Abstract
Objective
To assess the short term health effects of improving housing.
Design
Randomised to waiting list.
Setting
119 council owned houses in south Devon, UK.
Participants
About 480 residents of these houses.
Intervention
Upgrading houses (including central heating, ventilation, rewiring, insulation, and re‐roofing) in two phases a year apart.
Main outcome measures
All residents completed an annual health questionnaire: SF36 and GHQ12 (adults). Residents reporting respiratory illness or arthritis were interviewed using condition‐specific questionnaires, the former also completing peak flow and symptom diaries (children) or spirometry (adults). Data on health service use and time lost from school were collected.
Results
Interventions improved energy efficiency. For those living in intervention houses, non‐asthma‐related chest problems (Mann–Whitney test, p = 0.005) and the combined asthma symptom score for adults (Mann–Whitney test, z = 2.7, p = 0.007) diminished significantly compared with control houses. No difference between intervention and control houses was seen for SF36 or GHQ12.
Conclusions
Rigorous study designs for the evaluation of complex public health and community based interventions are possible. Quantitatively measured health benefits are small, but as health benefits were measured over a short time scale, there may have been insufficient time for measurable improvements in general and disease‐specific health to become apparent.
Keywords: housing, health service utilisation, quality of life, respiratory illness, community participation
The links between poor health and housing conditions have long been recognised.1,2,3,4 Asthma, arthritis, rheumatism, heart disease, and poor mental health have all been associated with damp, cold housing, and poor ventilation.5 Such associations have been recognised in government reports and policies for some time,3 but are mostly derived from methodologically weak evidence, such as cross sectional studies.6,7,8 A causative relation between health and housing conditions has thus not been conclusively established. Persuasive evidence of a causative relation between poor housing conditions and poor health will have profound effects on social policy. In particular, establishing such a link will have implications for a government's investment in both housing and health. Although the need for such evaluations has been recognised,6 we are aware of only one previous randomised study.9 Successful rigorous evaluations in this field might prove transferable to other community‐wide interventions.
Methods
Background and study design
The study was set in Torquay, which is a popular holiday resort on the south coast of England and, although outwardly affluent, has pockets of deprivation. Watcombe is an estate of former council owned properties in Torquay with a Jarman index of 22.70 (indicating much higher levels of deprivation than the Devon average of 12.75) and the highest out of hours visiting rate by family doctors in the town—15% above the town average.10 Half the estate population were receiving benefits and 45% of children under five were living in single parent households. Study development and design have been described elsewhere.11 A randomised to waiting list design was agreed with residents and the Council. The South Devon local research ethics committee gave approval for the study.
Our evaluation attempted to answer the question of whether housing upgrades improved the general or disease‐specific health of the residents in the first year after the improvements.
Populations
Houses
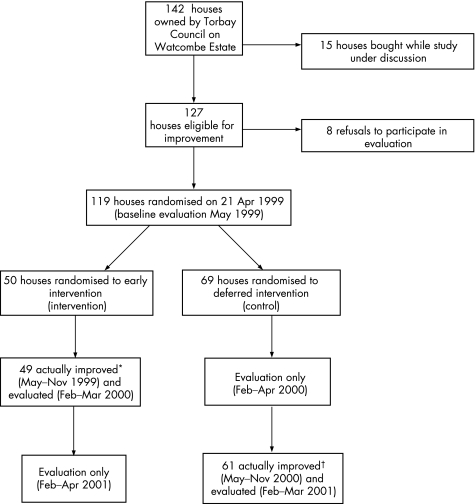
Of the 142 properties on the estate, 15 were purchased under the Right to Buy (RTB) initiative and eight declined to participate in the evaluation scheme, leaving 119 houses eligible for randomisation (fig 1).
Figure 1 Flow chart: the Watcombe Housing Study. *One household dropped out of the study; its replacement was not randomised and therefore omitted from the evaluation. †Four houses not improved due to tenants exercising their Right To Buy; two households left before improvements; one refused following randomisation; one denied access to house. (The Council took the decision not to improve those houses of tenants who exercised their Right To Buy, or for the reasons given above.)
Residents
There were 481 people living in randomised houses at the start of the study (table 1), although numbers fluctuated subsequently.
