Abstract
High cardiothoracic ratio (CTR) is a marker of enlarged heart and is associated with poor outcomes in heart failure (HF). However, to what extent this association is independent of other confounders is not well known. To study this, we used propensity score matching to design a study in which HF patients with normal (≤0.50) and high (>0.50) CTR were well-balanced in all measured baseline covariates. In the Digitalis Investigation Group trial (N=7788), 4690 patients had high (>0.50) CTR. Propensity scores for high CTR were calculated for each patient and were then used to match 2586 pairs of patients with normal and high CTR. Matched Cox regression analyses were used to estimate associations of high CTR with mortality and hospitalization during 37 months of median follow-up. All-cause mortality occurred in 28.5% (rate, 919/10,000 person-years of follow-up) of patients with normal CTR and 34.3% (rate, 1185/10,000 person-years) of patients with high CTR (hazard ratio {HR} 1.35; 95% confidence interval {CI} 1.21–1.51; p<0.0001). All-cause hospitalization occurred in 64.8% (rate, 3513/10,000 person-years) of patients with normal CTR and 66.2% (rate, 3932/10,000 person-years) of patients with high CTR (HR 1.10; 95% CI 1.01–1.20; p=0.032). Respective HR’s (95% CI) for other outcomes were: 1.48 (1.30–1.68; p <0.0001) for cardiovascular mortality, 1.57 (1.28–1.92; p <0.0001) for HF mortality, 1.18 (1.08–1.30; p =0.001) for cardiovascular hospitalization and 1.27 (1.13–1.44; p <0.0001) for HF hospitalization. In conclusion, baseline CTR >0.50 was associated with increased mortality and morbidity in ambulatory chronic HF patients.
Keywords: heart failure, cardiothoracic ratio, mortality, outcomes
High cardiothoracic ratio (CTR), estimated by chest roentgenogram, is a marker of cardiomegaly, and has been shown to be associated with poor outcomes in heart failure (HF).1–3 However, to what extent this association is independent of other confounders is not well known. Residual bias due to confounding covariates is a concern for studies based on regression-based risk adjustment methods. Further, most of these studies had relatively small sample sizes, short follow up duration, and mortality was the only outcome studied. The objective of this propensity-matched study was to determine the association of baseline high CTR with a broad spectrum of natural history endpoints in a cohort of ambulatory chronic HF patients where patients with normal (≤0.50) and high (>0.50) CTR were well-balanced in all measured baseline covariates.
Methods
The DIG trial enrolled 7788 ambulatory patients with chronic HF in normal sinus rhythm from 302 clinical centers in the United States and Canada from 1991 to 1993.4,5 Of these patients, 6800 had left ventricular ejection fractions of <45% and 4690 had high (>0.50) CTR. The primary end points were mortality and hospitalizations due to all causes, cardiovascular causes, and worsening HF. Data on vital status were 99% complete.6
Because of significant imbalance in baseline covariates between patients with normal and high CTR (Table 1), we used propensity score matching to assemble a cohort of patients where patients with normal and high CTR would be well-balanced in all measured baseline covariates.7–11 We estimated propensity scores for high CTR for each of the 7788 patients using a non-parsimonious, multivariate logistic regression model, adjusting for all available baseline covariates presented in Table 1. We then used an SPSS macro (SPSS, Inc., Chicago, Illinois) to match 2586 pairs of patients with normal and high CTR who had similar propensity scores. The details of the matching protocol have been described elsewhere.12–16 We then objectively estimated bias reduction using absolute standardized differences (<10% being inconsequential bias).12,14–18
Table 1.
