Abstract
Background: There are currently no field data about the effect of implementing European Working Time Directive (EWTD)-compliant rotas in a medical setting. Surveys of doctors’ subjective opinions on shift work have not provided reliable objective data with which to evaluate its efficacy.
Aim: We therefore studied the effects on patient's safety and doctors’ work-sleep patterns of implementing an EWTD-compliant 48 h work week in a single-blind intervention study carried out over a 12-week period at the University Hospitals Coventry & Warwickshire NHS Trust. We hypothesized that medical error rates would be reduced following the new rota.
Methods: Nineteen junior doctors, nine studied while working an intervention schedule of <48 h per week and 10 studied while working traditional weeks of <56 h scheduled hours in medical wards. Work hours and sleep duration were recorded daily. Rate of medical errors (per 1000 patient-days), identified using an established active surveillance methodology, were compared for the Intervention and Traditional wards. Two senior physicians blinded to rota independently rated all suspected errors.
Results: Average scheduled work hours were significantly lower on the intervention schedule [43.2 (SD 7.7) (range 26.0–60.0) vs. 52.4 (11.2) (30.0–77.0) h/week; P < 0.001], and there was a non-significant trend for increased total sleep time per day [7.26 (0.36) vs. 6.75 (0.40) h; P = 0.095]. During a total of 4782 patient-days involving 481 admissions, 32.7% fewer total medical errors occurred during the intervention than during the traditional rota (27.6 vs. 41.0 per 1000 patient-days, P = 0.006), including 82.6% fewer intercepted potential adverse events (1.2 vs. 6.9 per 1000 patient-days, P = 0.002) and 31.4% fewer non-intercepted potential adverse events (16.6 vs. 24.2 per 1000 patient-days, P = 0.067). Doctors reported worse educational opportunities on the intervention rota.
Conclusions: Whilst concerns remain regarding reduced educational opportunities, our study supports the hypothesis that a 48 h work week coupled with targeted efforts to improve sleep hygiene improves patient safety.
Introduction
The 1993 European Working Time Directive (EWTD) is intended to improve patient and doctor's safety by limiting the maximum required working hours to 48 per week, and was adopted into UK law in 1998 with an extension before full implementation.1 A package of measures to improve the lives of junior doctors (the New Deal), at the same time also contemplates extending working hours and ensuring that adequate rest time is built into rota systems.2 Since August 2007 the average hours worked by junior doctors, calculated over 6 months, have been reduced to 56 per week with the intention of complying with the 48 h required by the EWTD by August 2009.3
In the United States the rate of serious medical errors made by junior doctors are substantially higher when they work a traditional on-call system involving frequent periods of duty lasting for 24 h or more. The introduction of an intervention schedule, which limited scheduled continuous duty to 16 h and reduced the total number of hours worked from 85 to 65 per week, resulted in more sleep, fewer attentional failures on duty and fewer serious medical errors.4–6 These results provided objective measurements of what had previously been mainly anecdotal reports about the effect on patient safety of doctors working for extended periods. The number of continuous hours worked increases the risk that safety incidents will occur, a risk that is compounded by night working and increases with each successive shift.7–8 Similarly, US junior doctors have twice the risk of having a car crash driving home from an extended shift as compared to driving home after a non-extended shift9 and are at increased risk of sharp injuries when working overnight and ‘post-call’.10
The need to implement the requirements of EWTD competes with demands to maintain adequate medical cover at all times while ensuring that doctors are able to access the educational and training opportunities necessary to guarantee a safe and competent workforce in the future.11 Concerns have also been raised regarding the reduced time that is available for training junior doctors, the effect that this will have on clinical experience (including continuity of care), quality of care and quality of life for doctors as a result of the new directive. None of the proposed new shift patterns have been evaluated objectively prior to implementation for their effect on patient safety and resident health. The UK Multidisciplinary Working Group of the Royal College of Physicians has proposed a theoretically optimized schedule built around a 9 h shift system which aims to promote the design of a rota that will minimize the risk to doctors’ health and patient safety particularly with regard to the length and frequency of night shifts.12 We hypothesize that medical error rates would be reduced following introduction of a 48 h a week rota as compared to the 56 h rota currently in use.
There are few objective data in support of continuing to schedule medical trainees to work long shifts and long work weeks. There are currently no field data about the effect of implementing EWTD-compliant rotas in a medical setting and previous surveys of doctors’ subjective opinions on shift working have not provided reliable objective data with which to evaluate its efficacy.13 An evidence-based approach is needed to document the effect of work practices on junior doctors’ health, access to education, on patient safety and continuity of care.14
This study aims to address this lack of evidence15 by measuring patient safety, quality of handover, doctors’ rest and sleep after implementing a 2009 EWTD-compliant shift system for junior doctors in a large NHS Hospital Trust.
Methods
Ethics
The study was approved by the local research ethics committee (Ref: 07/Q2802/4). Written informed consent was provided by all doctors prior to the start of the study.
Study design
The study was carried out at the University Hospitals Coventry & Warwickshire NHS Trust, a 1250-bed Hospital in Coventry, over a 12-week period in 2007. During this period there were 1707 admissions to the wards included in this study.
The study was a single-blind between-groups clinical study with an intervention group consisting of 9 junior doctors covering in rotation the Clinical Decision Unit (CDU: 32 beds) and the Endocrinology ward (42 beds) who were scheduled to a 2009 EWTD-compliant rota with an average of up to 48 h/week (Figure 1, right), and a group working on their traditional schedule, comprising 10 junior doctors covering in rotation the Care of the Elderly (42 beds) and the Respiratory ward (52 beds), who were scheduled to a traditional rota of up to 54 h/week on average (Figure 1, left), for a duration of 12 weeks. The allocation of groups to intervention or traditional was random. Due to expected differences in case load in CDU (intervention) and Care of the Elderly (traditional) and given that the two firms of doctors would have to cover two wards in their rota, the analysis plan was to compare only Endocrinology (Intervention) vs. Respiratory (Traditional) due to expected comparability in case mix.
