Abstract
Objective
To estimate the association between ethnicity and discharge destination in older patients with traumatic brain injury (TBI).
Design
A retrospective analysis.
Setting
Nationally representative sample of older patients from the Uniform Data System for Medical Rehabilitation in 2002 and 2003.
Participants
Patients (N=9240) aged 65 years or older who received inpatient rehabilitation services for TBI.
Interventions
Not applicable.
Main Outcome Measures
Discharge destination (home, assisted living facility, institution) and ethnicity (white, black, Hispanic).
Results
Multinomial logit models showed that older Hispanics (odds ratio [OR] = 2.24; 95% confidence interval [CI], 1.66 –3.02) and older blacks (OR=2; 95% CI, 1.55–2.59) with TBI were significantly more likely to be discharged home than older whites with TBI, after adjusting for relevant risk factors. Older blacks were also 78% less likely (OR = .22; 95% CI, .08–.60) to be discharged to an assisted living facility than whites after adjusting for relevant risk factors.
Conclusions
Our findings indicate that older minority patients with TBI were significantly more likely to be discharged home than white patients with TBI. Studies are needed to investigate underlying factors associated with this ethnic difference.
Keywords: Elderly, Ethnic groups, Head injuries, Rehabilitation
Each year approximately 1.5 million people in the United States experience a traumatic brain injury (TBI).1 Although TBI is most prevalent in adolescents and young adult men, the risk is also high in older adults, typically because of falls and other accidents.1–3 Consequences of TBI in older adults can range from mobility and cognitive dysfunction to social isolation.
Most older adults who suffer a moderate to severe TBI are typically referred to an inpatient medical rehabilitation facility for ongoing care. A primary goal of inpatient medical rehabilitation, which can include some combination of physical, occupational, or speech therapy, is to help patients regain functional independence. Many studies4–7 have shown the effectiveness of these rehabilitative therapies, where significant increases in physical and cognitive function have been achieved. However, important outcomes associated with change in physical and cognitive function including discharge destination have not been widely studied in the rehabilitation literature and have been mostly limited to persons with stroke.8–12
Research studies in rehabilitation outcomes have found racial and ethnic differences in patients with TBI.13–16 Rosenthal et al13 reported that, compared with white patients with TBI, minority patients are less involved with family, friends, and recreational activities at 1-year follow-up. Hart et al14 found that black patients with TBI have lower levels of social integration at 1-year follow-up compared with white patients. Arango-Lasprilla et al15 also report Hispanic patients tend to report poorer functional status and lower levels of community integration compared with white patients. However, little is known about whether there are ethnic differences in discharge destination in patients with TBI.
The purpose of this study was to estimate whether ethnicity is associated with discharge destination (home, assisted living facility [ALF], institution) in older white, black, and Hispanic patients with TBI. We focused on persons 65 years and older because this population will be eligible for Medicare, although a small percentage of older adults may have been insured through private insurance because of employment or a purchased secondary policy. We chose this age population to reduce the variability in health insurance coverage among patients less than 65 years of age that might influence discharge planning and setting. We hypothesized that older white patients would report higher functional status and would be more likely to be discharged home than older blacks or Hispanics after inpatient medical rehabilitation.
METHODS
Data Source
The data were from the Uniform Data System for Medical Rehabilitation (UDSMR) for the years 2002 and 2003. The UDSMR dataset includes patients who received inpatient medical rehabilitation services from over 800 rehabilitation facilities in 50 states. It is the largest nongovernmental medical rehabilitation outcome measurement dataset.17 Inpatient evaluation of each patient is conducted within 72 hours of admission and discharge using the Inpatient Rehabilitation Facilities Patient Assessment Instrument (IRF-PAI) developed by the Centers for Medicare & Medicaid Services (CMS). The IRF-PAI includes sociodemographic factors, clinical diagnoses (International Classification of Diseases, Ninth Revision [ICD-9], codes), facility characteristics, prehospitalization data, discharge settings, length of stay (LOS), and functional status. Functional status is measured by the FIM instrument ratings at admission and discharge. Extensive previous research has examined and established the validity and reliability of the FIM instrument.18–22
Study Population
The initial study population included 9825 persons with TBI (CMS Rehabilitation Impairment codes 2.20–2.22) and aged 65 years or older. Persons with TBI were those with unspecified traumatic injury, open head injury, or closed head injury. Because the numbers of Asians, Hawaiians, and Native Americans were small (n=245), they were excluded from the analysis. We further removed 340 people with missing information. A total of 9240 people (94%) had complete information at admission and discharge and were included in the final analysis. The institutional review board granted approval of the study.
