SUMMARY
We have recently shown in non-human primates that caloric restriction (CR) initiated during adulthood can delay T-cell aging and preserve naïve CD8 and CD4 T cells into advanced age. An important question is whether CR can be initiated at any time in life, and whether age at the time of onset would modulate beneficial effects of CR. In the current study we evaluated the impact of CR started before puberty or during advanced age on T cell senescence and compared it to the effects of CR started in early adulthood. Our data demonstrate that the beneficial effects of adult onset CR upon T-cell aging were lost by both early and late CR onset. In fact, some of our results suggest that inappropriate initiation of CR may be harmful to the maintenance of T cell function. This suggests that there may be an optimal window during adulthood where CR can delay immune senescence and improve correlates of immunity in primates.
INTRODUCTION
Human life expectancy has increased worldwide, with the most dramatic gains achieved in the developed world. Thus, in the U.S., the proportion of elderly individuals (over the age of 65) currently makes up 13% of the population and is projected to reach 20% by the year 2020. An obvious, but uniquely complex and multilayered, challenge for medical and biomedical scientists is to reduce morbidity and mortality and improve health and quality of life in this rapidly growing population. One of the most remarkable advances leading to the increase in human lifespan was made by improving sanitary and public health conditions to control infectious diseases. While that has drastically reduced mortality from infectious diseases up to advanced adulthood, infectious diseases remain a significant problem for the elderly, being consistently amongst the top five leading causes of death (Htwe, Mushtaq et al. 2007; Liang and Mackowiak 2007).
Aging results in a progressive structural alteration and functional decline in multiple organ systems, including a general decline in immunity referred to as immune senescence. Immune senescence is marked by changes in multiple components of the immune system, with the changes in adaptive immunity being the most pronounced and most consistent. These changes include loss of naïve T and B lymphocytes and accumulation of memory phenotype cells, resulting in a dramatic decrease in repertoire diversity (Johnson and Cambier 2004; Gruver, Hudson et al. 2007), which is further compounded by the appearance of T and B cell clonal expansions (Szabo, Li et al. 2004; Clambey, Kappler et al. 2007). This loss of naive lymphocytes coincides with reduced lymphocyte responsiveness to stimulation on a per-cell basis (Miller 2000), which further contributes to poor responses to infection and vaccination seen in the elderly. Another hallmark of immune senescence is increased production of proinflammatory cytokines, including IL-6 and TNFα (Ershler and Keller 2000), which have the potential to contribute to a wide range of age-related diseases, including, but not limited to, Alzheimer’s disease, osteoporosis, atherosclerosis and certain types of cancers (Vasto, Candore et al. 2007).
Among the potential interventions to increase lifespan and improve the quality of life and decrease morbidity in the elderly, caloric restriction (CR) has gained status as a frontrunner over the last several decades. CR is the only intervention to date known to increase both the median and maximal life span in a wide variety of short-lived species (rev. in (Masoro 2003; Roth, Ingram et al. 2007)), and to reduce the incidence of age-related diseases. With regard to the function of the immune system, long-term CR was shown to improve several aspects of immune function in laboratory animals (rev. in (Pahlavani 2004; Nikolich-Zugich and Messaoudi 2005)). Thus, in rodents CR augments immune competence, inhibits age related dysregulation of cytokine secretion (Effros, Svoboda et al. 1991; Spaulding, Walford et al. 1997), and prevents the accumulation of senescent T cells through the enhancement of apoptosis (Spaulding, Walford et al. 1997). CR also reduces the incidence of autoimmune disease and cancer (Weindruch and Walford 1982; Weindruch 1989; Volk, Pugh et al. 1994).
Despite the plethora of data supporting the beneficial impact of CR on immunological function, our understanding of the mechanisms of action of CR remains incomplete. Thus, while new discoveries keep emerging (Masoro 2004; Bishop and Guarente 2007; Medvedik and Sinclair 2007), we still do not fully understand molecular mechanisms by which CR extends lifespan and promotes health. Similarly, our understanding of the effect of CR in long-lived species, of the impact of CR on primate physiology, and of the plasticity of the aging process in response to CR onset at different points in the lifespan remain incomplete.
An informative series of studies have been forthcoming from the nonhuman primate (rhesus macaques, Macaca mulatta, RM in the text) cohorts established at the National Institute on Aging (NIA) and the Wisconsin National Primate Research Center (WNPRC) (Lane, Ingram et al. 1999; Ramsey, Colman et al. 2000). Initial results from these studies have demonstrated that in primates CR exerts many of the same physiological changes seen in rodents (Lane, Black et al. 2001), including a decrease in body weight and fat mass, reduced blood lipids, improved glucoregulatory function and decreased blood pressure (Verdery, Ingram et al. 1997; Edwards, Rudel et al. 1998; Cefalu, Wagner et al. 1999). Furthermore, CR attenuated the age-related decrease in dehydroepiandrosterone (DHEA) and melatonin (Roth, Lesnikov et al. 2001) in male RM, and there are indications that similar changes are occurring under CR in humans (Roberts and Schoeller 2007).
Using the NIA RM cohort, we have recently shown that long-term CR initiated during adolescence (at 3–5 years of age; adolescent-onset CR or AO-CR) can delay T cell senescence as measured by higher numbers of circulating naïve T cells, lower numbers of inflammatory cytokine-secreting memory T cells, and higher proliferative capacity (Messaoudi, Warner et al. 2006). These changes would be expected to improve immune response to infection and vaccination. However, these results were a significant departure from earlier reports that suggested a decrease in immune function in rhesus macaques with shorter exposure to CR, specifically lymphopenia and reduced T cell proliferation to mitogenic stimulus and immunization. (Grossmann, Rabinovitch et al. 1995; Roecker, Kemnitz et al. 1996; Weindruch, Lane et al. 1997). In addition to length of time on a CR diet, the age of initiation was different between the two study populations. While our earlier study reported on monkeys that began CR between the 3 and 5 years old, the latter study reported on monkeys initiated at 8 to 14 years of age. (Kemnitz, Weindruch et al. 1993; Roecker, Kemnitz et al. 1996). To address whether the age of CR onset can influence T cell homeostasis and function in RM, we compared two additional groups of monkeys that began calorie restriction either as juveniles (1–2 years, juvenile onset CR or JO-CR) or late in life (>15 years, old onset or OO-CR) to the adult (adolescent) cohort (3–5 yr at onset) on measures of T cell senescence. Our results strongly suggest that adulthood onset CR improved T cell function in RM while CR started during early years of development led to accelerated T cell senescence. Initiation of CR in the advanced age did not have any beneficial effects upon T-cell senescence, and, by one parameter, was shown to potentially further erode T-cell proliferative capacity. We conclude that there is an optimal window in the course of which CR interventions can retard aging of the immune system.
RESULTS
Early onset of caloric restriction leads to accelerated loss of naïve T cells
Our prior studies showed that CR initiated during early adulthood can significantly delay the age-related loss of naïve T cells (Messaoudi, Warner et al. 2006). To determine the impact of age at onset of CR on T cell homeostasis and subset distribution, we measured the frequency of naïve, central memory (CM) and effector memory (EM) T cells in peripheral blood mononuclear cells (PBMC) isolated from animals that started calorie restriction either before puberty (JO-CR) or at an advanced age (OO-CR). These subsets were defined based on the expression of CD28 and CD95 as described previously (Pitcher, Hagen et al. 2002): Naïve T cells are CD28intCD95lo, CM T cells are CD28hiCD95hi, and EM T cells are CD28negCD95hi. We and others have shown that advanced age in humans and nonhuman primates results in loss of naïve T cells from >40% to <20% of total circulating T cells (Wikby, Maxson et al. 1998; Jankovic, Messaoudi et al. 2003; Cicin-Sain, Messaoudi et al. 2007). This loss is accompanied by an accumulation of EM T cells especially in the CD8 compartment (Jankovic, Messaoudi et al. 2003; Czesnikiewicz-Guzik, Lee et al. 2008). In the experiments described below, we used the frequency of naïve and EM T cells as a correlate for the severity of T-cell immune senescence.