Table 1 Comparison of residents in houses improved as an early intervention compared with those in houses deferred for improvement at start of study.
| Intervention | Control | |
|---|---|---|
| (a) Houses | ||
| House type | n = 50 (%) | n = 69 (%) |
| Semi‐detached | 28 (56) | 33 (48) |
| Terrace | 14 (28) | 22 (32) |
| End terrace | 8 (16) | 14 (20) |
| Occupancy | n = 48 (%) | n = 63 (%) |
| Not overcrowded (<1 person/room) | 33 (69) | 49 (78) |
| Overcrowded (1–1.5 person/room) | 14 (29) | 13 (21) |
| Severe overcrowding (1.5+ person/room) | 1 (2) | 1(2) |
| Heating | n = 48 (%) | n = 63 (%) |
| Central heating downstairs | 30 (63) | 39 (62) |
| Central heating upstairs | 5 (10) | 5 (8) |
| Open fire downstairs | 8 (17) | 5 (8) |
| Gas fire downstairs | 35 (73) | 48 (76) |
| Temperature | n = 48 (%) | n = 65 (%) |
| Living room below 21°C | 43 (90) | 58 (89) |
| Bedroom below 18°C | 38 (79) | 49 (75) |
| Indoor air pollutant exposure | n = 49 (%) | n = 63 (%) |
| With pet | 34 (71) | 43 (68) |
| With smoker | 37 (77) | 42 (67) |
| Gas cooking | 33 (67) | 40 (64) |
| (b) Residents | ||
| Sex | n = 209 (%) | n = 272 (%) |
| Male | 104 (50) | 133 (49) |
| Female | 105 (50) | 139 (51) |
| Age (years) | n = 207 (%) | n = 269 (%) |
| 0–4 | 30 (15) | 26 (10) |
| 5–17 | 94 (45) | 109 (42) |
| 18–44 | 65 (31) | 80 (31) |
| 45–64 | 13 (6) | 35 (13) |
| 65+ | 5 (2) | 12 (5) |
| Employment | n = 82 (%) | n = 120 (%) |
| Unemployed | 41 (50) | 52 (43) |
| Smoking | n = 109 (%) | n = 136 (%) |
| Yes | 47 (43) | 55 (40) |
| Suffer from asthma | n = 207 (%) | n = 263 (%) |
| Yes | 58 (28) | 66 (25) |
Randomisation
Randomisation took place at a public meeting, with a local councillor pulling the house numbers out of a bucket. Funding was available for 50 houses to be upgraded during the first year (intervention) and the remaining 69 were improved the following year (control).
Statistical considerations
Sample size was determined by the population of 142 houses, which was estimated at 580. Houses, and hence residents, were allocated at random to intervention and control groups. Assuming a response rate to the questionnaires of 67% (390 respondents), and using a two sided alternative hypothesis at a type I error level of 5%, the study would have a power of 80% to detect a difference of 12% in the prevalence of a current respiratory condition (for example, bronchitis in the previous month) between the residents of improved and unimproved houses (that is, 30% in unimproved houses, 18% in improved).
Intervention
Improvements were aimed at bringing each house up to current standards and included re‐roofing, full central heating, rewiring, ventilation systems, double glazed doors, cavity wall and roof insulation. Residents also received a booklet explaining the correct use of the new equipment.
Data and data collection
Data collection is summarised in table 2. An annual postal questionnaire elicited information on a range of conditions potentially influenced by housing. Questions were based on conditions identified by the residents as affected by their housing. This was sent to the contact name on the Council's housing list. One respondent replied to questions concerning the house, each adult completed a health questionnaire, and children under 16 had a health questionnaire completed on their behalf. All adults were later interviewed by a community nurse trained in the use of the survey instruments. Those reporting wheeze, arthritis, rheumatism, or angina in the postal survey and who confirmed this at interview were administered condition specific severity schedules12,13,14 and asked about current medication. At this point too, respondents completed the SF3615 and GHQ12.16 Data on health care utilisation comprised hospital admissions, accident and emergency department (A&E) attendances, and primary care contacts through hospital activity data and general practitioner (GP) notes, respectively. Energy savings from the housing improvements were imputed using standard assessment procedure (SAP) scores, or energy rating, for the intervention and control houses. The SAP rating assesses the energy efficiency of a building from its capacity, design, and construction.17 Data collection was repeated annually throughout the course of the study, during late winter and early spring. The time between completion of the upgrades and the collection of health data was variable but in the majority of cases it was between six and nine months.
