Abstract
Dieulafoy’s ulcer is a rare cause of gastrointestinal bleeding. The lesion is usually located in the stomach, although it may occur anywhere in the gastrointestinal tract. A 44-year-old man was admitted to hospital due to cerebral infarction. On the 23rd day of hospitalization, he showed massive hematochezia. He underwent an urgent colonoscopy. There was a visible protuberant vessel without significant ulceration at the fundus of the rectum, consistent with a Dieulafoy’s ulcer. It was treated by endoscopic hemoclipping. However, rebleeding occurred three times despite repeated hemoclipping. Finally, endoscopic band ligation was successfully performed to achieve permanent hemostasis. Endoscopic band ligation is an effective treatment for bleeding rectal Dieulafoy’s ulcer.
Keywords: Dieulafoy’s ulcer, Endoscopic band ligation, Rectum
Abstract
L’ulcère de Dieulafoy est une rare cause de saignements gastrointestinaux. La lésion se trouve généralement dans l’estomac, mais elle peut se manifester n’importe où dans le tube digestif. Un homme de 44 ans a été hospitalisé en raison d’un infarctus cérébral. Le 23e jour de son hospitalisation, il a présenté une émission massive de selles sanglantes. Il a subi une coloscopie d’urgence. On constatait une protubérance des vais-seaux sans ulcération significative au fond du rectum, caractéristique d’un ulcère de Dieulafoy. On l’a traité à l’aide de pinces hémostatiques endoscopiques. Cependant, de nouveaux saignements se sont produits trois fois, malgré l’application répétée de pinces hémostatiques. Enfin une ligature élastique endoscopique a permis d’obtenir une hémostase permanente. La ligature élastique endoscopique est un traitement efficace de l’ulcère rectal hémorragique de Dieulafoy.
Dieulafoy’s ulcer is an uncommon lesion that usually presents with massive bleeding. This lesion is a dilated aberrant sub-mucosal vessel which erodes the overlying epithelium in the absence of a primary ulcer (1). The typical endoscopic appearance is an abnormally large submucosal artery that protrudes through a solitary small mucosal defect. Histologically, it is defined as a thick-walled arterial vessel surrounded by a very shallow ulcer without the evidence of aneurysm formation, atherosclerosis, arteritis or inflammation. Dieulafoy’s ulcers are usually found in the stomach, predominantly lying in the proximal one-third of the lesser curvature (2). Similar lesions have been reported throughout the rest of the gastrointestinal (GI) tract, including the esophagus, duodenum (1,3–5), jejunum (6), colon (7–9) and rectum (10–33). To date, 30 cases of rectal Dieulafoy’s ulcer have been reported in English medical literature. We report a case that was successfully treated with endoscopic band ligation after incomplete hemostasis with endoscopic hemoclipping.
CASE PRESENTATION
A 44-year-old man was admitted to hospital for a sudden disturbance of consciousness. He had a past medical history of hypertension, hyperlipidemia, diabetes mellitus and fatty liver. He had never previously experienced GI bleeding, colonic polyps or neoplasm. On admission, he was in a state of right hemiplegia, anarthria and consciousness disorder (Japan coma scale I: 2 to 3), as a result of a cerebral infarction due to the occlusion of the left internal carotid artery as demonstrated on computed tomography and magnetic resonance imaging. Other physical examinations were unremarkable. Blood examinations were normal except for leukocyte levels of 9.3 × 109/L (normal levels 4 × 109/L to 9 × 109/L), glutamic-oxaloacetic transaminase levels of 79 U/L (normal levels 9 U/L to 38 U/L), and glutamic-pyruvic transaminase levels of 105 U/L (normal levels 4 U/L to 36 U/L). He had a family history of hypertension, hyperlipidemia, diabetes mellitus, cerebral stroke, sudden death and heart disease. He was treated by fluid transfusion and anticoagulation therapy. His medication included 100 mg of acetylsalicylic acid daily.