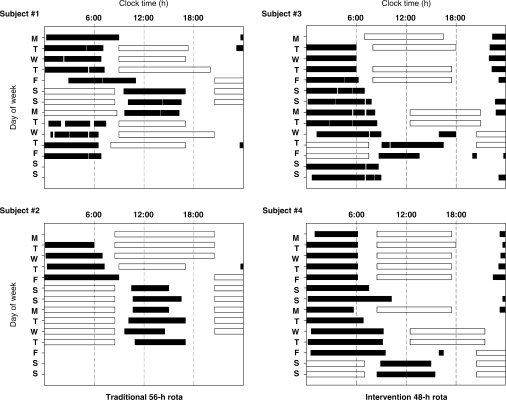
Figure 1.
Representative examples of junior doctor work and sleep patterns. Self-reported sleep times (filled bars) and work hours (open bars) are shown for four junior doctors while working on either a 56 h schedule (subjects 1 and 2, left panels) or a 48 h schedule (subjects 3 and 4, right panels). Clock time is plotted on the abscissa (0:00–0:00 h) with day of the week plotted on the ordinate over 14 consecutive days of the 12-week study. During the standard 56 h schedule, junior doctors were required to make an abrupt change from day shifts to night shifts, and were scheduled to work 3 or more consecutive 12.5 h night shifts (from 20:30–20:45 to 9:00–9:15 h) (e.g. Fri to Sun, subject 1; Fri to Wed, subject 2). During the 48 h intervention schedule, the transition from day shifts to night shifts was made more gradually. Evening shifts (8:5–9:0 h; 12:30–21:00 h or 15:00–00:00 h) were scheduled for the 2–3 days prior to starting the night shifts (e.g. second Mon and Tue, subject 3; second Wed and Thu, subject 4), and shorter 8:75–11:00 h night shifts (start range 20:30–23:00 h, end range 7:30–9:00 h) were limited to a maximum three consecutive shifts, and usually only for two (61% of occasions). The sequence of shifts from day-evening-night also facilitated sleep by permitting extended sleep before the evening shift. Doctors were also encouraged to take a nap in the afternoon before the night shift.
Rotas
The traditional rota consisted of blocks of three and four 12.5 h night shifts in succession and day shifts of 9 h that could include attached on-call duties which extended the working day to 12.5 h. A novel 9 h shift system was introduced in a single tier of junior doctors (SHO/F2 level) for the intervention group (n = 9). This was a close approximation of the rota that the UK Multidisciplinary Working Group of the Royal College of Physicians had identified as the safer of possible rotas, the ‘three 9 h shifts for 24 h’, both New Deal and EWTD-compliant.12,16 The intervention rota was designed to allow doctors to have sequential shifts in optimal order for circadian adaptation ‘early > evening > night’, facilitating acclimatization to night-working. The night-shifts were shorter (9 h) reduced to blocks of two or less often three nights. The rota comprised a sequence of two consecutive early shifts (07:00–16:00 h), followed by two consecutive evening shifts (15:00–24:00 h) and then two-three consecutive night shifts (23:00–08:00 h). The intervention group was given written advice on sleep hygiene and on the importance of naps. After the first 6 weeks the intervention rota caused concerns particularly as it left daytime shifts with increased work pressures and frequent handovers. At an interim meeting held with junior doctors, research team, supporting consultants, NHS managers and representatives of the NHS Workforce, it was agreed to modify the intervention rota aiming at increasing daytime coverage by commencing the late shift earlier (12:30) and extending the night shift from the original 9 h to a maximum of 11 h. This schedule was then followed for the remaining 6 weeks of the study.
Work and sleep patterns
Doctors were asked to complete a work and sleep diary every day for the duration of the study. Start and finish of shift were recorded daily. Sleep patterns included time going to bed, estimated time falling asleep, time waking up, arousals and naps.
Data collection of medical errors
Our study used retrospective case note review to detect medical errors and adverse events.4,17 The doctors and relevant ward staff were informed that records of patients who had completed an episode of care on each of the four study wards would be randomly selected for this purpose.
Medical chart review was conducted by two nurses (AB and GW) with a background in clinical care. Incidents with potential to cause harm were identified using an established methodology.17–19 All components of the inpatient medical record, including admission and discharge summaries, medication prescription charts, physician and nursing progress notes, were reviewed for possible medical errors and adverse events. In addition, ‘triggers’ (i.e. incidents suggestive of possible adverse events) drawn from the Institute of Healthcare Improvement's (IHI) Global Trigger Tool list were used to enhance this process20 (Appendix 1).
The degree of concordance between the nurses in detecting incidents was ascertained by double review of a random sample of notes (n = 40). For 85% of reviews there was agreement. Discrepancies were related to detection of errors on diagnostic tests (n = 3), medication (n = 2) and documentation of known drug allergy (n = 1).
The selected records were checked to ensure that each patient had spent at least 24 h under the care of the study team. Each episode of care was reviewed, either until patient discharge, transfer elsewhere or death. A 30 min time limit was set for checking each record. Incidents that occurred when the patient was not on the study ward or under the care of the study team were excluded (see additional methods).
Patient safety incidents for the study wards which were reported by staff to the hospital's Clinical Governance department during the observation period were also obtained. There were a total of 60 of these from the four clinical areas (30 each from the traditional and intervention groups) for 49 patients relating to events such as falls (n = 47) and medication incidents (n = 13). These incidents are typical of those most commonly reported to the National Patient Safety Agency (NPSA).21 None of the falls were linked to any medical error while six medication incidents were detected by the researchers in the selected notes and associated with a medical error.
