Abstract
OBJECTIVE:
Nutrition education is a required part of gastrointestinal training programs. The involvement of gastroenterologists in clinical nutrition once their training has been completed is unknown. The aim of the present study was to determine the practice pattern of gastroenterologists in clinical nutrition and their perceived adequacy of nutrition training during their gastroenterology (GI) fellowship.
METHODS:
The Canadian Association of Gastroenterology mailed a survey to all of its 463 Canadian clinician members and 88 trainee members. Components of the survey included knowledge of nutritional assessment and total parenteral nutrition, involvement in a nutrition support service, physician involvement in nutritional assessment and nutrition support teams, obesity management, insertion of gastrostomy (G) tubes and management of tube-related complications, and adequacy of training in clinical nutrition.
RESULTS:
Sixty per cent (n=279) of the Canadian Association of Gastroenterology clinicians and 38% (n=33) of the fellows responded. Of the clinicians, 80% were practicing adult gastroenterologists with the following demographics: those practicing full time in academic centres (42%), community practice (45%), completed training in the last 10 years (32%) and those that completed training in the United States (14%). Although only 6% had a primary focus of nutrition in their GI practices, 65% were involved in nutrition support (including total parenteral nutrition), 74% placed G tubes and 68% managed at least one of the major complications of G tube insertion. Respondents felt a gastroenterologist should be the physician’s consultant on nutrition support services (89%). Areas of potential inadequate training included nutritional assessment, indications for nutrition support, management of obesity and management of G tube-related complications. The majority of clinicians (67%) and trainees (73%) felt that nutrition training in their GI fellowship was underemphasized.
CONCLUSIONS:
The majority of Canadian gastroenterologists are involved in nutrition support. However, this survey demonstrated that nutritional training is underemphasized in most training programs. It is important for GI fellowship programs to develop standardized nutrition training that prepares trainees for their practice.
Keywords: Gastroenterology, Nutrition training
Abstract
OBJECTIF :
La formation en nutrition est un élément obligatoire des programmes de formation en gastroentérologie. On ne connaît pas l’engagement des gastroentérologues en nutrition clinique une fois leur formation terminée. La présente étude visait à déterminer le schéma de pratique des gastroentérologues en nutrition clinique ainsi que la pertinence perçue de leur formation en nutrition pendant leur postdoctorat en gastroentérologie (GI).
MÉTHODOLOGIE :
L’Association canadienne des gastroentérologues a posté un sondage à ses 463 membres cliniciens et à 88 membres stagiaires. Les éléments du sondage incluaient les connaissances de l’évaluation nutritionnelle et de l’alimentation parentérale totale, la participation à un service de soutien nutritionnel, la participation aux équipes d’évaluation nutritionnelle et de soutien nutritionnel, la prise en charge de l’obésité, l’insertion d’une sonde de gastrostomie (G) et la prise en charge des complications reliées aux sondes, ainsi que la pertinence de la formation en nutrition clinique.
RÉSULTATS :
Soixante pour cent (n=279) des cliniciens de l’Association canadienne de gastroentérologie, et 38 % (n=33) des stagiaires y ont répondu. Parmi les cliniciens, 80 % exerçaient la gastroentérologie pour adultes, selon les caractéristiques démographiques suivantes : ceux qui exerçaient à temps plein dans des centres universitaires (42 %), en pratique générale (45 %), avaient terminé leur formation depuis les dix dernières années (32 %) ou avaient effectué leur formation aux États-Unis (14 %). Seulement 6 % axaient leur pratique de GI sur la nutrition, mais 65 % participaient au soutien nutritionnel (y compris l’alimentation parentérale totale), 74 % installaient des sondes G et 68 % prenaient en charge au moins l’une des complications majeures reliées à l’installation de sondes G. Les répondants étaient d’avis que les gastroentérologues devraient être les médecins consultants en matière de services de soutien nutritionnel (89 %). Les secteurs possibles de formation insuffisante étaient l’évaluation nutritionnelle, les indications de soutien nutritionnel, la prise en charge de l’obésité et la prise en charge des complications reliées aux sondes G. La majorité des cliniciens (67 %) et des stagiaires (73 %) étaient d’avis que la formation en nutrition n’était pas assez mise en évidence pendant le postdoctorat en GE.
CONCLUSIONS :
La majorité des gastroentérologues canadiens participent au soutien nutritionnel. Cependant, ce sondage démontre que la formation nutritionnelle n’est pas assez mise en relief dans la plupart des programmes de formation. Il est important d’élaborer une formation standardisée en nutrition dans les programmes postdoctoraux en GI afin de préparer les stagiaires à leur pratique.