Baseline patient characteristics of heart failure (HF) patients, by cardiothoracic ratio (CTR), before and after propensity score matching
| Before matching
|
After matching
|
|||||
|---|---|---|---|---|---|---|
| Variables: N (%) or mean ±SD | CTR ≤0.50 (n = 3,098) | CTR >0.50 (n = 4,690) | p Value | CTR ≤0.50 (n = 2,586) | CTR >0.50 (n = 2,586) | p Value |
| Age (years) | 63 ± 11 | 65 ± 11 | <0.0001 | 64 ± 10 | 64 ± 11 | 0.611 |
| Age ≥65 years | 1,500 (48%) | 2,536 (54%) | <0.0001 | 1,324 (51%) | 1,292 (50%) | 0.389 |
| Female | 510 (17%) | 1,416 (30%) | <0.0001 | 492 (19%) | 491 (19%) | 1.000 |
| Non-white | 267 (9%) | 861 (18%) | <0.0001 | 259 (10%) | 242 (9%) | 0.452 |
| Body mass index, kg/m2 | 27 ± 5 | 28 ± 6 | <0.0001 | 27 ± 5 | 27 ± 5 | 0.650 |
| Duration of HF (months) | 30 ± 35 | 29 ± 37 | 0.385 | 30 ± 35 | 30 ± 38 | 0.873 |
| Primary cause of HF | ||||||
| Ischemic | 2,308 (75%) | 3,052 (65%) | 1,873 (72%) | 1,885 (73%) | ||
| Hypertensive | 254 (8%) | 551 (12%) | <0.0001 | 231 (9%) | 235 (9%) | |
| Idiopathic | 365 (12%) | 746 (16%) | 324 (13%) | 317 (12%) | 0.938 | |
| Others | 171 (6%) | 341 (7%) | 158 (6%) | 149 (6%) | ||
| Prior myocardial infarction | 2,119 (68%) | 2,789 (60%) | <0.0001 | 1,717 (66%) | 1,733 (67%) | 0.329 |
| Current angina pectoris | 895 (29%) | 1,220 (26%) | 0.005 | 725 (28%) | 716 (28%) | 0.780 |
| Hypertension | 1,290 (42%) | 2,384 (51%) | <0.0001 | 1,145 (44%) | 1,163 (45%) | 0.634 |
| Diabetes mellitus | 818 (26%) | 1,400 (30%) | 0.001 | 715 (28%) | 719 (28%) | 0.901 |
| Chronic kidney disease | 1,310 (42%) | 2,217 (47%) | <0.0001 | 1,162 (45%) | 1,139 (44%) | 0.520 |
| Medications | ||||||
| Pre-trial digoxin use | 1,271 (41%) | 2,094 (45%) | 0.002 | 1,091 (42%) | 1,114 (43%) | 0.536 |
| Trial use of digoxin | 1,554 (50%) | 2,335 (50%) | 0.763 | 1,303 (50%) | 1,286 (50%) | 0.637 |
| ACE inhibitors | 2,884 (93%) | 4,390 (94%) | 0.376 | 2,423 (94%) | 2,421 (94%) | 0.955 |
| Hydralazine & nitrates | 21 (1%) | 90 (2%) | <0.0001 | 21 (1%) | 17 (1%) | 0.626 |
| Diuretics | 2,171 (70%) | 3,905 (83%) | <0.0001 | 1,967 (76%) | 1,961 (76%) | 0.871 |
| PS diuretics | 234 (8%) | 362 (8%) | 0.828 | 207 (8%) | 220 (9%) | 0.544 |
| Potassium supplement | 736 (24%) | 1,463 (31%) | <0.0001 | 681 (26%) | 687 (27%) | 0.850 |
| Symptoms and signs of HF | ||||||
| Dyspnea at rest | 510 (17%) | 1,195 (26%) | <0.0001 | 468 (18%) | 485 (19%) | 0.542 |
| Dyspnea on exertion | 2,236 (72%) | 3,626 (77%) | <0.0001 | 1,898 (73%) | 1,911 (74%) | 0.705 |
| Limitation of activity | 2,236 (72%) | 3,667 (78%) | <0.0001 | 1,925 (74%) | 1,920 (74%) | 0.899 |