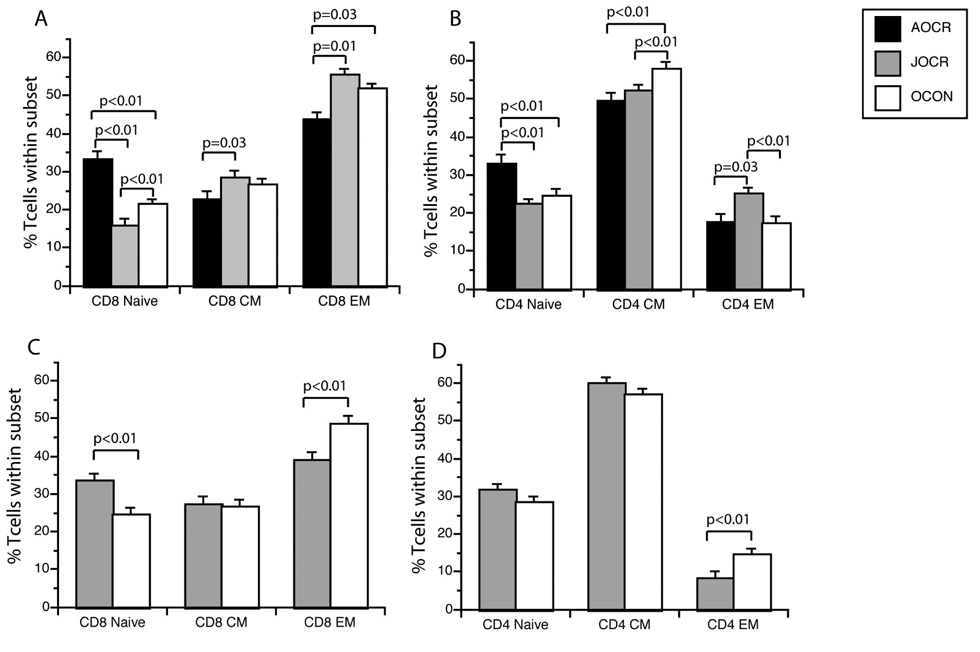
Our analysis revealed that juvenile onset of CR (JO-CR) in male RM resulted in a dramatic reduction in the frequency of circulating CD8 naïve T cells and a modest decrease in the frequency of naive CD4 T cells (Fig 1A and B) compared to age-matched controls. Although the decrease in the frequency of CD4 naïve T cells in JO-CR male RM was not considerable, a statistically significant increase in the frequency of EM T cells in both the CD8 and CD4 subsets was detected. We previously reported that, in contrast to CD8 T cells, age-related loss of naïve CD4 T cells results in an accumulation of CM and not EM cells (Jankovic, Messaoudi et al. 2003; Cicin-Sain, Messaoudi et al. 2007). Because EM cells are considered to be closer to terminal differentiation (Geginat, Lanzavecchia et al. 2003), the increase in EM CD4 T cells in JO-CR male RM instead of the typical increase in CM cells could suggest an accelerated rate of T cell senescence in these animals.
Figure 1. Phenotypic changes in aged male and female RM T cell subset distribution as a consequence of CR.
(A and B) Percentages of naïve, CM and EM subsets in CD4 and CD8 T cells found in peripheral blood in JO-CR, AO-CR and age-matched control male RM. JO-CR results in accelerated loss of naïve CD8 T cells, and the accumulation of EM CD4 and CD8 T cells. (C and D) Percentages of naïve, CM and EM CD4 and CD8 T cell subsets in JO-CR and age-matched control female RM. Data from AO-CR cohort was not included for comparison because the animals within that cohort are 5 years older than the animals within the JO-CR cohort. JO-CR resulted in a decrease in EM T cells in both CD4 and CD8 subsets, but a significant increase in naive T cells was only observed in CD8 T cells. For all panels, mean values are shown for each group at four time points over a 42 month span. Statistical analysis was carried out using the mixed-effects model and significance is denoted by two-sided P values above the bars.
It is also important to stress that JO-CR did not alter numbers of circulating total lymphocytes based on complete blood counts (Table 1). Thus, we can conclude that in male RM JO-CR led to accumulation of EM T cells at the expense of naive T cells, thereby increasing the rate of T cell senescence. These results contrast with the improved maintenance of naïve T cells induced by adult onset CR (AO-CR) (Fig. 1A and B and (Messaoudi, Warner et al. 2006)) and strongly suggest that early onset of CR negatively impacts T cell aging in this nonhuman primate species.
Table 1.
Animal groups, ages and hematological analysis for the number of white blood cells (WBC), lymphocytes (LYM) and neutrophils by animal group.
| Group | No of animals | Age, yr | WBC | LYM | NE |
|---|---|---|---|---|---|
| Males | |||||
| JO-CR | 8 | 19–23 | 4.93±1.8 | 1.71±0.44 | 2.38±0.98 |
| O-CON | 18 | 19–23 | 5.09±1.67 | 1.99±0.40 | 2.46±0.86 |
| OO-CR | 6 | 36–42 | 5.21±2.45 | 3.42±0.48 | 1.82±2.28 |
| OO-CON | 6 | 36–38 | 10.93±2.08 | 2.56±0.52 | 4.45±1.06 |
| Females | |||||
| JO-CR | 8 | 16–18 | 5.28±2.16 | 1.75±0.45 | 2.93±1.12 |
| JO-CON (F) | 7 | 16–18 | 4.97±2.33 | 1.60±0.48 | 2.90±1.19 |
In contrast to the results described above, JO-CR in female RM resulted in decreased numbers of EM CD8 and CD4 T cells, but a significant increase in the number of naïve T cells was observed in only the CD8 subset. This difference in JO-CR outcome between the male and female cohort could be due to gender-based differences in response to CR. However given that AO-CR exerted similar benefits in both males and females (Messaoudi, Warner et al. 2006), it is possible that the differences in outcome are due to the fact that JO-CR females were 5 years younger than the male JO-CR group at the time of tissue collection. However, a better understanding of the mechanisms underlying the different outcomes of JO-CR between male and female RM requires further studies.
Old onset CR (OO-CR) did not result in any changes in subset distribution in either CD4 or CD8 T cells (Supplemental Fig. 1). However, OO-CR animals exhibited a reduced number of circulating white blood cells compared to age-matched controls, mediated mostly by a lower number of neutrophils (Table 1). Given that the number of circulating neutrophils was higher in the very old control animals (OO-CON, 35–38 yr of age) compared to O-CON (19–23 yr of age; designations of OO-CON and O-CON are used to highlight that there is a marked difference in ages between these two control groups of animals), it is unclear whether the CR-mediated loss of neutrophils may be detrimental or beneficial.
Taken together, these data strongly suggest that JO-CR and OO-CR in male nonhuman primates accelerate T cell senescence. JO-CR in females, on the other hand, might exert beneficial effects, however, a fully accurate interpretation of JO-CR impact in this group will have to await until these animals reach at least 21–23 years of age.