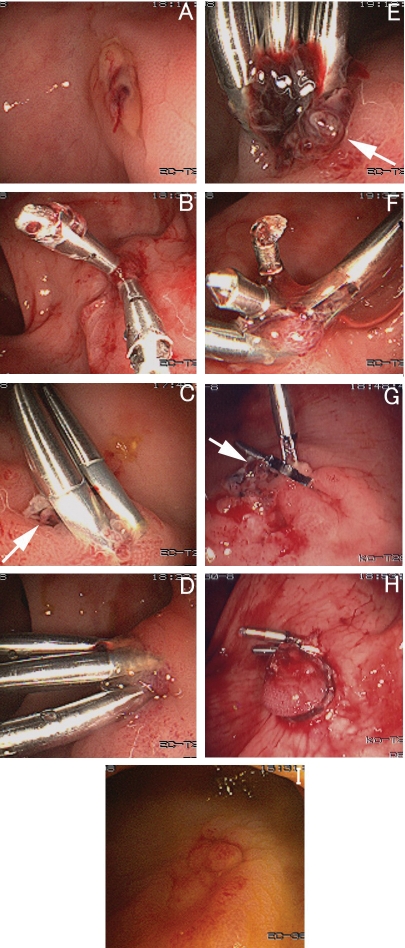
On the 23rd hospitalization day (HD), he showed massive hematochezia without abdominal pain. A digital rectal examination revealed a large amount of fresh blood and clots but no mass or fissure. His hemoglobin level dropped from 153 g/L to 123 g/L over 8 h and he therefore underwent urgent colonoscopy. A protuberant vessel was demonstrated at 5 cm above the anal verge without any significant ulceration at the fundus, consistent with a Dieulafoy’s ulcer of the rectum (Figure 1A). It was endoscopically treated using two hemoclips (Figure 1B).
Figure 1).
Series of endoscopic views of Dieulafoy’s ulcer in the rectum. A (23rd hospitalization day [HD]): A protuberant vessel was surrounded by an almost normal mucosa; B (23rd HD): Endoscopic hemoclipping was performed; C (27th HD), E (31st HD): A protuberant vessel was evident beside the hemoclips (arrow); D (27th HD); F (31st HD): Additional hemoclipping was performed; G (35th HD): A small ulcer was found to have formed beside the remaining hemoclips. A small amount of blood oozed from the small vessel in the ulcer bed (arrow); H (35th HD): Endoscopic band ligation was performed; I (42nd HD): A red ulcer scar was detected in the rectum. There was no further bleeding
On the 27th HD, he again developed hematochezia. His hemoglobin level dropped to 75 g/L. Transfusion of four units of red blood cell (RBC) concentrates raised the hemoglobin level to 98 g/L. The patient underwent a second urgent colonoscopy. Active bleeding was not found throughout the colon. The protuberant vessel was still evident just next to the remaining hemoclips (Figure 1C) and one more hemoclip was applied (Figure 1D). The patient also underwent esophagogas-troduodenoscopy. Mild duodenitis was detected at the bulbus but it was not considered to be the source of massive bleeding.
Bleeding recurred on the 31st HD. His blood pressure fell to 75/50 mmHg. He became hemodynamically unstable and required transfusion with eight units of RBC concentrates. A technetium 99m-labelled RBC scintigraphy was performed to search for another source of the hemorrhage. It revealed an increased activity throughout the colon but it failed to identify the bleeding site. A third urgent colonoscopy was carried out. There was fresh blood and clots in the rectum and a protuberant vessel was visible again beside the hemoclips (Figure 1E). There was no other source of bleeding in the colon and two more hemoclips were applied to that lesion (Figure 1F).
On the 35th HD, he again developed massive hematochezia, amounting to 1100 mL. His hemoglobin level dropped from 113 g/L to 83 g/L. He was transfused with two units of RBC concentrates. He underwent a fourth urgent colonoscopy. Some of the hemoclips dropped out and there was a small ulcer beside the remaining hemoclips. A small vessel was visible in the ulcer bed and a small amount of blood was found to be oozing from it (Figure 1G). There was no blood in the proximal colon and no other lesions were detected in the distal colon with careful irrigation. A standard upper endoscope attached with a single band ligation device (Pneumo-Activated EVL device, Sumitomo Bakelite, Japan) was inserted into the rectum. A single elastic band was then applied on the vessel, leading to a complete cessation of the bleeding (Figure 1H). No complications occurred during the procedure.
A follow-up colonoscopy on the 42nd HD showed a red scar in the rectum (Figure 1I). There was no recurrence of bleeding during the one-year follow-up.