Outcome Measure
The outcome measure, discharge destination, was assessed at discharge from inpatient rehabilitation services. Discharge destination was categorized as “home,” “assisted living,” and “institution.” ALFs included board and care, transitional living, and ALF. Institution consisted of intermediate care, skilled nursing facility (SNF), chronic hospital, rehabilitation facility, alternate level of care unit, and subacute settings.
Main Independent Measure
The main independent measure, ethnicity, was obtained from the medical record and was categorized as white (n=8270), black (n=529), and Hispanic (n=441).
Covariates
We included variables that were found to be significantly associated with discharge decision from previous rehabilitation studies as covariates.8–12 These covariates included functional status (motor FIM and cognitive FIM instrument ratings) at discharge, age, sex, marital status, prehospital living settings, LOS, primary insurance, and a comorbidity index. The comorbidity index (range, 0–10) was the total number of comorbidities reported in the medical record.
Statistical Analysis
We examined demographic variables, functional status, and the outcome variable using descriptive and univariate statistics. For continuous variables, the mean and the standard deviation (SD) were reported. For categoric variables, frequencies and percentages were reported. Mantel-Haenszel chi-square analysis was used to examine the differences between the 3 ethnic groups and discharge destination, age, sex, marital status, prehospital living setting, primary insurance, and comorbidity. A 1-way analysis of variance was used to compare differences in LOS, motor FIM, cognition FIM, and total FIM instrument ratings among the 3 ethnic groups.
A number of interactions were tested including ethnicity by age, sex, and marital status. Results showed that these interaction terms were not statistically significant; therefore, only main effects were included in the analyses. Multinomial logit models were used to calculate odds (95% confidence intervals [CIs]) of association between discharge setting and ethnicity. Because the outcome variable was categorized as a 3-level response, we used discharge to institution as the reference group compared with discharge to home and discharge to ALF. We did not compare discharge to home versus discharge to ALF, because these 2 categories share similarities and are community settings.
We first examined the bivariate association between discharge setting and ethnicity (model 1). We next examined this association adjusting for all demographic variables including age, sex, marital status, prehospital living settings, primary insurance, LOS, and comorbidity (model 2). A final model included additional discharge motor FIM instrument rating and cognitive FIM instrument ratings (model 3). All statistical analyses used the SAS systema for Windows and statistical significance (α) was set at the 2-sided .05 level.
RESULTS
The mean age of white, black, and Hispanic patients with TBI was 79.0±7.1 years, 76.9±7.3 years, and 76.7±7.2 years, respectively. Other demographic characteristics are summarized in table 1. Statistical differences among the 3 ethnic groups were found for age (Mantel-Haenszel χ2=40.18, P<.001) and marital status (Mantel-Haenszel χ2=13.27, P=.001). White patients were more likely to be older than either Hispanic or black patients; black patients were least likely to be married (40%). There were no statistically significant differences in terms of sex or prehospital living settings among the 3 ethnic groups.
Table 1.