| Jugular venous distension | 254 (8%) | 766 (16%) | <0.0001 | 240 (9%) | 249 (10%) | 0.704 |
| Third heart sound | 570 (18%) | 1,276 (27%) | <0.0001 | 529 (21%) | 531 (21%) | 0.973 |
| Pulmonary râles | 334 (11%) | 967 (21%) | <0.0001 | 315 (12%) | 327 (13%) | 0.643 |
| Lower extremity edema | 479 (16%) | 1,154 (25%) | <0.0001 | 444 (17%) | 451 (17%) | 0.797 |
| Number of symptom/signs | 5.1 ± 2.1 | 5.7 ± 2.0 | <0.0001 | 5.3 ± 2.0 | 5.3 ± 2.1 | 0.527 |
| NYHA functional classes | ||||||
| Class I | 525 (17%) | 578 (12%) | 398 (15%) | 408 (16%) | ||
| Class II | 1,844 (60%) | 2,400 (51%) | <0.0001 | 1,505 (58%) | 1,483 (57%) | 0.824 |
| Class III | 710 (23%) | 1,577 (34%) | 664 (26%) | 671 (26%) | ||
| Class IV | 19 (1%) | 135 (3%) | 19 (1%) | 24 (1%) | ||
| Heart rate (/minute) | 77 ± 12 | 79 ± 13 | <0.0001 | 78 ± 13 | 78 ± 13 | 0.782 |
| BP, systolic (mm Hg) | 127 ± 20 | 127 ± 1 | 0.864 | 128 ± 20 | 128 ± 21 | 0.727 |
| BP, diastolic (mm Hg) | 75 ± 11 | 75 ± 12 | 0.120 | 75 ± 11 | 75 ± 11 | 0.590 |
| Pulmonary congestion by chest x-ray | 228 (7%) | 881 (19%) | <0.0001 | 226 (9%) | 227 (9%) | 0.843 |
| Serum creatinine (mg/dL) | 1.27 ± 0.436 | 1.29 ± 0.438 | 0.035 | 1.28 ± 0.437 | 1.28 ± 0.436 | 0.807 |
| Serum potassium (mEq/L) | 4.4 ± 0.4 | 4.3 ± 0.5 | <0.0001 | 4.4 ± 0.4 | 4.4 ± 0.4 | 0.377 |
| Estimated glomerular filtration rate, ml/min per 1.73 m2 | 65 ± 21 | 63 ± 23 | <0.0001 | 64 ± 22 | 64 ± 20 | 0.595 |
| Ejection fraction (%) | 34 ± 12 | 30 ± 13 | <0.0001 | 33 ± 12 | 33 ± 13 | 0.944 |
| Ejection fraction >45% | 492 (16%) | 496 (11%) | <0.0001 | 346 (13%) | 365 (14%) | 0.443 |
ACE=angiotensin-converting enzyme; BP=blood pressure; NYHA=New York Heart Association; PS=potassium sparing
The baseline characteristics of patients with normal and high CTR were compared using Pearson’s chi-square and Wilcoxon’s rank-sum tests. Kaplan-Meier analysis and matched Cox regression analyses were used to determine the association of high CTR (relative to normal CTR) with various outcomes. Subgroup analyses and first-order interactions were used to test the heterogeneity of the association between high CTR and mortality. All statistical tests were done using SPSS-14 for Windows (SPSS, Inc., Chicago, Illinois).
Results
Patients had a mean (±SD) age of 64 (±11) years, 19% were women, and 10% were nonwhites. All significant imbalances in baseline covariates before matching were balanced after matching (Table 1). Values of absolute standardized differences for all covariates after matching between patients with normal and high CTR were <5% (Figure 1).
Figure 1.
