Abstract
Background
Lateral epicondylitis represents a frequent overuse injury. In spite of many conservative treatment procedures, prolonged symptoms and relapse are frequently observed.
Objective
To compare the outcome of patients performing an isokinetic eccentric training with that of age‐, gender‐, activity‐matched patients receiving a non‐strengthening classical rehabilitation.
Methods
Ninety‐two patients with unilateral chronic lateral epicondylar tendinopathy (mean duration of symptoms 8±3 months) were assigned either to a control group (n = 46) or to an eccentrically trained group (n = 46). The control group underwent a passive standardised rehabilitation programme that excluded strengthening exercises. In addition to this programme, the trained group also performed eccentric exercises based on the repetitive lengthening of the active musculo‐tendinous unit. The latter exercises started with submaximal contraction intensity and slow speed movement. Modalities were progressively intensified (increase in intensity contraction and speed movement) over a long priod of treatment. Programme effectiveness was assessed through pain score evaluation, a disability questionnaire, muscle strength measurement and ultrasonographic examination.
Results
Compared to the non‐strengthening control group, the following observations were made in the eccentrically trained group: (1) a significantly more marked reduction of pain intensity, mainly after one month of treatment; (2) an absence of strength deficit on the involved side through bilateral comparison for the forearm supinator and wrist extensor muscles; (3) an improvement of the tendon image as demonstrated by decreasing thickness and a recovered homogenous tendon structure; and (4) a more marked improvement in disability status during occupational, spare time and sports activities.
Conclusion
These results highlight the relevance of implementing isokinetic adapted eccentric training in the management of chronic lateral epicondylar tendinopathy.
Keywords: elbow, chronic tendinopathy, rehabilitation, isokinetic, eccentric
Lateral epicondylitis, which affects about 1–3% of the population,1,2 represents a common but frustrating injury caused by repetitive gestures entailing repetitive microtrauma arising from sports activity, industrial work and hobby activities.3,4,5,6 Eccentric contractions imposed during these particular activities may be a factor that contributes to tennis elbow.7 Almekinders et al evoked the concept of overuse disorder, possibly predisposed by pre‐existing weakening of the tendon.8
Despite a wide range of conservative treatment methods based mainly on rest, ice, brace, nonsteroidal anti‐inflammatory drugs, ultrasound, laser, electrical stimulation, phonophoresis, deep friction massage, stretching, extracorporeal shock‐wave therapy, acupuncture or injections,9,10,11,12,13,14,15,16 prolonged symptoms or relapse upon return to the offending activity are frequently observed.17,18,19 In contrast to the passive pattern of many therapies dedicated to tendon disorders, some authors have promoted an eccentric training model.20,21,22,23 Initially applied to patellar and Achilles tendinosis rehabilitation,24,25,26,27 this concept is currently being extended to include some other injured tendons. Such active eccentric training programmes are aimed at thwarting an aetiopathogenic theory proposing insufficient tensile strength of the tendon exposed to external loads which could progressively damage it.8,21 Though the literature remains incomplete on tendon architecture remodeling and real histological adaptations following an adapted eccentric training, clinical results following such therapy appear promising.23,25,28,29
Resistance‐based exercise programmes are occasionally prescribed in elbow tendinosis.9,27,30,31 A few eccentric exercise models have been proposed in the management of tennis elbow,32,33,34 yet, to our knowledge, an isokinetic eccentric protocol specifically worked out for this condition has never been rigorously investigated. The goal of this study was to analyse, in comparison with a passive intervention, the effectiveness of a newly designed programme based on eccentric isokinetic training for chronic lateral epicondylar tendinopathy. Its effects on pain, strength, ultrasonographic examination and disability during occupational, free time and sports activities were evaluated.
Material and methods
Subjects
Ninety‐two patients (85 right‐handed and 7 left‐handed) suffering from unilateral chronic lateral epicondylar tendinopathy participated in the study. They were characterised by a relatively long mean (±SD) duration of symptoms (8±3 months) which did not respond to earlier conservative non‐strengthening treatments (injections, oral and percutaneous medications, support and physical therapy). Inclusion criteria consisted of pain and tenderness localised to the lateral epicondyle and proximal portion of the extensor muscle mass, increased pain on resisted middle finger extension with the elbow in an extended position and increased pain on elbow extension with full wrist flexion. Clinical examination was complemented with an ultrasonographic examination that systematically confirmed the tendon injury, and patients underwent radiography aimed at verifying the presence of calcification. In order to treat the tendinous disorder exclusively, the following exclusion criteria were applied: pain over the radial and posterior interosseous nerve; pain and tenderness over the radiohumeral joint; exacerbation of pain on movement of the neck or on cervical compression; and sensory disturbance in the affected arm. Cases with bilateral symptoms or with other significant upper limb disorders were also excluded.
Manual work, participation in racquet sports and sex are factors considered as having prognostic significance regarding patient outcomes in lateral epicondylar tendinopathy.35,36 Consequently, instead of performing a randomised allocation of patients into the different treatment groups, we decided to take into consideration age, gender and activity. Therefore, 46 patients were assigned to a non‐eccentric control group (CG) and 46 age‐, gender‐ and activity‐matched patients were assigned to an eccentrically trained group (ECC) (table 1). Prior informed consent was obtained from all patients and the study was approved by the Ethics Committee of the University of Liege.
