Abstract
The aim of this study was to investigate whether a relationship exists between ethnicity and uptake of the first dose of mumps, measles and rubella (MMR1) vaccination, and to study important factors influencing the parental decision about vaccination. Examination of routine data on uptake of MMR1 vaccine among children living in the London borough of Brent, North West London, for associations with ethnicity was carried out. Six focus group interviews were held and a questionnaire on factors related to immunisation by convenience samples of mothers from Asian, Afro‐Caribbean and White backgrounds was completed. The routine data reported MMR1 vaccine status for 6444 children living in Brent who were aged between 18 months and 3 years on 1 December 2003. A total of 37 mothers took part in the 6 focus group sessions. Significantly higher coverage by MMR1 vaccine in the Asian population (87.1%) compared with Afro‐Caribbeans (74.7%) and the White group (57.5%) was noticed. The qualitative data revealed clear differences between the ethnic groups with respect to awareness of the controversy surrounding MMR vaccination (related to use of English‐language media) and influence of grandparents and health professionals in decisions about immunisation. A multiple logistic regression model showed that although coverage of MMR vaccination increased with increasing socioeconomic status, there was no evidence of a statistically significant interaction between socioeconomic status and ethnicity. An important association between ethnicity and uptake of MMR1 vaccine is observed. This has implications for efforts to improve the currently inadequate levels of MMR vaccination across the population as a whole.
Measles is still the most common cause of child death worldwide.1 Although most cases occur in developing countries, outbreaks of measles still occur in Europe, with occasional fatalities. The World Health Organization aims to eliminate the indigenous measles virus from the European region by 2007.2 However, the current public debate in the UK about the safety of the mumps, measles and rubella (MMR) vaccine and the resulting decrease in uptake after 19973 have rendered this target unrealistic. Following a report in 1998 suggesting a possible link between the MMR vaccine and autism,4 immunisation has become a controversial issue. Yet, relatively little is known about parents' views, specifically among different ethnic groups.
After the MMR vaccination was introduced in 1988, coverage at national level increased from 80% in 19893 to 92% in 1997.3 Levels of uptake started to decline in 1997, and had fallen to 87.9% by 2001.3 A similar decrease in uptake has taken place in Brent, North‐West London, where, in 2002, only 78.4% of the population who were eligible to receive the first dose of the MMR vaccine (MMR1) had done so (Brent PCT MMR Records Interface Audit: 2002–2003—unpublished data). This is well below the 95% level advocated by the Department of Health in order to achieve herd immunity. The decline in immunisation in Brent is of special concern as a number of cases of measles were reported within the borough during 2004. Four children required admission to hospital and one spent time in an intensive care unit.
Given the consequences of a decline in uptake of MMR vaccine, it is extremely important that the factors involved in decisions about vaccination are fully understood. In their work, Roberts et al5 identified important factors such as lay beliefs about vaccination, advice from health professionals, socioeconomic status, religious or moral beliefs about immunisation, media representation of vaccination, and structural issues such as access to vaccination clinics and appointment times.
There are few studies examining associations between ethnicity and uptake of the MMR vaccine. Baker et al6 failed to identify any directly relevant work, but documented the differences between the ethnic groups in terms of uptake of vaccination. They made no attempt to investigate the factors behind the observed differences. Similarly, a study undertaken among Asian children living in Glasgow7 did not include efforts to identify the reasons behind the findings that coverage by immunisation was higher among the Asian group compared with controls from European backgrounds. A study by Martineau et al8 found that there was no difference in immunisation between the sexes within Asian groups who had migrated to Britain. There is a difference in rates between the sexes, however, in the countries from which they had migrated. The researchers discussed the possibility of the free healthcare system in Britain as being an important reason for this finding.
The UK is extremely ethnically diverse and over four million people living in Britain come from minority ethnic groups.9 Each ethnic group has its own set of beliefs that influence the decisions of its members. Differences in health needs, approaches to health and definitions of health can exist even within small geographical areas. At the same time, there is a strong inter‐relationship between deprivation and health outcomes,9 and ethnic minority groups in the UK tend to have a more unfavourable socioeconomic profile than the indigenous White population.9 In a study of the social distribution of MMR immunisation between 1991 and 2001,10 the coverage was higher among affluent populations, but the decline in uptake of the MMR vaccination seen after 1998 was more marked within this group. Similarly, unpublished data from Brent show an MMR vaccination “cold spot” in the more affluent areas of the borough, within a mainly White population. Before 1998, this area had the highest uptake within the borough.
We investigated whether ethnicity is associated with uptake of the first dose of MMR (MMR1) vaccination and sought to elicit the important factors influencing parental decisions about vaccination. We also examined the relationship between socioeconomic status and uptake of MMR vaccine.
Methods
This study was conducted in Brent, North‐west London. Uptake of the MMR1 vaccine, according to ethnic origin, was assessed using routine data from the Brent Primary Care Trust (PCT) database for all children aged between 18 months and 3 years on 1 December 2003 (appendix). Data for 6444 children (including date of birth, MMR vaccination status, maternal ethnicity and individual postcodes) were retrieved and entered into a Microsoft Excel spreadsheet. Ethnic groups were ranked by the uptake of MMR1 vaccine (measured as a percentage) and the series was then divided into tertiles, representing high, medium and low levels of uptake of MMR1 vaccine. A relatively large ethnic group was selected from each tertile for further research in the focus‐group phase of the study: Asian, Afro‐Caribbean and White groups.