Reduction in T cell repertoire diversity with JO-CR
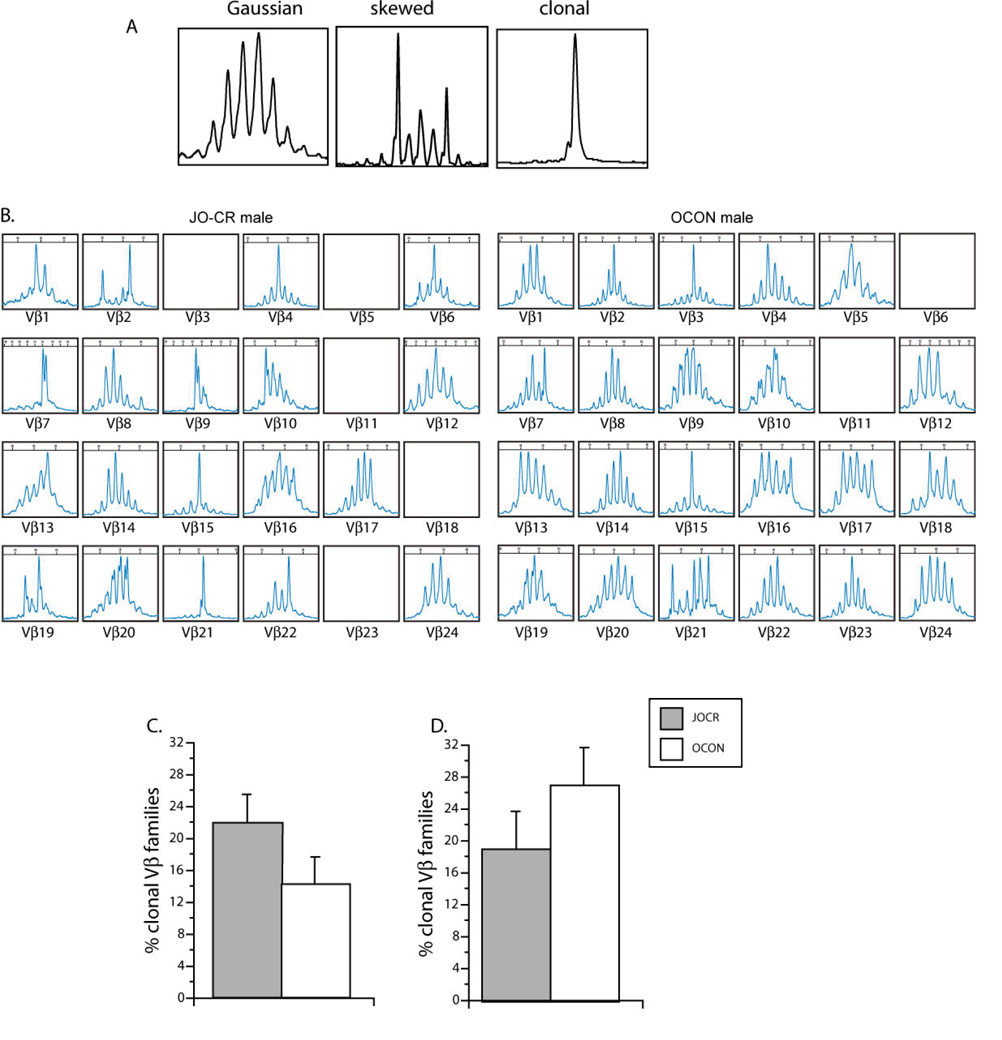
Loss of naïve T cells due to advanced age or lymphopenia results in decreased T cell repertoire diversity (Messaoudi, Lemaoult et al. 2004; Messaoudi, Warner et al. 2006; Weyand and Goronzy 2006). To directly test whether the changes in naïve T cell frequencies described above impacted T cell repertoire diversity, we measured TCRβ chain CDR3 length polymorphism (Pannetier, Cochet et al. 1993) as described previously (LeMaoult, Messaoudi et al. 2000; Messaoudi, Warner et al. 2006). A diverse CDR3 profile is characterized with a Gaussian distribution of CDR3 sizes. With age or during infection, this distribution is often disturbed and skewed profiles marked by a dominant CDR3 length are frequently detected. In some extreme cases the Vβ family is dominated by a clonotypic expansion, which can be detected as a single dominant peak (Fig. 2A). Frequency of T cell clonal expansions (TCE) steadily increases with age and can be used to measure the extent of T cell senescence (Callahan, Kappler et al. 1993; Posnett, Sinha et al. 1994; Schwab, Szabo et al. 1997; LeMaoult, Messaoudi et al. 2000).
Figure 2. TCR repertoire analysis of T cell obtained from JO-CR and CON RM.
(A) representative examples of Gaussian (left), skewed (middle) and clonal (right) CDR3 size distribution. (B) representative examples of CDR3 length polymorphism repertoires from a JO-CR male and a OCON male RM. (C, D) Prevalence of T cell clonal expansion (TCE) in PBMC isolated from JO-CR and control male (B) and female (C) RM was calculated as described in materials and methods. Although differences do not reach statistical significance, there is increased TCE incidence in JO-CR males in agreement with reduction in prevalence of naïve T cells. On the other hand, JO-CR led to a decrease in TCE incidence in female RM in agreement with decreased number of EM T cells.
To assess the impact of JO-CR or OO-CR on T cell repertoire diversity in this current study, we measured the frequency of TCE in PBMC. JO-CR resulted in decreased repertoire diversity and increased prevalence of clonal expansions in male RM (Fig 2 B). Although the differences observed were not statistically significant, they were in line with the observation that JO-CR led to an increase in EM CD4 and CD8 subsets. In females JO-CR led to an increase in TCRβ CDR3 size diversity, which, although not statistically significant, corresponded to the increase in naive CD8 T cells and decreases in CD8 and CD4 EM T cells observed in these animals (Fig 2C). No change in repertoire diversity was observed when CR was initiated late in life. This finding was not surprising since OO-CR did not affect frequency of naïve and memory T cell subsets between OO-CR and control animals.
JO-CR increases the frequency of T cells secreting proinflammatory cytokines
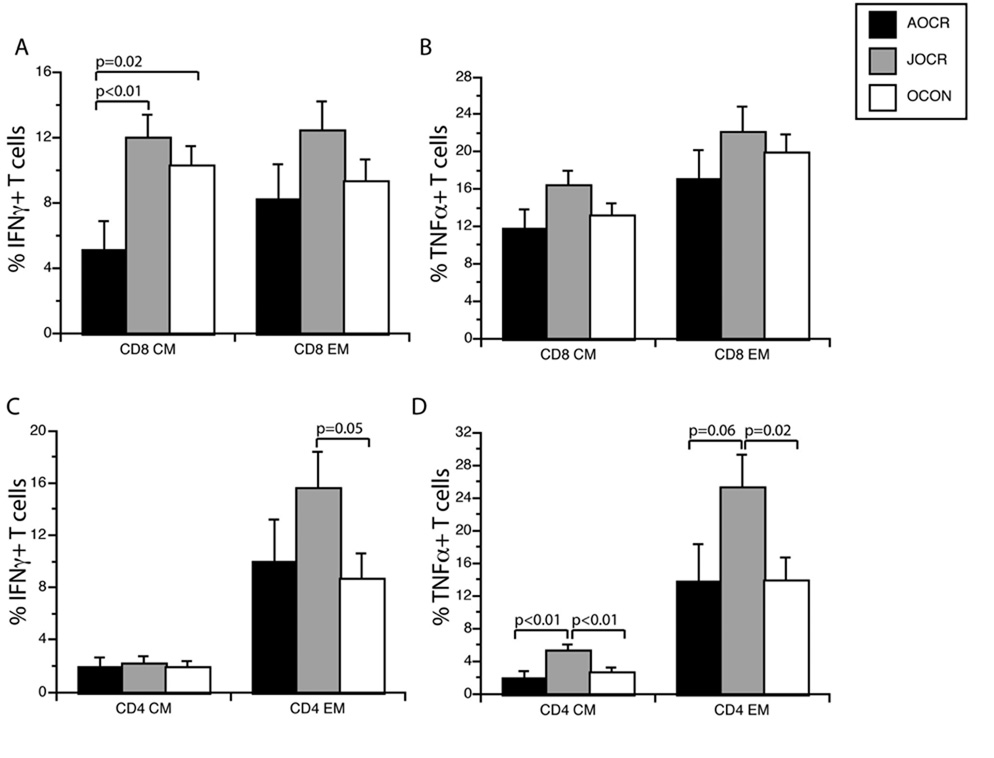
Age-related accumulation of memory T cells in rodents (Ernst, Weigle et al. 1993), humans (McNerlan, Rea et al. 2002; Zanni, Vescovini et al. 2003) and RM (Jankovic, Messaoudi et al. 2003; Messaoudi, Warner et al. 2006) correlates to an increase in proinflammatory cytokines, which represents another hallmark of immune senescence. This state has been labeled “inflamm-aging”, and has been speculated to contribute significantly to several age-related morbidities such as osteoporosis, sarcopenia, Atherosclerosis, and certain types of cancer (De Martinis, Franceschi et al. 2005; Wikby, Nilsson et al. 2006; Vasto, Candore et al. 2007). We recently showed that adult onset CR decreased the number of CM and EM T cells that secreted the inflammatory cytokines IFNγ and TNFα following polyclonal stimulation (Fig 3A–D and (Messaoudi, Warner et al. 2006)). To determine how age at onset of CR impacted the frequency of inflammatory cytokine-secreting T cells, we measured the frequency of IFNγ and TNFα secreting T cells following a brief (6 hr.) in vitro stimulation with anti CD3 as previously described (Jankovic, Messaoudi et al. 2003). Cells were then stained with anti CD8, CD4, CD28 and CD95 to delineate naïve and memory T cell subsets. Subsequently, cells were fixed, permeabilized and stained with anti IFNγ and TNFα antibodies.