Demographic and Functional Information for the Study Sample
| Characteristic | White (n=8270) | Black (n=529) | Hispanic (n=441) | Statistics | P |
|---|---|---|---|---|---|
| Age (y), n (%) | χ2=40.18 | <.001 | |||
| 65–74 | 2195 (27) | 205 (39) | 170 (38) | ||
| 75–84 | 3985 (48) | 215 (41) | 179 (41) | ||
| ≥85 | 2090 (25) | 109 (20) | 92 (21) | ||
| Sex, n (%) | χ2=0.52 | .47 | |||
| Male | 4359 (53) | 273 (52) | 244 (55) | ||
| Female | 3911 (47) | 256 (48) | 197 (45) | ||
| Marital status, n (%) | χ2=13.27 | <.001 | |||
| Married | 4304 (52) | 209 (40) | 215 (49) | ||
| Not married | 3966 (48) | 320 (60) | 226 (51) | ||
| Prehospital living settings, n (%) | χ2=0.38 | .54 | |||
| Home | 7839 (95) | 506 (96) | 420 (95) | ||
| Assisted living | 314 (4) | 9 (1) | 9 (2) | ||
| Institution | 117 (1) | 14 (3) | 12 (3) | ||
| Primary insurance (%) | χ2=32.74 | <.001 | |||
| Medicare | 7477 (90.4) | 459 (87) | 353 (80.0) | ||
| Medicaid | 13 (0.2) | 16 (3) | 24 (5.5) | ||
| Private insurance | 688 (8.3) | 42 (8) | 50 (11.3) | ||
| Other | 92 (1.1) | 12 (2) | 14 (3.2) | ||
| LOS (d) | F=4.57 | .01 | |||
| Mean ± SD | 15.6±9.7 | 16.4±10.3 | 16.8±11.5 | ||
| Median | 14 | 14 | 14 | ||
| FIM at discharge | |||||
| Motor | 58.6±18.7 | 54.1±20.5 | 57.5±20.2 | F=14.44 | <.001 |
| Cognition | 23.1±7.8 | 21.1±8.2 | 22.4±7.9 | F=18.15 | <.001 |
| Total | 81.8±24.7 | 75.2±27.1 | 79.9±26.2 | F=17.81 | <.001 |
| Comorbidity, n (%) | χ2=39.17 | <.001 | |||
| 0 | 216 (3) | 34 (6) | 25 (6) | ||
| 1–3 | 699 (8) | 76 (14) | 44 (10) | ||
| >3 | 7355 (89) | 419 (80) | 372 (84) |
NOTE. Values are mean ± SD or as indicated.
White patients had the highest motor FIM, cognition FIM, and total FIM instrument ratings at discharge, followed by Hispanic and black patients (P<.001). A similar pattern was found for LOS, for which white patients had the shortest stay of 15.6±9.7 days (F=4.57, P=.01). White patients were also more likely (89%) to have 3 or more comorbidities (Mantel-Haenszel χ2=39.17, P<.001) and Medicare (90.5%) as primary insurance (Mantel-Haenszel χ2=32.74, P<.001) than either blacks or Hispanics.
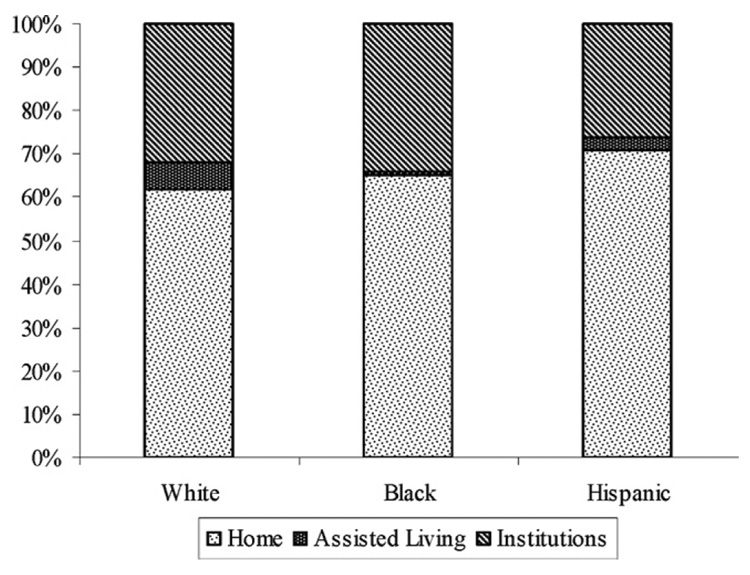
The unadjusted distribution of discharge destination among the 3 ethnic groups (fig 1) showed that Hispanics were more likely to be discharged home (71%) than either blacks (65%) or whites (62%). Six percent of white patients were discharged to an ALF compared with 3% of Hispanic and 1% of black patients. Black patients had the highest percentage (34%) of institutionalization.
Fig 1.
Distribution of discharge destination by race and ethnicity.
Results from a multinomial logit model are presented in table 2. In the unadjusted model (model 1, with discharge to institution as the referent), Hispanic patients were 42% more likely to be discharged home (odds ratio [OR]=1.42; 95% CI, 1.14 –1.77) than white patients. In model 2, after adjusting for demographic and health-related variables (age, sex, martial status, prehospital living setting, primary insurance, LOS, comorbidity), Hispanics remained 42% (OR=1.42; 95% CI, 1.13–1.78) more likely to be discharged home than white patients. When further adjustments were made for functional status (discharge motor and cognitive FIM ratings) (model 3), Hispanic patients were 2.24 times (OR=2.24; 95% CI, 1.66–3.02) as likely to be discharged home as white patients, and black patients were twice (OR=2, 95% CI, 1.55–2.59) as likely to be discharged home.