Table 2 Health and economic outcome measures.
| Outcome | Instrument | Mode of collection | Respondents |
|---|---|---|---|
| General health | SF36 | Self completion during interview* | All adults |
| GHQ12 | |||
| Respiratory health | Asthma symptom questionnaire (symptoms over preceding month) | Completed during interview* | Adults and children reporting respiratory illness† |
| Symptoms | 3 day diaries | Self completion (parents and children) | Children reporting respiratory illness (asthma)† |
| (a) smiley faces | age <6 | ||
| (b) bother profile | age 6–17 | ||
| Lung function | |||
| PEFR | Peak flow meter | During interview* | Children reporting respiratory illness age 6–17† |
| FEV1/FVC | Spirometer | During interview* | Adults reporting respiratory illness† |
| Medication | Proforma | Completed by nurse during interview* | Adults and children reporting respiratory illness† |
| Musculoskeletal health | |||
| Symptoms | AIMS questionnaire (symptoms over preceding month) | Completed during interview* | Adults reporting arthritis or rheumatism† |
| Medication | Proforma | Completed by nurse during interview* | Adults reporting arthritis or rheumatism† |
| Health service contacts | |||
| Primary care consultations | GP records | Retrospective record review | All adults and children |
| A&E attendances | A&E records | ||
| Hospital admissions | Hospital records | ||
| Time lost from school because of asthma | Questionnaire | Completed by nurse during interview* | School age children reporting respiratory illness† |
| Interventions to houses and improvement costs | Questionnaire | Collected by nurse at interview* | All houses |
| Torbay Council records | Retrospective record review |
*Interviews conducted in respondents' houses by community nurses trained in the use of the instruments.
†Residents reporting specific health conditions (respiratory illness (asthma, bronchitis or other), arthritis and rheumatism) identified by postal questionnaire 4–5 months before interviews conducted. This questionnaire also collected information on household size, employment, heating and cooking methods, smoking habits, and pet ownership. It was completed by one adult member of each household.
A&E, accident and emergency department; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; GHQ12, 12 item general health questionnaire; GP, general practitioner; SF36, 36 item short form health survey.
Information on contacts with primary health care professionals (GP, practice nurse, health visitor, telephone advice) and pharmaceuticals was collected from GP records. The cost per primary care contact was obtained from work published by the Personal Social Services Research Unit of the University of Kent at Canterbury.18 Pharmaceuticals were priced using the electronic version of the British National Formulary. Information on secondary care use (inpatient stays, outpatient visits, and A&E attendances) was obtained from computerised hospital records and costed using NHS reference costs. All costs are expressed at October 2000 prices.
Analysis
The primary end point of the study was the change in outcomes between 1999 and 2000 for the occupants of those houses in the intervention group compared with those in the control group (fig 1). At this point, houses in the intervention group had been upgraded and those in the control group were awaiting upgrading. The statistical test used here was the Mann–Whitney U test, using SPSS version 11.5. Analysis was conducted on an intention to treat basis.
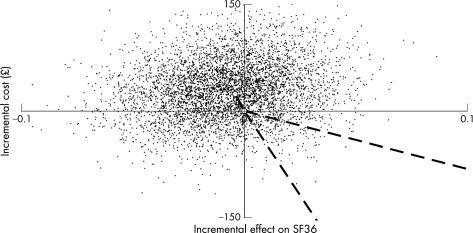
For the cost‐effectiveness analysis, the health gain for adults was calculated from the SF36 (v2), using an algorithm by Brazier19 to determine utility flows pre‐ and post‐intervention. For children, the outcome measure used was the value of lost education for those children reporting asthma symptoms. Energy savings from the housing improvements were imputed using the change in energy efficiency ratings (SAP) scores pre‐ and post‐ intervention. Intervention costs were then calculated net of energy savings, with annual equivalent housing costs calculated using the Treasury discount rate of 3.5%. Angular confidence limits were calculated by re‐sampling data for adults based on incremental SF36 scores and incremental costs, both derived from an analysis of covariance (ANCOVA) procedure to control for differences in pre‐intervention SF36 scores. If individual cost elements were missing, incremental health care and housing costs were imputed.