Figure 3. Production of pro-inflammatory cytokines TNFα and IFNγ by T cell subsets isolated from CR and control male RM.
(A, B) percentage of CM and EM CD8 T cells that secrete IFNγ (A) or TNFα (B) in response to a 6 hr. in vitro stimulation with anti-CD3. In contrast to AO-CR, JO-CR results in increased prevalence of inflammatory cytokine-secreting memory T cells. (C, D) Percentage of CM and EM CD4 T cells that secrete IFNγ (C) or TNFα (D) in response to anti CD3 stimulation. JO-CR results in increased frequency of inflammatory cytokine-secreting CD4 T cells as well.
Our data show that in contrast to AO-CR, JO-CR led to a significant increase in the number of CD4 CM secreting TNF a and EM CD4 T cells secreting IFNγ or TNFα. A similar trend was observed for the CD8 subset but only reached significance for the CD8 CM T cells secreting IFNγ. Since JO-CR in male monkeys also resulted in an increase in the frequency of CD4 EM and CM cells, these data strongly suggest that the overall frequency of T cells that can contribute to the inflammatory milieu is significantly higher in JO-CR male RM animals compared with controls. Interestingly, JO-CR also led to an increase in the numbers of IFNγ or TNFα secreting T cells, in female JO-CR RM (supplemental Fig.2). This trend was statistically significant for the CD4 CM T cell secreting TNFα. While these differences did not always reach significance, a clear trend was easily detectable (Suppl. Fig. 2). Finally, we detected no differences in the frequency of IFNγ or TNFα secreting T cells between OO-CR animals and their age-matched controls (data not shown).
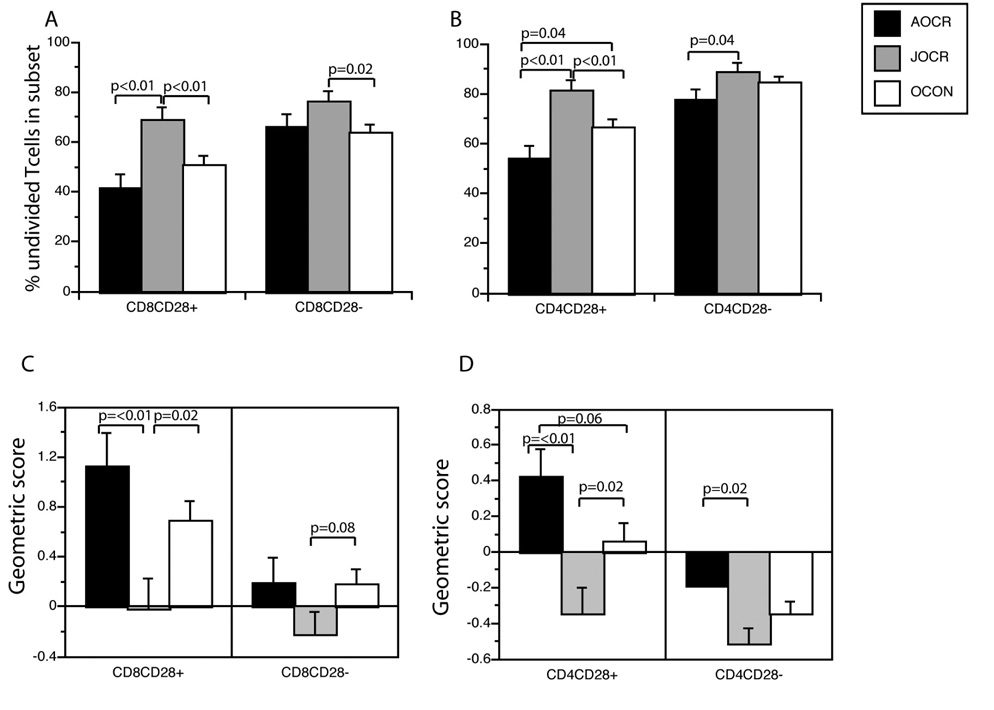
JO-CR leads to loss of proliferative potential in T-cells
Accumulation of EM T cells in the course of aging is often accompanied by a loss in proliferative potential in the T cell compartment. We previously showed that AO-CR maintained the proliferative capacity of T cells in aged animals compared to controls (Messaoudi, Warner et al. 2006) as judged by a fraction of T-cells that remained undivided upon TCR/CD3 stimulation. Furthermore, T cells from AO-CR animal underwent higher number of divisions than T cells from control animals. To examine the impact of age at CR onset upon proliferative potential of circulating lymphocytes, PBMC were labeled with CFSE, stimulated with an agonistic antibody against TCR/CD3 and cultured for four days (Jankovic, Messaoudi et al. 2003).
Our studies revealed that in male RM, JO-CR significantly reduced the number of dividing T cells as measured by the number of cells that remained undivided (CFSEhi) after four days of stimulation compared to both controls and AO-CR animals (Fig. 4A, B). This observation was true for both CD4 and CD8 T cells and especially for the CD28+ subsets. Furthermore, we determined a geometric division score that is derived from the percentage of the cells in each division and gives more weight to cells that have undergone multiple rounds of division. T cells from AO-CR animals have a positive geometric score indicative of a significant percentage of cells that underwent several (>3) rounds of proliferation (Fig. 4C, D). T cells from JO-CR animals on the other hand, had negative scores since most of the dividing cells remained in the first division.
Figure 4. Proliferation of T cells isolated from CR and control male RM.
(A, B) Percentage of CD8 (A) and CD4 (B) T cells that remained undivided as defined by CFSEhi after 4 days of stimulation with immobilized anti-CD3. In contrast to AO-CR, JO-CR results in loss of proliferative capacity indicated by a higher proportion of CD8 and CD4 that remain undivided especially in the CD28+ subset. (C, D) Geometric score of T cell divisions was calculated for CD8 (C) and CD4 (D) subsets as described in materials and methods section. This analysis gives increased weight to later divisions. JO-CR severely limits T cells ability to undergo multiple rounds of divisions.
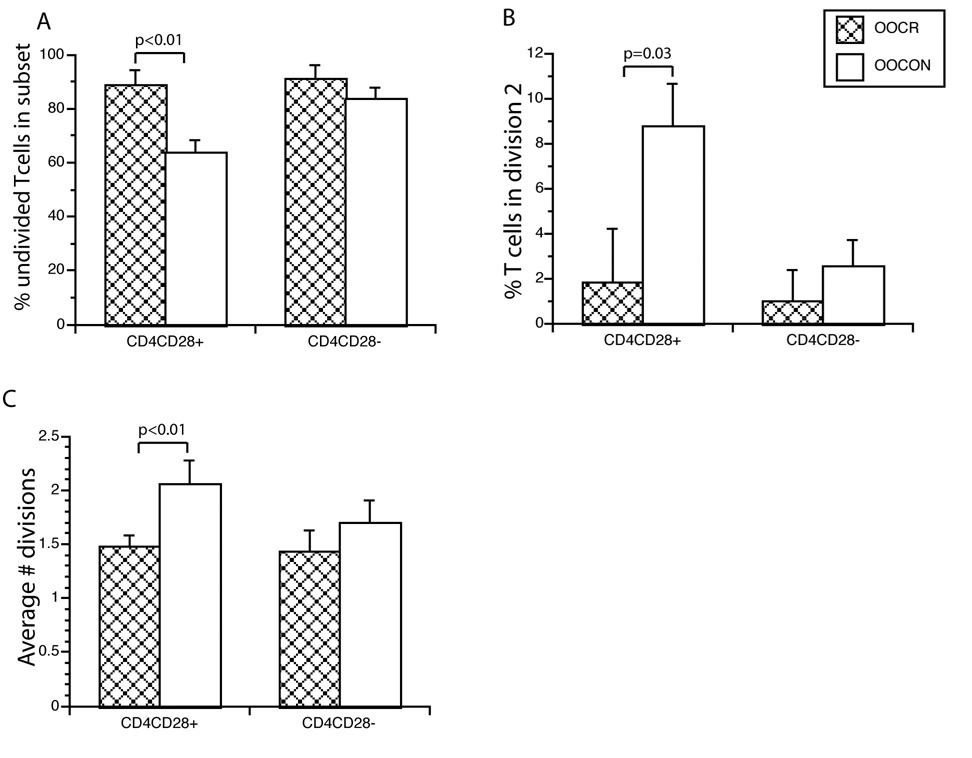
Surprisingly, there was no difference in the number of proliferating T cells between JO-CR and control females (Supplemental Fig. 3). This result was unexpected given the increase in naïve CD8 T cells and decrease in EM T cells detected in JO-CR females, and suggest that proliferative (and perhaps other) function of naïve T cells might be altered in JO-CR females. Even more surprisingly, OO-CR resulted in decreased T cell proliferation potential of the CD4+CD28+ subset in male RM. This is evident in the number of cells that remained undivided (Fig. 5A), the percentage of cells that underwent two divisions (Fig 5B) as well as the average number of divisions they underwent (Fig 5C). These data suggest that OO-CR can negatively impact T cell function in the absence of any overt phenotypic changes.