DISCUSSION
The causes of lower GI bleeding may be grouped into several categories: anatomy (diverticulosis), vasculature (angiodysplasia, ischemia and Dieulafoy’s ulcer), inflammation (infection, radiation and idiopathy) and neoplasm. Diverticulosis accounts for approximately 30% to 50% and angiodysplasia accounts for approximately 15% to 30% of massive lower GI bleeding. In the evaluation of patients with severe lower GI bleeding, urgent colonoscopy has been proven to be superior to angiography, scintigraphy and surgery, demonstrating bleeding sites in up to 90% of cases (34–36). In addition, colonoscopy offers a chance for therapeutic intervention. The same therapeutic modalities used in upper endoscopy are available but the risk of complications is higher because of the thin wall of the colon in comparison to that of the stomach (9,34).
Dieulafoy’s ulcer of the rectum is an unusual cause of lower GI hemorrhage. In 1991, Franco et al (10) first reported a patient with Dieulafoy’s ulcer of the rectum; since then, 30 additional cases have been reported, including the present case (Table 1). There may be a higher incidence in middle-aged men but this disease has been reported in all ages. The diagnosis of Dieulafoy’s ulcer may be difficult because poor bowel preparation and stagnant blood contribute to the poor visualization. Improvement of general conditions with blood and/or fluid transfusion, pretreatment of colon with cleaning solution and careful irrigation are essential. The average number of colonoscopies to diagnose the lesions as Dieulafoy’s ulcers was 1.7±0.9 in 28 cases in literature. In two cases (case 5 and case 13 in Table 1), the source of hemorrhage could not be found with colonoscopy. Case 5 was diagnosed and treated surgically. Case 13 was treated with angiographic embolization, and subsequent sigmoidoscopy confirmed the lesion. In recent studies, rectal Dieulafoy’s ulcers were easily found, and the lesion could be determined in the first colonoscopy with careful irrigation. Although a histological diagnosis was not made in our case, the distinctive endoscopic features of the protuberant vessel without significant ulceration allowed us to diagnose it as a Dieulafoy’s ulcer.
TABLE 1.
Characteristics of the reported rectal Dieulafoy’s ulcers
| Reference | Year | Age (years) | Sex | Endoscopic finding | Diagnostic attempts | Treatment | Rebleeding | Retreatment |
|---|---|---|---|---|---|---|---|---|
| Franko et al (10) | 1991 | 20 | M | Pulsatile bleeding | 1 | EC (failure) + SL | – | |
| Abdulian et al (11) | 1993 | 43 | M | Protuberant vessel | 1 | EtI | + (4 days) | EtI + SI |
| Tooson et al (12) | 1995 | 5 | F | Protuberant vessel | 3 | EpI + HP | – | |
| Yeoh et al (13) | 1996 | 66 | M | Protuberant vessel | 1 | EpI | – | |
| Eguchi et al (14) | 1997 | 78 | M | Failed to diagnosis | (1) | SL | – | |
| Kalmann et al (15) | 1997 | 33 | M | Protuberant adherent clot | 1 | EpI + EC | + (7 days) | EC |
| Abdelmalek et al (16) | 1997 | 76 | M | Pulsatile bleeding | 2 | EpI + HP + SL | – | |
| Meister et al (17) | 1998 | 5 | F | Protuberant vessel | 4 | EpI + HP | – | |
| 74 | M | Protuberant vessel | 2 | EpI + HP | – | |||
| 77 | M | Adherent clot | 1 | HP | – | |||
| 67 | M | Pulsatile bleeding | 1 | EpI + HP | – | |||
| 7 | M | Dieulafoy-like lesion | 1 | EpI + HP | – | |||
| Dobson and Nicholson (18) | 1999 | 75 | F | Failed to diagnosis | (1) | AE | – | |
| Amaro et al (19) | 1999 | 73 | F | Pulsatile bleeding | 1 | EpI + HP | + (3 days) | EpI + HP |
| Nozoe et al (20) | 1999 | 65 | M | Protuberant vessel | 1 | CL | – | |
| Yarze et al (21) | 2000 | 77 | F | Protuberant vessel | 2 | EpI | + (4 days) | SL |