Table 1 Study populations (means ± SD for age, weight and duration of symptoms).
| Control group (CG, n = 46) | Eccentric group (ECC, n = 46) | |
|---|---|---|
| Men/women | 18/28 | 18/28 |
| Mean age (years) | 38±8 | 40±8 |
| Mean weight (kg) | ||
| Men | 73±8 | 74±8 |
| Women | 59±7 | 57±9 |
| Dominant/non‐dominant affected side | 36/10 | 37/9 |
| Duration of symptoms (months) | 8±3 | 8±4 |
Treatment content
The CG received non‐strengthening rehabilitation including ice, analgesic TENS, ultrasound, deep friction massage and stretching, which are considered as common passive rehabilitation modalities.17
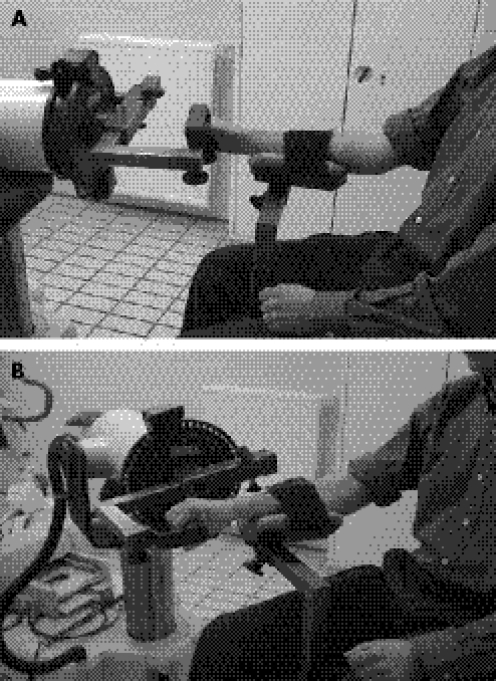
In addition to this programme, the ECC group also performed isokinetic eccentric training administered to the involved side using a Cybex Norm (Henley Healthcare, Sugar Land, TX, USA) dynamometer. During each session, wrist extensors and forearm supinators were successively exercised. For the forearm supinators, patients were seated in front of the dynamometer with the forearm in a neutral position supported on a horizontal plane (fig 1A). The axis of the dynamometer was aligned with the forearm and the elbow was maintained at 60° of flexion. Wrist extensors were trained with subjects seated, the forearm supported on a horizontal plane and the elbow maintained flexed at 60° (fig 1B). The centre of the wrist joint was aligned with the rotational axis of the dynamometer and the forearm placed in a pronation position.37 Exercise modalities of the eccentric training programme are shown in table 2.
Figure 1 Patient installation on the isokinetic tool for training and testing the forearm supinators (A) and the wrist extensors (B). The patient gave consent for the photographs to be published.
Table 2 Modality description of the isokinetic eccentric training model.
| Sessions | Velocity | Intensity |
|---|---|---|
| From 1 to 5 | 30°/s | 30% MAX |
| From 6 to 10 | 60°/s to 90°/s | 30% MAX |
| From 11 to 15 | 30°/s to 90°/s | 60% MAX |
| From 16 to 20 | 30°/s to 60°/s | 80% MAX |
| From 21 to 30 | 60°/s to 90°/s | 80% MAX |
Extensors and supinators were successively exercised in the form of pain‐free contractions (2 sets of 10 repetitions for each muscle group, with the workload increased twofold from the 21st session). Outcome measurement times are described in the evaluation section.
General rules were as follows:
After eccentric contraction, return to the articular start position occurred passively, the motion being carried out by the machine at the same speed as used in the eccentric work;
Whenever possible, training involved a complete range of joint motion. However, pain occasionally precluded the use of exercise until maximal length position of the muscle‐tendon unit was reached. Thus, the range of motion, controlled by electronic and mechanical stops, was individually adapted and led progressively to a full range of motion when painless;
At the beginning, loading was low (30% maximal intensity) as was the speed of isokinetic movement (30°/s). Progressive intensification of exercises by successively increasing velocity and intensity remained subordinate to lack of pain. When pain occurred, previous modalities were temporarily restored. Prior to training, preliminary submaximal repetitions routinely preceded each isokinetic session.
For both groups of patients, treatment was prescribed three times a week, with 26±3 and 25±3 sessions for ECC and CG respectively (corresponding to a mean duration of 9 weeks). Patients were instructed to avoid movements provoking pain or discomfort when participating in occupational, sport or hobby activities in the course of treatment.
Evaluation
Pain score
Subjective sensation of pain at rest was evaluated by the patients under supervision of the same examiner using a visual analogue scale (VAS) graded from 0 (no pain at all) to 10 (most severe pain) units, before rehabilitation, after 4 weeks, after 7 weeks and at the end of the treatment.
Muscle strength
The isokinetic assessments were performed using the Cybex Norm device with a patient installation corresponding to that used during training. Subjects did not receive visual feedback during testing, albeit verbal encouragement was given. No gravity compensation was allowed by the dynamometer. Wrist extensors and forearm supinators were evaluated in the concentric mode at 30°/s (4 repetitions) and 90°/s (4 repetitions); eccentric performances were recorded at 60°/s (4 repetitions). The range of motion consisted of 70° of flexion and 70° of extension or 80° of supination and 80° of pronation. The warm‐up procedure consisted of submaximal isokinetic repetitions at various angular speeds.
