Abstract
Background
Activation of the alveolar macrophage is centrally important to the development of lung ischemia reperfusion injury. Alveolar macrophages and type 2 pneumocytes secrete a variety of proinflammatory mediators in response to oxidative stress. The manner in which they interact and how the macrophage may influence pneumocyte responses in lung ischemia reperfusion injury is unknown. Utilizing an in vitro model of hypoxia and reoxygenation, we sought to determine if the proinflammatory response of type 2 pneumocytes to oxidative stress would be amplified by alveolar macrophage secretory products.
Methods
Cultured pneumocytes were exposed to control media or media from cultured macrophages exposed to hypoxia and reoxygenation. Pneumocytes were subsequently subjected to hypoxia and reoxygenation and assessed for both nuclear translocation of nuclear factor kappa B and inflammatory cytokine and chemokine secretion. To examine for any reciprocal interactions, we reversed the experiment, exposing macrophages to conditioned pneumocyte media.
Results
In the presence of media from stimulated macrophages, production of proinflammatory mediators by type 2 pneumocytes was dramatically enhanced. In contrast, exposure of the macrophage to conditioned pneumocyte media had an inhibitory effect on macrophage responses subsequently exposed to hypoxia and reoxygenation.
Conclusions
The alveolar macrophage drives the development of lung reperfusion injury in part through amplification of the inflammatory response of type 2 pneumocytes subjected to hypoxia and reoxygenation.
Keywords: Transplantation, lung, Hypoxia, reoxygenation, Cell biology, culture
INTRODUCTION
Advances in donor management, organ preservation, surgical technique, post operative care and immunosuppression have improved overall survival rates following lung transplantation, but the incidence of lung ischemia reperfusion injury (LIRI) remains unchanged at 20% (1,2,3). Clinically, LIRI is characterized by pulmonary edema, reduced pulmonary compliance and poor gas exchange (4). Treatment options are supportive. Patients surviving the initial insult face an upregulation of MHC class II molecules, which can vary depending on the severity of LIRI, increasing the risk of both acute rejection and obliterative bronchiolitis (5,6,7). Characterization of the cellular mechanisms leading to the development of LIRI may lead to therapeutic interventions and improved outcomes.
Studies performed on in vivo rodent models have established the existence of a biphasic response to lung ischemia and reperfusion (8). The early response occurs following 90 minutes of ischemia and 15 minutes of reperfusion and involves the nuclear translocation of proinflammatory transcription factors with subsequent upregulation of transcription and secretion of inflammatory cytokines and chemokines (9,10,11). In the lung, there is a transient increase in vascular permeability together with a brief burst of oxidant release. As this phase has been shown to be neutrophil independent, resident cell types within the lung must be responsible for this early proinflammatory response. This initial release of mediators is critically important to driving the late phase of lung reperfusion injury, characterized by a sustained rise in vascular permeability and accumulation of neutrophils in the lung.
Alveolar macrophages (AM) are a rich source of oxidants, cytokines, chemokines, growth factors and arachidonic metabolites (12). Previous studies have implicated the AM as centrally important to the development of LIRI. Within 15 minutes of reperfusion, tumor necrosis factor-alpha (TNF-α) is localized exclusively to the AM but not other lung cell types. AM depletion with liposomal clodronate or suppression with gadolinium is associated with significant reductions in vascular permeability, nuclear translocation of transcription factors, bronchoalveolar lavage fluid concentrations of TNF-α, macrophage inflammatory protein-2 (MIP-2), cytokine-induced neutrophil chemoattractant (CINC), and macrophage inflammatory protein-1α (MIP-1α), and accumulation of tissue neutrophils (13,14). These findings indirectly suggest that AM derived products are important to the development of injury. While the role of the AM in orchestrating inflammatory responses to oxidative stress in the lung is apparent, how they exert that influence has not been fully elucidated.