Absolute standardized differences before and after propensity score matching comparing covariate values for patients with cardiothoracic ratio ≤0.5 and >0.5
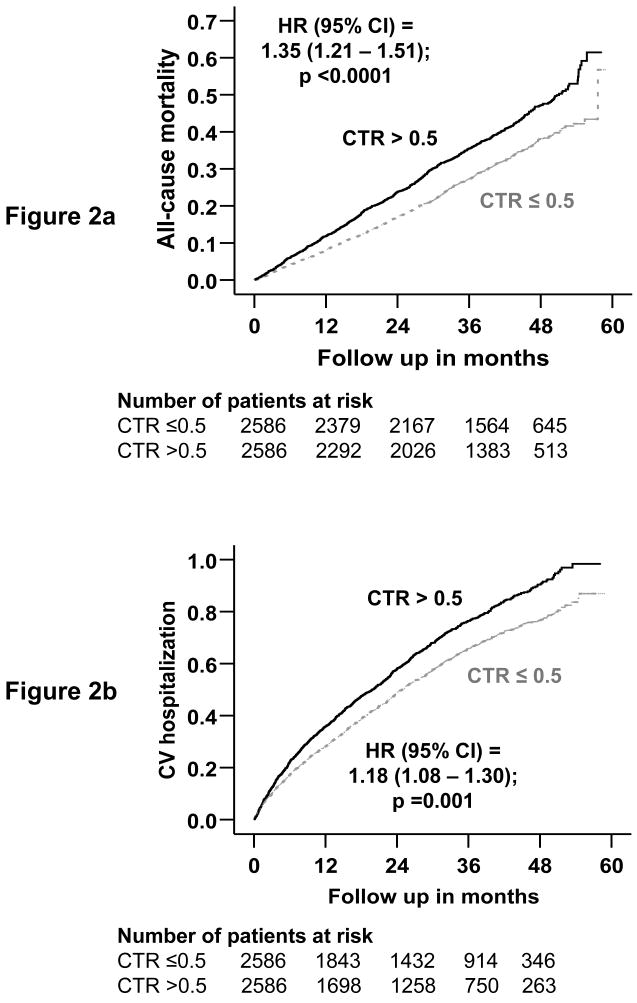
Overall, 1625 patients (31%) died, including 1272 (25%) due to cardiovascular causes and 521 (10%) due to progressive HF, during the median follow-up period of 37 months. Kaplan-Meier plots for all-cause mortality are displayed in Figure 2A. All-cause mortality occurred in 738 patients (rate, 919/10,000 person-years) with normal CTR during 8028 years of follow-up and in 887 patients (rate, 1185/10,000 person-years) with high CTR during 7485 years of follow up (hazard ratio {HR}, 1.35; 95% confidence interval {CI}, 1.21–1.51; p<0.0001; Table 2). High CTR was associated with similar increases in cardiovascular and HF mortality (Table 2). High CTR-associated all-cause mortality was observed across various subgroups of patients (Figure 3).
Figure 2.
Kaplan-Meier plots for (a) all-cause mortality and (b) cardiovascular (CV) hospitalization by cardiothoracic ratio (CTR)
Table 2.
Mortality and hospitalizations by causes in heart failure patients before and after matching by propensity scores for cardiothoracic ratio (CTR) >0.50
| Outcomes | CTR=0.50 (N=2582)
|
CTR>0.50 (N=2582)
|
Absolute rate difference* (per 10,000 person-years) | Hazard ratio(95% confidence interval) | P value |
|---|---|---|---|---|---|
| Rate, per 10,000 person-years (Events/total follow up years) | |||||
| Mortality | |||||
| All-cause | 919 (738/8028) | 1185 (887/7485) | + 265 | 1.35 (1.21–1.51) | <0.0001 |
| Cardiovascular | 689 (553/8028) | 961 (719/7485) | + 272 | 1.48 (1.30–1.68) | <0.0001 |
| Progressive heart failure | 280 (225/8028) | 395 (296/7485) | + 115 | 1.57 (1.28–1.92) | <0.0001 |
| Hospitalization† | |||||
| All-cause | 3513 (1676/4771) | 3932 (1712/4354) | + 419 | 1.10 (1.01–1.20) | 0.032 |
| Cardiovascular | 2187 (1250/5715) | 2647 (1358/5131) | + 460 | 1.18 (1.08–1.30) | 0.001 |
| Progressive heart failure | 927 (650/7011) | 1180 (746/6321) | + 253 | 1.27 (1.13–1.44) | <0.0001 |
| Number of total hospitalizations | 5932 | 6779 | + 847 | ||
Absolute differences in rates of events per 10,000 person-year of follow up were calculated by subtracting the event rates in the normal-CTR group from the event rates in the high-CTR group (before values were rounded).