Incident classification
An adverse event was defined as an incident in which medical management resulted in harm to the patient. In addition, any errors with potential to cause harm were documented, reviewed and categorized20,22 (additional methods and Appendix 2).
Incident certification
Before beginning data collection, all staff received intensive training in the consistent, objective collection of data using standardized forms. Given that it was not possible to blind data collectors to the study schedule, determinations of the preventability and classification of events were not made by the primary data collectors. Instead, each suspected error or adverse event identified was independently rated by two senior physicians who were unaware of the identity of those involved and whether the incident occurred during the traditional or intervention rota. Blinded reviewers categorized each incident as an adverse event, non-intercepted potential adverse events, intercepted potential adverse events or error with little potential for harm (Appendix 3) and rated the preventability of adverse events using a Likert scale (was prevented, definitely preventable, probably preventable, probably not preventable or definitely not preventable); the preventability scale was dichotomized to include only ‘preventable events’ and ‘non-preventable events’ before analysis. Events deemed more likely to be due to patients’ underlying illness than to medical therapy were excluded (Appendix 4). The inter-rater reliability was calculated by means of the Cohen's kappa (κ) statistic. Any disagreements were resolved either by discussion or a third physician. For methods of questionnaire, interviews and handovers see additional methods online. Analysis of the latter was qualitative23–24 (see Box 1–4 online).
Statistical analysis
Prior research conducted by our group and others using surveillance methodology has established that medical errors in general ward settings typically occur at a rate of ∼100–150 per 1000 patient-days, including minor errors as well as more serious errors. Estimating that we would detect 100 per 1000 patient-days in our control group, we powered the study to detect a 25% reduction in serious errors in our intervention group. With 2000 patient-days per group (4000 patient-days in total), we calculated that we would have 80% power to detect a 25% reduction in medical errors, assuming a two-sided alpha error of 0.05. Non-normally distributed variables are reported as median with interquartile range (IQR). Non-parametric Mann–Whitney test was used for comparisons of patients’ characteristics between intervention and traditional rotas while Kruskal–Wallis test was used for the comparisons among wards. We computed incidence rates by assuming a Poisson distribution since patients had more than one type of errors. The age information was included as the covariate in a Generalized Linear Model and log-transformed length of stay on study was considered as the offset component the comparison of rates used chi-square test. Sleep and work hours data were compared using Student's t-test. Statistical tests were two-tailed and P < 0.05 was defined as statistically significant. Cohen's kappa statistic (κ) was used to assess the level of agreement between physician reviewers for incident classification (κ = 0.813; 95% CI 0.756–0.869). The incidence rate comparisons were carried out using Intercooled Stata 9.2 for Windows and the remaining statistical tests using SPSS (v15 for Windows). Results are reported as means (95% CIs, SDs or ranges).
Results
Out of a total of 1707 admissions in the four study wards during the study period, 916 (54%) were randomly selected for review [251/628 (40%) from the CDU, 233/348 (67%) from the Endocrinology ward, 248/462 (54%) from the Respiratory ward and 184/269 (68%) from the Care of the elderly ward]. The percentages varied slightly due to some records not being available for review during the time limit set in the study. However, the sample was representative of all admissions during the time of the study (data not shown).
Doctors’ characteristics
Of the 19 doctors, 11 were women (six in the traditional and five in the intervention group). Mean age was 31.5 (SD 5.6) years in the traditional and 29.7 (SD 4.0) years in the intervention group. Body mass index was 26.3 (95% CI 21.6–30.9) and 23.2 (95% CI 20.2–26.2) kg/m2, respectively. Median year of qualification (and range) were the same in the two groups [2002 (1990–2005)]. All but one were non-smokers and they were comparable for self-reported alcohol consumption [2.7 (0.8 to 6.1) units/week vs. 4.9 (0.9 to 10.6) units/week], caffeinated drinks consumption [3.0 (range 0–5.0) cups/day vs. 2.3 (range 1.0–4.5) cups/day] and SF-36 Mental Component Score [49.1 (8.1) vs. 49.6 (6.6)].
Work and sleep patterns
Figure 1 reports representative examples of junior doctor work and sleep patterns. During the traditional 56 h rota, junior doctors were required to make an abrupt change from day shifts to night shifts, and were scheduled to work 3 or more consecutive 12.5 h night shifts. During the 48 h intervention rota, the transition from day shifts to night shifts was made more gradually. Evening shifts were scheduled for the 2–3 days prior to starting the night shifts which were shorter and limited to a maximum three consecutive shifts, and usually only for two (61% of occasions). In the intervention group the sequence of shifts from day-evening-night was designed to facilitate sleep by permitting extended sleep before the evening shift. Doctors were also encouraged to take a nap in the afternoon before the night shift.
The distribution of scheduled weekly work hours is shown in Figure 2a. Although the average weekly work hours differed by less than 10 h/week between the traditional and intervention rotas [52.4 (11.2) h/week vs. 43.2 (7.7) h/week, respectively; P < 0.001], there was a remarkable difference in the range and distribution of weekly hours. Under the traditional 56 h rota, scheduled weekly work hours ranged from 30 to 77 h/week, with 25% of work weeks lasting longer than 58 h (Figure 2a). In contrast, the intervention rota had a maximum of 60 h/week (range 26–60) with only 2% of weeks with work ∼58 h/week (Figure 2a).