Another constituent cell population in the lung, type 2 pneumocytes (T2P), help control fluid balance and composition in the alveolar space and can proliferate and differentiate into type 1 pneumocytes to maintain alveolar integrity following lung injury (15). T2P have also been shown to upregulate proinflammatory signaling cascades in response to oxidative stress. In vitro studies of T2P established that nuclear translocation of nuclear factor kappa B (NFκB), and secretion of CINC and monocyte chemotactic protein 1 (MCP-1), are all increased in response to hypoxia and reoxygenation (H/R) (16).
The ability of the AM secretory products to augment inflammatory signaling in other lung cell types in response to oxidative stress has recently been described (17). Chemokine secretion by pulmonary artery endothelial cells (PAEC) when subjected to H/R was shown to be enhanced when cells were exposed to inflammatory mediators secreted by AM. We hypothesized that a similar crosstalk exists between T2P and AM. Utilizing an in vitro cell culture model, we examined if T2P inflammatory signaling in response to oxidative stress was altered when cells were exposed to media collected from AM subjected to H/R. To examine for a reciprocal influence of T2P products on AM, AM were subjected to the same oxidative stress in the presence of control media or media from T2P previously exposed to H/R.
METHODS
Reagents
All reagents were purchased from Sigma Chemicals (St Louis, MO) unless otherwise specified.
Alveolar macrophage harvest
Pathogen-free adult male Long-Evans rats (Simonsen Labs, Gilroy, CA) weighing 250 g to 300 g were used for all experiments. The University of Washington Animal Care Committee approved all experimental protocols. Animals received humane care in compliance with the “Principles of Laboratory Animal Care” formulated by the National Society for Medical Research and “The Guide for the Care and the Use of Laboratory Animals” prepared by the Institute of Laboratory Animal Resources and published by the Institute of Health.
Animals were euthanized with 120 mg/kg of intraperitoneal pentobarbitol. A 14-gauge angiocatheter was inserted into the trachea through a midline neck incision and secured with a 4-0 braided silk suture. A median sternotomy was performed and the heart lung block rapidly excised. Intratracheal lavage of the lungs was performed 15 times with graduated volumes of 3 to 10ml with cold phosphate-buffered saline (PBS) to minimize damage to lung tissue. This process yielded a 90% lavage recovery. Collected lavage fluid was centrifuged at 1,500 g for 10 minutes and the cell pellet resuspended in serum free RPMI (Gibco BRL). Cells counts and viability were assessed by trypan blue exclusion methods, and RPMI added until a density of 500,000 cells per milliliter was reached. One ml of this cellular media was loaded for each well of a 12-well culture plate (Fisher Scientific, Pittsburgh, PA), and AM were incubated at 37°C for 60 minutes to allow adherence. Media was then substituted with fresh RPMI containing 5% heat inactivated fetal bovine serum (FBS). The concentration of FBS was identical among all experimental and control groups.
Hypoxia and reoxygenation
We generated three types of AM media for subsequent exposure to T2P. Control media was generated by plating AM and leaving them unstimulated for 6 hours. Early AM media was collected from AM that underwent 2 hours of hypoxia and 15 minutes of reoxygenation and used to investigate the effects of AM products released during hypoxia or early in reoxygenation. This simulates the “early phase” of LIRI. Late AM media was generated by subjecting AM to 2 hours of hypoxia followed by 4 hours of reoxygenation and used to investigate the influence of AM products generated later in reoxygenation.
Prepared AM were incubated in a humidified hypoxic chamber (Coy Lab Products, Grass Lake, MI) with 0.5% oxygen for 2 hours at 37°C. Reoxygenation was achieved by removing the plate from the hypoxic chamber and placing it into a normoxic humidified incubator for either 15 minutes or 4 hours, which restores normal oxygen tension in the media within two minutes. Media was then aspirated and stored at −80°C. Media samples were either analyzed for baseline chemokine content by enzyme linked immunoassay (ELISA) or used for stimulation of T2P. The baseline chemokine content produced by AM was subtracted from total amounts in media collected at the end of the co-culture experiments, allowing for specific assessment of the chemokine response of T2P. Cell viability following hypoxia and reoxygenation has been previously demonstrated as >95% for both T2P and AM (16,18).