Results
Randomisation produced similar frequencies of potential confounders in each group (table 1).
For the self completed questionnaires and health interviews, response rates, as a proportion of our baseline sample, were 99% and 86%, respectively, in the first year, 87% and 86% in the second, and 91% and 66% in the third.
Between 1999 and 2000, changes in the frequency of self reported asthma, arthritis, rheumatism, angina, and bronchitis are not significantly different between the two groups (table 3). For respiratory conditions, including bronchitis but excluding asthma, the difference was significant, with residents of unimproved houses reporting increased levels of these conditions (Mann–Whitney, z = 2.8; p = 0.005). The symptoms also include itchy eyes, watery eyes, blocked nose, running nose, and dry throat.
Table 3 All residents reporting target conditions by year and phase.
| 1999 | 2000 | 2001 | 1999–2000 | ||||
|---|---|---|---|---|---|---|---|
| I | C | I | C | I | C | Comparison of prevalence change between I and C | |
| Number (%) | 207 | 263 | 193 | 254 | 187 | 239 | p Value |
| Suffering from: | |||||||
| Asthma | 58 (28) | 66 (25) | 40 (21) | 55 (22) | 27 (14) | 34 (14) | 0.36 |
| Arthritis | 16 (8) | 26 (10) | 16 (8) | 20 (8) | 18 (10) | 27 (11) | 0.93 |
| Rheumatism | 8 (4) | 6 (2) | 14 (7) | 10 (4) | 3 (2) | 9 (4) | 0.65 |
| Arthritis/rheumatism† | 22 (11) | 29 (11) | 25 (13) | 26 (10) | 20 (11) | 31 (13) | 0.99 |
| Bronchitis | 7 (3) | 17 (7) | 13 (7) | 17 (7) | 6 (3) | 6 (3) | 0.52 |
| Other respiratory* | 24 (12) | 19 (7) | 22 (11) | 29 (11) | 16 (9) | 19 (8) | 0.005 |
†Arthritis or rheumatism, or both.
*Includes bronchitis but excludes those with asthma.
C, control; I, intervention.
Asthma symptoms over the preceding month were rated on a five point scale12 and analysed individually and as summed scores, for both adults and children (tables 4 and 5). Adults, but not children, in improved houses showed a significant improvement in the combined symptom score (Mann‐Whitney, z = 2.7, p = 0.006).
Table 4 Mean asthma symptom score and asthma step by age, year, and group: adults.
| 1999 | 2000 | 2001 | Change 1999–2000 (where both available) | p Value changes, | |||||
|---|---|---|---|---|---|---|---|---|---|
| I | C | I | C | I | C | I | C | I v C | |
| Number | 20 | 25 | 18 | 20 | 9 | 19 | 14 | 13 | |
| Breathless on exercise | 3.7 | 3.8 | 3.3 | 3.2 | 3.3 | 3.0 | –0.3 | –0.6 | 0.62 |
| Breathless not on exercise | 2.6 | 2.0 | 2.0 | 2.1 | 2.2 | 2.0 | –0.6 | +0.2 | 0.38 |
| Wheeze day | 2.3 | 2.6 | 2.2 | 2.7 | 2.4 | 2.3 | –0.4 | +0.4 | 0.26 |
| Wheeze night | 2.9 | 2.2 | 2.5 | 2.0 | 2.7 | 2.3 | –0.6 | +0.1 | 0.38 |
| Cough day | 2.5 | 2.4 | 2.2 | 2.8 | 3.0 | 2.4 | –0.4 | +0.3 | 0.30 |
| Cough night | 2.4 | 2.0 | 2.5 | 2.7 | 2.9 | 2.5 | –0.1 | +0.7 | 0.14 |
| Summed score | 16.4 | 15.0 | 14.7 | 15.4 | 16.6 | 14.3 | –2.3 | +1.1 | 0.006 |
C, control; I, intervention.