Malnutrition is common in hospitalized patients and is often not recognized by physicians (1–5). Gastroenterologists are involved in clinical nutrition in several different ways:
Insertion of gastrostomy (G) tubes in patients to provide access for enteral nutrition;
Management of patients with gastrointestinal disorders (eg, inflammatory bowel disease, celiac disease and structural abnormalities of the gastrointestinal tract) associated with malnutrition; and
Involvement in the nutritional support of patients requiring long-term total parenteral nutrition (TPN) (eg, short-bowel syndrome).
Because of these factors, many gastroenterologists are involved in nutrition support teams and in the administration of TPN. Also, the basic nutritional physiology involves digestion and absorption of nutrients from the gastrointestinal tract, which is an integral part of the gastroenterology (GI) curriculum.
For these reasons, the GI core curriculum developed by a consortium of American GI associations, including the American Gastroenterological Association, the American Association for the Study of Liver Diseases, the American College of Gastroenterology and the American Society for Gastrointestinal Endoscopy, has designated nutrition training of GI fellows as a mandatory component (6). In Canada, the Royal College of Physicians and Surgeons of Canada requires training in nutrition in GI fellowships.
Despite these requirements, the nature and extent of involvement of practicing gastroenterologists in clinical nutrition is not known. It is also not clear whether the training in nutrition during the GI fellowships is perceived to be adequate by the practicing gastroenterologists and the current GI trainees in Canada. Therefore, we conducted a survey of practicing Canadian gastroenterologists and current GI fellowship trainees to determine the relevance, practice patterns and adequacy of training of clinical nutrition to gastroenterologists in Canada.
METHODS
An 18-question survey with self-addressed, stamped, return envelopes was mailed out to all 463 members of the Canadian Association of Gastroenterology (CAG) who were listed as practicing in Canada, and 88 trainee members of the CAG. The survey was accompanied with a cover letter explaining the objectives of the study. The responses remained anonymous to the investigators. In addition to demographics, questions in the survey focused on the knowledge of nutritional assessment and timing of nutrition support, involvement in a nutrition support service, obesity management, insertion of G tubes and management of tube-related complications, and adequacy of training in clinical nutrition. The mailing was sent out in November 2003 and the responses included in the present study were received until April 2004. The study protocol was approved by the Research Ethics Board of the University of Manitoba (Winnipeg, Manitoba).
Statistical analysis
Descriptive statistics were used to calculate the response frequency. The sum of the responses to some of the questions was more than 100% because the respondents marked more than one of the choices listed. χ2 testing was used to compare the responses. The significance level was determined at P<0.05.
RESULTS
Response rates
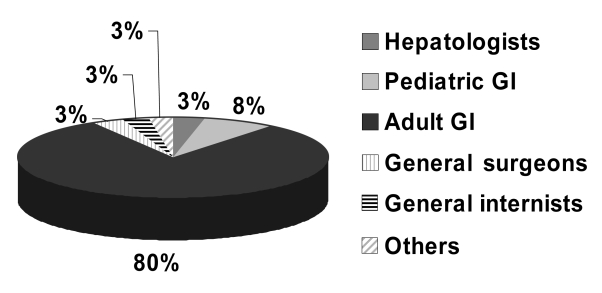
Sixty per cent (n=279) of clinically active members of the CAG returned the survey. Thirty-eight per cent (n=33) of the trainee members responded. Eighty per cent (n=225) of the responding clinical members were adult gastroenterologists (Figure 1). Their responses formed the basis for the rest of the report. Those who identified themselves as surgeons, internists with special interest in GI, hepatologists, pediatric gastroenterologists or members of other specialties (such as pathology or radiology) were not included in the final analysis.
Figure 1).
Specialties of those practicing members of the Canadian Association of Gastroenterology who returned the survey. GI Gastroenterologists
Demographics (Table 1)
TABLE 1.