Type 2 Pneumocytes
A rat T2P cell line, RLE-6TN (American Tissue Cell Company, Manassas, VA) was maintained in Hams F-12 culture media containing 10% heat inactivated FBS. The T2P were cultured in 12 well plates at a density of 200,000 cells per milliliter. Cell counts and viability were assessed by a standard trypan blue exclusion technique and media was replenished every 48 hours until confluence was achieved.
Treatment of T2P with AM media
Before placing T2P in the hypoxic chamber, media was exchanged for media obtained from one of the three pre-conditioned AM groups, (control, early or late). The effects of AM media on T2P were assessed under three different conditions. Negative control T2P were maintained at normoxic conditions and 37°C, additional T2P were subjected to 0.5% oxygen for 2 hours at 37°C. Reoxygenation was achieved by removing the plate from the hypoxic chamber and placing it into a normoxic humidified incubator for either 15 minutes (H/R 15) or 4 hours (H/R 4). After 15 minutes of reoxygenation, nuclear protein was harvested from cells to assess nuclear translocation of NFκB by electromobility shift assay (EMSA). After 15 minutes and 4 hours of reoxygenation, media was collected and analyzed for chemokine content by ELISA. Thirty-six samples from each combination of media and H/R condition were assessed for chemokine content.
Reciprocal Experiment – Treatment of AM with media derived from T2P
T2P were maintained in Hams F-12 and exposed to the conditions described for generation of AM media. Control media was not subjected to H/R. A second group underwent 2 hours of hypoxia and 15 minutes of reoxygenation, generating early T2P media. The third group was subjected to 2 hours of hypoxia followed by 4 hours of reoxygenation, generating late T2P media.
Conditioned T2P media was collected and samples were analyzed for baseline chemokine content by ELISA. This would allow for correction of total chemokine content in the media so that the amount produced specifically by the AM could be determined.
At the start of the experiment, AM media was exchanged with conditioned media generated from one of the three pre-treated T2P groups. AM were then incubated in the hypoxic chamber and reoxygenated as described above. After 15 minutes and 4 hours of reoxygenation both groups underwent analysis for NFκB by EMSA and chemokine content by ELISA as described below.
Nuclear Protein Extraction
Cells were harvested in a 100 μl solution of low-salt buffer containing MgCl2 (1.5 mM), KCl (10 mM) and HEPES (10 mM). This solution was spun at 1200g for 1 minute, and the pellet resuspended in 40 μl of a low-salt buffer solution containing MgCl2 (1.5 mM), KCl (10 mM), HEPES (10 mM), 0.06% Nonidet P-40, and 0.01 μg/ml of leupeptin. This solution was spun a at 1200g for 10 minutes and the pellet resuspended in a buffer containing NaCl (420 mM), HEPES (20 mM), EDTA (0.2 mM), MgCl2 (1.5 mM), PMSF (0.5 mM), DTT (0.5 mM), 25% glycerol and incubated at 4°C for 20 minutes. The suspension was centrifuged for at 1200g for 10 minutes, and the supernatant containing the nuclear protein was collected and frozen at −80°C. Quantification of nuclear protein yield was achieved via bicinchoninic acid assay (Pierce, Rockford, IL).
Electromobility Shift Assay
10 μg aliquots of nuclear protein were incubated in a binding reaction with a double stranded 32P end-labeled oligonucleotide containing the consensus NFκB binding sequence 5′-GCCATTGGGGATTTC-CTCTTTACTGG-3′ (Promega, Madison, WI). The binding reaction was performed at room temperature for 60 minutes and protein resolved on a 6% non-denaturing polyacrylamide gel at 100v for 1 to 2 hours. The gels were dried and subsequently radiographed. Duplicate samples for each condition were analyzed from each experiment. Densitometry was performed with Image J software (Version 1.2, Silver Spring, MD) to assess relative signal intensity. Results were verified by at least three independent experiments.
