Abstract
Eosinophilic pancreatitis (EP) is a rare disease. It typically occurs in the setting of either eosinophilic gastroenteritis or the hypereosinophilic syndrome. Isolated eosinophilic infiltration of the pancreas is less common. EP usually presents as a pancreatic tumour with abdominal pain and/or obstructive jaundice. The diagnosis is often not made until after pancreatic resection under suspicion of a pancreatic tumour.
The case of a 14-year-old boy whose initial presentation was suggestive of a pancreatic tumour is reported. Radiological evaluation revealed a pancreatic mass suggestive of a pancreatic tumour obstructing the duodenum and common bile duct. The patient underwent surgery and a gastrojejunal anostomosis, tube cholecystostomy and biopsy were performed with no postoperative complications. The diagnosis of EP was established after surgical biopsy. The biopsy specimen revealed prominent eosinophilic infiltration. Serum immunoglobulin E levels were elevated. The patient was treated with oral prednisolone (40 mg/day). After two months of oral steroid therapy, clinical manifestations rapidly improved and peripheral eosinophilia subsided. Computed tomography scan revealed remission of the pancreatic mass-like lesion.
Keywords: Eosinophilic gastroenteritis, Eosinophilic pancreatitis, Hypereosinophilic syndrome
Abstract
La pancréatite à éosinophiles (PÉ) est une maladie rare. D’ordinaire, elle se déclare en présence d’une gastroentérite à éosinophiles ou d’un syndrome hyperéosinophilique. L’infiltration éosinophilique isolée du pancréas est moins courante. En général, la PÉ a l’aspect d’une tumeur pancréatique accompagnée de douleurs abdominales ou d’une jaunisse obstructive. Souvent, le diagnostic n’est pas posé avant la résection du pancréas justifiée par une présomption de tumeur du pancréas.
Est décrit le cas d’un garçon de 14 ans dont la présentation initiale était évocatrice d’une tumeur du pancréas. L’évaluation radiologique a révélé une masse pancréatique laissant supposer la présence d’une tumeur pancréatique obstruant le duodénum et le canal cholédoque. Le patient a été opéré; une anastomose gastrojénunale, une cholécystostomie et une biopsie ont été exécutées, sans complications postopératoires. Le diagnostic de PÉ a été posé après une biopsie chirurgicale. Le prélèvement biopsique a révélé une importante infiltration à éosinophiles. Les taux d’immunoglubiline E sérique étaient élevés. Le patient a reçu de la prednisone par voie orale (40 mg/jour). Après deux mois de corticothérapie par voie orale, les manifestations cliniques se sont rapidement atténuées, et l’éosinophilie périphérique s’est résorbée. La tomodensitométrie a révélé une rémission de la lésion pancréatique à l’allure de masse.
Eosinophilic infiltration is quite rare in the pancreas (1–4). Usually, the diagnosis cannot be made unless the pancreas undergoes resection for a suspected pancreatic tumour (1,3,5). The syndrome is generally accompanied by eosinophilic gastroenteritis or the hypereosinophilic syndrome (3). Isolated eosinophilic infiltration in the pancreas is a more rarely encountered entity (3). In the present study, a patient admitted to Karadeniz Technical University, Medical Faculty, Department of Pediatric Surgery clinic (Turkey) with complaints of vomiting and jaundice and diagnosed with eosinophilic pancreas is presented and discussed in the light of information in literature.
CASE PRESENTATION
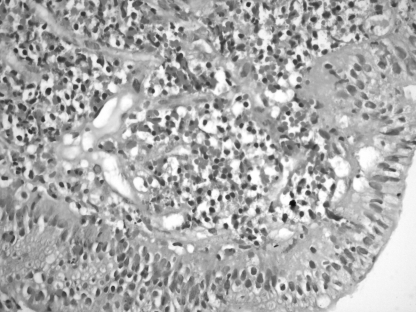
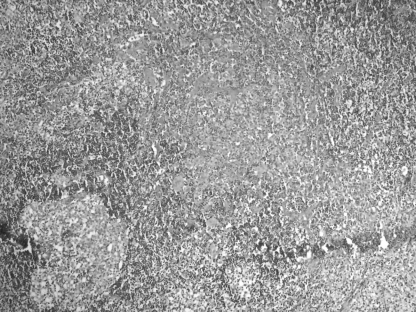
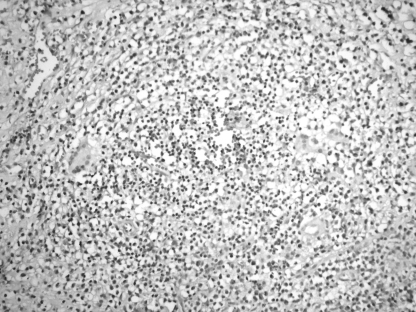
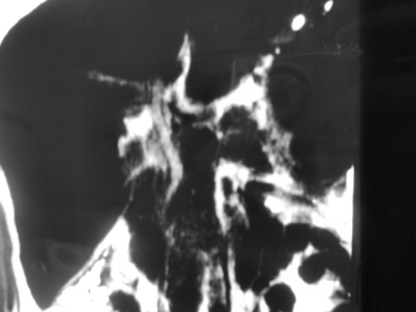
A 14-year-old male patient was admitted to Karadeniz Technical University, Medical Faculty, Department of Pediatric Surgery clinic (Turkey) with complaints of vomiting, abdominal pain and jaundice. He had been suffering from intermittent abdominal pain above the umbilical region appearing after meals, which had been persisting for a year and a half. The patient rarely vomited previously but the frequency of postprandial vomiting that contained food contents increased and he began to vomit following every meal in the three days before admission. In addition, the patient developed jaundice 10 days before admission. During his physical examination, a mass of approximately 4 cm × 3 cm was palpated above the umbilicus. Complete blood count showed a hemoglobin of 120.1 