Demographics of the Canadian Association of Gastroenterology adult clinicians who completed the survey*
| Practice | % | Training | % |
|---|---|---|---|
| Full time in academic centre | 42 | Training <10 years ago | 32 |
| Part time in academic centre | 12.5 | Training >20 years ago | 33 |
| Community practice | 45 | Trained in the United States | 14 |
| Geographic distribution | % | Special interest in GI | % |
|---|---|---|---|
| Western Canada | 25 | General GI | 73 |
| Ontario | 42 | Endoscopy | 27 |
| Quebec | 21 | Hepatology | 15 |
| Maritimes | 9 | Research | 8 |
| Motility | 7 | ||
| Nutrition | 6 |
Responses may add up to more than 100% because individuals were allowed to mark off more than one answer to some of the questions. GI Gastroenterology
The number of respondents practicing full time in academic medical centres was similar to that in community practices. The respondents were well-distributed according to time, from completion of the fellowship, with approximately one-third finishing training in the last 10 years, one-third finishing 10 to 20 years ago and one-third more than 20 years ago. The respondents were from all across Canada. The most common special interests included general GI, endoscopy and hepatology. A special interest in nutrition was reported by 6% (n=13) of the respondents. Of the trainees, most expressed special interest in general GI (67%, n=22) followed by endoscopy (34%, n=11). Only one of the responding current GI trainees expressed special interest in nutrition.
Involvement in clinical nutrition (Tables 2 and 3)
TABLE 2.
Gastroenterologist involvement in clinical nutrition
| Clinical nutrition activity | % |
|---|---|
| Insertion of percutaneous endoscopic gastrostomy tubes | 74 |
| Nutrition support | 65 |
| Able to write total parenteral nutrition orders | 62 |
| Manage obesity | 10 |
TABLE 3.
Management of gastrostomy tube complications after patient discharge
| Complication | Managing this complication (%) |
|---|---|
| Stomal infection | 60 |
| Stomal pain | 46 |
| Stomal granulation tissue | 37 |
| Blocked gastrostomy tube | 66 |
| Infected gastrostomy tube | 47 |
Two-thirds of the respondents (n=146) reported that they were involved in nutrition support, including TPN. There was no significant difference whether they finished their training in the last 10 years, 10 to 20 years ago or more than 20 years ago. The majority (n=138) reported that they could write TPN orders without a dietitian or a nurse clinician. Seventy-four per cent (n=167) were inserting percutaneous G tubes and 68% (n=154) were managing at least one of the major G tube-related complications listed in the questionnaire. Approximately one-third (34%, n=77) were managing all of the major complications of G tube insertion.
Physician involvement in nutrition support teams
Fifty-three per cent (n=120) of the gastroenterologists across the country reported that there was a physician on the nutrition support team at the hospital at which they practiced. Almost all (89%, n=201) of the respondents felt that a gastroenterologist should be a consultant on the nutrition support team.
Obesity management
Ten per cent (n=23) of the respondents reported that they managed obesity in their practices. Six of the 10 respondents who listed themselves as hepatologists responded that they were involved in the management of obesity.
Nutritional assessment (Tables 4 and 5)
TABLE 4.
Respondents’ opinion as to who should primarily be responsible for nutrition assessment
| Primarily responsible for nutrition assessment | % |
|---|---|
| Dietitian | 62 |
| Admitting physician | 37 |
| House staff | 6 |
| Nurse | 2 |
TABLE 5.
Responses by the practicing gastroenterologists as to the best clinical indicator of nutritional status
| Clinical indicators of nutritional status | % |
|---|---|
| Subjective global assessment | 60 |
| Nutrition risk index | 11 |
| Albumin or prealbumin | 20 |
| History of weight loss | 7 |
| Creatinine-height index | 4 |
| Physical findings of vitamin and trace element deficiency | 1 |
| Others | 2 |
The majority of the respondents thought that a dietitian should be primarily responsible for nutritional assessment of hospitalized patients. Subjective global assessment was thought to be the best clinical indicator for nutritional assessment by most of the respondents. A significant minority thought that albumin or prealbumin were the best markers for the assessment nutritional status. Responses of the trainees were similar, with 70% considering subjective global assessment as the best marker for assessing a persons nutritional status and 12% albumin or prealbumin.
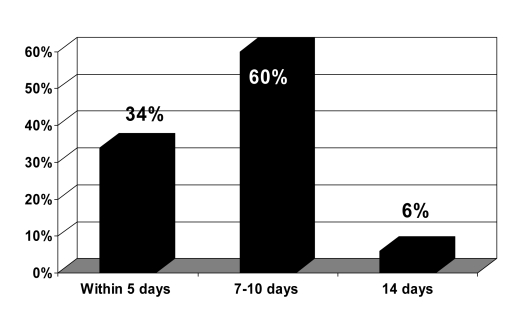
Initiation of nutrition support (Figure 2)
Figure 2).
Response to the question ‘After how many days of minimal oral intake by a well-nourished individual, would you initiate nutrition support?’
Approximately 60% of the respondents recommended initiation of nutrition support within seven to 10 days of minimal nutrition intake in a well-nourished individual, while one-third recommended nutrition support within five days.