Table 2.
Multinomial Logit Models Examining Discharge Destination by Ethnicity
| Model 1 |
Model 2 |
Model 3 |
||||
|---|---|---|---|---|---|---|
| Characteristic | Home vs Institution | Assisted Living vs Institution | Home vs Institution | Assisted Living vs Institution | Home vs Institution | Assisted Living vs Institution |
| Ethnicity | ||||||
| Black | 1.00 (0.83–1.21) | 0.16 (0.07–0.40)* | 1.02 (0.84–1.24) | 0.16 (0.06–0.40)* | 2.00 (1.55–2.59)* | 0.22 (0.08–0.60)* |
| Hispanic | 1.42 (1.14–1.77)* | 0.61 (0.34–1.12) | 1.42 (1.13–1.78)* | 0.61 (0.32–1.14) | 2.24 (1.66–3.02)* | 0.86 (0.44–1.68) |
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Age | 0.97 (0.97–0.98) | 1.02 (1.01–1.04) | 0.99 (0.99–1.00) | 1.04 (1.03–1.06)* | ||
| Sex | ||||||
| Male | 0.77 (0.70–0.85) | 0.98 (0.79–1.22) | 0.85 (0.75–0.96)* | 1.03 (0.82–1.30) | ||
| Female | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Marital status | ||||||
| Not married | 0.68 (0.62–0.75) | 2.45 (1.90–3.14) | 0.45 (0.40–0.51)* | 1.74 (1.34–2.27)* | ||
| Married | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Prehospital living settings | ||||||
| Home | 3.29 (2.29–4.71) | 0.88 (0.46–1.70) | 2.88 (1.83–4.55)* | 0.78 (0.39–1.56) | ||
| Assisted living | 0.57 (0.35–0.93) | 5.41 (2.73–10.71) | 0.66 (0.37–1.20) | 6.35 (3.04–13.29)* | ||
| Institution | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Primary insurance | ||||||
| Other | 1.40 (0.90–2.19) | 2.20 (0.88–5.55) | 1.23 (0.70–2.17) | 1.88 (0.69–5.12) | ||
| Private | 1.00 (0.85–1.19) | 1.03 (0.69–1.55) | 1.01 (0.81–1.25) | 1.03 (0.68–1.58) | ||
| Medicaid | 0.87 (0.47–1.59) | 1.39 (0.31–6.29) | 1.01 (0.45–2.28) | 1.45 (0.29–7.28) | ||
| Medicare | 1.00 | 1.00 | 1.00 | 1.00 | ||
| LOS | 0.99 (0.99–1.00) | 1.02 (1.01–1.03) | 1.00 (1.00–1.01) | 1.03 (1.02–1.04)* | ||
| Comorbidity | ||||||
| 1–3 | 1.38 (1.03–1.86) | 1.39 (0.67–2.88) | 1.09 (0.73–1.63) | 1.25 (0.57–2.74) | ||
| >3 | 1.41 (1.09–1.82) | 1.49 (0.79–2.82) | 1.35 (0.95–1.93) | 1.58 (0.79–3.16) | ||
| None | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Functional status at discharge | ||||||
| Motor FIM | 1.09 (1.08–1.09)* | 1.09 (1.08–1.10)* | ||||
| Cognition FIM | 1.04 (1.03–1.05)* | 0.99 (0.98–1.01) | ||||
Results were statistically significant, with 95% CI excluding 1.
We also compared discharge to ALF by ethnic group (with discharge to institution as the referent). In the unadjusted model (model 1), black patients were 84% less likely to be discharged to an ALF (OR=.16; 95% CI, .07–.40) than white patients. The results were similar (model 2) when we added demographic and health-related variables to the model (model 2) (OR=.16; 95% CI, .06–.40). With the addition of functional status, black patients were 78% less likely (OR=.22; 95% CI, .08 –.60) to be discharged to an ALF than white patients. Non-significant differences were found between Hispanic and white patients on discharge to an ALF.