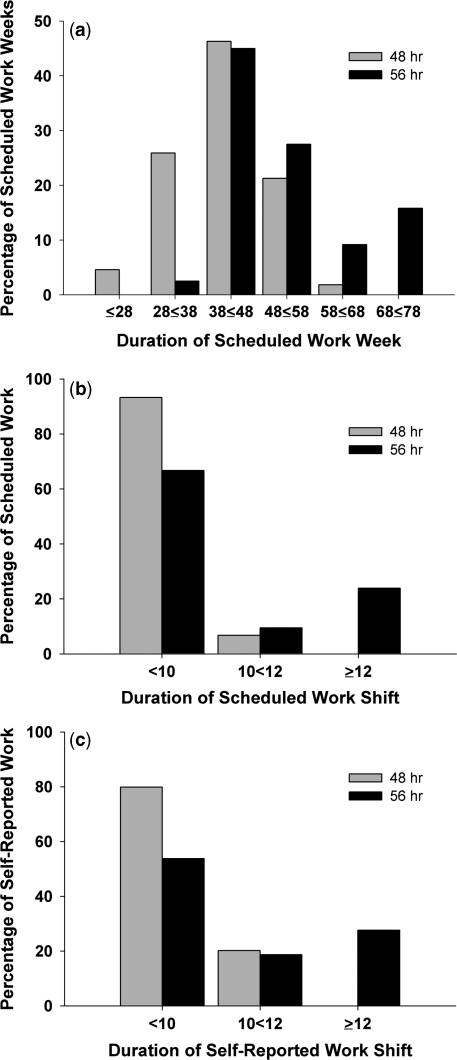
Figure 2.
(a) Distribution of scheduled weekly work hours across the 12 weeks for the two groups. (b) Distribution of scheduled work shift duration for all individuals. (c) Distribution of self-reported work shift duration in a subset of subjects working the 48 h (n = 4) or 56 h (n = 5) rotas.
The 48 h intervention rota reduced the average duration of scheduled work shifts by nearly an hour as compared to the traditional rota [9.9 (1.7) h (range 4.5–12.5; n = 10) vs. 9.0 (0.8) h (3.0–11.0; n = 9); P < 0.001] and abolished continuous duty shifts >12 h, which were scheduled nearly 25% of the time on the traditional 56 h rota (Figure 2b). Shifts of 10 h or more were scheduled only 7% of the time on the intervention rota, but were more than four times more frequent (33%) during the traditional 56 h rota (Figure 2b). The average duration [9.9 (1.9) h (3.0–13.0) vs. 9.2 (0.8) h (5.5–11.5); P < 0.001] and distribution of scheduled hours agreed closely with self-reported work hours from the subset of subjects with the most comprehensive diary data (n = 9) (Figure 2c).
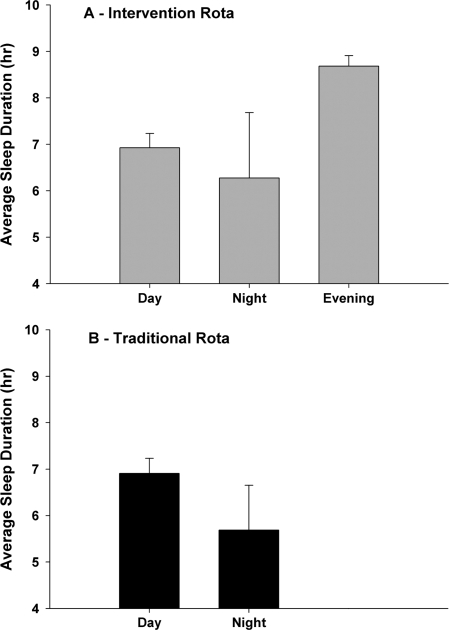
Total sleep time per day tended to be longer during the intervention as compared to the traditional rota [7.26 (0.36) h vs. 6.75 (0.40) h, respectively; P = 0.095] and as intended, the shift sequence during the intervention rota permitted a substantial recovery sleep of nearly 9 h [8.68 (0.23) h] after the evening shift, significantly more than after the day [6.93 (0.31) h] or night [6.28 (1.41) h] shift (P < 0.05; Figure 3a). Sleep duration was shortest following the night shift on the traditional rota [5.69 (0.97) h] (Figure 3b).
Figure 3.
Comparison of average duration of sleep after each shift type during the 48 h a week intervention rota (n = 4) and the traditional 56 h a week rota (n = 5) (mean and standard deviation).
Characteristics of work on different wards
The whole chart assessment review involved 8038 patient-days (4842 during the traditional rota and 3207 during the intervention rota), representing 916 admissions (54% of 1707 total admissions to the study wards) during the 12-week observation period: 432 during the traditional rota [184 for Care of the Elderly and 248 for the Respiratory ward] and 484 during the intervention rota [233 for the Endocrinology ward and 251 for the CDU]. A total of 346 incidents were presented to physicians for classification, of which 293 (85%) were categorized as adverse events and errors (66 for Care of the Elderly, 95 for Respiratory, 68 for Endocrinology and 64 for the CDU). The remaining 53 incidents were excluded as not satisfying the error criteria.
The case-mix and the characteristics of hospital stay were, as expected, significantly different across the four wards under study. Patients were older in the Care of the Elderly ward [median age (IQR) 82 years (12)] compared to Respiratory, Endocrinology and CDU [71 (27), 71 (31) and 74 (25) years, respectively] (P < 0.001). Hospital stay was longer in the Care of the Elderly ward [median (IQR) 17 patient-days (17)] and shorter in the CDU [5 patient-days (7)] than both Respiratory [10 patient-days (9)] and Endocrinology [9 patient-days (13)] wards (P < 0.001). Likewise, length of stay during the study period was longer in the Care of the Elderly [11 patient-days (14)] and shorter in the CDU [3 patient-days (1)] than both Respiratory [7 patient-days (7)] and Endocrinology [7 patient-days (10)] wards (P < 0.001). As mentioned above, the intention-to-treat analysis was carried out comparing error rates between Respiratory (Traditional) and Endocrinology (Intervention) wards only. These wards were comparable as far as number of admissions and patients seen, age of patients, patient-days in hospital and on study ward and in the rate of death whilst in hospital (Table 1).
