institute. Cigars: Health effects and trends. 1998. (Smoking and Tobacco Control Monograph No. 9). Retrieved 10 November 2007, from http://cancercontrol.cancer.gov/tcrb/monographs/9/ [Google Scholar]
- National Cancer Institute. United States cancer statistics: 1999–2002 incidence and mortality web-based report version. 2005. Retrieved 8 November 2007, from http://apps.nccd.cdc.gov/uscs/ [Google Scholar]
- Okuyemi KS, Harris KJ, Scheibmeir M, Choi WS, Powell J, Ahluwalia JS. Light smokers: Issues and recommendations. Nicotine & Tobacco Research. 2002;4(Suppl. 2):S103–S112. doi: 10.1080/1462220021000032726. [DOI] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, et al. A multiple motives approach to tobacco dependence: The Wisconsin Inventory of Smoking Dependence Motives (WISDM-68) Journal of Consulting and Clinical Psychology. 2004;72:139–154. doi: 10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Kassel JD, Paty J, Gnys M, Zettler-Segal M. Smoking typology profiles of chippers and regular smokers. Journal of Substance Abuse. 1994;6:21–35. doi: 10.1016/s0899-3289(94)90052-3. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA. Smoking patterns and dependence: Contrasting chippers and heavy smokers. Journal of Abnormal Psychology. 2006;115:509–523. doi: 10.1037/0021-843X.115.3.509. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JD, Elash C. Nicotine withdrawal in chippers and regular smokers: Subjective and cognitive effects. Health Psychology. 1995;14:301–309. doi: 10.1037//0278-6133.14.4.301. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2010. Washington, DC: U.S. Department of Health and Human Services; 2001. [Google Scholar]
- Welsch SK, Smith SS, Wetter DW, Jorenby DE, Fiore MC, Baker TB. Development and validation of the Wisconsin smoking withdrawal scale. Experimental and Clinical Psychopharmacology. 1999;7:354–361. doi: 10.1037//1064-1297.7.4.354. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Mazas C, Daza P, Nguyen L, Fouladi RT, Li Y, et al. Reaching and treating Spanish-speaking smokers through the National Cancer Institute's Cancer Information Service: A randomized controlled trial. Cancer. 2007;109:406–413. doi: 10.1002/cncr.22360. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Pulvers K, Zhuang Y, Baezconde-Garbanati L. Most Latino smokers in California are low-frequency smokers. Addiction. 2007;102(Suppl. 2):104–111. doi: 10.1111/j.1360-0443.2007.01961.x. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Sun J, Hawkins S, Pierce J, Cummins S. A population study of low-rate smokers: Quitting history and instability over time. Health Psychology. 2003;22:245–252. doi: 10.1037/0278-6133.22.3.245. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.