| Azimuddin et al (22) | 2000 | 86 | F | Protuberant vessel | 2 | SL | – | |
| 81 | F | Punctate mucosal defect | 4 | SE | – | |||
| Kayali et al (23) | 2000 | 77 | F | Protuberant vessel | 2 | EpI + EtI | – | |
| 73 | F | Protuberant vessel | 2 | EpI + EtI | – | |||
| Rajendra et al (24) | 2000 | 78 | M | Protuberant vessel | 2 | (EpI + EC) (failure) + SL | – | |
| Matsuoka et al (25) | 2000 | 54 | F | Protuberant vessel | 3 | EtI + EC | – | |
| Enns (26) | 2001 | 72 | M | Pulsatile bleeding | 2 | EpI + EC | – | |
| Guy et al (27) | 2001 | 18 | F | Pulsatile bleeding | 2 | AE (failure) + ST | – | |
| Jani (28) | 2001 | 60 | M | Adherent clot | 1 | EpI | – | |
| Nomura et al (29) | 2002 | 82 | M | Protuberant vessel | 1 | CL | – | |
| Mizukami et al (30) | 2002 | 85 | F | Protuberant vessel | 1 | EpI + BL | – | |
| Abe et al (31) | 2003 | 55 | M | Protuberant vessel | 1 | CL | – | |
| Fujimaru et al (32) | 2003 | 83 | F | Pulsatile bleeding | 1 | EpI + BL | – | |
| Lee et al (33) | 2004 | 73 | M | Pulsatile bleeding | 1 | AE | + (5 h) | EpI + BL |
| Yoshikumi (present paper) | 2005 | 44 | M | Protuberant vessel | 1 | CL | +++ (4, 4, 4 days) | BL |
+Yes; – No; AE Angiographic embolization; BL Band ligation; CL Hemoclipping; EC Electrocoagulation; EpI Adrenaline injection; EtI Ethanol injection; F Female; HP Heater probe thermocoagulation; M Male; SE Surgical excision; SI Sclerosant Injection; SL Surgical ligation; ST Surgical treatment
There is no consensus on the treatment of bleeding rectal Dieulafoy’s ulcer and there are no randomized controlled studies comparing the different endoscopic therapies. Of the 30 reported cases, 21 patients were treated with endoscopic modalities alone, angioembolization was used in two cases and surgical treatment with or without other treatment was used in seven. Rebleeding occurred in five cases (17%), in which the initial treatment was not uniform. One patient was treated with ethanol injection (n=1), one with adrenaline injection (n=3), one with adrenaline injection and electrocoagulation (n=2), one with adrenaline injection and heater probe coagulation (n=6), and one with angiographic embolization (n=2). Recurrent bleeding was not reported after surgical treatment (n=7; five suture ligations, one excision and one unknown). Rebleeding tended to occur several days after the treatment except for case 30. Lee et al (33) reported a case of rebleeding 5 h after angiographic embolization but it was not clear whether complete hemostasis had been obtained by embolization.
In the present case, we first used endoscopic hemoclipping. Endoscopic treatment by hemoclip is recommended for rectal Dieulafoy’s ulcer. It usually causes little injury to the colorectal wall, and complete hemostasis was obtained in all reported cases (20,30,32). However, rebleeding from the lesion occurred three times in our patient. We paid careful attention to the optimal placement of the hemoclips. Rebleeding may have been due to the fragility of the wall, sclerotic change of the vessel or the application of anticoagulation therapy. In the first urgent colonoscopy, we tried endoscopic clipping with six hemoclips, in which only two hemoclips firmly grasped the lesion. This middle-aged man had several risk factors and a family history of atherosclerosis. Acetylsalicylic acid was continued up to the 27th HD, because iodine-123-labelled N-isopropyl-p-iodoamphetamine brain single photon emission computed tomography revealed moderate to severe hypoperfusion in the larger area of the left internal carotid artery territory than in the infarcted area.