Table 5 Mean asthma symptom score and asthma step by age, year, and group: children.
| 1999 | 2000 | 2001 | Change 1999–2000 | p Value changes, | |||||
|---|---|---|---|---|---|---|---|---|---|
| (where both available) | |||||||||
| I | C | I | C | I | C | I | C | I v C | |
| Number | 36 | 45 | 28 | 29 | 20 | 27 | 25 | 27 | |
| Breathless on exercise | 2.3 | 2.8 | 2.1 | 2.4 | 1.9 | 1.8 | –0.4 | –0.2 | 0.42 |
| Breathless not on exercise | 1.5 | 1.8 | 1.3 | 1.6 | 1.3 | 1.3 | –0.2 | 0.0 | 0.21 |
| Wheeze day | 2.0 | 2.3 | 1.8 | 1.9 | 1.5 | 1.4 | –0.2 | 0.0 | 0.38 |
| Wheeze night | 1.9 | 2.4 | 1.8 | 1.8 | 1.6 | 1.4 | –0.3 | –0.2 | 0.51 |
| Cough day | 2.7 | 2.6 | 2.4 | 2.3 | 2.2 | 2.0 | –0.5 | –0.2 | 0.58 |
| Cough night | 2.7 | 2.7 | 2.3 | 2.2 | 2.3 | 2.2 | –0.6 | –0.3 | 0.27 |
| Summed score | 12.9 | 14.6 | 11.8 | 12.2 | 10.7 | 10.1 | –1.8 | –1.0 | 0.17 |
C, control; I, intervention.
Prescribed medication, as reported by each respondent reporting asthma, was used to calculate their “step” according to the BTS management guidelines for chronic asthma.20Table 6 includes all those reporting asthma, whether or not they also report current symptoms, medication use, or both. Similar patterns are seen if those reporting asthma, but not symptoms or medication, are excluded (data not shown). Paired data also show similar results.
Table 6 Mean BTS asthma step.
| 1999 | 2000 | 2001 | Change 1999–2000 (where both available) | p Value changes, | |||||
|---|---|---|---|---|---|---|---|---|---|
| I | C | I | C | I | C | I | C | I v C | |
| Number (adults/children) | 20/36 | 25/45 | 18/28 | 20/28 | 6/15 | 13/24 | 14/25 | 13/27 | |
| Adults | 1.5 | 1.3 | 1.3 | 1.4 | 2.0 | 1.9 | –0.1 | –0.2 | 0.72 |
| Children | 0.8 | 1.1 | 0.6 | 1.2 | 0.8 | 0.9 | –0.2 | –0.1 | 0.59 |
BTS, British Thoracic Society; C, control; I, intervention.
No significant differences between groups or over time were seen in any of the subscales of the SF36. The GHQ12 score improved over time, but not significantly (data not shown).
No significant changes in spirometry were seen in those reporting asthma, either between groups or over time.
Total costs to Torbay Council varied between groups; for the 49 houses improved in 1999, total costs were £380 240, giving an average cost per house of £7760, while for the 63 houses improved in 2000 with different contractors the total cost was £332 538, giving an average cost per house of £4819.
There was no significant difference in intervention costs, health care costs, and utility flows between occupants in intervention houses compared with those in control group houses (table 7). Angular confidence limits show replicates distributed across all sectors of the cost‐effectiveness plane (fig 2), implying that it is not possible to determine whether housing improvements produce a utility gain (in terms of health or more schooling) for occupants of improved houses.
Table 7 Costs and consequences of housing improvements.