Owing to intense persistent pain after preliminary attempts (personal unpublished data), and on the grounds of patient safety, bilateral isokinetic measurements were not conducted prior to initiation of treatment. In order to estimate the contraction intensity for eccentric exercises to be applied to the injured side in the ECC group, maximal performances were evaluated before treatment solely on the contralateral healthy side. At the end of the treatment, both sides were assessed in both groups. Bilateral asymmetries (in percentage) were calculated from peak torques, and body weight normalised peak torques (in N.m/BW) were also analysed.
Disability questionnaire
A questionnaire was used to determine the degree of disability caused by the lateral epicondylitis. The patients answered 10 questions dealing with occupational, free time and sports activities; each question allowed patients to distinguish between four grades of severity, from ‘no disability' to ‘activity impossible'. From the completed questionnaires, an average score of disability was calculated for each patient, with theoretical extreme values ranging from 0 (worst disability) to 20 (no disability). The questionnaire was completed both before and at the end of treatment.
Ultrasonographic examination
Bilateral ultrasonographic examination (Aloka Pro Sound 5500 Ultrasound System Transducer, 7.5–15 MHz, Aloka, Tokyo, Japan) of epicondylian tendons was performed before and after rehabilitation by a single experienced radiologist.38 Direct contact scanning with gel was used for every patient, supplying both longitudinal and transverse images. Characteristics of left and right tendons were measured at the same level. Findings were classified according to the following criteria:
Echoic aspect of the tendon showing either intratendinous hypoechoic lesion or homogeneous tendon structure;
Diameter of the tendon in comparison with the uninjured contralateral side indicating a normal size or a thickness classified into three levels (third grade corresponding to the most pronounced thickness) by the radiologist;
Longitudinal splitting of the tendon;
Intratendinous calcification.
All examiners were blinded with regard to patient allocation into the ECC and CG groups.
Statistical analysis
Values were expressed as means ±SD. The pain score evolution VAS and the questionnaire results were tested by analysis of variance (ANOVA) and a Newman‐Keuls test was used for multiple comparisons. The Kruskal‐Wallis non‐parametric test was used in the analysis of isokinetic strength asymmetry indices. The chi‐squared test was used for analysing the ultrasonographic findings. The level of statistical significance in that study was set at p<0.05.
Results
Eccentric programme delivery
Thirty‐four patients in the ECC group strictly followed the planned eccentric exercise modalities described in table 2. Six patients were unable to reach 60% of the maximal contraction intensity before the end of treatment because of pain when performing the exercises; and six others were moderately delayed in the predetermined eccentric programme while performing, without any complaint, normally the last phase of training at 80% of maximal intensity.
Pain score
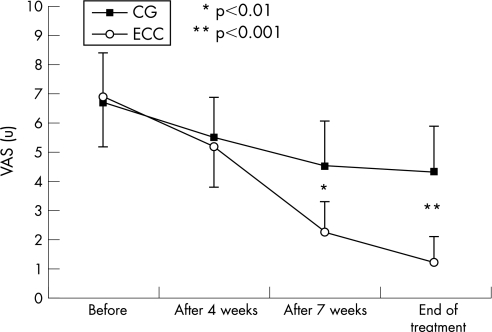
Before treatment, both groups of patients started at the same level of arbitrary pain when evaluated on the VAS (6.7±1.5 in the CG versus 6.9±1.5 in the ECC) (fig 2). After 4 weeks of treatment, we observed a significant (p<0.05) reduction of pain intensity in both groups, although their respective average values remained superior to 5 at that time. The pain score assessment after 7 weeks showed significant differences (p<0.01) between CG and ECC, with a more marked reduction in the ECC group. Pain evolution between the seventh week and the end of treatment showed a significant (p<0.05) decrease in ECC, yet no significant progress was observed in CG. At the end of treatment, the average score reached 4.3±1.6 in the CG, versus 1.2±0.9 in the ECC (p<0.001).
Figure 2 Subjective pain evaluated on a visual analogue scale (in units, u) before, during and at the end of treatment: comparative study between control and trained groups.
Isokinetic performances
At the end of the rehabilitation programme, the injured side among ECC group patients did not show on average any reduction of peak torque, when compared with the contralateral side, whatever the muscle group and the testing modality (table 3). In the ECC group, eccentric muscle performances were significantly (p<0.05) higher on the treated side in comparison with the contralateral side. The bilateral comparison in the CG group revealed a significant reduction of peak torque (p<0.05) in both muscle groups (all modalities of testing) of the injured side. The comparison of bilateral asymmetry indices between both groups of patients indicated a significant (p<0.05) difference in all testing conditions, although peak torques measured on the non‐involved sides in both groups did not differ significantly.
Table 3 Post‐treatment isokinetic concentric (Conc) and eccentric (Ecc) peak torques (in N.m) in both groups of patients: comparative study between treated and non‐involved sides (asymmetry in %).
| Control group (n = 46) | Eccentric group (n = 46) | |||||
|---|---|---|---|---|---|---|
| Treated | Non‐involved | Asymmetry | Treated | Non‐involved | Asymmetry | |
| Wrist extensors | ||||||
| Conc 30°/s | 7.2±3.4 | 10.8±2.5 | −33±19%* | 10.9±2.8 | 10.6±2.4 | + 3±14% |
| Conc 90°/s | 6.6±2.6 | 9.2±2.2 | −28±17%* | 9.2±2.5 | 9.1±2.2 | + 1±15% |
| Ecc 60°/s | 9.7±3.8 | 15.6±3.2 | −38±19%* | 17.4±3.4 | 15.8±3.3 | + 10±15%* |
| Forearm supinators | ||||||
| Conc 30°/s | 5.3±2.9 | 7.3±2.3 | −27±17%* | 7.5±2.8 | 7.1±2.1 | + 6±15% |
| Conc 90°/s | 4.8±2.4 | 6.9±2.1 | −30±18%* | 7±2.2 | 6.8±2.0 | + 3±14% |
| Ecc 60°/s | 7.1±3.3 | 11.4±2.7 | −38±19%* | 13.3±3.1 | 11.2±2.5 | + 16±16%* |
*represents a significant (p<0.05) difference between the treated and non‐involved sides in each group of patients.