Data shown include the first hospitalization of each patient for each cause.
Figure 3. Hazard ratio (HR) and 95% confidence interval (CI) for all-cause mortality for cardiothoracic ratio > 0.5 in subgroups of heart failure patients.
Chronic kidney disease defined as estimated glomerular filtration rate <60 ml/min/1.73m2. NYHA=New York Heart Association
Overall, 3388 patients (66%) were hospitalized for all causes, including 2608 (50%) for cardiovascular causes and 1396 (27%) for worsening HF. Kaplan-Meier plots for all-cause hospitalization are displayed in Figure 2B. All-cause hospitalization occurred in 1676 normal-CTR patients (rate, 3513/10,000 person-years) during 4771 years of follow-up and 1712 high-CTR patients (rate, 3932/10,000 person-years) during 4354 person-years of follow-up (HR, 1.10; 95% CI, 1.01–1.20; p<0.0001; Table 2). High CTR was associated with similar increases in hospitalizations due to cardiovascular causes and worsening HF (Table 2).
Discussion
The results of the current analysis demonstrate that high CTR at baseline as measured by chest x-ray was a marker of poor prognosis for a wide range of major natural history end points in chronic HF. To the best of our knowledge, this is the first demonstration of such association in a large population of propensity-matched chronic systolic and diastolic HF patients with long follow-up of a range of cause-specific mortalities and hospitalizations. These findings are important as despite common use of electrocardiograph and echocardiograph in the evaluation of HF in developed nations, use of chest x-ray is an important element in the initial assessment of patients with chronic HF.19,20
An enlarged heart, often clinically estimated by a radiographic evidence of CTR >0.50 or an electrocardiographic evidence of left ventricular hypertrophy, is considered abnormal, especially in the context of HF. An enlarged heart may be the results of myocardial fibrosis and ventricular remodeling, which may in part explain the high-CTR associated poor prognosis in HF.21,22 Recent data suggest that CTR is significantly increased in primary pulmonary hypertension and may predominantly reflect right- rather than left-sided cardiomegaly,23,24 both of which are independent predictors of poor outcomes in HF.25–29
The results of our study are consistent with those of reported by other investigators.1–3 However, our study is distinguished from prior studies by its large sample size, long follow up of wide spectrum of major naturally history end points, and use of propensity score matching to design the study. Before matching, patients with a high baseline CTR were more likely to be elderly, have ischemic heart disease, hypertension, diabetes, and chronic kidney disease, more severe HF, and lower ejection fraction (Table 1, Figure 1), all characteristics associated with poor outcomes. Because post-match absolute standardized differences for all measured baseline covariates were <5%, it is unlikely that the results of our study can be explained by baseline variations in covariates. The results of our study highlights the importance of routine chest x-ray during initial assessment of HF, and risk stratify patients based on CTR.19,20
Key limitations of our study include those associated with non-randomize design of our study and its inability to account for unmeasured confounders. Our sensitivity analysis suggests that an unmeasured binary covariate could potentially invalidate the results of our study if it would also increase the odds of high CTR by as little as 21%.30 However, for that unmeasured covariate to become a confounder, it should be a strong predictor of mortality and also should not be strongly correlated with any of the measured covariates (Table 1). Of note, the results of sensitivity analysis cannot determine the existence of such a covariate. Other limitations are related to the age of the study data and characteristic of study population (largely young white male systolic HF patients with normal sinus rhythm from pre β-blocker era of HF therapy), which may limit generalizability to contemporary HF patients. In conclusion, baseline CTR >0.5 is associated with increased mortality and hospitalization in chronic HF. Chest x-ray assessment of CTR should be routinely incorporated as a part of initial assessment of HF, and may be used to risk-stratify HF patients.