Nutrition training (Table 6)
TABLE 6.
Perception of adequacy of training
| Years since gastroenterology training completed | Nutrition training underemphasized (%) |
|---|---|
| Less than 10 | 66 |
| 10 to 20 | 68 |
| Greater than 20 | 73 |
| Current trainees | 73 |
The majority of the respondents thought that training in nutrition was underemphasized in their fellowship programs. There was no significant difference in the responses of those who had finished training recently when compared with those who had finished their training some time ago. Response of the current GI trainees was not significantly different from the practicing physicians and the majority thought that the training in nutrition was underemphasized in their training program. Only one of the respondents, a practicing gastroenterologist, felt that the training in nutrition had been overemphasized in his/her training.
DISCUSSION
Our survey of the Canadian clinical gastroenterologists suggested that 89% of Canadian gastroenterologists believe that a gastroenterologist should be involved in clinical nutrition as a consultant on the nutrition support team. In spite of this, it was thought by most that the training in nutrition continues to be underemphasized during the fellowship programs.
Inadequate training in nutrition during GI fellowship programs may be due to a lack of gastroenterologists who are physician nutrition specialists. Gastroenterologists with expertise in nutrition are most important in providing leadership in the education of GI fellows. Currently, there is little opportunity for individuals with an interest in clinical nutrition to achieve additional training. As a result, the paucity of gastroenterologists, who are also clinical nutrition specialists, is likely to continue. In the United States, the number of clinical nutrition training programs for physicians to develop into physician nutrition specialists is declining (7). There is a need to develop clinical fellowships in nutrition for Canadian GI fellows.
Our survey demonstrated that there are still misunderstandings about the interpretation of visceral proteins and nutritional status. A significant number of gastroenterologists and GI trainees believe that albumin or prealbumin are the best markers for nutritional assessment. In hospitalized patients, these proteins are usually a reflection of underlying physiological injury as opposed to malnutrition (8). Albumin levels are predictors of morbidity and mortality, and therefore are important in overall patient assessment (1,9). In addition, they provide useful information as to how catabolic a patient may be. However, these levels do not independently predict whether an individual is malnourished and this needs to be emphasized in the training programs.
Most Canadian gastroenterologists are inserting percutaneous G tubes. However, few are managing all of the G tube insertion-related complications. In a recent survey (10) of home nutrition patients, we have shown that G tube-related complications are quite common when patients are followed long-term. As more of these enteral access devices are inserted, the number of individuals with tube-related complications will increase. It is important that new trainees develop the expertise to deal with these complications.
Approximately one-third of the surveyed Canadian gastroenterologists recommended starting nutrition support within five days of inadequate oral intake in a well-nourished patient. While there is no universally agreed upon optimal time for initiating nutrition support, clinical guidelines suggest starting nutrition support after seven to 10 days in previously well-nourished individuals (11). TPN given routinely to well-nourished or mildly malnourished patients may be associated with a worse outcome (12). Inappropriate use of TPN could lead to increased costs of care and worse outcomes, including longer hospital stays and increased risk of infectious complications (13,14). There is a need to include this type of training in fellowship programs.
The surgical management of obesity shows dramatic increases in the United States. In Canada, there are few dedicated obesity programs. Gastroenterologists have a potentially important role in the management of obesity including presurgical selection, complications during postsurgery requiring endoscopic intervention, and malnutrition and vitamin deficiencies postsurgery. Nonalcoholic fatty liver disease is a common cause of abnormal liver enzymes and in many cases is related to underlying obesity. This is an entity that is frequently seen by gastroenterologists and at present the only known treatment is weight loss. For all of these reasons, obesity management has become an important topic for gastroenterologists and thus, training in some aspects of obesity should also be included in a GI fellowship program.
Self-reported nutrition proficiency has been previously positively correlated with the perceived quality of nutritional training (15). We suggest that training in nutrition in Canadian GI programs needs to be emphasized and standardized. This would best be accomplished by gastroenterologists who are physician nutrition specialists. For the practicing physicians, nutrition content should be included in CAG programs. The Canadian Society of Clinical Nutrition sponsors clinical nutrition symposia and many of these have been relevant to gastroenterologists. There is evidence that these courses can have an effect on clinical practice. In Latin America, a two-day course in clinical nutrition developed for physicians has been completed by over 8000 physicians in 16 Latin American countries (16). A recent survey (17) performed six months after the participants had completed the course showed that even such a short course was effective in changing the nutritional management practices of physicians. Similar courses and symposia have also been recently organized by the American Gastroenterological Association in the United States.