Table 1.
Characteristics of patients and episodes
| Traditional respiratory | Intervention endocrinology | P-value | |
|---|---|---|---|
| Admissions (n) | 248 | 233 | |
| Patients (n) | 244 | 230 | |
| Age (years), median (IQR) | 71 (27) | 71 (31) | 0.14 |
| Patient-days in hospital, median (IQR) | 10 (9) | 9 (13) | 0.37 |
| Patient-days on study ward, median (IQR) | 7 (7) | 7 (10) | 0.61 |
| Death rate, n (%) | 34 (13.7) | 38 (16.3) | 0.43 |
| Death rate (age adj.), n (%) | 34 (14.2) | 38 (15.8) | 0.62 |
Medical errors
During a total of 4782 patient-days involving 481 admissions (2315 in the Respiratory ward—Traditional group and 2467 in the Endocrinology ward—Intervention group), 32.7% fewer total medical errors occurred during the intervention than the traditional rota (27.6 vs. 41.0 per 1000 patient-days, P = 0.006). The Hazard ratio (95% CI) was 0.62 (0.45–0.84), P < 0.05. There were 82.6% fewer intercepted potential adverse events (1.2 vs. 6.9 per 1000 patient-days, P = 0.002) with Hazard ratio 0.16 (0.05–0.57), P < 0.05 and 31.4% fewer non-intercepted potential adverse events (16.6 vs. 24.2 per 1000 patient-days, P = 0.067) with a Hazard ratio of 0.63 (0.42–0.94), P < 0.05 (Table 2). Preventable adverse events did not differ between groups (Table 2). Differences in error rates did not differ substantially between the first 6 weeks (26.0 vs. 30.4 per 1000 patient-days) and the latter 6 weeks (31.4 vs. 56.0 per 1000 patient-days) of the study period.
Table 2.
Adverse events and error rates between intervention and traditional rotas
| Traditional respiratory | Intervention endocrinology | Percentage of rate reduction (95% CI)a | P-value | |
|---|---|---|---|---|
| Patient-days | 2315 | 2467 | ||
| Preventable adverse events, n (rateb) | 5 (2.2) | 4 (1.6) | −27.3 (−85.1 to 249) | 0.68 |
| Intercepted potential adverse events, n (rate) | 16 (6.9) | 3 (1.2) | −82.6 (−97.7 to −38.5) | 0.002 |
| Non-intercepted potential adverse events, n (rate) | 56 (24.2) | 41 (16.6) | −31.4 (−55.2 to 4.6) | 0.067 |
| Minor errors, n (rate) | 18 (7.8) | 20 (8.1) | 3.8 (−52.2 to 91.0) | 0.90 |
| Overall, n (rate) | 95 (41.0) | 68 (27.6) | −32.7 (−52.9 to −10.4) | 0.006 |
aRate reduction = (rate of Endocrine – rate of Respiratory) × 100/rate of Respiratory.
bRate is expressed as number (per 1000 patient-days).
Interview findings (see expanded results online)
Reduced junior medical staff cover during the normal day was reported by several doctors in both groups (Boxes 1 and 2 in appendix). Lack of time for interaction with the rest of the team with less chance of feed-back on their performance was another theme. Most doctors in the intervention group felt that their educational opportunities were compromised. Doctors in the traditional group generally made positive comments about learning opportunities (Box 3 in appendix). Comments on rest and sleep varied (Box 4 in appendix). Both intervention and traditional groups reported that working in the evening or on night shifts and at weekends had a negative impact on social and family life. Doctors were almost unanimous in their description of procedures and selection of patients for handover (see additional results online). Some reported that they would hand over or be handed over jobs that had not been done because the outgoing doctor had not had time to do them. Few had concerns about the quality of handover but several spoke about the risk of omissions in care when patients were the subject of frequent handovers on the intervention rota. Thirty-four handovers were observed. Often the extra handovers during the frequent shift changeover did not take place or happened only informally.
Discussion
The current article is, to our knowledge, the first prospective study conducted in an NHS hospital in the United Kingdom on the effects of a 48 h/week EWTD-compliant rota on patient care, as assessed objectively from medical error rates. The study shows that 33% fewer medical errors occurred on an intervention rota with shifts up to 48 h, as compared to a traditional 56 h/week schedule. While differences in clinical specialty may explain some differences in error rates between rotas, the study suggests that implementation of a 48 h work week can be accomplished without an adverse effect on patient safety. Notably, the study was conducted during a difficult period for junior doctors when many of them were involved in applying for training posts under the Medical Training Application Service (MTAS) scheme which caused well-publicized dissatisfaction and had a negative effect on the morale of many of those participating.24 Nevertheless the results are striking.
There has been considerable controversy regarding the appropriateness of implementing the EWTD in the NHS. Concerns have been raised that the new directive would put doctors’ and patients’ lives at risk25, would lead to reduced time available for training, will have negative impacts on clinical experience and quality of care.26–28 These strong assertions are, without exception, based on opinions, anecdotes or non-validated questionnaires and surveys.29–32 Our study is the first objective assessment of the impact of 2009 EWTD-compliant schedules on patient care, the primary concern of healthcare providers, and presents scientific evidence upon which to begin basing policy decisions.