Finally, endoscopic band ligation was successfully performed. Band ligation has been proven to be safe and effective in the treatment of bleeding esophageal varices (37–39) with fewer complications compared with sclerotherapy. Recently, this modality has been used effectively in the endoscopic treatment of bleeding rectal varices (40) and nonvariceal upper GI bleeding (41). Endoscopic band ligation with adrenaline injection was reported to be successful for the recurrent bleeding after angioembolization (33) as well as for naïve cases of rectal Dieulafoy’s ulcer (30,32). In our patient, endoscopic band ligation was applied for recurrent bleeding from Dieulafoy’s ulcer without an adrenaline injection. The lesion was located 5 cm from the anal verge, on the anal side of the peritoneal reflection, so we decided that a perforation due to the endoscopic procedures was unlikely to occur. Recurrent bleeding has not been reported after surgical treatment and therefore we took surgery into consideration in cases of rebleeding rectal Dieulafoy’s ulcer. Endoscopic band ligation is simple, readily available, relatively inexpensive and may be highly effective in patients with coagulopathies or hemorrhages (42). We used a standard upper endoscope to perform band ligation in the present case. However, the banding apparatus fitted on colonoscopes with smaller diameters such as the Olympus PCF series (Japan). Small bleeding lesions were occasionally missed while we attached the apparatus. In cases using those scopes, band ligation can be performed without changing the scopes. The ligation apparatus can be fixed on the tip of the endoscope more quickly and easily than conventional hemoclips. This modality may have a potential to be used as a first-line therapy. Band ligation completely controlled the bleeding with no evidence of recurrence in all four patients, including our patient (30,32,33). The mechanism of hemostasis by mechanical strangulation of the vessel makes this technique very suitable in patients with coagulopathies or using anticoagulant drugs.
In conclusion, endoscopic band ligation was found to be an effective treatment for bleeding rectal Dieulafoy’s ulcer even after other therapeutic modalities had failed.
REFERENCES
- 1.Lee YT, Walmsley RS, Leong RW, Sung JJ. Dieulafoy’s lesion. Gastrointest Endosc. 2003;58:236–43. doi: 10.1067/mge.2003.328. [DOI] [PubMed] [Google Scholar]
- 2.Veldhuyzen van Zanten SJ, Bartelsman JF, Schipper ME, Tytgat GN. Recurrent massive haematemesis from Dieulafoy vascular malformations: Review of 101 cases. Gut. 1986;27:213–22. doi: 10.1136/gut.27.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pollack R, Lipsky H, Goldberg RI. Duodenal Dieulafoy’s lesion. Gastrointest Endosc. 1993;39:820–22. doi: 10.1016/s0016-5107(93)70276-x. [DOI] [PubMed] [Google Scholar]
- 4.Anireddy D, Timberlake G, Seibert D. Dieulafoy’s lesion of the esophagus. Gastrointest Endosc. 1993;39:604. doi: 10.1016/s0016-5107(93)70198-4. [DOI] [PubMed] [Google Scholar]
- 5.Choudari CP, Palmer KR. Dieulafoy’s lesion of the duodenum; successful endoscopic therapy. Endoscopy. 1993;25:371. doi: 10.1055/s-2007-1010334. [DOI] [PubMed] [Google Scholar]
- 6.Matuchansky C, Babin P, Abadie JC, Payen J, Gasquet C, Barbier J. Jejunal bleeding from a solitary large submucosal artery: Report of two cases. Gastroenterology. 1978;75:110–3. [PubMed] [Google Scholar]
- 7.Barbier P, Luder P, Triller J, Ruchti C, Hassler H, Stafford A. Colonic hemorrhage from a solitary minute ulcer: Report of three cases. Gastroenterology. 1985;88:1065–8. doi: 10.1016/s0016-5085(85)80030-5. [DOI] [PubMed] [Google Scholar]