At present, training in clinical nutrition is perceived to be inadequate in most Canadian GI fellowship programs. The majority of Canadian gastroenterologists are currently involved in clinical nutrition in their practice and feel this is an important role. Training of clinical nutrition in GI training programs needs to be relevant and standardized to better prepare future gastroenterologists for clinical and academic practice.
REFERENCES
- 1.Waitzberg DL, Correia MI. Nutritional assessment in the hospitalized patient. Curr Opin Clin Nutr Metab Care. 2003;6:531–8. doi: 10.1097/00075197-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Bistrian BR, Blackburn GL, Vitale J, Cochran D, Naylor J. Prevalence of malnutrition in general medical patients. JAMA. 1976;235:1567–70. [PubMed] [Google Scholar]
- 3.Correia MI, Campos AC. Prevalence of hospital malnutrition in Latin America: The multicenter ELAN study. Nutrition. 2003;19:823–5. doi: 10.1016/s0899-9007(03)00168-0. [DOI] [PubMed] [Google Scholar]
- 4.Wyszynski DF, Perman M, Crivelli A. Prevalence of hospital malnutrition in Argentina: Preliminary results of a population-based study. Nutrition. 2003;19:115–9. doi: 10.1016/s0899-9007(02)00925-5. [DOI] [PubMed] [Google Scholar]
- 5.McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ. 1994;308:945–8. doi: 10.1136/bmj.308.6934.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Training the gastroenterologist of the future: The Gastroenterology Core Curriculum. Gastroenterology. 1996;110:1266–300. doi: 10.1053/gast.1996.1101266. [DOI] [PubMed] [Google Scholar]
- 7.Heimburger DC, Stallings VA, Routzahn L. Survey of clinical nutrition training programs for physicians. Am J Clin Nutr. 1998;68:1174–9. doi: 10.1093/ajcn/68.6.1174. [DOI] [PubMed] [Google Scholar]
- 8.Klein S, Jeejeebhoy KN. The malnourished patient: Nutritional assessment and management. In: Feldman M, Friedman LS, Sleisenger MH, editors. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease. 7th ed. Philadelphia: WB Saunders Co; 2002. pp. 265–85. [Google Scholar]
- 9.Covinsky KE, Covinsky MH, Palmer RM, Sehgal AR. Serum albumin concentration and clinical assessments of nutritional status in hospitalized older people: Different sides of different coins? J Am Geriatr Soc. 2002;50:631–7. doi: 10.1046/j.1532-5415.2002.50156.x. [DOI] [PubMed] [Google Scholar]
- 10.Crosby J, Duerksen D. A retrospective survey of tube-related complications in patients receiving long-term home enteral nutrition. Dig Dis Sci. 2005;50:1712–7. doi: 10.1007/s10620-005-2923-z. [DOI] [PubMed] [Google Scholar]
- 11.ASPEN Board of Directors Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. J Parenter Enteral Nutr. 2002;26(Suppl 1):1–138A. [Google Scholar]
- 12.Perioperative total parenteral nutrition in surgical patients. The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group. N Engl J Med. 1991;325:525–32. doi: 10.1056/NEJM199108223250801. [DOI] [PubMed] [Google Scholar]
- 13.Braunschweig C, Gomez S, Sheean PM. Impact of declines in nutritional status on outcomes in adult patients hospitalized for more than 7 days. J Am Diet Assoc. 2000;100:1316–22. doi: 10.1016/S0002-8223(00)00373-4. [DOI] [PubMed] [Google Scholar]
- 14.Robinson G, Goldstein M, Levine GM. Impact of nutritional status on DRG length of stay. J Parenter Enteral Nutr. 1987;11:49–51. doi: 10.1177/014860718701100149. [DOI] [PubMed] [Google Scholar]
- 15.Mihalynuk TV, Scott CS, Coombs JB. Self-reported nutrition proficiency is positively correlated with the perceived quality of nutrition training of family physicians in Washington State. Am J Clin Nutr. 2003;77:1330–6. doi: 10.1093/ajcn/77.5.1330. [DOI] [PubMed] [Google Scholar]
- 16.Waitzberg DL, Campos AC. Nutrition support in Brazil: Past, present, and future perspectives. J Parenter Enteral Nutr. 2004;28:184–91. doi: 10.1177/0148607104028003184. [DOI] [PubMed] [Google Scholar]
- 17.Waitzberg DL, Correia MI, Echenique M, et al. Total nutritional therapy: A nutrition education program for physicians. Nutr Hosp. 2004;19:28–33. [PubMed] [Google Scholar]