Results of a multinomial logit model indicated that FIM motor and cognitive ratings, age, sex, martial status, prehospital living settings, and LOS were significantly associated with discharge settings (see table 2). Each 1-point increase in FIM motor rating was associated with a 9% increase in the odds of being discharged home or to an ALF. Each 1-point increase in FIM cognition rating was associated with a 4% increase in the odds of being discharged to home. Each 1-year increase in age was significantly associated with being discharged to an ALF (OR=1.04; 95% CI, 1.03–1.06). Male patients were 15% less likely to be discharged home (OR=.85; 95% CI, .75–.96) than female patients. Patients who were not married were 55% less likely (OR=.45; 95% CI, .40 –.51) to return home and 74% more likely (OR=1.74; 95% CI, 1.34–2.27) to go to an ALF than those who were married. Patients who were admitted from home were 2.88 times (OR=2.88; 95% CI, 1.83–4.55) more likely to return home, whereas patients who came from ALFs were 6.35 times (OR=6.35; 95% CI, 3.04–13.29) more likely to be discharged to an ALF. Each 1-day increase in LOS was associated with a 3% increase in the odds of being discharged to an ALF (OR=1.03; 95% CI, 1.02–1.04).
DISCUSSION
The aim of this study was to examine the association between ethnicity and discharge destination in older patients with TBI. Our results showed that ethnicity was significantly associated with discharge destination. Hispanic and black patients were twice as likely to be discharged home as their white counterparts after controlling for relevant risk factors. Black patients were significantly less likely than white patients to be discharged to an ALF compared with an institution. We found that approximately 30% of patients with TBI were discharged to institutions including subacute care facilities, SNFs, inter-mediate care units, and acute care units. This finding suggested that although patients with TBI benefited from inpatient rehabilitation programs, one third of them required further rehabilitation or specialized care.
Previous studies have shown that functional status at discharge is a major factor associated with discharge planning.8–10 In the current study, white patients with TBI had the highest total FIM, motor FIM, and cognition FIM instrument ratings at discharge compared with blacks and Hispanics. However, and contrary to our hypothesis, we found the odds were more than 2 times as great that black and Hispanic patients would be discharged home as white patients after adjusting for relevant risk factors.
One possible explanation is that going home is culturally and socially important to older minority patients and their families. Home is a symbol of independence, privacy, and competence. 23–25 Families in minority populations may prefer caring for an older adult with physical and cognitive disabilities at home rather than seeing him/her institutionalized. In the Hispanic culture, the elderly play a central role in the family and are treated with respect, status, and authority by other family members.26 Conversely, white patients and their families may be more open to alternative choices such as board and care homes or ALFs as a transitional stage for further rehabilitation programs.
Financial resources also may be another major determinant of discharge setting. Minority elderly frequently have lower incomes than their white counterparts.27 The average out-of-pocket cost for staying in an ALF is about $2100 to $2900 a month,28 which could pose a financial barrier for older minority patients and their families. This may explain why only 1% of black and 3% of Hispanic older patients with TBIs were discharged to an ALF in our study. Although the percentage of minority older patients discharged to an ALF was small, it provided an opportunity to explore differences in discharge decision among ethnic groups.
Results from the unadjusted distribution of discharge destination indicated that black patients with TBI had the highest percentage (34%) of institutionalization. The FIM motor and cognition ratings at discharge in older black patients with TBI were the lowest among the 3 ethnic groups (see table 1); these patients may require a longer recovery process from injury than the other 2 ethnic groups.
Study Limitations
The current study has a number of limitations. First, although the study sample from the UDSMR database has been found to be representative of rehabilitation facilities providing services to patients who receive Medicare,29 there is a possible bias with sample selection. Previous studies show that each year approximately 80% of patients with TBI visit emergency departments and are released home without further medical treatment needed.2 Only about 20% of patients with TBI require hospitalization, and 7.7% of these patients are transferred to inpatient rehabilitation programs.30,31 Persons aged 75 years and older with TBI are the most frequently admitted to hospitals for medical care. They have to meet specific criteria to receive inpatient medical rehabilitation services. These admission criteria are associated with age, functional status, secondary complications, comorbidities, ability to tolerate 3 hours a day of rehabilitation, and physician referral.32–34 Thus, less than 5% of patients hospitalized with TBI under coverage of Medicare would receive inpatient rehabilitation services.
Williams et al35 report significant regional differences in outcomes and health care utilization in patients with ischemic stroke. We could expect a similar issue with regional variation of access to rehabilitation services to exist among patients with TBI. However, this will require further investigation. There may also be interactions between regional variation and ethnic and racial status. These are important areas for future investigation.