- 8.Richards WO, Grove-Mahoney D, Williams LF. Hemorrhage from a Dieulafoy-type ulcer in the colon: A new cause of lower gastrointestinal bleeding. Am Surg. 1988;54:121–4. [PubMed] [Google Scholar]
- 9.Dy NM, Gostout CJ, Balm RK. Bleeding from the endoscopically-identified Dieulafoy lesion of the proximal small intestine and colon. Am J Gastroenterol. 1995;90:108–11. [PubMed] [Google Scholar]
- 10.Franko E, Chardavoyne R, Wise L. Massive rectal bleeding from a Dieulafoy’s type ulcer of the rectum: A review of this unusual disease. Am J Gastroenterol. 1991;86:1545–7. [PubMed] [Google Scholar]
- 11.Abdulian JD, Santro MJ, Chen YK, Collen MJ. Dieulafoy-like lesion of the rectum presenting with exsanguinating hemorrhage: Successful endoscopic sclerotherapy. Am J Gastroenterol. 1993;88:1939–41. [PubMed] [Google Scholar]
- 12.Tooson JD, Marsano LS, Gates LK., Jr Pediatric rectal Dieulafoy’s lesion. Am J Gastroenterol. 1995;90:2232–3. [PubMed] [Google Scholar]
- 13.Yeoh KJ, Kang JY. Dieulafoy’s lesion in rectum. Gastrointest Endosc. 1996;43:614–16. doi: 10.1016/s0016-5107(96)70202-x. [DOI] [PubMed] [Google Scholar]
- 14.Eguchi S, Maeda J, Taguchi H, Kanematusu T. Massive gastrointestinal bleeding from a Dieulafoy-like lesion of the rectum. Clin Gastroenterol. 1997;24:262–3. doi: 10.1097/00004836-199706000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Kalman DR, Banner BF, Barnard GF. Rectal Dieulafoy’s or angiodysplasia? Gastrointest Endosc. 1997;46:91–2. doi: 10.1016/s0016-5107(97)70224-4. [DOI] [PubMed] [Google Scholar]
- 16.Abdelmalek MF, Pockaj BA, Leighton JA. Rectal bleeding from a mucous fistula secondary to a Dieulafoy’s lesion. J Clin Gastroenterol. 1997;24:259–61. doi: 10.1097/00004836-199706000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Meister TE, Varilek GW, Marsano LS. Endoscopic management of rectal Dieulafoy-like lesions: A case series and review of literature. Gastrointest Endosc. 1998;48:302–5. doi: 10.1016/s0016-5107(98)70197-x. [DOI] [PubMed] [Google Scholar]
- 18.Dobson CC, Nicholson AA. Treatment of rectal hemorrhage by coil embolization. Cardiovasc Intervent Radiol. 1999;22:143–6. doi: 10.1007/BF03035356. [DOI] [PubMed] [Google Scholar]
- 19.Amaro R, Petruff CA, Rogers AI. Rectal Dieulafoy’s lesion: Report of a case and review of the literature. Dis Colon Rectum. 1999;42:1339–41. doi: 10.1007/BF02234226. [DOI] [PubMed] [Google Scholar]
- 20.Nozoe T, Kitamura M, Matsumata T, Sugimachi K. Dieulafoy-like lesions of colon and rectum in patients with chronic renal failure on long-term hemodialysis. Hepatogastroenterology. 1999;46:3121–3. [PubMed] [Google Scholar]
- 21.Yarze JC, Schupp SL, Friz HP, Lusignan DN. Hemorrhage related to an anal Dieulafoy-like lesion. Am J Gastroenterol. 2000;95:1593–4. doi: 10.1111/j.1572-0241.2000.02107.x. [DOI] [PubMed] [Google Scholar]
- 22.Azimuddin K, Stasik JJ, Rosen L, Riether RD, Khubchandani IT. Dieulafoy’s lesion of the anal canal: A new clinical entity. Report of two cases. Dis Colon Rectum. 2000;43:423–6. doi: 10.1007/BF02258313. [DOI] [PubMed] [Google Scholar]
- 23.Kayali Z, Sangchantr W, Matsumoto B. Lower gastrointestinal bleeding secondary to Dieulafoy-like lesion of the rectum. J Clin Gastroenterol. 2000;30:328–30. doi: 10.1097/00004836-200004000-00028. [DOI] [PubMed] [Google Scholar]
- 24.Rajendra T, Chung YF, Ong HS. Rectal Dieulafoy’s lesion: Cause of massive lower gastrointestinal tract hemorrhage. Aust NZJ Surg. 2000;70:746–7. doi: 10.1046/j.1440-1622.2000.01946.x. [DOI] [PubMed] [Google Scholar]
- 25.Matsuoka J, Taniai K, Kojima K, et al. A case of rectal Dieulafoy’s ulcer and successful endoscopic sclerotherapy. Acta Med Okayama. 2000;54:281–3. doi: 10.18926/AMO/32279. [DOI] [PubMed] [Google Scholar]