Enzyme Linked Immunoassay of Cytokine or Chemokine Content
Sandwich ELISAs for CINC, MIP-1α and MCP-1 were performed per the manufacturer’s instructions. 50 μl of a 10 μg/ml anti-chemokine antibody was added (Peprotech, Rocky Hills, New Jersey) to a carbonate-coating buffer solution (pH=9.6). The solution was plated in a 96-well immunoassay plate (Dynex) and incubated overnight at room temperature. The plate was washed with phosphate buffered saline containing 0.05% Tween (PBST) before blocking nonspecific binding sites with a 1% bovine serum albumin/phosphate buffered saline solution for 1 hour at room temperature. Samples and standards were diluted 1:1 in phosphate buffered saline and 100 μl was added to each well and incubated at room temperature for 2 hours. The wells were washed in PBST, and between 0.5 to 2 μg/ml of secondary biotinylated antibody (Peprotech, Rocky Hills, New Jersey) was added to each well and incubated for 2 hours at room temperature. Wells were washed in PBST for a third time, and incubated for 20 minutes with a streptavidin-horseradish-peroxidase conjugate (Pierce, Rockford, IL). The assay was developed by adding o-phenylenediamine dihydrochloride substrate and analyzed on a spectrophotometer. The linear sensitivity range of the assays has been determined and the assays show no cross reactivity with one other. Samples and standards were run in triplicate, and well-to-well variation did not exceed 5%.
Statistical Analysis
A biostatistician, Dr. Chris Gross, was consulted for statistical analysis. All data was presented as mean values (± the standard deviation) unless otherwise designated. Statistical differences between groups were assessed using two-tailed Student’s t-test (Microsoft Excel 2002, Microsoft Corp., Redmond, Washington) with post-hoc Bonferroni adjustment for multiple comparisons. Statistical significance was defined as a p<0.05.
RESULTS
Response of separate cell types to hypoxia and reoxygenation
Under the influence of H/R, secretion of CINC and MCP-1 was increased in isolated AM and T2P (Tables 1 and 2). A dramatic increase in production of these two chemokines occurs after 2 hours of hypoxia and 15 minutes of reoxygenation but was most pronounced after 4 hours of reoxygenation. Secretion of MIP-1α was similarly increased under the influence of H/R in AM.
Table 1.
Effect of early and late alveolar macrophage products on type 2 pneumocyte response to hypoxia and reoxygenation.
| Media | |||
|---|---|---|---|
| Product | Control Media | Early AM Mediaa | Late AM Mediaa |
| CINC (pg/mL +/− SD) | |||
| Normoxic Control | 98 +/− 13 | 173 +/−8 b | 524 +/− 45b, d |
| Hypoxia | |||
| with 15 minutes reoxygenation | 259 +/− 21b | 2090 +/− 104c | 1023 +/− 71c, d |
| with 4 hours reoxygenation | 429 +/− 16b | 2445 +/− 342c | 2677 +/− 239c |
|
| |||
| MCP-1 (pg/mL +/− SD) | |||
| Normoxic Control | 1530 +/− 59 | 2040 +/− 113b | 6475 +/− 250b, d |
| Hypoxia | |||
| with 15 minutes reoxygenation | 4075 +/− 217b | 16983 +/− 606c | 14869 +/− 205c, d |
| with 4 hours reoxygenation | 10639 +/−125b | 34350 +/− 2232c | 38200 +/− 1716c |
Cytokine content corrected for baseline content in media;
p<0.01 compared with normoxic controls;
p<0.01 compared with control media, comparable hypoxia/reoxygenation state;
p<0.01 compared with early media, comparable hypoxia/reoxygenation state; CINC=cytokine-induced neutrophil chemoattractant; MCP-1=monocyte chemoattractant protein-1; AM=alveolar macrophage.
N=36 for each media/hypoxia-reoxygenation condition
Table 2.