Figure 5. Proliferation of T cells isolated from OO-CR and control animals.
OO-CR leads to a diminished proliferative capacity in the absence of overt phenotypic changes in T cell subsets as evidence by a higher percentages of CD4+CD8+ T cells that remained undivided (A), a lower percentage of cells that underwent at least two divisions (B) and a decreased average number of divisions (C). Similar differences were detected for the CD8 subset but did not reach statistical significance.
DISCUSSION
Caloric restriction (CR) remains the only intervention that consistently increases median and maximal life spans in short-lived mammals. While the exact mechanisms by which CR exerts its effects are not completely understood, the consensus in the field is that CR reduces the intrinsic rate of aging (Bishop and Guarente 2007) and prevents several age-related diseases, including cancer and cardiovascular disorders. Moreover, CR protects against diabetes, autoimmunity, and neurodegenerative disorders. If these benefits translated to humans, they would not only lead to an extension in life span but perhaps more importantly to an improvement in the quality in life. Since long-term CR studies in humans are burdened with ethical, logistical and temporal difficulties, the long-term CR studies of nonhuman primates (rhesus macaques, RM) of both sexes and various ages have been invaluable. So far the data from these studies suggest that CR leads to similar physiological benefits in nonhuman primates as rodents (Mattison, Roth et al. 2007) including improvement in the homeostasis and function of the T-cell arm of the immune system (Messaoudi, Warner et al. 2006)
In this study, we examined the impact of the age at onset of CR on T cell homeostasis and function in male and female rhesus macaques. Our data show that juvenile onset CR (JO-CR) is associated with accelerated loss of naive T cells and accumulation of EM T cells in male RM. Moreover, JO-CR was associated with decreased T cell repertoire diversity and an increase in frequency in T cell clonal expansions, which we previously showed to be a predisposing factor for reduced immune response to infection (Messaoudi, Lemaoult et al. 2004). These outcomes are in contrast to the beneficial effects exerted by CR when initiated during early adulthood. The accumulation of EM (CD28neg) T cells is a predictor of poor immune competence in old age (reviewed in (Vallejo 2005)) and could also contribute to age-related co-morbidities. EM CD8 T cells have little proliferative capacity (Posnett, Edinger et al. 1999; Bandres, Merino et al. 2000; Zhang, Fujii et al. 2002), along with shortened telomeres (Effros, Dagarag et al. 2005) and are resistant to apoptosis (Vallejo, Nestel et al. 1998; Spaulding, Guo et al. 1999). These cells secrete large quantities of inflammatory cytokines, allowing them to potentially participate in immune pathology (Posnett, Edinger et al. 1999; Bandres, Merino et al. 2000; Zhang, Fujii et al. 2002). They were reported to correlate with poor generation of protective immune responses following vaccination (Saurwein-Teissl, Lung et al. 2002) and were speculated to even interfere with such responses (Effros 1998; Goronzy, Fulbright et al. 2001; Saurwein-Teissl, Lung et al. 2002). Indeed, in the RM male cohorts, and in accordance with our finding that JO-CR lead to an accumulation of EM T cells, we found an increase in the frequency of CD8 and CD4 T cells that secrete IFNγ and TNFα following polyclonal stimulation compared to controls. More importantly, JO-CR in male RM led to an increase of the prevalence of proinflammatory cytokine-secreting cells within both the EM and CM subsets. Finally, CR was previously shown to maintain T cell proliferative capacity in rodents (Wolf, Penn et al. 1995; Spaulding, Walford et al. 1997; Hursting, Lavigne et al. 2003), and we showed that early adult onset CR maintains T cell ability to undergo cell divisions in nonhuman primates (Messaoudi, Warner et al. 2006). Again, JO-CR showed deleterious effects in the male RM cohort, reducing T cell proliferative capacity. Overall, by any measure taken, the immune system of male RM placed on CR in the juvenile period exhibited signs of exacerbated, rather than retarded and reduced, aging.
The situation was somewhat different in female RM. In these animals, JO-CR decreased the prevalence of CD4 and CD8 EM T cells and significantly increased representation of naive cells in the CD8 compartment. The difference in JO-CR impact on memory T cell frequency between male and female RM could be a result of genuine gender differences in immune system homeostasis during aging or, perhaps more trivially, the fact that the female cohort was, on average, 5 years younger than the males at the time of sample collection. Therefore, loss of naïve T cells could be more pronounced between 15 and 20 years of age and it is possible that in five years the JO-CR females would experience a more rapid loss of naive T cells than age-matched controls. It is worth noting that JO-CR resulted in a more significant delay in skeletal muscle development and weight gain in males than females (Lane, Ingram et al. 1999). This delay in development was accompanied with a more pronounced reduction in abdominal trunk fat with males experiencing a three-fold decrease whereas females experience only a two-fold decrease compared to controls (Lane, Ingram et al. 1999). Such gender-specific differences in response to CR could impact lymphopoeisis, lymphocyte homeostasis and function as well.
More importantly, however, while phenotypic changes (increase in CD8 naïve T cells) may suggest that JO-CR could be somewhat beneficial for the female CD8 T-cells, by functional criteria the treatment had detrimental or neutral effects. Specifically, female RM subject to JO-CR displayed a trend of increased frequency of IFNγ and TNFα secreting T cells, suggesting that the pro-inflammatory propensity of old T-cells was not alleviated by CR under these conditions. Furthermore, female RM on JO-CR showed no benefit from CR when proliferative responses were measured. These results highlight the importance of measuring multiple phenotypic and functional parameters when evaluating and interpreting the impact of an intervention on immune senescence. Taken together, our data strongly suggest that JO-CR has the potential to increase inflamm-aging in both sexes.
The most significant features observed in the T-cells of OO-CR monkeys were lymphopenia and decreased T-cell proliferative capacity. Other measurements in this cohort also revealed trends towards worsening of immune phenotype and function, but with no significant differences. We conclude that CR initiated at advanced age has no benefit for the composition of peripheral T-cell pool and function of primate T-cells, and that our results suggest that the latter may be adversely affected. Given that nutritional stress of CR is likely to have other unwanted effects upon the physiology of old primates (D. Ingram and J. Mattison, unpublished observations), these results at a minimum urge caution in initiating late-life CR.
It is of interest to contrast our observations to those obtained from rodent studies, where a 30% to 60% reduction in caloric intake early in life (shortly after weaning to 6 months of age) caused a proportionate increase in life span and improved several aspects of immune functions (Weindruch, Kristie et al. 1982). These divergent observations may be reconciled in light of the recently published findings which showed that mice calorically restricted shortly after weaning were at increased risk from severe disease following bacterial or viral challenge compared to control animals (Sun, Muthukumar et al. 2001; Gardner 2005; Kristan 2007). A potential complicating factor in interpreting results of these studies is that the disease induced by pathogens studied led to weight loss, and it is well known that the animals on CR already have depleted excess weight and fat reserves. However, another explanation is that CR initiated very early in life (shortly after weaning) is detrimental to immune function, despite phenotypic changes (such as increased percentage of naïve T cells), which would be consistent with findings presented above.