Disability questionnaire
Before starting the rehabilitation programme, no difference was observed in the completed disability questionnaires between both groups of patients, the average score reaching respectively 7.8±3.5 in CG and 8.5±3.8 in ECC. After treatment, a significant (p<0.05) improvement in both groups was observed, with average values of 10.2±3.8 in CG and 14.4±4.6 in ECC. Nevertheless, that final score differed significantly (p<0.001) between both groups of patients. The median calculated on the whole sample of patients (n = 92) after treatment reached 12.5. After treatment, 26% and 74% of the CG and ECC groups respectively showed a score higher than 12.5.
Ultrasonographic examination
Before treatment, intratendinous hypoechoic lesions, as well second‐ or third‐grade thickness, were observed in the whole group of patients (n = 92). Echographic observations at the end of treatment are represented in table 4. Respectively, 28% and 48% of patients in the CG and ECC groups (p = 0.055) recovered homogeneous tendon structure with normalisation of the diameter (‘Normalisation' in the table). ‘Improvement' status indicated that moderate alterations in echostructure and first‐grade thickness persisted. A ‘no modification' profile, compared to the pre‐treatment ultrasonographic findings, was observed in 37% cases of CG versus 11% cases of ECC (p = 0.0035). The relative risk (RR) index reached 3.4 (confidence interval 1.4; 8.4) for the ‘no modification' status; this indicates that treatment without eccentric training increases threefold the risk of no improvement in echographic image.
Table 4 Ultrasonographic image evolution in comparison with pre‐treatment findings.
| CG | ECC | p Values | |
|---|---|---|---|
| Normalisation | 13/46 | 22/46 | 0.055 |
| Improvement | 16/46 | 19/46 | 0.52 |
| No modification | 17/46 | 5/46 | 0.0035 |
After the eccentric programme (ECC), 2/8 longitudinal splittings initially observed in pre‐treatment had disappeared, 5/8 were reduced in length and 1/8 did not change in length. Seven pre‐treatment intratendinous calcifications did not change in size. After the non‐strengthening intervention (CG), no modification was observed in either initial longitudinal splittings (n = 6), or in intratendinous calcifications (n = 8).
Discussion
As early as 1986, Stanish et al suggested that the use of eccentric exercises in the treatment of patellar tendon overuse injuries could produce promising clinical results.23 The concept was based on the belief that tendinosis could result from repetitive tensile loads exceeding mechanical strength of the tendon.21,23,39 If loading is increased beyond a certain threshold, normal cellular maintenance is not sufficient to sustain the integrity of the structure and it becomes susceptible to microtrauma.40 Recently, tendinosis has been considered as a connective‐tissue disease that involves the production of collagen that is not remodeled into normal tendon.30 Khan et al referred to a non‐inflammatory degenerative condition of unknown aetiology,41 and Rees et al underlined that, traditionally, treatments have placed a heavy emphasis on anti‐inflammatory strategies which are often inappropriate.42 Such theories highlight the need for structural adaptation of the musculotendinous units in order to protect it from increased stresses and thus prevent re‐injury. Further, most authors underline the incomplete effectiveness of conventional treatment in neglecting strengthening exercises, and being both passive and lacking in induced tendon adaptations.29,39,43,44 It is also well established that disuse and immobilisation provoke collagen and cross‐linked concentration decline, inducing tissue weakness both structurally and materially.21
In our study, while the non‐strengthening programme of treatment applied in the CG group induced a significant reduction of pain on the VAS, it was certainly not as efficient as when combined with the newly designed eccentric training; the pain score still reaching 4.3 at the end of intervention. In spite of a significant improvement in the disability questionnaire score, non‐strengthening treatment did not markedly alleviate symptoms upon return to the activities which caused the original injuries. A deficit of wrist extensor and forearm supinator isokinetic peak torques also persisted at the end of treatment, possibly influenced by lingering symptoms through maximal contraction intensity. Ultrasonographic examination demonstrated inconsistent improvement of the tendon structure, the 28% of cases of normalisation (almost twice less than ECC) contrasting with the absence of any modification in 37% of patients (three times more than ECC).
Bisset et al evaluated wrist posture, upper‐limb reaction time, speed of movement and grip strength in lateral epicondylalgia.11 Motor performance deficits were highlighted which strongly suggest the need for active exercises in treatment prescription.
In the recent literature, numerous studies have used eccentric exercises as a model for Achilles tendinitis management.25,27,29 Thus, Alfredson et al strongly suggested that an eccentric model be properly applied before surgical intervention is instituted in recreational runners suffering from Achilles tendinosis.25 Although a few authors suggested an eccentric exercise model of management in tennis elbow,32,33,34 the use of an isokinetic device to deliver an elaborate eccentric programme has, to our knowledge, never been investigated.