g/L, leukocyte count of 21.6×109 and erythrocyte sedimentation rate of 85 mm/h. The serum biochemistry showed an aspartate aminotransferase of 249 U/L, alanine aminotransferase of 388 U/L, amylase of 593 U/L, lactate dehydrogenase of 386 U/L, gamma-glutamyl transpeptidase of 471 U/L, alkaline phosphatase of 1180 U/L, total bilirubin of 155.61 μmol/L and direct bilirubin of 119.7 μmol/L. In the abdominal ultrasonography, the gall bladder was 96 mm × 34 mm with a hydropic appearance and a proximally dilated main bile duct. The right and left hepatic ducts were also dilated. A relatively well-demarcated 19 mm × 13 mm mass was observed in the head of the pancreas. The width of the main pancreatic duct was measured as 2.3 mm in the corporal segment. In the computed tomography (CT) scan, the liver was found to be enlarged and the intrahepatic and the main bile ducts were found to be dilated up to the level of the pancreatic head. A larger-than-normal pancreatic head, suggesting cancer of the pancreatic head, and a few lymph nodes in the mesentery were observed (Figure 1). In the CT cholangiography, a stricture of the main bile duct at the level of the pancreatic head and dilation of the more proximal main and intrahepatic bile ducts were observed (Figure 2). The patient underwent an operation for the suspected mass in the pancreatic head. Before laparotomy, gastroduodenoscopy was performed under general anesthesia, during which the second segment of duodenum was reached and both the second segment of the duodenum and ampulla of Vater were found to be edematous, irregular and fragile; in addition, the intestinal lumen was narrowed, while the stomach was normal. Biopsy specimens were obtained from the ampulla of Vater and the second segment of the duodenum. Later, laparotomy was performed and the pancreatic mass was exposed. The surface of the mass was irregular, adherent to surrounding tissues, fragile and hemorrhageous. The gall bladder was severely hydropic. The mass was found to surround the second segment of the duodenum, hepatic hilus and the large vessels in a manner that prevented resection. Several excisional biopsy specimens were obtained from the mass. In the examination of perioperative biopsy specimens, no neoplastic structure was found. Gastrojejunostomy and tube cholecystotomy were performed with no postoperative complications. In the histopathological examination of tissue specimens taken from the duodenum during gastroduodenoscopy, edematous villus structures and dense mixed inflammatory cell infiltration including polymorphonuclear leukocytes rich in eosinophils within the lamina propria were observed, while no sign of neoplasm was detected (Figure 3). In the specimens obtained from mesenteric lymph nodes, dense eosinophilic infiltration was observed (Figure 4). In the examination of tissue samples taken from the mass, fibrosis, eosinophilic microabcess-forming chronic purulent inflammation and lymph nodes with giant cell reaction were observed (Figure 5). The investigation conducted for suspected eosinophilic pancreatitis (EP) revealed the immunoglobulin (Ig) E level as 1767 U/mL (normal values greater than 240 U/mL) and the leukocyte profile showed prominent eosinophilia. Methylprednisolone treatment at a double dose of 20 mg was initiated. In the follow-up CT performed two months later, the mass lesion was found to have shrunk (Figure 6). In the follow-up cholangiography, the dilated biliary ducts were found to have returned to normal (Figure 7). The cholecystotomy tube was removed on the 33rd day once the bile drainage completely ceased. During the follow-ups of the patient every three months, no complications were observed.
Figure 1).
Contrast-enhanced axial computed tomography scan showing a mass in the pancreatic head
Figure 2).
A computed tomography cholangiography image, showing a narrowing in the main bile duct at the level of the pancreatic head. The intrahepatic bile ducts are dilated
Figure 3).
Biopsy of the duodenum revealing significant eosinophilic infiltration in the lamina propria
Figure 4).
Significant eosinophilic infiltration seen in a biopsy specimen obtained from the lymph node
Figure 5).
Significant eosinophilic infiltration seen in a biopsy specimen obtained from the mass
Figure 6).
Post-treatment computed tomography scan showing the disappearance of the mass in the pancreatic head
Figure 7).