In summary, our results show that adulthood onset of CR in a nonhuman primate shows uniquely beneficial impact upon homeostasis and function of the T-cell compartment, suggesting the existence of an optimal window for CR efficacy. Additional studies will be required to evaluate the relative importance of these benefits and weigh them against the increase in life span and improved function of other organs or systems.
EXPERIMENTAL PROCEDURES
Animal groups
Experimental groups consisted of control (CON) and calorically restricted CR rhesus macaques (RM) of both sexes, listed in Table 1. All animals were kept in conventional housing and were positive for Herpes B and Rhesus Cytomegalovirus. There were no indications that any of the groups had distinct exposure to viral or other pathogens.
Some of the animals were calorically restricted before puberty (1–2 years of age, juvenile onset, JO-CR) or at advanced age (>15 years, old onset, OO-CR). Male RM within the JO-CR group were 19–23 years of age during the completion of these studies. These animals were age-matched to the cohort of adult onset CR (AO-CR) animals that we recently described (Messaoudi, Warner et al. 2006). Therefore we were able to directly compare the impact of the age at onset between all three groups of animals: CON, AO-CR and JO-CR males.
JO-CR females were 17–18 years of age at the completion of the studies. We could not therefore directly compare the recently published impact of AO-CR (Messaoudi, Warner et al. 2006) to that of JO-CR on T cell function in female RM in this study since the AO-CR cohort was 21–23 years of age. Therefore, we compared female JO-CR only to age-matched female controls. Only male RM were available for the old onset group (OO-CR). The animals were 35–38 years old and 36–40 years old for the OO-CON and OO-CR groups, respectively.
T cell phenotype
T cell phenotype was determined using flow cytometry (FCM), as previously described (Messaoudi, Warner et al. 2006). CD8β antibody was purchased from Beckman Coulter. All remaining antibodies were purchased from BD-Pharmingen (San Diego, CA). Samples were acquired using the LSRII cytometer equipped with DiVa 5.0 software (Beckton Dickinson, San Jose, CA) and analyzed using FlowJo (TreeStar, Ashland, OR). A minimum of 106 events were collected for each sample, lymphocyte gate positioned on small/medium lymphocytes using forward and orthogonal scatter, and single-color compensation performed per manufacturer’s instructions. Naïve (N), central memory (CM) and effector/effector memory (EM) populations were defined using a combination of CD28 and CD95, as originally validated by Pitcher et al.(Pitcher, Hagen et al. 2002). Cells with fluorescence above that of the highest fluorescence intensity of the control samples were denoted positive for a given marker.
T cell repertoire analysis
Analysis of complementary determining region 3 (CDR3) length polymorphism was carried out exactly as described in (Messaoudi, Warner et al. 2006). Briefly, RNA was isolated from 3 to5 ×106 PBMC using RNA isolator (Sigma), and was used to generate cDNA following reverse transcription. PCR conditions, runoff labeling procedure and all primers were previously published (Messaoudi, Warner et al. 2006).
Intracellular cytokine staining
PBMC were stimulated with soluble RM-specific anti-CD3 mAb (clone FN18, Biosource, Invitrogen), as well as with anti-human CD28 and CD49d (Pharmingen) for 6 hr. Brefeldin A was added for the last 5 hr to block cytokine secretion. At the end of the incubation, PBMC were stained with surface antibodies CD8, CD8, CD28 and CD95. The cells were then fixed and permeabilized using a kit from Pharmingen as per manufacturer’s recommendation. Finally, the cells were stained with antibodies against IFNγ and TNFα, and analyzed by FCM as above. PBMC stimulate with anti-human CD28 and CD49d (Pharmingen) for 6 hr were used as negative controls.
T cell Proliferation assay
Details of this assay were described elsewhere (Jankovic, Messaoudi et al. 2003; Messaoudi, Warner et al. 2006). Briefly, PBMC were labeled with CFSE then plated in the presence of plate bound anti-CD3 for 96 hr, stained with CD8, CD4 and CD28 and analyzed as above. We measured both the percentage of cells that remain undivided (CFSEhi), as well as the number of divisions based on CFSE dilutions. In addition we calculated a geometric score of division as follows: G_score= (D1+D2×2+D3×4+D4×8+D5×16+D6×32-Undivided)/100. This calculation gives increasing weight as the cells undergo an increasing number of divisions.
Statistical analysis
Data were analyzed as described in our recent manuscript (Messaoudi, Warner et al. 2006). Mixed effects model was used to analyze the data and to account for observations on successive occasions in time (no more than 7 month intervals over a period of three years) and for animal-to-animal variation. Analysis of variance (ANOVA) and contrast tests were used to address the questions of interest.
Supplementary Material
Acknowledgments
Supported in part by the USPHS Awards AG21384 (to J. N-Z.), 5T32 AI007472-10 (I.M.) and RR0163 (to the ONPRC) from the National Institute on Aging, National Institute of Allergy and Infectious Diseases and the National Institute for Research Resources, respectively, as well as by the NIA Intramural Program, NIH.
Authors wish to express appreciation for the work and dedication of April Hobbs and Ed Tilmont (NIA Intramural Research Program, Poolesville, MD) as well as to Drs. Doug Powell and Rick Herbert (Veterinary Research Program, NIH at Poolesville, MD) and Drs. Frank Kogler, Mary Zelinski, Theodore Hobbs, Jennifer Wilk and Anne Lewis and Ms. (Oregon National Primate Research Center, Beaverton, OR) for the complex coordination of experiments, veterinary care of the monkeys in this study and for collection of the specimens. We in particular wish to acknowledge and remember the outstanding surgical work and the friendship and the dedication of the late Dr. John Fanton (ONPRC).