Another limitation of the study is that the database we used was intended for clinical assessment; information on personal income, education, occupation, social network, or numbers of caregivers was not included. The database included standard ICD-9 codes, but lacked detailed information, such as neuroimaging, regarding the type and severity of injury. Further studies are needed to examine the relationship between types or severity of injury, race and ethnicity, and outcome.
CONCLUSIONS
We found ethnic differences in discharge destination for community-dwelling older patients with TBI. Contrary to our hypothesis, minorities including blacks and Hispanics were significantly more likely to be discharged home than their white counterparts, even though whites had higher functional status at discharge. Future studies are needed to examine factors such as social support or financial resources that may interact with ethnicity and influence discharge destination.
Acknowledgments
Supported by the National Institutes of Health, U.S. Department of Health and Human Services (grant nos. K02-AG019736, K01-HD046682, R01-AG024806).
Footnotes
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
Supplier
a. Version 9.1; SAS Institute, 100 SAS Campus Dr, Cary, NC 27513-2414.
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Accessed June 30, 2006];What is traumatic brain injury? Available at: http://www.cdc.gov/ncipc/tbi/TBI.htm.
- 2.Langlois JA, Rutland-Brown W, Thomas KE. [Accessed July 26, 2006];Atlanta: Centers for Disease Control and Prevention; Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. 2004 Available at: http://www.cdc.gov/ncipc/tbi/SL/TBI/TBI777_files/textonly/start-TBI.html.
- 3.Bruns J, Jr, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia. 2003;44 Suppl 10:2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 4.Rapoport MJ, Feinstein A. Outcome following traumatic brain injury in the elderly: a critical review. Brain Inj. 2000;14:749–761. doi: 10.1080/026990500413777. [DOI] [PubMed] [Google Scholar]
- 5.Flanagan SR, Hibbard MR, Riordan B, Gordon WA. Traumatic brain injury in the elderly: diagnostic and treatment challenges. Clin Geriatr Med. 2006;22:449–468. doi: 10.1016/j.cger.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Gan BK, Lim JH, Ng IH. Outcome of moderate and severe traumatic brain injury amongst the elderly in Singapore. Ann Acad Med Singapore. 2004;33:63–67. [PubMed] [Google Scholar]
- 7.Cruise CM, Sasson N, Lee MH. Rehabilitation outcomes in the older adults. Clin Geriatr Med. 2006;22:257–267. doi: 10.1016/j.cger.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Bottemiller KL, Bieber PL, Basford JR, Harris M. FIM score, FIM efficiency, and discharge disposition following inpatient stroke rehabilitation. Rehabil Nurs. 2006;31:22–25. doi: 10.1002/j.2048-7940.2006.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 9.van Boxel YJ, Bergen MP, de Beer MC, Stam HJ. Discharge accommodation decisions for stroke patients after hospital-based inpatient rehabilitation. J Rehabil Sci. 1996;9:11–15. [Google Scholar]
- 10.Mauthe RW, Haaf DC, Hayn P, Krall JM. Predicting discharge destination of stroke patients using a mathematical model based on six items from the Functional Independence Measure. Arch Phys Med Rehabil. 1996;77:10–13. doi: 10.1016/s0003-9993(96)90212-9. [DOI] [PubMed] [Google Scholar]
- 11.Lutz BJ. Determinants of discharge destination for stroke patients. Rehabil Nurs. 2004;29:154–163. doi: 10.1002/j.2048-7940.2004.tb00338.x. [DOI] [PubMed] [Google Scholar]
- 12.Neufeld SW, Lysack CL, Macneill SE, Lichtenberg PA. Living arrangements decisions at discharge and later: differences in criteria and outcomes. Home Health Care Serv Q. 2004;23:29–47. doi: 10.1300/J027v23n04_03. [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal M, Dijkers M, Harrison-Felix C, Nabors N, Witol AD, Young ME. Impact of minority status on functional outcome and community integration following traumatic brain injury. J Head Trauma Rehabil. 1996;11:40–57. [Google Scholar]