Computed tomography cholangiography scan showing the normalization of the narrowing in the main bile duct
DISCUSSION
EP is a rare disease (1–4). The patients usually present with complaints of a pancreatic mass due to eosinophilic inflammatory infiltration and accompanying obstructive jaundice (6). The diagnosis is difficult and usually made following surgery performed for a suspected pancreatic tumour (1,3,6). Cases of false-positive pancreas resection due to this disease have been reported (1). Likewise, the diagnosis in our case was made after histopathological examination of the tissue specimens obtained surgically. The etiology of EP has not been fully understood. Neoplasias, parasitic infestations, hypersensitivity to drugs such as carbamezepine and atopic diseases have been proposed as underlying causes of EP (1). Flejou et al (4) have suggested that the high IgE levels in the case they presented was indicative of allergic mechanisms being responsible for the disease. In veterinary literature, EP has been reported in horses infested by Strongylus equines, in dogs infested by Toxocaria canis and in horses with T-cell lymphoma (1). Our patient had no history of drug use or allergy, but amoebic cysts and trophozooids were found in his stool. Majority of cases with EP have eosinophilia in peripheral blood, increased serum IgE levels and/or eosinophilic infiltration in the gastrointestinal system (1). Likewise, our patient had peripheral eosinophilia and IgE levels were seven times the upper limit of normal. Eosinophilic infiltration of the pancreas was observed in the background of eosinophilic gastroenteritis or hypereosinophilic syndrome (1,3). Eosinophilic gastroenteritis is eosinophilic infiltration of the digestive system (4,7). The stomach and jejunum are involved in majority of the cases (7). Le Connie et al (7) have reported the following diagnostic criteria for eosinophilic gastroenteritis: the presence of digestive system symptoms such as abdominal pain, vomiting, diarrhea; a biopsy result indicative of eosinophilic infiltration in the intestinal wall ruling out the presence of a parasite; and absence of involvement outside the digestive system. Although our patient had vomiting and abdominal pain, he did not have diarrhea. Hence, we suggest that the vomiting was due to the stricture of duodenum caused by the pancreatic mass surrounding it as opposed to digestive system involvement. Though eosinophilic infiltration in the lamina propria was observed in biopsies taken from the second segment of duodenum during preoperative gastroduodenoscopy, the stomach was normal. We therefore suggest that the infiltration in the duodenum was secondary to the pancreatic mass. Also, an amoebic infestation was detected in our patient. Criteria for the hypereosinophilic syndrome are as follows: the presence of an eosinophil count greater than 1.5×109/L for more than six months; presence of allergic situations such as rhinitis and bronchial asthma; involvement of other organs such as the skin, heart and the digestive system; and absence of eosinophilia causes such as parasitic infestations or leukemia (1). The case we present does not meet the criteria for eosinophilic gastroenteritis or the hypereosinophilic syndrome. We consider this case to be an isolated eosinophilic infiltration of the pancreas. To our knowledge, this is the first report of a case in the pediatric age group. Review of related literature reveals that almost every patient reported had responded considerably well to steroid treatment. Likewise, the mass in our patient disappeared two months following the initiation of methylprednisolone treatment at a dose of 40 mg/day. If EP could have been diagnosed preoperatively, the patient would have been treated without the need for surgery. However, our case could only be diagnosed postoperatively.
Despite the fact that EP is a rare disease, it should be considered in the differential diagnosis in patients in the pediatric age group presenting with a pancreatic mass and findings of obstructive jaundice, vomiting and diarrhea. In such cases, the eosinophil count and IgE levels should be investigated.
REFERENCES
- 1.Abraham SC, Leach S, Yeo CJ, et al. Eosinophilic pancreatitis and increased eosinophils in the pancreas. Am J Surg Pathol. 2003;27:334–42. doi: 10.1097/00000478-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Barthet M, Hastier P, Buckley MJ. Eosinophilic pancreatitis mimicking pancreatic neoplasia: EUS and ERCP findings – is nonsurgical diagnosis possible? Pancreas. 1998;17:419–22. [PubMed] [Google Scholar]
- 3.Euscher E, Vaswani K, Frankel W. Eosinophilic pancreatitis: A rare entity that can mimic a pancreatic neoplasm. Ann Diagn Pathol. 2000;4:379–85. doi: 10.1053/adpa.2000.19371. [DOI] [PubMed] [Google Scholar]
- 4.Flejou JF, Potet F, Bernades P. Eosinophilic pancreatitis: A rare manifestation of digestive allergy? Gastroenterol Clin Biol. 1989;13:731–3. [PubMed] [Google Scholar]
- 5.O’Toole D, Palazzo L, Vullierme MP, Maire F, Levy P, Ruszniewski P. Bile duct obstruction caused by an eosinophilic papillary pseudotumor. Gastrointest Endosc. 2003;58:445–8. doi: 10.1067/s0016-5107(03)00027-0. [DOI] [PubMed] [Google Scholar]
- 6.Maeshima A, Murakami H, Sadakata H, et al. Eosinophilic gastroenteritis presenting with acute pancreatitis. J Med. 1997;28:265–72. [PubMed] [Google Scholar]
- 7.Le Connie D, Nguyen H. Eosinophilic gastroenteritis, ascites, and pancreatitis: A case report and review of the literature. South Med J. 2004;97:905–6. doi: 10.1097/01.SMJ.0000139403.55785.1C. [DOI] [PubMed] [Google Scholar]