ABBREVIATIONS
- AO-CR
adult onset caloric restriction, at 3–5 yr of rhesus macaque life
- CR
caloric restriction
- CM
central memory T-cells
- EM
effector/effector memory T-cells
- FCM
flow cytofluorometry
- JO-CR
juvenile onset CR, at 1–2 yr of age
- N
naïve T-cells
- OO-CR
old onset CR, started> 17 yr of age
- RM
rhesus macaque
- TCE
T-cell clonal expansions
- TCR
T-cell receptor
REFERENCES
- Bandres E, Merino J, et al. The increase of IFN-gamma production through aging correlates with the expanded CD8(+high)CD28(−)CD57(+) subpopulation. Clin Immunol. 2000;96(3):230–235. doi: 10.1006/clim.2000.4894. [DOI] [PubMed] [Google Scholar]
- Bishop NA, Guarente L. Genetic links between diet and lifespan: shared mechanisms from yeast to humans. Nat Rev Genet. 2007;8(11):835–844. doi: 10.1038/nrg2188. [DOI] [PubMed] [Google Scholar]
- Callahan JE, Kappler JW, et al. Unexpected expansions of CD8-bearing cells in old mice. J. Immunol. 1993;151:6657–6669. [PubMed] [Google Scholar]
- Cefalu WT, Wagner JD, et al. Influence of caloric restriction on the development of atherosclerosis in nonhuman primates: progress to date. Toxicol Sci. 1999;52(2 Suppl):49–55. doi: 10.1093/toxsci/52.2.49. [DOI] [PubMed] [Google Scholar]
- Cicin-Sain L, Messaoudi I, et al. Dramatic increase in naive T cell turnover is linked to loss of naive T cells from old primates. Proc Natl Acad Sci U S A. 2007;104:19960–19965. doi: 10.1073/pnas.0705905104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clambey ET, Kappler JW, et al. CD8 T cell clonal expansions & aging: A heterogeneous phenomenon with a common outcome. Experimental Gerontology. 2007;42(5):407–411. doi: 10.1016/j.exger.2006.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czesnikiewicz-Guzik M, Lee WW, et al. T cell subset-specific susceptibility to aging. Clin Immunol. 2008 doi: 10.1016/j.clim.2007.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Martinis M, Franceschi C, et al. Inflamm-ageing and lifelong antigenic load as major determinants of ageing rate and longevity. FEBS Lett. 2005;579(10):2035–2039. doi: 10.1016/j.febslet.2005.02.055. [DOI] [PubMed] [Google Scholar]
- Edwards IJ, Rudel LL, et al. Caloric restriction in rhesus monkeys reduces low density lipoprotein interaction with arterial proteoglycans. J Gerontol A Biol Sci Med Sci. 1998;53(6):B443–B448. doi: 10.1093/gerona/53a.6.b443. [DOI] [PubMed] [Google Scholar]
- Effros RB. Replicative senescence: impact on T cell immunity in the elderly. Aging (Milano) 1998;10(2):152. [PubMed] [Google Scholar]
- Effros RB, Dagarag M, et al. The role of CD8+ T-cell replicative senescence in human aging. Immunol Rev. 2005;205:147–157. doi: 10.1111/j.0105-2896.2005.00259.x. [DOI] [PubMed] [Google Scholar]
- Effros RB, Svoboda K, et al. Influence of age and caloric restriction on macrophage IL-6 and TNF production. Lymphokine Cytokine Res. 1991;10(5):347–351. [PubMed] [Google Scholar]
- Ernst DN, Weigle WO, et al. The age-associated increase in IFN-gamma synthesis by mouse CD8+ T cells correlates with shifts in the frequencies of cell subsets defined by membrane CD44, CD45RB, 3G11, and MEL-14 expression. J Immunol. 1993;151(2):575–587. [PubMed] [Google Scholar]
- Ershler WB, Keller ET. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu Rev Med. 2000;51:245–270. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- Gardner EM. Caloric restriction decreases survival of aged mice in response to primary influenza infection. J Gerontol A Biol Sci Med Sci. 2005;60(6):688–694. doi: 10.1093/gerona/60.6.688. [DOI] [PubMed] [Google Scholar]
- Geginat J, Lanzavecchia A, et al. Proliferation and differentiation potential of human CD8+ memory T-cell subsets in response to antigen or homeostatic cytokines. Blood. 2003;101(11):4260–4266. doi: 10.1182/blood-2002-11-3577. [DOI] [PubMed] [Google Scholar]
- Goronzy J, Fulbright J, et al. Value of immunological markers in predicting responsiveness to influenza vaccination in elderly individuals. J. Virol. 2001;75:12182–12187. doi: 10.1128/JVI.75.24.12182-12187.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossmann A, Rabinovitch PS, et al. Influence of age, sex, and dietary restriction on intracellular free calcium responses of CD4+ lymphocytes in rhesus monkeys (Macaca mulatta) J Cell Physiol. 1995;162(2):298–303. doi: 10.1002/jcp.1041620216. [DOI] [PubMed] [Google Scholar]
- Gruver AL, Hudson LL, et al. Immunosenescence of ageing. J Pathol. 2007;211(2):144–156. doi: 10.1002/path.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Htwe TH, Mushtaq A, et al. Infection in the Elderly. Infectious Disease Clinics of North America. 2007;21(3):711–743. doi: 10.1016/j.idc.2007.07.006. [DOI] [PubMed] [Google Scholar]
- Hursting SD, Lavigne JA, et al. Calorie restriction, aging, and cancer prevention: mechanisms of action and applicability to humans. Annu Rev Med. 2003;54:131–152. doi: 10.1146/annurev.med.54.101601.152156. [DOI] [PubMed] [Google Scholar]
- Jankovic V, Messaoudi I, et al. Phenotypic and functional T-cell aging in rhesus macaques (Macaca mulatta): differential behavior of CD4 and CD8 subsets. Blood. 2003;102(9):3244–3251. doi: 10.1182/blood-2003-03-0927. [DOI] [PubMed] [Google Scholar]
- Johnson SA, Cambier JC. Ageing, autoimmunity and arthritis: senescence of the B cell compartment - implications for humoral immunity. Arthritis Res Ther. 2004;6(4):131–139. doi: 10.1186/ar1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemnitz JW, Weindruch R, et al. Dietary restriction of adult male rhesus monkeys: design, methodology, and preliminary findings from the first year of study. J Gerontol. 1993;48(1):B17–B26. doi: 10.1093/geronj/48.1.b17. [DOI] [PubMed] [Google Scholar]
- Kristan DM. Chronic calorie restriction increases susceptibility of laboratory mice (Mus musculus) to a primary intestinal parasite infection. Aging Cell. 2007;6(6):817–825. doi: 10.1111/j.1474-9726.2007.00345.x. [DOI] [PubMed] [Google Scholar]
- Lane MA, Black A, et al. Caloric restriction in primates. Ann N Y Acad Sci. 2001;928:287–285. doi: 10.1111/j.1749-6632.2001.tb05658.x. [DOI] [PubMed] [Google Scholar]
- Lane MA, Ingram DK, et al. Nutritional modulation of aging in nonhuman primates. J Nutr Health Aging. 1999;3(2):69–76. [PubMed] [Google Scholar]
- LeMaoult J, Messaoudi I, et al. Age-related dysregulation in CD8 T cell homeostasis: kinetics of a diversity loss. J. Immunol. 2000;165:2367–2373. doi: 10.4049/jimmunol.165.5.2367. [DOI] [PubMed] [Google Scholar]
- Liang SY, Mackowiak PA. Infections in the Elderly. Clinics in Geriatric Medicine. 2007;23(2):441–456. doi: 10.1016/j.cger.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Masoro EJ. Subfield history: caloric restriction, slowing aging, and extending life. Sci Aging Knowledge Environ. 2003;2003(8) doi: 10.1126/sageke.2003.8.re2. RE2. [DOI] [PubMed] [Google Scholar]
- Masoro EJ. Role of sirtuin proteins in life extension by caloric restriction. Mech Ageing Dev. 2004;125(9):591–594. doi: 10.1016/j.mad.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Mattison JA, Roth GS, et al. Dietary restriction in aging nonhuman primates. Interdiscip Top Gerontol. 2007;35:137–158. doi: 10.1159/000096560. [DOI] [PubMed] [Google Scholar]
- McNerlan SE, Rea IM, et al. A whole blood method for measurement of intracellular TNF-alpha, IFN-gamma and IL-2 expression in stimulated CD3+ lymphocytes: differences between young and elderly subjects. Exp Gerontol. 2002;37(2–3):227–234. doi: 10.1016/s0531-5565(01)00188-7. [DOI] [PubMed] [Google Scholar]
- Medvedik O, Sinclair DA. Caloric restriction and life span determination of yeast cells. Methods Mol Biol. 2007;371:97–109. doi: 10.1007/978-1-59745-361-5_9. [DOI] [PubMed] [Google Scholar]
- Messaoudi I, Lemaoult J, et al. Age-related CD8 T cell clonal expansions constrict CD8 T cell repertoire and have the potential to impair immune defense. J Exp Med. 2004;200(10):1347–1358. doi: 10.1084/jem.20040437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messaoudi I, Warner J, et al. Delay of T cell senescence by caloric restriction in aged long-lived nonhuman primates. Proc Natl Acad Sci U S A. 2006;103(51):19448–19453. doi: 10.1073/pnas.0606661103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RA. Effect of aging on T lymphocyte activation. Vaccine. 2000;18(16):1654–1660. doi: 10.1016/s0264-410x(99)00502-2. [DOI] [PubMed] [Google Scholar]