- 14.Hart T, Whyte J, Polansky M, Kersey-Matusiak G, Fidler-Sheppard R. Community outcomes following traumatic brain injury: impact of race and preinjury status. J Head Trauma Rehabil. 2005;20:158–172. doi: 10.1097/00001199-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Arango-Lasprilla JC, Rosenthal M, DeLuca J, Cifu DX, Hanks R, Komaroff E. Functional outcomes from inpatient rehabilitation after traumatic brain injury: how do Hispanics fare? Arch Phys Med Rehabil. 2007;88:11–18. doi: 10.1016/j.apmr.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 16.Burnett DM, Kolakowsky-Hayner SA, Slater D, et al. Ethno-graphic analysis of traumatic brain injury patients in the national Model Systems database. Arch Phys Med Rehabil. 2003;84:263–267. doi: 10.1053/apmr.2003.50091. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton BB, Granger CV, Sherwin FS, Zielezny M, Tashman JS. A uniform national data system for medical rehabilitation. In: Fuhrer M, editor. Rehabilitation outcomes: analysis and measurement. Baltimore: PH Brookes; 1987. pp. 137–150. [Google Scholar]
- 18.Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger CV. Prediction of rehabilitation outcomes with disability measures. Arch Phys Med Rehabil. 1994;75:133–143. [PubMed] [Google Scholar]
- 19.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatient. Arch Phys Med Rehabil. 1993;74:531–536. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 20.Granger CV, Cotter AC, Hamilton BB, Fiedler RC. Functional assessment scales: a study of persons after stroke. Arch Phys Med Rehabil. 1993;74:133–138. [PubMed] [Google Scholar]
- 21.Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level functional independence measure (FIM) Scand J Rehabil Med. 1994;26:115–119. [PubMed] [Google Scholar]
- 22.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 23.Unsworth C. Clients’ perception of discharge housing decisions after stroke rehabilitation. Am J Occup Ther. 1996;50:207–216. doi: 10.5014/ajot.50.3.207. [DOI] [PubMed] [Google Scholar]
- 24.Swenson MM. The meaning of home to five elderly women. Health Care Women Int. 1998;19:381–393. doi: 10.1080/073993398246160. [DOI] [PubMed] [Google Scholar]
- 25.Roush CV, Cox JE. The meaning of home: how it shapes the practice of home and hospice care. Home Healthc Nurse. 2000;18:388–394. doi: 10.1097/00004045-200006000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Paz JJ. Support of Hispanic elderly. In: McAdoo HP, editor. Family ethnicity. Newbury Park: Sage; 1993. pp. 177–190. [Google Scholar]
- 27.American Association of Retired Persons. [Accessed July 31, 2006];A portrait of older minorities. Available at: http://www.aarp.org/research/reference/minorities/aresearch-import-509.html.
- 28.American Association of Retired Persons. [Accessed July 6, 2006];Assisted living in the United States. Available at: http://www.aarp.org/research/housing-mobility/assistedliving/assisted_living_in_the_united_states.html.
- 29.Carter GM, Buchanan JL, Donyo Y, Inkelas M, Spritzer KL. A prospective payment system for inpatient rehabilitation. Santa Monica: Rand; 1997. National Technical Information Service No. PB98-106024. [Google Scholar]
- 30.Centers for Disease Control and Prevention. Rates of hospitalization related to traumatic brain injury—nine states, 2003. MMWR Morb Mort Wkly Rep. 2007;56(8):167–170. [PubMed] [Google Scholar]
- 31.Thurman D, Guerrero J. Trends in hospitalization associated with traumatic brain injury. JAMA. 1999;282:954–957. doi: 10.1001/jama.282.10.954. [DOI] [PubMed] [Google Scholar]
- 32.Wrigley JM, Yoels WC, Webb CR, Fine PR. Social and physical factors in the referral of people with traumatic brain injuries to rehabilitation. Arch Phys Med Rehabil. 1994;75:149–155. [PubMed] [Google Scholar]
- 33.Haas JF. Admission to rehabilitation centers: selection of patients. Arch Phys Med Rehabil. 1988;69 329-3. [PubMed] [Google Scholar]
- 34.Foster M, Flemin J, Tilse C, Rosenman L. Referral to post-acute care following traumatic brain injury (TBI) in the Australian context. Brain Inj. 2000;14:1035–1045. doi: 10.1080/02699050050203531. [DOI] [PubMed] [Google Scholar]
- 35.Williams LS, Echert GJ, L’italien GJ, Lapuerta P, Weinberger M. Regional variation in health care utilization and outcomes in ischemic stroke. J Stroke Cerebrovasc Dis. 2003;12:259–265. doi: 10.1016/j.jstrokecerebrovasdis.2003.09.008. [DOI] [PubMed] [Google Scholar]