Effect of early and late type 2 pneumocyte products on alveolar macrophage response to hypoxia and reoxygenation.
| Media |
|||
|---|---|---|---|
| Product | Control Media | Early T2P Mediaa | Late T2P Mediaa |
| CINC (pg/mL +/− SD) | |||
| Normoxic Control | 33 +/− 3 | 94 +/− 15b | 257 +/− 60b |
| Hypoxia | |||
| with 15 minutes reoxygenation | 205 +/− 20b | 440 +/− 50 | 260 +/− 37 e |
| with 4 hours reoxygenation | 725 +/− 137b | 149 +/− 21c | 327 +/− 70c, e |
|
| |||
| MCP-1 (pg/mL +/− SD) | |||
| Normoxic Control | 148 +/− 5 | 424 +/− 48b | 896 +/− 73b, e |
| Hypoxia | |||
| with 15 minutes reoxygenation | 358 +/− 58 b | 566 +/− 41 | 805 +/− 95e |
| with 4 hours reoxygenation | 699 +/− 138 b | 515 +/− 59 d | 875 +/− 62d, e |
|
| |||
| MIP-1α (pg/mL +/− SD) | |||
| Normoxic Control | 3908 +/−303 | 2291 +/−294b | 2319 +/−371b, e |
| Hypoxia | |||
| with 15 minutes reoxygenation | 11284 +/−959b | 12257 +/−1608 | 6373 +/−675e |
| with 4 hours reoxygenation | 16999 +/− 1031b | 4801 +/−545 c | 2271 +/−178 c, e |
Cytokine content corrected for baseline content in media;
p<0.01 compared with normoxic controls;
p<0.01 compared with control media, comparable hypoxia/reoxygenation state;
p<0.01 compared with control media, comparable hypoxia/reoxygenation state;
p<0.01 compared with early media, comparable hypoxia/reoxygenation state; MIP-1α=macrophage inflammatory protein 1α CINC=cytokine-induced neutrophil chemoattractant; MCP-1=monocyte chemoattractant protein-1; AM=alveolar macrophage.
N=36 for each media/hypoxia-reoxygenation condition
Effect of AM Products on T2P Responses
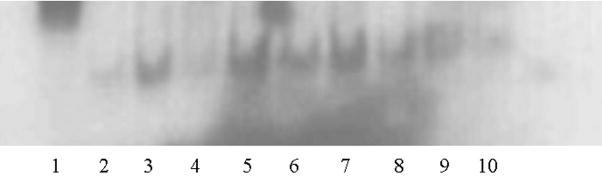
When T2P underwent H/R in the presence of stimulated AM media there was a marked response in transcription factor nuclear translocation and chemokine secretion. NFκB nuclear translocation increased substantially when T2P were stimulated with hypoxia and 15 minutes of reoxygenation in the presence of stimulated AM products. The rise in NFκB translocation was most pronounced when T2P were co-stimulated with early macrophage products (Figure 1).
Figure 1. Representative EMSA for NFκB content in T2P treated with AM media.
NFκB translocation was increased in T2P subjected to hypoxia and 15 minutes of reoxgenation (H/R 15) in the presence of early AM media (Lanes 5, 6, 7) compared to T2P undergoing H/R 15 with control AM media (Lanes 2, 3, 4) (p=0.03). A non-statistically significant trend toward increased NFκB translocation was noted for T2P costimulated with late AM media (Lanes 8, 9, 10). Cold competition (Lane 1) verified the band was NFκB.
Both early and late conditioned AM media provoke a striking increase in the production of MCP-1 and CINC from T2P subjected to 2 hours of hypoxia and 15 minutes of reoxygenation. No further enhancement could be demonstrated after 4 hours of reoxygenation
Effects of T2P Media on AM Responses
Exposure of the AM to T2P media did not significantly alter MCP-1 production by the AM assessed after 4 hours of reoxygenation. Interestingly, both MIP-1α and CINC production by AM were inhibited by T2P secretory products
COMMENT
Early AM secretory products significantly augmented the nuclear translocation of NFκB in T2P undergoing H/R. Late AM secretory products resulted in a nonstatistically significant trend toward increased translocation of NFκB in T2P undergoing H/R. The increase in the translocation of NFκB seen in the conditioned AM media correlated with enhanced secretion of inflammatory mediators MCP-1 and CINC to levels significantly greater than those produced by T2P in the absence of conditioned AM media. Conversely, T2P products demonstrated an inhibitory effect on the production of CINC and MIP-1α by the AM. Differences in NFκB translocation between these groups may reflect differential production of mediators involved in the signaling response following H/R.