- Nikolich-Zugich J, Messaoudi I. Mice and flies and monkeys too: caloric restriction rejuvenates the aging immune system of non-human primates. Exp Gerontol. 2005;40(11):884–893. doi: 10.1016/j.exger.2005.06.007. [DOI] [PubMed] [Google Scholar]
- Pahlavani MA. Influence of caloric restriction on aging immune system. J Nutr Health Aging. 2004;8(1):38–47. [PubMed] [Google Scholar]
- Pannetier C, Cochet M, et al. The sizes of the CDR3 hypervariable regions of the murine T-cell receptor beta chains vary as a function of the recombined germ-line segments. Proceedings of the National Academy of Sciences USA. 1993;90:4319–4323. doi: 10.1073/pnas.90.9.4319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitcher CJ, Hagen SI, et al. Development and homeostasis of T cell memory in rhesus macaque. J Immunol. 2002;168(1):29–43. doi: 10.4049/jimmunol.168.1.29. [DOI] [PubMed] [Google Scholar]
- Posnett DN, Edinger JW, et al. Differentiation of human CD8 T cells: implications for in vivo persistence of CD8+CD28- cytotoxic effector clones. 1999;11:229–241. doi: 10.1093/intimm/11.2.229. [DOI] [PubMed] [Google Scholar]
- Posnett DN, Sinha R, et al. Clonal populations of T cells in normal elderly humans: the T cell equivalent to “benign monoclonal gammapathy”. J Exp Med. 1994;179(2):609–618. doi: 10.1084/jem.179.2.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey JJ, Colman RJ, et al. Dietary restriction and aging in rhesus monkeys: the University of Wisconsin study. Exp Gerontol. 2000;35(9–10):1131–1149. doi: 10.1016/s0531-5565(00)00166-2. [DOI] [PubMed] [Google Scholar]
- Roberts SB, Schoeller DA. Human Caloric Restriction for Retardation of Aging: Current Approaches and Preliminary Data. J. Nutr. 2007;137(4):1076–1077. doi: 10.1093/jn/137.4.1076. [DOI] [PubMed] [Google Scholar]
- Roecker EB, Kemnitz JW, et al. Reduced immune responses in rhesus monkeys subjected to dietary restriction. J Gerontol A Biol Sci Med Sci. 1996;51(4):B276–B279. doi: 10.1093/gerona/51a.4.b276. [DOI] [PubMed] [Google Scholar]
- Roth GS, Ingram DK, et al. Nutritional interventions in aging and age-associated diseases. Ann N Y Acad Sci. 2007;1114:369–371. doi: 10.1196/annals.1396.048. [DOI] [PubMed] [Google Scholar]
- Roth GS, Lesnikov V, et al. Dietary Caloric Restriction Prevents the Age-Related Decline in Plasma Melatonin Levels of Rhesus Monkeys. J Clin Endocrinol Metab. 2001;86(7):3292–3295. doi: 10.1210/jcem.86.7.7655. [DOI] [PubMed] [Google Scholar]
- Saurwein-Teissl M, Lung TL, et al. Lack of antibody production following immunization in old age: association with CD8(+)CD28(−) T cell clonal expansions and an imbalance in the production of Th1 and Th2 cytokines. J Immunol. 2002;168(11):5893–5899. doi: 10.4049/jimmunol.168.11.5893. [DOI] [PubMed] [Google Scholar]
- Schwab R, Szabo P, et al. Expanded CD4+ and CD8+ clones in elderly humans. Journal of Immunology. 1997;158:4493–4499. [PubMed] [Google Scholar]
- Spaulding C, Guo W, et al. Resistance to apoptosis in human CD8+ T cells that reach replicative senescence after multiple rounds of antigen-specific proliferation. Exp Gerontol. 1999;34(5):633–644. doi: 10.1016/s0531-5565(99)00033-9. [DOI] [PubMed] [Google Scholar]
- Spaulding CC, Walford RL, et al. The accumulation of non-replicative, non-functional, senescent T cells with age is avoided in calorically restricted mice by an enhancement of T cell apoptosis. Mech Ageing Dev. 1997;93(1–3):25–33. doi: 10.1016/s0047-6374(96)01808-8. [DOI] [PubMed] [Google Scholar]
- Spaulding CC, Walford RL, et al. Calorie restriction inhibits the age-related dysregulation of the cytokines TNF-alpha and IL-6 in C3B10RF1 mice. Mech Ageing Dev. 1997;93(1–3):87–94. doi: 10.1016/s0047-6374(96)01824-6. [DOI] [PubMed] [Google Scholar]
- Sun D, Muthukumar AR, et al. Effects of calorie restriction on polymicrobial peritonitis induced by cecum ligation and puncture in young C57BL/6 mice. Clin Diagn Lab Immunol. 2001;8(5):1003–1011. doi: 10.1128/CDLI.8.5.1003-1011.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo P, Li F, et al. Evolution of B-cell clonal expansions with age. Cell Immunol. 2004;231(1–2):158–167. doi: 10.1016/j.cellimm.2005.01.002. [DOI] [PubMed] [Google Scholar]
- Vallejo AN. CD28 extinction in human T cells: altered functions and the program of T-cell senescence. Immunol Rev. 2005;205:158–169. doi: 10.1111/j.0105-2896.2005.00256.x. [DOI] [PubMed] [Google Scholar]
- Vallejo AN, Nestel AR, et al. Aging-related deficiency of CD28 expression in CD4+ T cells is associated with the loss of gene-specific nuclear factor binding activity. J. Biol. Chem. 1998;273(14):8119–8129. doi: 10.1074/jbc.273.14.8119. [DOI] [PubMed] [Google Scholar]
- Vasto S, Candore G, et al. Inflammatory networks in ageing, age-related diseases and longevity. Mech Ageing Dev. 2007;128(1):83–91. doi: 10.1016/j.mad.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Verdery RB, Ingram DK, et al. Caloric restriction increases HDL2 levels in rhesus monkeys (Macaca mulatta) Am J Physiol. 1997;273(4 Pt 1):E714–E719. doi: 10.1152/ajpendo.1997.273.4.E714. [DOI] [PubMed] [Google Scholar]
- Volk MJ, Pugh TD, et al. Dietary restriction from middle age attenuates age-associated lymphoma development and interleukin 6 dysregulation in C57BL/6 mice. Cancer Res. 1994;54(11):3054–3061. [PubMed] [Google Scholar]
- Weindruch R. Dietary restriction, tumors, and aging in rodents. J Gerontol. 1989;44(6):67–71. doi: 10.1093/geronj/44.6.67. [DOI] [PubMed] [Google Scholar]
- Weindruch R, Lane M, et al. Dietary restriction in rhesus monkeys: lymphopenia and reduced mitrogen-induced proliferation in peripheral blood mononuclear cells. 1997;9:304–308. doi: 10.1007/BF03341833. [DOI] [PubMed] [Google Scholar]
- Weindruch R, Walford RL. Dietary restriction in mice beginning at 1 year of age: effect on life-span and spontaneous cancer incidence. Science. 1982;215(4538):1415–1418. doi: 10.1126/science.7063854. [DOI] [PubMed] [Google Scholar]
- Weindruch RH, Kristie JA, et al. Influence of weaning-initiated dietary restriction on responses to T cell mitogens and on splenic T cell levels in a long-lived F1-hybrid mouse strain. Exp Gerontol. 1982;17(1):49–64. doi: 10.1016/0531-5565(82)90008-0. [DOI] [PubMed] [Google Scholar]
- Weyand CM, Goronzy JJ. T-cell-targeted therapies in rheumatoid arthritis. Nat Clin Pract Rheumatol. 2006;2(4):201–210. doi: 10.1038/ncprheum0142. [DOI] [PubMed] [Google Scholar]
- Wikby A, Maxson P, et al. Changes in CD8 and CD4 lymphocyte subsets, T cell proliferation responses and non-survival in the very old: the Swedish longitudinal OCTO-immune study. 1998;102(2–3):187–198. doi: 10.1016/s0047-6374(97)00151-6. [DOI] [PubMed] [Google Scholar]
- Wikby A, Nilsson BO, et al. The immune risk phenotype is associated with IL-6 in the terminal decline stage: findings from the Swedish NONA immune longitudinal study of very late life functioning. Mech Ageing Dev. 2006;127(8):695–704. doi: 10.1016/j.mad.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Wolf NS, Penn PE, et al. Caloric restriction: conservation of in vivo cellular replicative capacity accompanies life-span extension in mice. Exp Cell Res. 1995;217(2):317–323. doi: 10.1006/excr.1995.1092. [DOI] [PubMed] [Google Scholar]
- Zanni F, Vescovini R, et al. Marked increase with age of type 1 cytokines within memory and effector/cytotoxic CD8+ T cells in humans: a contribution to understand the relationship between inflammation and immunosenescence. Exp Gerontol. 2003;38(9):981–987. doi: 10.1016/s0531-5565(03)00160-8. [DOI] [PubMed] [Google Scholar]
- Zhang X, Fujii H, et al. Aging leads to disturbed homeostasis of memory phenotype CD8(+) cells. J Exp Med. 2002;195(3):283–293. doi: 10.1084/jem.20011267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.