In 2006 the Royal College of Physicians Multidisciplinary Working Group recommended (i) that rotas involving seven consecutive 13 h night shifts must be stopped due to their inherent high risk of fatigue and potential harm to patients and staff; (ii) that the number of night shifts in succession should not exceed four and the length of each night shift should be minimized; (iii) to encourage the use of three 9 h shifts to cover 24 h with the aim of improving patient health and safety, junior doctors’ safety, teaching, supervision and efficiency; (iv) to use evidence-based approaches in order to define optimal 48 h rotas by 2009; (v) that a ‘cell’ of 10 junior doctors is necessary for any post that provides 24 h cover.12 Inspired by the RCP recommendations, we proposed a study to test the feasibility of implementing a EWTD-compliant 48 h a week schedule and to assess objectively its impact on patient safety. The intervention rota was based on the schedule that the RCP proposed as the most promising in its review in minimizing the risk to patient safety and doctors’ health with particular regard to the length and frequency of night shifts.12
The intervention rota had several important components that were based on well-established principles of sleep medicine and circadian biology.14,33 First, it limited consecutive night shifts to three nights maximum and for the majority of weeks, only two, in order to reduce the build-up of chronic partial sleep deprivation due to the limited sleep between night shifts. Second, shift duration was limited to 12 h maximum in order to minimize acute sleep deprivation, which represented a distinct difference from the current 56 h a week rota which scheduled 25% of shifts >12 h. Third, the sequence of shifts was designed to abolish ‘slam shifts’ in which doctors change from a day to a night shift immediately, which ensures complete circadian desynchrony,34 and instead gradually stagger the shifts from morning to evening to night in the direction that the circadian system most easily adapts to.35 This sequence also facilitates sleep and reduces performance decrements on the first night shift36 by providing an opportunity for a long recovery sleep after the evening shift prior to starting the first night shift. Finally, the intervention rota dramatically reduced the proportion of long work weeks, with an upper limit of 60 h per week, again reducing chronic sleep deprivation, in stark contrast to the current 56 h rota, during which 25% of the shifts were >58 h/week and as long as 77 h/week.
Given that extended duration duty hours and long work weeks had previously been shown to be associated with increased risk to patient safety and resident health,4–5,9–10,37 we hypothesized that medical errors rates would be reduced following introduction of the 2009 EWTD-compliant 48 h a week rota as compared to the 56 h rota currently in use. Indeed, we found that significantly fewer errors occurred on the 48 h rota as compared to the 56 h rota. This proportional benefit is comparable to that found in our previous study in medical- and cardiac-intensive care units in the United States4 although it must be noted that the US study was carried out in units where the absolute rate of errors, given the intensity of work, was much higher than we found in medical wards. It also appears, on first impression, that much more substantive rota changes were introduced in the US study (continuous scheduled duty changed from 24–30 h to 16 h and scheduled work weeks changed from 80 h/week to 63 h/week).4 On closer inspection, however, the fact that the 56 h EWTD regulations allow averaging weekly work hours over 6 months permits work weeks in the UK that, during some weeks, are comparable to the US limit of 80 h a week averaged over 4 weeks.38 We have previously argued that such weekly limit terms are misleading14 given that, in both the United States and UK, weekly work hours can be much longer than the nominal ‘limits’ if they are balanced by shorter weeks elsewhere in the rota. We believe that in the current study, the reduction in error rates observed may have been due to the effect of the intervention on reducing the range of weekly work hours, rather than the average hours per week. The difference between 56 and 48 h/week on average may appear small, but the difference may be much greater in any given week, as doctors still work nearly 80 h a week for some weeks under the current regulations.
In the study, only nine doctors worked on the intervention team while the traditional rota maintained its roster of 10 doctors. This imbalance was not ideal and the successes of the intervention study in improving work and sleep patterns, as well as the low rate of medical errors were, in part, offset by a number of unfavorable impressions of the intervention rota. The intervention rota resulted initially in too few doctors being available for duty during the day. The problems with reduced cover were precipitated by sick leave, annual leave and study leave. For a full implementation of our rota in future iterations of the schedule, these changes should be synchronized with normal hospital practices10 and should include more doctors, recently argued to be between 12 and 13 per cell28, but at minimum 10. Nevertheless our study in NHS-based medical wards was able to detect significant differences in work hours with important implications for patients’ safety, despite doctors’ perceptions that the new rota would worsen care and represent harm to patients.
As in a previous study,4 the reduction in medical errors was achieved despite a modest increase in the number of handovers, which may be a source of error in its own right.39 Regardless of shift length, the process of handing over care between shifts is error-prone, and should be a focus of future improvement efforts. Introduction of computerized handover tools40–41 or standardized, consistent verbal handover procedures could further improve patient safety on these rotas.
The study has several limitations. The two study groups were working in different wards so the case mix was different between the groups. Respiratory and Endocrine groups were similar in terms of doctors’ duties, though the medications and interventions employed differed somewhat, which may have affected detected rates of medical errors. The CDU differed substantially from both of these units, in that the patients were all emergency admissions; the Care of the Elderly also differed substantially, with longer length of stay and a higher proportion of patients who were terminally ill and in need of palliative care. The marked nature of the differences between the CDU and Care of the Elderly Wards precluded any reasonable comparison. As the Endocrine and Respiratory wards were more similar, we felt it reasonable to comparatively evaluate error rates between these two, but we do so with some caution; larger, closely controlled studies will be needed to confirm our findings.
Direct observation identifies higher error rates than other techniques but its cost and organizational implications limit its use.42 Retrospective case reviews is the most widely used clinical surveillance methodology for detecting medical errors and adverse events; rates of adverse events ranging from 2.9 to 16.6% have been reported from centres in North America and Australasia.43 A study in two acute hospital wards in the UK found an incidence rate of 11.7%.44 Retrospective case note review, as used in this study, is less expensive and labour intensive than observation but nevertheless time-consuming and may not provide such a clear cut view of events especially since it is entirely dependent on the ‘accuracy, completeness and legibility’ of medical records.45 These limitations applied to both study groups, however, and the physician review of errors was conducted blind to condition.