The eccentric programme designed in this study was based on three parameters: length, load and speed. In the eccentric mode of contraction, the patient's effort to resist movement imposed by an external force (produced by the dynamometer) is overwhelmed, which permits repetitive lengthening of the active musculo‐tendinous system. Exercises started with very low contraction intensity (30% of maximum), slow limb movement rate (30°/s) and individually adapted range of motion. The use of an isokinetic device allows the therapist to accurately control the exercise development:
The isokinetic dynamometer maintains its preset velocity;
Permanent resistance adaptation provides an inherent safety mechanism and regular movement;
Instantaneous torque measurement and screen feedback offers the patient the opportunity to adjust the predetermined contraction intensity exactly;
Exercise bouts are performed through a constant range of motion (adjusted by electronic and mechanical stops), possibly avoiding a painful sector such as the end of motion (corresponding to the lengthening position of the tendon);
A passive motion can be used to return to the start position, instead of a concentric loading phase.
The isokinetic eccentric training model combined with classical rehabilitation in the ECC group showed convincing results. Based on progressive intensification of eccentric exercise modalities as described in our programme, treatment was generally well tolerated by the tendon and did not provoke delayed onset muscle soreness (DOMS).45 Nevertheless, 13% of patients in the ECC group did not follow precisely the preset training because of lingering pain when attempting to intensify loading. Therefore, incapacity to reach 60% of maximal exercise intensity after four to five weeks of treatment represents an indicator of poor prognosis in our experience.
At the end of ECC treatment, the subjective sensation of pain at rest evaluated on a VAS appeared to be drastically reduced, even if the score still averaged 1.2. Interestingly, the pain score reduction mainly occurred after one month of treatment. Adaptive responses of tendons to training are slower than those in muscles,46 justifying the slow rate of inducement. That observation, combined with a continuous reduction of pain between the seventh week and the end of treatment, supports the need for a long treatment course. Echographic examination concluded regular improvement in tendon structure, while a relative risk index showed that eccentric training as proposed in our study decreases by 3.4 the risk of ‘no modification' in US findings in comparison with the control group. Nevertheless, 52% of ECC cases did not recover fully normalised images. One hypothesis is that some cases cannot normalise because of initial lesion magnitude linked to long duration of symptoms. A further study would investigate the effectiveness of a longer eccentric programme (e.g. 50 sessions) on ultrasonographic appearance. On the other hand, Khan et al reported that US studies show only moderate correlation with clinical assessment of chronic Achilles tendinopathy.47 Cook et al showed no statistically significant relationship between ultrasonographic patellar tendon abnormalities and clinical outcome in elite male athletes.48 In a previous study, Khan et al also found that patellar tendon sonographic hypoechoic areas can resolve, remain unchanged or even expand in female basketball players without predicting symptoms of jumper's knee.49 According to these findings, the management of lateral epicondylar tendinopathy should not be based solely on ultrasonographic appearance.
The questionnaire applied in our study aimed to reflect disability status through occupational, spare time and sports activities. Starting before treatment with the same score of disability as CG, the patients benefiting from the eccentric programme showed much more marked improvement at the end of the follow‐up. One limitation of this study may be that the disability questionnaire, inspired by a previous study,50 was not validated. However, our experimental findings indicated that a patient with chronic lateral epicondylar tendinopathy has more than two times a greater chance of obtaining relief with eccentric intervention.
Post‐treatment strength measurement in ECC revealed no significant differences in average concentric and eccentric peak torques between the injured and non‐injured sides. Thus, eccentrically treated patients in our study commonly resume activity in the absence of muscle performance deficit. Furthermore, the injured side wrist extensors and forearm supinators showed outstanding eccentric peak torques. Considering the advocated role of eccentric tensile loads in lateral epicondylitis development, such profile could represent an interesting preventive factor of relapse. Obviously, it would have been worthwhile investigating possible strength deficits before launching treatment, as suggested by Pienimäki et al through concentric testing.51 Unfortunately, preliminary attempts to measure strength before starting treatment provoked pain to the injured side during 1 to 2 weeks. Curwin advises against early strength tests involving maximal loading and possibly reproducing the injury pattern if used before full recovery.21 For these reasons, the intensity of eccentric exercise was based on healthy side peak torque measured at the beginning of the training regimen.
According to the prognosis of lateral epicondylitis treated with classical physical therapy,52 the eccentric model's effectiveness would depend on several factors. The differential diagnoses must initially exclude inter‐current pathologies,6,44 such as entrapment of the posterior interosseous nerve or cervical disease with a C6‐7 radiculopathy.6,31,53,54 Commonly, eccentric training will be implemented beyond the initial acute phase. The remodeling phase, characterised by increased cross‐linking in collagen,18 appears more favourable. We chose to perform workouts three times a week in order to give the tendon a sufficient rest period between successive sessions. Effectively, periods of mechanical weakness occur in tendons during adaptation to loading conditions.40 On the other hand, we refute the often advocated principle of ‘no pain, no gain'.22,25 As outlined above, intense exercises aimed at measuring maximal torque before treatment provoked pain in some preliminary cases, which had the effect of delaying treatment effectiveness and making patients suspicious. Nevertheless, 87% of the patients involved in the study succeeded in reaching a painless, very high intensity (80% of the maximal) of contraction throughout the eccentric training sessions. Based on these clinical observations, our position is that pain must be interpreted as an alarm signal and that if the injurious effects of the repetitive motion continue, tendinous suffering may persist or even worsen. Presence of intratendinous calcification complicated the prognosis in our study: this feature was predominantly associated after treatment with persistence of pain and poor decrease in symptoms when returning to the injury‐inducing activities. The failure of an adequate rehabilitation intervention, including progressive eccentric exercises, could indicate the need for surgery.30,31,44,55,56 In addition, it could be appropriate to perform postural retraining11 and to prevent excessive loadings of tendon upon return to activity by controlling intensity and duration of activity, equipment quality and performance technique.53
In spite of the increased refinement in exercise dosage afforded by the isokinetic nature of the eccentric exercise, it would be relevant to test an eccentric training regimen in simpler approaches. The use of elastic resistance bands, manual resistance or free weights could be investigated in further comparative study. Nevertheless, some issues, such as the return to the starting position without experiencing concentric loading, the speed of movement and contraction intensity control, would have to be addressed. In the study by Martinez‐Silvestrini et al,34 a non‐isokinetic eccentric exercise programme combined with stretching did not seem more conclusive than either stretching alone or stretching associated with concentric training.