In our in vitro model, both early and late AM media augmented the T2P response to oxidative stress, suggesting that this co-stimulatory effect is physiologically relevant. It likely occurs during the early signaling phase of LIRI within 15 minutes of reperfusion in vivo. Given that T2P represent 10–15% of the total lung cell population, this secretory amplification may have a substantial effect on the development of LIRI.
During lung transplantation, there is approximately 90 minutes of warm atelectatic ischemia, the duration of which correlates strongly with acute graft dysfunction. Clinically, this lung injury begins to manifest within an hour of reperfusion and is usually obvious within several hours (19, 20). As such, we used 90 minutes of hypoxia followed by measurements of secretory products after 15 minutes and 4 hours of reoxygenation. These methods of hypoxia and reoxygenation have been developed as a model for the physiologic effects occurring during lung transplantation and often result in LIRI (21).
The use of the RLE-6TN cell line as a model for alveolar type II epithelial cells is one limitation of our study because it represents an immortalized rat lung epithelial-T-antigen negative cell line (22). Published reports demonstrate these cells are likely derived by spontaneous immortalization and may not be a true representation of oxidatively stressed alveolar epithelium, though these cells demonstrate similar staining characteristics to primary alveolar type II cells (22,23). The RLE-6TN cell line was used in our model due to the limitations of harvesting and culturing primary type II cells from rodents including contamination with macrophages after cell harvest and differentiation into cells characteristic of type I cells.
We recognize that conclusions drawn from cell culture experiments cannot necessarily be extrapolated to explain in vivo events. However, in related studies, we have shown that our co-culture system approximates our rodent model of LIRI. Immunostaining has localized TNF-α and IL-1β to AM in vivo after 15 minutes of reperfusion following 90 minutes of ischemia (13,14). Mitogen-activated protein kinase (MAPK) activation has similar patterns of cell specific activation in vivo to what is seen in cultured cells (24). After ischemia and 15 minutes of reperfusion, JNK and p38 localize to AM while ERK1/2 is activated in T2P and PAEC. These patterns are unchanged after 4 hours of reperfusion. Similarly p38 and JNK are phosphorylated in AM after H/R while ERK1/2 is not. ERK1/2 phosphorylation occurs in T2P and PAEC but not macrophages (25).
Our findings suggest many parallels between in vitro and in vivo models. Signaling events are difficult to map in complex in vivo systems. They are more discretely characterized using such cell culture systems. Our system is a useful tool in this regard.
These studies have directly implicated AM secretory products as capable of enhancing T2P responses to H/R. This supports our central hypothesis that the AM is the key coordinating cell in the inflammatory response to oxidative stress in the lung. Proinflammatory mediators secreted by the AM in response to oxidative stress prime surrounding T2P to secrete greater levels of chemokines than they would in response to oxidative stress alone. Preliminary data from our laboratory has also identified the release of TNF- α and IL-1 β by AM in response to H/R as specific mediators augmenting the responses of T2P and PAEC. Furthermore, we have demonstrated an inhibitory affect of both early and late T2P media on MIP-1a production in the setting of normoxia and H/R, suggesting a negative feedback loop which warrants further investigation in the future.