| 1999 Cost per person (n) | 2000 Cost per person (n) | 2001 Cost per person (n) | ||||
|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |
| Annual equivalent intervention costs net of annual energy saving | £0 (174) | £0 (228) | £–18.82 (158) | £0 (225) | £0 (174) | £–16.56 (174) |
| Health care costs | ||||||
| Inpatient costs | £37.44 (93) | £54.95 (140) | £41.57 (93) | £14.34 (137) | £10.78 (97) | £35.82 (134) |
| Outpatient costs | £105.62 (93) | £101.86 (140) | £108.95 (93) | £66.46 (137) | £76.62 (97) | £61.06 (134) |
| A&E costs | £13.28 (93) | £13.64 (140) | £10.1 (93) | £10.72 (137) | £2.73 (97) | £3.16 (134) |
| Primary care consultation costs | £55.38 (87) | £62.63 (131) | £44.82 (88) | £59.31 (127) | £44.53 (72) | £50.68 (118) |
| Primary care pharmaceutical costs | £3.5 (93) | £6.92 (140) | £9.61 (93) | £11.74 (137) | £5.47 (97) | £11.61 (134) |
| Primary care out of hours costs | £2.31 (86) | £1.74 (130) | £2.47 (89) | £0.55 (126) | £2.00 (74) | £2.66 (117) |
| All NHS costs | £204.86 (85) | £220.49 (129) | £224.97 (88) | £171.54 (124) | £135.72 (70) | £165.56 (116) |
| Benefits | ||||||
| SF36 (adults) | 0.73 (62) | 0.75 (77) | 0.77 (57) | 0.8 (78) | 0.72 (35) | 0.8 (74) |
| Value of lost education (children) | £240.7 (19) | £288.44 (45) | £352.28 (17) | £247.59 (37) | £80.92 (16) | £169.92 (35) |
SF36, 36 item short form health survey.
Figure 2 Bootstrapped cost‐effectiveness estimate (solid line) with 95% angular confidence intervals (hatched lines) for the incremental effect of the intervention compared with controls.
Discussion
The Watcombe Study is only the second randomised trial of housing conditions we are aware of, but provides a possible template for the evaluation of other similar interventions. The study arose from the community development project funded by the Health Authority, which led to the residents conducting their own survey of their housing conditions. As the residents had identified their housing needs, they were interested in the evaluation study and keen to help. The project team tried to maintain the residents' interest and engagement throughout the research process. The outstanding response rates reflect this partnership, which has continued after the study. Residents have described their participation at both local and national meetings.
The interventions succeeded in producing warmer, drier houses that were more energy efficient as measured by changes in the indoor environment and energy rating (SAP) of the house; these results are reported in detail elsewhere.21 Residents appreciated the improvements and felt their health and wellbeing had improved as a result, as elicited by a small number of semistructured interviews.22 Greater use of the whole house, improved relationships within families, and a greater sense of self esteem were all mentioned as benefits. It is thus disappointing that these benefits are not generally reflected in the health outcomes. It may be that the time between the intervention rounds was too short to produce more appreciable differences in the physical health of residents. However, it would not have been possible to delay the second round of interventions longer without losing the participants' goodwill. Practical considerations to do with timetabling the improvements also detracted from our (theoretically) robust design: building work was delayed occasionally and thus the time between upgrading and outcome measurement was variable.
Respiratory health
We expected that respiratory health would be the most likely condition to show improvement following intervention, both because of the existing evidence base and because asthma was the commonest health problem reported by the residents. Results, however, are conflicting.
For the primary end point, we saw no difference between occupants of intervention compared with control houses in terms of self reported prevalence of asthma or severity of disease, as measured by medication use according to BTS asthma guidelines. Symptom scores over the previous month did show a difference, with residents in intervention houses having a reduction in total symptom score from 1999 to 2000, while residents of control houses showed a small increase in score. This lack of effect on asthma prevalence is not surprising, as we would not anticipate that housing improvements would alter the underlying tendency to asthma in individuals. Housing improvements, however, may alter asthma severity in either direction: it is possible that during the improvements, asthma symptoms worsen because of indoor air pollutants but improve in the long term because of a warmer, drier home. We have no information on the time scale over which these possible changes may occur. Upgrading had barely been completed in some homes when the self completed questionnaire was carried out, while the health surveys recording symptoms and medication were completed some three to four months later. It may be that a longer period is needed for some health benefits to appear.
What is already known
There is an association between poor housing conditions and a range of physical and mental illnesses.
Only one randomised trial of housing has been published.
Public health interventions are rarely rigorously evaluated.
There was also a difference in reported levels of “other respiratory” conditions, including bronchitis, with an increase reported in residents of unimproved houses while those in improved houses showed little change. We are not certain what this category consists of, but it probably includes intercurrent respiratory infections likely to be prevalent during January when the self reported questionnaire was completed. The difference in symptom score may reflect these other conditions, rather than asthma, suggesting that residents of control houses were more susceptible. The lack of change in asthma medication would also suggest that this increase in prevalence and symptoms is short term.