What is already known on this topic
Current concepts on the lateral epicondylar tendinopathy underline a non‐inflammatory degenerative condition.
Conventional passive treatment that neglects strengthening exercises has been reported as incompletely effective.
Few investigations have focused on adapted eccentric training for tennis elbow.
What this study adds
To the authors' knowledge, this is the first study of eccentric training for tennis elbow involving an elaborate exercise programme using an isokinetic dynamometer.
The short‐term effectiveness of the intervention suggests implementing this adapted eccentric training in the management of chronic lateral epicondylar tendinopathy.
Remodeling process of the tendon by eccentric loading has been hypothesised. Leadbetter suggested that significant reparative response capability resided within the activated tenocyte post‐injury or after overload stimulation.57 While tendinous tissue strength is positively correlated with collagen content and density of stable cross‐links,21,58 enhancement of tensile capacity will probably be linked to the production of ‘normal' collagen, in contrast with ‘abnormal' collagen (type III) observed in tendinosis.30,59 Kraushaar and Nirschl,30 suspecting that it is the extracellular alignment and cross‐linking of collagen that fails in tendinosis, suggested their adaptation could improve the tendon's ability to withstand high levels of tensile force. Indeed, adaptive mechanisms do not simply result from loading exercises, but are probably dependent on the mode of contraction. Effectively, Mafi et al demonstrated that eccentric protocols were significantly more effective than their concentric counterparts in treating chronic Achilles tendinitis.27 More recently, Jonsson and Alfredson showed, through a prospective randomised study, superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee.60 An effect of stretching with a ‘lengthening' of the musculo‐tendinous unit,22 and consequently less strain during an equivalent joint motion, has also been proposed following eccentric bouts.25 Focusing on chronic mid‐portion Achilles tendinosis, Ohberg and Alfredson have suggested that good clinical effects might be mediated through neovascularisation.61
Conclusion
The purpose of this study was to clarify the relevance of an isokinetic eccentric programme in the outcome of chronic lateral epicondylar tendinopathy treatment. We aimed at allowing patients a safer and painless return to the original injury‐inducing occupational, spare time and sports activities. In comparison with a classical non‐strengthening rehabilitation intervention, the designed eccentric model permitted: (a) a significantly more marked reduction of pain intensity after treatment; (b) prevention of forearm supinator and wrist extensor strength deficits on the injured side while maximising the level of eccentric maximal performance; (c) improvement or normalisation of the tendon echographic examination in 89% of cases; (d) participation in occupational, free time and sports activities with marked relief of symptoms. We insist on the specific modalities of the eccentric model promoted in this study, namely: a long treatment course based on very low loads and low speeds in exercise at the beginning, applied three times a week and avoiding pain activation. This clinical study brings up to date the management of chronic lateral epicondylar tendinopathy by providing evidence of the short‐term effectiveness of an isokinetic eccentric training programme. Further studies should focus on the long‐term beneficial effects of this new programme and on understanding the tissular adaptive mechanisms following eccentric exercise loading.