- 26.Enns R. Dieulafoy’s lesion of the rectum: A rare cause of lower gastrointestinal bleeding. Can J Gastoenterol. 2001;15:541–5. doi: 10.1155/2001/851354. [DOI] [PubMed] [Google Scholar]
- 27.Guy RJ, Ang ES, Tan KC, Tsang CB. Massive bleeding from a Dieulafoy-like lesion of rectum in a burns patient. Burns. 2001;27:767–9. doi: 10.1016/s0305-4179(01)00031-6. [DOI] [PubMed] [Google Scholar]
- 28.Jani PG. Dieulafoy’s lesion: Case report. East Afr Med J. 2001;78:109–10. doi: 10.4314/eamj.v78i2.9100. [DOI] [PubMed] [Google Scholar]
- 29.Nomura S, Kawahara K, Yamasaki K, Nakanishi Y, Kaminishi M. Massive rectal bleeding from a Dieulafoy lesion in the rectum: Successful endoscopic clipping. Endoscopy. 2002;34:237. doi: 10.1055/s-2002-20297. [DOI] [PubMed] [Google Scholar]
- 30.Mizukami Y, Akahoshi K, Kondoh N, Harada N, Nawata H. Endoscopic band ligation for rectal Dieulafoy’s lesion: Serial endoscopic images. Endoscopy. 2002;34:1032. doi: 10.1055/s-2002-35835. [DOI] [PubMed] [Google Scholar]
- 31.Abe T, Okada N, Akamatsu H, et al. Successful endoscopic hemostasis of rectal Dieulafoy’s ulcer by clipping: Aging may be a factor. Dig Endosc. 2003;15:64–8. [Google Scholar]
- 32.Fujimaru T, Akahoshi K, Matsuzaka H, Sumita Y, Kubokawa M. Bleeding rectal Dieulafoy’s lesion. Gastrointest Endosc. 2003;57:922. doi: 10.1016/s0016-5107(03)70035-2. [DOI] [PubMed] [Google Scholar]
- 33.Lee CS, Widjaja D, Siegel M, Bodenheimer HC., Jr Endoscopic band ligation of a rectal Dieulafoy’s lesion. J Clin Gastroenterol. 2004;38:828–30. doi: 10.1097/01.mcg.0000139056.05297.9f. [DOI] [PubMed] [Google Scholar]
- 34.Jensen DM, Machicado GA. Advanced therapeutic endoscopy. New York: Raven; 1994. pp. 201–8. [Google Scholar]
- 35.Jensen DM, Machicado GA. Diagnosis and treatment of severe hematochezia: The role of urgent colonoscopy after purge. Gastroenterology. 1988;95:1569–74. doi: 10.1016/s0016-5085(88)80079-9. [DOI] [PubMed] [Google Scholar]
- 36.Richter JM, Christensen MR, Kaplan LM, Nishioka NS. Effectiveness of current technology in the diagnosis and management of lower gastrointestinal hemorrhage. Gastrointest Endosc. 1995;41:93–8. doi: 10.1016/s0016-5107(05)80588-7. [DOI] [PubMed] [Google Scholar]
- 37.Laine L, El-Newihi HM, Migikovsky B, Sloane R, Garcia F. Endoscopic ligation compared with sclerotherapy for the treatment of bleeding esophageal varices. Ann Intern Med. 1993;119:1–7. doi: 10.7326/0003-4819-119-1-199307010-00001. [DOI] [PubMed] [Google Scholar]
- 38.Stiegmann GV, Goff JS, Michaletz-Onody PA, et al. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N Engl J Med. 1992;326:1527–32. doi: 10.1056/NEJM199206043262304. [DOI] [PubMed] [Google Scholar]
- 39.Gimson AE, Ramage JK, Panos MZ, et al. Randomized trial of variceal banding ligation versus injection sclerotherapy for bleeding esophageal varices. Lancet. 1993;342:391–4. doi: 10.1016/0140-6736(93)92812-8. [DOI] [PubMed] [Google Scholar]
- 40.Levine J, Tahiri A, Banerjee S. Endoscopic ligation of bleeding rectal varices. Gastrointest Endosc. 1993;39:188–9. doi: 10.1016/s0016-5107(93)70067-x. [DOI] [PubMed] [Google Scholar]
- 41.Tseng C, Burke S, Connors P, Green R, Carr-Locke DL. Endoscopic band ligation for treatment of non-variceal upper gastrointestinal bleeding. Endoscopy. 1991;23:297–8. doi: 10.1055/s-2007-1010693. [DOI] [PubMed] [Google Scholar]
- 42.Nikolaidis N, Zezos P, Giouleme O, et al. Endoscopic band ligation of Dieulafoy-like lesions in the upper gastrointestinal tract. Endoscopy. 2001;33:754–60. doi: 10.1055/s-2001-16522. [DOI] [PubMed] [Google Scholar]