What this study adds
Improved housing leads to a lessening of asthma symptoms in adults and appears to protect against non‐asthma respiratory conditions in adults and children.
Improved housing changes the way the house is used and has a beneficial influence on relationships within the household.
It is possible to conduct randomised trials on community‐wide interventions.
Overall asthma prevalence reduced markedly across the three years of the study, but this was not associated with the housing improvements. If people with mild asthma or intermittent symptoms only did not continue to report their condition in the later years of the study, we would expect symptom scores and medication use to increase, reflecting a smaller number of current asthmatics with more chronic and severe disease. In children, symptom scores tend to decrease and medication use is unchanged, suggesting that this reduction in prevalence is associated with a genuine reduction in morbidity. In adults, medication use possibly increases while symptom scores remain unchanged, which could be interpreted as indicating an increase in severity of disease accompanied by more effective management. The study raised awareness of the BTS asthma guidelines in local practices. A reduction in symptom scores coupled with an increase in medication use may indicate that guidelines were being followed more conscientiously, leading to more effective control of symptoms. It is not certain, however, that this is the likeliest interpretation of this finding in adults.
The reduction in asthma prevalence does not therefore seem to be completely explained by changes in asthma reporting, disease severity, or management, although all may have some role. There were no changes in smoking prevalence or pet ownership, both of which were high throughout the study.
Further support for the reduction in asthma prevalence being genuine comes from the lack of a trend in the prevalence of other conditions, particularly arthritis and rheumatism. In addition, we have seen no effect of housing improvements on the severity of arthritis or rheumatism. Again, it may be that our timescale is too short and that it takes longer than a few months for any benefits to become apparent.
The economic data represent NHS costs for all conditions, not just the ones the residents reported as being common or associated with their housing conditions. Results may therefore be influenced by one or two heavy service users whose conditions may have no connection with their housing situation—for example, an adult with leg ulcers requiring frequent home visits from community nurses and another with cancer requiring many admissions to hospital and home visits. We felt it important, however, to include all service use, particularly as the stimulus for setting up the initial community development project had been the heavy use of primary care and out‐of‐hours services by the local population. In contrast, we only collected data on NHS service use in those children who reported having asthma in the first survey. Our only measure of utility welfare in these children is time lost from school and the question has been confined to loss of schooling caused by asthma rather than other conditions. Our lack of effect on service use and schooling may again reflect time scales over which improvements occur.
The improvement in theoretical energy efficiency of the houses was substantial. This improvement might translate into an increased ability of the residents to keep their homes heated to a comfortable temperature, and we have some evidence from the environmental measurements that indoor temperatures improved as a result of the intervention,22 as well as the residents using more rooms in the house. Alternatively, residents may have chosen to heat their houses to the same temperature as previously, but at lower cost, and used the savings in other ways. However, we have no information on either the residents' actual expenditure on heating (consultation with residents revealed that they were unhappy at being asked such a question and, in any case, it was difficult to record current cost as payments frequently incorporated debt repayment), or any alternative use of savings such as increased expenditure on food. The high levels of unemployment and other markers of deprivation on the Watcombe estate suggest that many households would meet the criteria for being in fuel poverty,3 but we have no direct information on this. Nevertheless, as it seems likely that housing improvements can save money on heating bills, the consequent reduction in fuel poverty might be a sufficient reason for implementing a programme to upgrade the housing stock. In addition, the improvements in use of the houses and domestic relationships suggest other benefits that our specific quantitative outcome measures have been unable to capture and would also justify the expenditure.
There are very few trials of the effect of housing interventions on health with which we can compare our results. A systematic review6 identified 18 intervention studies, several of which found positive effects on health of improving housing, but the investigators commented that the small study sizes and lack of controlling for confounders limits their generalisability. The only other randomised study of which we are aware9 assessed the effect on mental health of rehousing people who were on the priority list for rehousing on medical grounds. While that study found an improvement in mental health after rehousing, its size, context, and the outcomes used are very different. However, it does show the feasibility of randomisation in a non‐health‐care setting while acknowledging the impossibility of maintaining other aspects of good randomised controlled trial design, such as concealment of allocation and blinding.