Abbreviations
CG - control group
ECC - eccentric
VAS - visual analogue scale
References
- 1.Hong Q N, Durand M J, Loisel P. Treatment of lateral epicondylitis: Where is the evidence? Joint, Bone, Spine: Rev Rhum 200471369–373. [DOI] [PubMed] [Google Scholar]
- 2.Walker‐Bone K, Palmer K T, Reading I.et al Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum 200451642–651. [DOI] [PubMed] [Google Scholar]
- 3.Ciccotti M G, Charlton W P. Epicondylitis in the athlete. Clin Sports Med 20012077–93. [DOI] [PubMed] [Google Scholar]
- 4.Järvinen M. Epidemiology of tendon injuries in sports. Clin Sports Med 199211493–504. [PubMed] [Google Scholar]
- 5.Pienimäki T T, Kauranen K, Vanharanta H. Bilaterally decreased motor performance of arms in patients with chronic tennis elbow. Arch Phys Med Rehabil 1997781092–1095. [DOI] [PubMed] [Google Scholar]
- 6.Plancher K D, Halbrecht J, Lourie G M. Medial and lateral epicondylitis in the athlete. Clin Sports Med 199615283–305. [PubMed] [Google Scholar]
- 7.Riek S, Chapman A E, Milner T. A simulation of muscle force and internal kinematics of extensor carpi radialis brevis during backhand tennis stroke: implications for injury. Clin Biomech 199914477–483. [DOI] [PubMed] [Google Scholar]
- 8.Almekinders L C, Weinhold P S, Maffulli N. Compression etiology in tendinopathy. Clin Sports Med 200322703–710. [DOI] [PubMed] [Google Scholar]
- 9.Ollivierre C O, Nirschl R P. Tennis elbow – current concepts of treatment and rehabilitation. Sports Med 199622133–139. [DOI] [PubMed] [Google Scholar]
- 10.Smidt N, Assendelft W J, Arola H.et al Effectiveness of physiotherapy for lateral epicondylitis: a systematic review. Ann Med 20033551–62. [DOI] [PubMed] [Google Scholar]
- 11.Bisset L M, Russell T, Bradley S.et al Bilateral sensorimotor abnormalities in unilateral lateral epicondylalgia. Arch Phys Med Rehabil 200687490–495. [DOI] [PubMed] [Google Scholar]
- 12.Hong Q N, Durand M J, Loisel P. Treatment of lateral epicondylitis: where is the evidence? J Bone Spine 200471369–373. [DOI] [PubMed] [Google Scholar]
- 13.Trudel D, Duley J, Zastrow I.et al Rehabilitation for patients with lateral epicondylitis: a systematic review. J Hand Ther 200417243–266. [DOI] [PubMed] [Google Scholar]
- 14.Buchbinder R, Green S E, Youd J M.et al Systematic review of the efficacy and safety of shock wave therapy for lateral elbow pain. J Rheumatol 2006331351–1363. [PubMed] [Google Scholar]
- 15.Hume P A, Reid D, Edwards T. Epicondylar injury in sport: epidemiology, type, mechanisms, assessment, management and prevention. Sports Med 200636151–170. [DOI] [PubMed] [Google Scholar]
- 16.Cook J L, Khan K M. What is the most appropriate treatment for patellar tendinopathy? Br J Sports Med 200135291–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sevier T L, Wilson J K. Treating lateral epicondylitis. Sports Med 199928375–380. [DOI] [PubMed] [Google Scholar]
- 18.Haahr J P, Andersen J H. Prognostic factors in lateral epicondylitis: a randomized trial with one‐year follow‐up in 266 new cases treated with minimal occupational intervention or the usual approach in general practice. Rheumatol 2003421216–1225. [DOI] [PubMed] [Google Scholar]
- 19.Lewis M, Hay E M, Paterson S M.et al Effects of manual work on recovery from lateral epicondylitis. Scand J Work Environ Health 200228109–116. [DOI] [PubMed] [Google Scholar]
- 20.El Hawary R, Stanish W D, Curwin S L. Rehabilitation of tendon injuries in sport. Sports Med 199724347–358. [DOI] [PubMed] [Google Scholar]
- 21.Curwin S. Acute sports injuries: the aetiology and treatment of tendonitis. In: Harries M, Williams C, Stanish WD, et al eds. Oxford Textbook of Sports Medicine. Oxford: Oxford Medical Publications, Oxford University Press, 1994512–528.
- 22.Fyfe I, Stanish W D. The use of eccentric training and stretching in the treatment and prevention of tendon injuries. Clin Sports Med 199211601–624. [PubMed] [Google Scholar]
- 23.Stanish W D, Rubinovich R M, Curwin S. Eccentric exercise in chronic tendonitis. Clin Orthop Rel Res 198620865–68. [PubMed] [Google Scholar]
- 24.Alfredson H, Lorentzon R. Chronic Achilles tendinitis: recommendations for treatment and prevention. Sports Med 200029135–146. [DOI] [PubMed] [Google Scholar]
- 25.Alfredson H, Pietilä I, Jonsson P.et al Heavy‐load eccentric calf muscle training for the treatment of chronic Achilles tendonitis. Am J Sports Med 199826360–366. [DOI] [PubMed] [Google Scholar]
- 26.Jensen K, Di Fabio R P. Evaluation of eccentric exercise in treatment of patellar tendinitis. Phys Ther 198969211–216. [DOI] [PubMed] [Google Scholar]
- 27.Mafi N, Lorentzon R, Alfredson H. Superior short‐term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendonitis. Arthrosc 2001942–47. [DOI] [PubMed] [Google Scholar]
- 28.Croisier J L, Forthomme B, Foidart‐Dessalle M.et al Treatment of recurrent tendinitis by isokinetic eccentric exercises. Isokinetics Exerc Sci 20019133–141. [Google Scholar]
- 29.Paavola M, Kannus P, Paakkala T.et al Long‐term prognosis of patients with Achilles tendonitis. Am J Sports Med 200028634–642. [DOI] [PubMed] [Google Scholar]
- 30.Kraushaar B S, Nirschl R P. Current concepts review. Tendinosis of the elbow (tennis elbow). J Bone Joint Surg 199981‐A259–278. [PubMed] [Google Scholar]
- 31.Nirschl R P. Elbow tendinosis/tennis elbow. Clin Sports Med 199211851–870. [PubMed] [Google Scholar]