ABBREVIATIONS
- AM
Alveolar macrophage
- CINC
Cytokine induced neutrophil chemoattractant
- ELISA
Enzyme linked immunosorbent assay
- EMSA
Electrophoretic mobility shift assay
- ERK1/2
Extracellular signal-regulated kinase
- FBS
Fetal bovine Serum
- H/R
Hypoxia/Reoxygenation
- IL-1β
Interleukin-1 beta
- JNK
c-Jun N-terminal kinase
- LIRI
Lung ischemia reperfusion injury
- MAPK
Mitogen-activated protein kinase
- MCP-1
Monocyte chemotactic protein-1
- MHC
Major histocompatibility complex
- MIP-1α
Macrophage inflammatory protein-1 alpha
- MIP-2
Macrophage inflammatory protein-2
- NFκB
Nuclear factor kappa B
- PAEC
Pulmonary artery endothelial cell
- PBS
Phosphate buffered saline
- PBST
Phosphate buffered saline with tween
- RPMI
Roswell Park Memorial Institute Media
- T2P
Type 2 pneumocyte
- TNF-α
Tumor necrosis factor alpha
References
- 1.Ardehali A, Laks H, Russell H, et al. Modified reperfusion and ischemia-reperfusion injury in human lung transplantation. J Thorac Cardiovasc Surg. 2003;126(6):1929–34. doi: 10.1016/s0022-5223(03)00976-0. [DOI] [PubMed] [Google Scholar]
- 2.Wittwer T, Wahler T, Fehrenbach A, Elki S, Haverich A. Improvement of pulmonary preservation with Celsior and Perfadex: impact of storage time on early post-ischemic lung function. J Heart Lung Transplant. 1999;18:1198–1201. doi: 10.1016/s1053-2498(99)00088-1. [DOI] [PubMed] [Google Scholar]
- 3.Christie JD, Bavaria JE, Palevsky HI, et al. Primary graft failure following lung transplantation. Chest. 1998;114:51–60. doi: 10.1378/chest.114.1.51. [DOI] [PubMed] [Google Scholar]
- 4.Meyers BF, Lynch J, Trulock EP, Guthrie TJ, Cooper JD, Patterson GA. Lung transplantation: a decade of experience. Ann Surg. 1999;230:362–70. doi: 10.1097/00000658-199909000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serrick C, Giaid A, Reis A, Shennib H. Prolonged ischemia is associated with more pronounced rejection in the lung allograft. Ann Thorac Surg. 1997;63(1):202–8. doi: 10.1016/s0003-4975(96)00898-3. [DOI] [PubMed] [Google Scholar]
- 6.Nikbakht-Sangari M, Qayumi AK, Duronio V. The increase in the steady-state level of major histocompatibility complex mRNA in the host peripheral T lymphocytes due to ischemia-reperfusion injury. Transpl Immunol. 1999;7(2):107–13. doi: 10.1016/s0966-3274(99)80027-6. [DOI] [PubMed] [Google Scholar]
- 7.Qayumi AK, MD, PhD, Nikbakht-Sangari M, BSc, et al. The relationship of ischemia-reperfusion injury of transplanted lung and the up-regulation of major histocompatibility complex II on host peripheral. J Thoracic Cardiovasc Surg. 1998;115:978–982. doi: 10.1016/s0022-5223(98)70395-2. [DOI] [PubMed] [Google Scholar]
- 8.Eppinger MJ, Jones ML, Deeb GM, Bolling SF, Ward PA. Pattern of injury and the role of neutrophils in reperfusion injury of rat lung. J Surg Res. 1995;58:713–18. doi: 10.1006/jsre.1995.1112. [DOI] [PubMed] [Google Scholar]
- 9.Ross SD, Kron IL, Gangemi JJ, et al. Attenuation of lung reperfusion injury after transplantation using an inhibitor of nuclear factor-kappa B. Am J Physiol Lung Cell Mol Physiol. 2000;279(3):L528–36. doi: 10.1152/ajplung.2000.279.3.L528. [DOI] [PubMed] [Google Scholar]
- 10.Baeuerle PA, Baltimore D. NFκB: ten years after. Cell. 1996;87:13–20. doi: 10.1016/s0092-8674(00)81318-5. [DOI] [PubMed] [Google Scholar]
- 11.Naidu BV, Farivar AS, Woolley SM, Byrne K, Mulligan MS. Chemokine response of pulmonary artery endothelial cells to hypoxia and reoxygenation. J Surg Res. 2003;114(2):163–71. doi: 10.1016/s0022-4804(03)00330-5. [DOI] [PubMed] [Google Scholar]