Our study was too short and not designed to assess the impact of the new 48 h rota on educational opportunities. Educational issues are intertwined with both patient safety issues and doctors well-being in the context of a training post. While the reduction of educational opportunities was raised as a concern, there are as yet no data testing the impact of shorter work hours on validated educational outcomes. Indeed, we could hypothesize that reducing work hours may enhance educational outcomes given the emerging importance of sleep in learning and memory consolidation46 and the difficulty with learning while ‘half asleep’ on duty.6 Additional controlled trials are needed to test these hypotheses.
While our intervention reduced the length of continuous duty and work week duration with the aim of reducing sleepiness and improving performance, most doctors did not consider that sleepiness was a major problem. These comments are not surprising given that self-ratings of sleepiness when sleep deprived do not reflect objective measurements of poor performance. Similar to the misperception of one's own performance induced by alcohol, sleep deprived subjects rate their alertness as better than their performance demonstrates.47,48 This example illustrates a larger point, however, namely that policy decisions should not be made based on subjective opinions. Such unsubstantiated preconceptions are not valid when designing safe schedules. Decisions regarding work hour reform should be based on data derived from controlled clinical trials data, just as objective data form the basis of evidence-based medical decision.12 Our current data represent the first step in this process and should be followed by additional hypothesis-driven studies.
Conclusions
An EWTD-compliant rota with reduced weekly hours can improve patient safety, as compared to a traditional rota. There is a need for a wider reengineering of shift systems and hospital processes than was possible in this pilot study to ensure that the safety gains for patients cared for by less tired doctors are not compromised by delayed investigations and treatment, which can result from difficulties managing the routine daytime workload. Our findings may not be directly applicable to all specialties, like surgery, or to all NHS Trusts; however, they do not indicate that a reduction in work hours inevitably leads to a reduction in the quality of patient care. Evidence-based policy decisions must be made for work hours in the same way as evidence-based medicine is used for clinical decisions.49
Supplementary Data
Supplementary data are available at QJM online.
Funding
The study was supported by the NHS National Workforce Projects. The study was carried out with independence from the funders.
Conflict of interest: None declared.
Supplementary Material
Acknowledgments
We thank the participating doctors, consultants reviewing the incidents (D. Bennett-Jones, J. Pohl, A. Short), ward Consultants, Matrons and Nurses, University Hospital Coventry & Warwickshire NHS Trust; M.A. Miller, N.-B. Kandala, J. Kidd, D. Cooper, A. Lowe, Warwick Medical School; C. A. Czeisler, Harvard Medical School and Brigham & Women's Hospital, Boston, MA, USA.
References
- 1.Jaeger vs. Landeshauptstadt Kiel. 2003. Social Policy – Council Directive 93/1 04/EC – Concepts of working time and rest period – On-call service provided by doctors in hospitals. [Google Scholar]
- 2.NHS Management Executive. 1991. Hours of Work of Doctors in Training, NHS Management Executive. [Google Scholar]
- 3.British Medical Association. [(accessed 8th April 2008)]; http://www.bma.org.uk/ap.nsf/Content/NIEWTD.
- 4.Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing intern's work hours on serious medical errors in intensive care units. New Engl J Med. 2004;351:1838–48. doi: 10.1056/NEJMoa041406. [DOI] [PubMed] [Google Scholar]
- 5.Barger LK, Ayas NT, Cade BE, Cronin JW, Rosner B, Speizer FE, Czeisler CA. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. Plos Med. 2006;3:e487. doi: 10.1371/journal.pmed.0030487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. New Engl J Med. 2004;351:1829–37. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 7.Folkard S, Tucker P. Shift work, safety and productivity. Occup Med. 2003;53:95–101. doi: 10.1093/occmed/kqg047. [DOI] [PubMed] [Google Scholar]
- 8.Folkard S, Lombardi DA, Tucker PT. Shift work: safety, sleepiness and sleep. Industrial Health. 2005;43:20–3. doi: 10.2486/indhealth.43.20. [DOI] [PubMed] [Google Scholar]
- 9.Barger LK, Cade BE, Ayas NT, Cronin JW, Rosner B, Speizer FE, et al. Extended work shifts and the risk of motor vehicle crashes among interns. New Engl J Med. 2005;352:125–34. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 10.Ayas NT, Barger LK, Cade BE, Hashimoto DM, Rosner B, Cronin JW, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296:1055–62. doi: 10.1001/jama.296.9.1055. [DOI] [PubMed] [Google Scholar]
- 11.Paice E, Reid W. Can training and service survive the European Working Time Directive? Med Educ. 2004;38:336–339. doi: 10.1111/j.1365-2929.2004.01834.x. [DOI] [PubMed] [Google Scholar]
- 12.Horrocks N, Pounder R on behalf of the Multidisciplinary Working Group of the Royal College of Physicians. Designing Safer Rotas for Junior Doctors in the 48-Hour Week. London: Royal College of Physicians; 2006. pp. 1–23. [Google Scholar]
- 13.Aitken M, Paice E. Trainees’ attitudes to shift work depend on grade and specialty. Br Med J. 2003;326:48. [PMC free article] [PubMed] [Google Scholar]
- 14.Lockley SW, Landrigan CP, Barger LK, Czeisler CA. When policy meets physiology. The challenge of reducing resident work hours. Clin Orthop Relat Res. 2006;449:116–27. doi: 10.1097/01.blo.0000224057.32367.84. [DOI] [PubMed] [Google Scholar]
- 15.Pounder R. European junior doctors who work at night. Eurohealth. 2006;12:5–7. [Google Scholar]