Acknowledgments
Funding/Support: Dr. Ahmed is supported by the National Institutes of Health through grants from the National Heart, Lung, and Blood Institute (1-R01-HL085561-01 and P50-HL077100).
“The Digitalis Investigation Group (DIG) study was conducted and supported by the NHLBI in collaboration with the DIG Investigators. This manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the DIG Study or the NHLBI.”
Footnotes
Conflict of Interest Disclosures: None
References
- 1.Ernst ER, Shub C, Bailey KR, Brown LR, Redfield MM. Radiographic measurements of cardiac size as predictors of outcome in patients with dilated cardiomyopathy. J Card Fail. 2001;7:13–20. doi: 10.1054/jcaf.2001.23244. [DOI] [PubMed] [Google Scholar]
- 2.Cohn JN, Johnson GR, Shabetai R, Loeb H, Tristani F, Rector T, Smith R, Fletcher R. Ejection fraction, peak exercise oxygen consumption, cardiothoracic ratio, ventricular arrhythmias, and plasma norepinephrine as determinants of prognosis in heart failure. The V-HeFT VA Cooperative Studies Group. Circulation. 1993;87:VI5–16. [PubMed] [Google Scholar]
- 3.Kearney MT, Fox KA, Lee AJ, Brooksby WP, Shah AM, Flapan A, Prescott RJ, Andrews R, Batin PD, Eckberg DL, Gall N, Zaman AG, Lindsay HS, Nolan J. Predicting sudden death in patients with mild to moderate chronic heart failure. Heart. 2004;90:1137–1143. doi: 10.1136/hrt.2003.021733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Digitalis Investigation Group. Rationale, design, implementation, and baseline characteristics of patients in the DIG trial: a large, simple, long-term trial to evaluate the effect of digitalis on mortality in heart failure. Control Clin Trials. 1996;17:77–97. doi: 10.1016/0197-2456(95)00065-8. [DOI] [PubMed] [Google Scholar]
- 5.The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–533. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 6.Collins JF, Howell CL, Horney RA. Determination of vital status at the end of the DIG trial. Control Clin Trials. 2003;24:726–730. doi: 10.1016/j.cct.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Rosenbaum PR, Rubin DB. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 8.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Asso. 1984;79:516–524. [Google Scholar]
- 9.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 10.Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- 11.Rubin DB. On principles for modeling propensity scores in medical research. Pharmacoepidemiol Drug Saf. 2004;13:855–857. doi: 10.1002/pds.968. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed A. A propensity matched study of New York Heart Association class and natural history end points in heart failure. Am J Cardiol. 2007;99:549–553. doi: 10.1016/j.amjcard.2006.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed A, Ali M, Lefante CM, Mullick MS, Kinney FC. Geriatric heart failure, depression, and nursing home admission: an observational study using propensity score analysis. Am J Geriatr Psychiatry. 2006;14:867–875. doi: 10.1097/01.JGP.0000209639.30899.72. [DOI] [PubMed] [Google Scholar]