- 12.Ward PA. Phagocytes and the lung. Ann NY Acad Sci. 1997;832:304–10. doi: 10.1111/j.1749-6632.1997.tb46258.x. [DOI] [PubMed] [Google Scholar]
- 13.Naidu BV, Krishnadasan B, Farivar AS, et al. Early activation of the alveolar macrophage is critical to the development of lung ischemia reperfusion injury. J Thorac Cardiovasc Surg. 2003;126(1):200–7. doi: 10.1016/s0022-5223(03)00390-8. [DOI] [PubMed] [Google Scholar]
- 14.Naidu BV, Woolley SM, Farivar AS, et al. Early tumor necrosis factor alpha release from the pulmonary macrophage in lung ischemia reperfusion injury. J Thorac Cardiovasc Surg. 2004;127(5):1502–8. doi: 10.1016/j.jtcvs.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 15.Wang S, Young RS, Witten ML. Age-related differences in pulmonary inflammatory responses to JP-8 jet fuel aerosol inhalation. Toxicol Ind Health. 2001;17(1):23–9. doi: 10.1191/0748233701th094oa. [DOI] [PubMed] [Google Scholar]
- 16.Farivar AS, Woolley SM, Fraga CH, Byrne K, Mulligan MS. Proinflammatory response of alveolar type II pneumocytes to in vitro hypoxia and reoxygenation. Am J Transplant. 2004;4(3):346–51. doi: 10.1111/j.1600-6143.2004.00352.x. [DOI] [PubMed] [Google Scholar]
- 17.McCourtie AS, Merry HE, Farivar AS, Goss CH, Mulligan MS. Alveolar macrophage secretory products augment the response of rat pulmonary artery endothelial cell to hypoxia and reoxygenation. Ann Thorac Surg. 2008;85:1056–60. doi: 10.1016/j.athoracsur.2007.10.058. [DOI] [PubMed] [Google Scholar]
- 18.McCourtie AS, Farivar AS, et al. Poly (ADP) ribose synthetase inhibition in alveolar macrophages undergoing hypoxia and reoxygenation. Experimental and Molecular Pathology Apr. 2008;84:141–144. doi: 10.1016/j.yexmp.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 19.De Perrot M, Liu M, Waddell TK, Keshavjee S. Ischemia-reperfusion-induced lung injury. Am J Respir Crit Care Med. 2003 Feb 15;167(4):490–511. doi: 10.1164/rccm.200207-670SO. [DOI] [PubMed] [Google Scholar]
- 20.Meyer BF, Lynch J, Trulock EP, Guthrie TJ, Cooper JD, Patterson GA. Lung transplantation: A decade of experience. Ann Surg. 1999;230:362–7. doi: 10.1097/00000658-199909000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naidu BV, Krishnadasan B, Byrne K, Farr AL, Rosengart M, Verrier ED, Mulligan MS. Regulation of chemokine expression by cyclosporine A in alveolar macrophages exposed to hypoxia and reoxygenation. Ann Thorac Surg. 2002 Sep;74(3):899–905. doi: 10.1016/s0003-4975(02)03746-3. [DOI] [PubMed] [Google Scholar]
- 22.Driscoll KE, Carter JM, Iype PT, et al. Establishment of an immortalized alveolar type II epithelial cell line from adult rats. In vitro Cell Dev Biol Anim. 1995;31:516–527. doi: 10.1007/BF02634029. [DOI] [PubMed] [Google Scholar]
- 23.Wang S, Young RS, Sun NN, Witten ML. Cytokine release from rat type II pneumocytes and alveolar macrophages following exposure to JP-8 jet fuel in co-culture. Toxicology. 2002;173:211–219. doi: 10.1016/s0300-483x(02)00037-9. [DOI] [PubMed] [Google Scholar]
- 24.Wolf PS, Merry HE, Farivar AS, McCourtie AS, Mulligan MS. Stress-activated protein kinase inhibition to ameliorate lung ischemia reperfusion injury. J Thorac Cardiovasc Surg. 2008;135(3):656–65. doi: 10.1016/j.jtcvs.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 25.Farivar AS, Mackinnon-Patterson BC, Barnes AD, McCourtie AS, Mulligan MS. Cyclosporine modulates the response to hypoxia-reoxygenation in pulmonary artery endothelial cells. Ann Thorac Surg. 2005;79(3):1010–6. doi: 10.1016/j.athoracsur.2004.08.078. [DOI] [PubMed] [Google Scholar]