- 16.Horrocks N, Pounder R. Who's for five nine-hour shifts a week? Clin Med. 2006;6:440–2. doi: 10.7861/clinmedicine.6-5-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. Br Med J. 2008;336:488–91. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 19.Walsh KE, Adams WG, Bauchner H, Vinci RJ, Chessare JB, Cooper MR, et al. Medication errors related to computer order entry in children. Pediatrics. 2006;118:1872–79. doi: 10.1542/peds.2006-0810. [DOI] [PubMed] [Google Scholar]
- 20.Griffin FA, Resar RK. IHI Innovation Series White Paper. Cambridge, Massachussetts: Institute for Healthcare Improvement; 2007. IHI global trigger tool for measuring adverse events. [Google Scholar]
- 21.Tamuz M, Thomas EJ, Franchois KE. Defining and classifying medical error: lessons from patient safety reporting systems. Qual Saf Health Care. 2004;13:13–20. doi: 10.1136/qshc.2002.003376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reason J. Human error: models and management. Br Med J. 2000;320:768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. London: Sage; 1990. [Google Scholar]
- 24.Lydall G, Malik A, Bhugra D. Mental health of applicants seems to be deteriorating. Br Med J. 2007;334:1335. doi: 10.1136/bmj.39254.905764.1F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murray A, Pounder R, Mather H, Black C. Junior doctors’ shifts and sleep deprivation. Br Med J. 2005;330:1404. doi: 10.1136/bmj.330.7505.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmed-Little Y. Implications of shift work for junior doctors. Br Med J. 2007;334:777. doi: 10.1136/bmj.39154.516667.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benger J. Not just about working hours. Br Med J. 2008;336:345. doi: 10.1136/bmj.39486.461250.3A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pounder R. Junior doctors’ working hours: can 56 go into 48? Clin Med. 2008;8:126–7. doi: 10.7861/clinmedicine.8-2-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gander PH, Purnell HM, Garden A, Woodward A. Work patterns and fatigue-related risk among junior doctors. Occup Environ Med. 2007;64:733–8. doi: 10.1136/oem.2006.030916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kara N, Patil PV, Shimi SM. Changes in working patterns hit emergency general surgical training. Ann R Coll Surg Engl. 2008;90(Suppl):60–3. [Google Scholar]
- 31.Grover K, Gatt M, MacFie J. The effect of the EWTD on surgical SpRs: a regional survey. Ann R Coll SurgEngl. 2008;90(Suppl):68–70. [Google Scholar]
- 32.Health Policy & Economic Research Unit. London: British Medical Association; 2008. Mar, BMA survey of junior doctors’ views on working hours and the European Working Time Directive; pp. 1–27. [Google Scholar]
- 33.Horrocks N, Pounder R. Working the night shift: preparation, survival and recovery – a guide for junior doctors. Clin Med. 2006;6:61–7. doi: 10.7861/clinmedicine.6-1-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Czeisler CA, Moore-Ede MC, Coleman RM. Rotating shift work schedules that disrupt sleep are improved by applying circadian principles. Science. 1982;217:460–3. doi: 10.1126/science.7089576. [DOI] [PubMed] [Google Scholar]
- 35.Czeisler CA, Duffy JF, Shanahan TL, Brown EN, Mitchell JF, Rimmer DW, et al. Stability, precision, and near-24-hour period of the human circadian pacemaker. Science. 1999;284:2177–81. doi: 10.1126/science.284.5423.2177. [DOI] [PubMed] [Google Scholar]
- 36.Santhi N, Horowitz TS, Duffy JF, Czeisler CA. Acute sleep deprivation and circadian misalignment associated with transition onto the first night of work impairs visual selective attention. PLoS One. 2007;2:e1233. doi: 10.1371/journal.pone.0001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cappuccio FP, Lockley SW. Safety and the flying doctor. Br Med J. 2008;336:218. [Google Scholar]
- 38.Accreditation Council for Graduate Medical Education. [(Accessed 15 April 2008)];Common Programme Requirements for Residents Duty Hours. http://www.acgme.org/acWebsite/dutyHours/dhComProgrRequirmentsDutyHours0707.pdf.
- 39.Petersen LA, Brennan TA, O'Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72. doi: 10.7326/0003-4819-121-11-199412010-00008. [DOI] [PubMed] [Google Scholar]
- 40.Petersen LA, Orav EJ, Teich JM, O'Neil AC. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Joint Commission J Qual Impr. 1998;24:77–87. doi: 10.1016/s1070-3241(16)30363-7. [DOI] [PubMed] [Google Scholar]
- 41.Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200:538–45. doi: 10.1016/j.jamcollsurg.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 42.Weingart SN, Wilson RMcL, Gibberd RW, Harrison B. Epidemiology of medical error. Br Med J. 2000;320:774–7. doi: 10.1136/bmj.320.7237.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian Adverse Event Study: the incidence of adverse events among hospitals patients in Canada. CMAJ. 2004;170:1678–86. doi: 10.1503/cmaj.1040498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vincent C, Neale G, Woloshymowych M. Adverse events in British hospitals: preliminary retrospective record review. Br Med J. 2001;322:517–9. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Woloshynowych M, Neale G, Vincent C. Case record review of adverse events: a new approach. Qual Saf Health Care. 2003;12:411–5. doi: 10.1136/qhc.12.6.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stickgold R. Sleep-dependent memory consolidation. Nature. 2005;437:1272–8. doi: 10.1038/nature04286. [DOI] [PubMed] [Google Scholar]
- 47.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 48.Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294:1025–33. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- 49.Muir Gray JA. Evidence-based policy making. Br Med J. 2004;329:988–9. doi: 10.1136/bmj.329.7473.988. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.