Conclusions
This study provides a model for the rigorous evaluation of community‐wide interventions such as housing improvements. There is limited evidence that housing improvements protect against respiratory disease, either asthma or non‐asthma‐related conditions. Future studies require similarly robust designs and incorporating qualitative components, but further methodological work is required, particularly on the quality, relevance, and sensitivity of outcome measures.
Acknowledgements
We are grateful to the residents of the Watcombe Housing Estate for their support and contributions throughout the study, to the Housing Department of Torbay Council and the Riviera Housing Trust.
Abbreviations
BTS - British Thoracic Society
GHQ - general health questionnaire
SAP - standard assessment procedure
SF36 - 36 item short form health survey
Footnotes
Funding: The study was funded by the NHS Executive Research & Development Directorate, South West.
Competing interests: None.
References
- 1.Black D, Morris J, Smith C.et alInequalities in health: report of a research working group. London: DHSS, 1980
- 2.Acheson D.Independent inquiry into inequalities in health. London: HMSO, 1988
- 3.Molyneux P. Making the case. Renovation and refurbishment. Briefing paper: Health & Housing. London: Health and Housing, 2000
- 4.Department of Health Tackling inequalities: a programme for action. London: HMSO, 2003
- 5.BMA Board of Education and Science Housing and health: building for the future, May 2003
- 6.Thomson H, Petticrew M, Morrison D. Health effects of housing improvement: systematic review of intervention studies. BMJ 2001323187–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilkinson D. Poor housing and ill health. A summary of research evidence. Housing Research Branch. The Scottish Office Central Research Unit, 1999. http://www.scotland.gov.uk/cru/documents/poor‐housing‐08.htm [26/06/2001]
- 8.Elliott E, Landes R, Popay J.et al Regeneration and health: a selected review of research”. In: Popay J, ed. Nuffield Institute for Health. Leeds: University of Leeds, 2001
- 9.Elton P J, Packer J M. A prospective randomised trial of the value of rehousing on the grounds of mental ill‐health. J Chron Dis 198639221–227. [DOI] [PubMed] [Google Scholar]
- 10.Plymouth and Torbay Health Authority Barton, Watcombe and Hele Health Gain Initiative June 1994
- 11.Somerville M, Basham M, Foy C, on behalf of the Torbay Healthy Housing Group et al From local concern to randomized trial: The Watcombe Housing Project. Health Expectations 20025127–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steen N, Hutchinson A, McColl E.et al Development of a symptom based outcome measure for asthma. BMJ 19943091065–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meenan R F, Gertman P M, Mason J H. Measuring health status in arthritis. The arthritis impact measurement scales. Arthritis Rheum 198023146–152. [DOI] [PubMed] [Google Scholar]
- 14.Rose G A. The diagnosis of ischaemic heart pain and intermittent claudication in field surveys. Bull WHO 196227645–658. [PMC free article] [PubMed] [Google Scholar]
- 15.Ware J E, Sherbourne C D. The MOS 36‐item short‐form health survey (SF‐36). I. Concepual framework and item selection. Med Care 199230473–483. [PubMed] [Google Scholar]
- 16.Goldberg D P, Williams P.A user's guide to the general health questionnaire. Windsor: NFER‐Nelson, 1998
- 17.Everall P F. The Government's Standard Assessment Procedure (SAP) for energy rating of dwellings. DETR Circular Letter 31 March 1999. London: HMSO, 1999
- 18.Netten A, Curtis L.Unit costs of health and social care 2001. Personal Social Services Research Unit, University of Kent, Canterbury 2001
- 19.Brazier J, Roberts J, Deverill M. The estimation of a preference‐based measure of health from SF‐36. J Health Econ 200221271–292. [DOI] [PubMed] [Google Scholar]
- 20.BNF Management of chronic asthma in adults and children. British National Formulary www.bnf.org
- 21.Richardson G, Barton A, Basham M, on behalf of the Torbay Healthy Housing Group et al The Watcombe Housing Study: the short term effect of improving housing on the indoor environment. Sci Total Environ 200636173–80 Epub 2005 Jun 24. [DOI] [PubMed] [Google Scholar]
- 22.Basham M. A qualitative study: central heating, its influence on the use of the house, the behaviour and relationships of the household in wintertime. Unpublished Masters Thesis. Plymouth: University of Plymouth, 2001