- 14.Ahmed A, Husain A, Love TE, Gambassi G, Dell’Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006;27:1431–1439. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed A, Perry GJ, Fleg JL, Love TE, Goff DC, Jr, Kitzman DW. Outcomes in ambulatory chronic systolic and diastolic heart failure: a propensity score analysis. Am Heart J. 2006;152:956–966. doi: 10.1016/j.ahj.2006.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmed A, Rich MW, Sanders PW, Perry GJ, Bakris GL, Zile MR, Love TE, Aban IB, Shlipak MG. Chronic kidney disease associated mortality in diastolic versus systolic heart failure: a propensity matched study. Am J Cardiol. 2007;99:393–398. doi: 10.1016/j.amjcard.2006.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 18.Normand ST, Landrum MB, Guadagnoli E, Ayanian JZ, Ryan TJ, Cleary PD, McNeil BJ. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 19.Radford MJ, Arnold JM, Bennett SJ, Cinquegrani MP, Cleland JG, Havranek EP, Heidenreich PA, Rutherford JD, Spertus JA, Stevenson LW, Goff DC, Grover FL, Malenka DJ, Peterson ED, Redberg RF. ACC/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Heart Failure Clinical Data Standards): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Failure Society of America. Circulation. 2005;112:1888–1916. doi: 10.1161/CIRCULATIONAHA.105.170073. [DOI] [PubMed] [Google Scholar]
- 20.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW, Antman EM, Smith SC, Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 21.Unverferth DV, Baker PB, Pearce LI, Lautman J, Roberts WC. Regional myocyte hypertrophy and increased interstitial myocardial fibrosis in hypertrophic cardiomyopathy. Am J Cardiol. 1987;59:932–936. doi: 10.1016/0002-9149(87)91128-3. [DOI] [PubMed] [Google Scholar]
- 22.Weber KT, Janicki JS, Pick R, Capasso J, Anversa P. Myocardial fibrosis and pathologic hypertrophy in the rat with renovascular hypertension. Am J Cardiol. 1990;65:1G–7G. doi: 10.1016/0002-9149(90)90952-w. [DOI] [PubMed] [Google Scholar]
- 23.Kanemoto N, Furuya H, Etoh T, Sasamoto H, Matsuyama S. Chest roentgenograms in primary pulmonary hypertension. Chest. 1979;76:45–49. doi: 10.1378/chest.76.1.45. [DOI] [PubMed] [Google Scholar]
- 24.Fukuta H, Ohte N, Brucks S, Carr JJ, Little WC. Contribution of right-sided heart enlargement to cardiomegaly on chest roentgenogram in diastolic and systolic heart failure. Am J Cardiol. 2007;99:62–67. doi: 10.1016/j.amjcard.2006.07.067. [DOI] [PubMed] [Google Scholar]
- 25.Dokainish H, Sengupta R, Patel R, Lakkis N. Usefulness of right ventricular tissue Doppler imaging to predict outcome in left ventricular heart failure independent of left ventricular diastolic function. Am J Cardiol. 2007;99:961–965. doi: 10.1016/j.amjcard.2006.11.042. [DOI] [PubMed] [Google Scholar]
- 26.Gavazzi A, Ghio S, Scelsi L, Campana C, Klersy C, Serio A, Raineri C, Tavazzi L. Response of the right ventricle to acute pulmonary vasodilation predicts the outcome in patients with advanced heart failure and pulmonary hypertension. Am Heart J. 2003;145:310–316. doi: 10.1067/mhj.2003.146. [DOI] [PubMed] [Google Scholar]
- 27.Ghio S, Gavazzi A, Campana C, Inserra C, Klersy C, Sebastiani R, Arbustini E, Recusani F, Tavazzi L. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001;37:183–188. doi: 10.1016/s0735-1097(00)01102-5. [DOI] [PubMed] [Google Scholar]
- 28.Kjaergaard J, Akkan D, Iversen KK, Kjoller E, Kober L, Torp-Pedersen C, Hassager C. Prognostic importance of pulmonary hypertension in patients with heart failure. Am J Cardiol. 2007;99:1146–1150. doi: 10.1016/j.amjcard.2006.11.052. [DOI] [PubMed] [Google Scholar]
- 29.Voelkel NF, Quaife RA, Leinwand LA, Barst RJ, McGoon MD, Meldrum DR, Dupuis J, Long CS, Rubin LJ, Smart FW, Suzuki YJ, Gladwin M, Denholm EM, Gail DB. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. Circulation. 2006;114:1883–1891. doi: 10.1161/CIRCULATIONAHA.106.632208. [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum PR. Sensitivity to Hidden Bias. In: Rosenbaum PR, editor. Observational Studies. New York: Springer-Verlag; 2002. pp. 110–124. [Google Scholar]