- 32.Svernlov B, Adolfsson L. Non‐operative treatment regime including eccentric training for lateral humeral epicondylalgia. Scan J Med Sci Sports 200111328–334. [DOI] [PubMed] [Google Scholar]
- 33.Stasinopoulos D, Stasinopoulou K, Johnson M I. An exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med 200539944–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martinez‐Silvestrini J A, Newcomer K L, Gay R E.et al Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther 200518411–419. [DOI] [PubMed] [Google Scholar]
- 35.Paolini J A, Murrell G A. Identification of prognostic indicators for patient outcomes in extensor tendinopathy at the elbow. Scand J Med Sci Sports 200414163–167. [DOI] [PubMed] [Google Scholar]
- 36.Waugh E J, Jaglal S B, Davis A M.et al Factors associated with prognosis of lateral epicondylitis after 8 weeks of physical therapy. Arch Phys Med Rehab 200485308–318. [DOI] [PubMed] [Google Scholar]
- 37.Forthomme B, Croisier J L, Foidart‐Dessalle M.et al Isokinetic assessment of the forearm and wrist muscles. Isokinetics Exerc Sci 200210121–128. [Google Scholar]
- 38.Marcelis S, Daenen B, Ferrara M A.Peripheral musculoskeletal ultrasound atlas. (Dondelinger RF, ed. ) New York: Thieme Medical Publishers, 1996
- 39.Almekinders L C, Temple J D. Etiology, diagnosis, and treatment of tendinitis: an analysis of the literature. Med Sci Sports Exerc 1998301183–1190. [DOI] [PubMed] [Google Scholar]
- 40.Archambault J M, Wiley J P, Bray R. Exercise loading of tendons and the development of overuse injuries. Sports Med 19952077–89. [DOI] [PubMed] [Google Scholar]
- 41.Khan K M, Cook J L, Bonar F.et al Histopathology of common tendinopathies. Sports Med 199927393–408. [DOI] [PubMed] [Google Scholar]
- 42.Rees J D, Wilson A M, Wolman R L. Current concepts in the management of tendon disorders. Rheumatol 200645508–521. [DOI] [PubMed] [Google Scholar]
- 43.Rivenburgh D W. Physical modalities in the treatment of tendon injuries. Clin Sports Med 199211645–659. [PubMed] [Google Scholar]
- 44.Bennett J B. Lateral and medial epicondylitis. Hand Clin 199410157–163. [PubMed] [Google Scholar]
- 45.Croisier J L, Camus G, Forthomme B.et al Delayed onset muscle soreness induced by eccentric isokinetic exercise. Isokinetics Exerc Sci 20031121–29. [Google Scholar]
- 46.Kannus P, Jozsa L, Natri A.et al Effects of training, immobilization and remobilization on tendons. Scand J Med Sci Sports 1997767–71. [DOI] [PubMed] [Google Scholar]
- 47.Khan K M, Forster B B, Robinson J.et al Are ultrasound and magnetic resonance imaging of value in assessment of Achilles tendon disorders? A two year prospective study. Br J Sports Med 200337149–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cook J L, Khan K M, Kiss Z S.et al Asymptomatic hypoechoic regions on patellar tendon ultrasound: A 4‐year clinical and ultrasound followup of 46 tendons. Scand J Med Sci Sports 200111321–327. [DOI] [PubMed] [Google Scholar]
- 49.Khan K M, Cook J L, Kiss Z S.et al Patellar tendon ultrasonography and jumper's knee in female basketball players: a longitudinal study. Clin J Sport Med 19977199–206. [DOI] [PubMed] [Google Scholar]
- 50.Overend T J, Wuori‐Fearn J L, Kramer J F.et al Reliability of a patient‐rated forearm evaluation questionnaire for patients with lateral epicondylitis. J Hand Ther 19991231–37. [DOI] [PubMed] [Google Scholar]
- 51.Pienimäki T T, Süra P T, Vanharanta H. Chronic medial and lateral epicondylitis: a comparison of pain, disability and function. Arch Phys Med Rehabil 200283317–321. [DOI] [PubMed] [Google Scholar]
- 52.Waugh E J, Jaglal S B, Davis A M.et al Factors associated with prognosis of lateral epicondylitis after 8 weeks of physical therapy. Arch Phys Med Rehabil 200485308–318. [DOI] [PubMed] [Google Scholar]
- 53.Nirschl R P, Ashman E S. Elbow tendinopathy: tennis elbow. Clin Sports Med 200322813–836. [DOI] [PubMed] [Google Scholar]
- 54.Ekstrom R A, Holden K. Examination of and intervention for a patient with chronic lateral elbow pain with signs of nerve entrapment. Phys Ther 2002821077–1086. [PubMed] [Google Scholar]
- 55.Rosenberg N, Henderson I. Surgical treatment of resistant lateral epicondylitis. Follow‐up study of 19 patients after excision, release and repair of proximal common extensor tendon origin. Arch Orthop Trauma Surg 2002122514–517. [DOI] [PubMed] [Google Scholar]
- 56.Whaley A L, Baker C L. Lateral epicondylitis. Clin Sports Med 200423677–691. [DOI] [PubMed] [Google Scholar]
- 57.Leadbetter W B. Cell‐matrix response in tendon injury. Clin Sports Med 199211533–578. [PubMed] [Google Scholar]
- 58.Hyman J, Rodeo S A. Injury and repair of tendons and ligaments. Phys Med Rehabil Clin North America 200011267–288. [PubMed] [Google Scholar]
- 59.Maffulli N, Ewen S W B, Waterston S W.et al Tenocytes from ruptured and tendinopathic Achilles tendons produce greater quantities of type III collagen than tenocytes from normal Achilles tendons. Am J Sports Med 200028499–505. [DOI] [PubMed] [Google Scholar]
- 60.Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper's knee: a prospective randomised study. Br J Sports Med 200539847–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Öhberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic mid‐portion Achilles tendinosis? Knee Surg Sports Traumatol Arthrosc 200412465–470. [DOI] [PubMed] [Google Scholar]