The 33 ethnic groups in the data were regrouped into ethnic categories from the 2001 Census: Asian, Black, White, Mixed or Other, and No Category Assigned, where there was no information about the mother's ethnic origin included within the routine data (http://neighbourhood.statistics.gov.uk). Regrouping was carried out in order to generate groups with sufficient numbers of subjects in so that meaningful results could be generated when statistically analysed. However, some ethnic heterogeneity in the data was lost when regrouping in this way.
Proportions of uptake of MMR1 vaccine in each census category and corresponding 95% CIs were calculated. We used the χ2 test to establish whether there was a relationship between ethnicity and uptake of MMR1 vaccine within the routine data.
Socioeconomic status was assigned to each subject using the individual's postcode. Using the all fields postcode directory, compiled by the Office for National Statistics, each postcode was allocated to a ward and the wards were then linked to the 2000 Index of Material Deprivation (IMD) score. Finally, wards were coded according to quintiles of IMD. Owing to small numbers in quintile 5, the most affluent group, we merged this category with quintile 4. The χ2 test was then used to examine the relationships between quintile of IMD and uptake of MMR1 vaccine and between quintile of IMD and ethnicity. IMD quintile and ethnicity data were entered into a multiple logistic model to examine the interaction between socioeconomic status and uptake of MMR vaccine and between socioeconomic status and ethnicity. The ethnic groups were categorised into White, African, Afro‐Caribbean, Asian (Indian, Pakistani and Bangladeshi), Other (including Black—Other, Black—British, Chinese and Mixed) and No Category Assigned. MMR vaccination status was assigned as 1, yes and 0, no.
The second part of the study explored interethnic differences in knowledge, attitudes and behaviour related to immunisation, using facilitated focus groups with parents from the three large ethnic groups identified in the first part of the study. A total of six focus group interviews were held, two per ethnic group selected. For each focus group, between 15 and 20 mothers were invited to participate. Within the Asian category, one group spoke English and the other spoke Gujarati.
Parents of young children from each of the three ethnic groups of interest were identified through pre‐existing networks, such as mother and toddler groups. This convenience sampling generated groups consisting of 6–10 individuals (a typical group size for focus group research11).
To ensure comparability across the groups, an interview guide was used. The discussions were audio taped and lasted approximately 30 min. The Asian Gujarati‐speaking group discussion was carried out using a trained medical interpreter, who translated verbatim what was said. Participants completed a questionnaire after the interview, which covered aspects of socioeconomic status using questions derived from the Townsend Material Deprivation Score. As the interviews had potential to raise anxiety among parents, having an undesirable effect upon uptake of MMR vaccine —quite the opposite of what was intended—the immunisation coordinator for Brent gave a brief talk after each discussion.
The interviews were downloaded and transcribed verbatim, and the transcripts were coded to categorise the data into different themes. We used the constant comparison method to identify the main themes arising in each group interview and reassessed these continually before conducting further interviews.12 To improve the validity of the analysis, a colleague independently coded the first two interview transcripts. The coding frame was then re‐examined and adjustments were made before the remaining transcripts were coded. We were also able to compare data from the focus groups with data gathered about groups of the same ethnic origin from the immunisation records. Finally, individuals' responses to the questionnaire were compared with patterns emerging from focus group interviews.
Ethical considerations
The Riverside Ethics Committee and Brent Ethics Committee approved the protocol for this study.
Results
Routine data
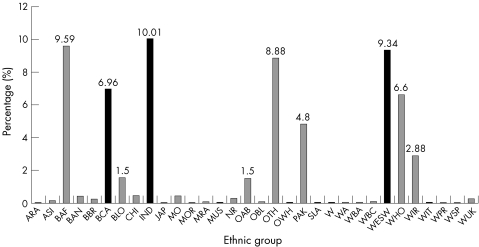
The uptake of MMR1 vaccine was reported for 6444 children in Brent. The routine data included codes for 33 different ethnic groups. Figure 1 demonstrates the proportion of children in each of these. In order to create an appropriate scale, it omits the 35% of children with no ethnicity assigned.
Figure 1 Percentage of children by ethnic group.
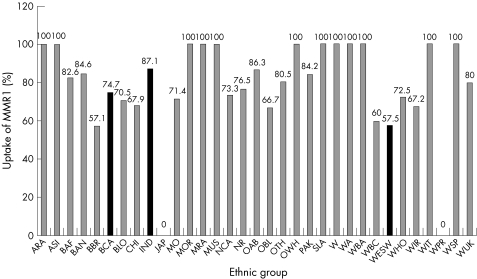
Figure 2 shows the uptake of MMR1 vaccine in each ethnic group. The highest uptake was among children from Asian backgrounds—for example, Indian (87.1%), other Asian background (86.3%), Bangladeshi (84.6%) and Pakistani (84.2%). The average across the whole of Brent was 75.0%.
Figure 2 Uptake of the first dose of mumps, measles and rubella (MMR1) vaccine by ethnic group.
The three groups selected for research in the second part of the study have been highlighted in black in figs 1 and 2. The Indian group, which accounts for 10% of the data, has the highest uptake of MMR1 vaccine, as described above. The Afro‐Caribbean group accounts for 6.7% of the data and has a medium level of uptake (74.7%). The lowest uptake, 57.5%, is in the White group, representing 9.3% of the data. Table 1 summarises the data after regrouping of individuals into principal categories from the 2001 census. There was a highly statistically significant relationship between uptake of MMR1 vaccine and ethnicity (χ2 = 152.0, df = 4, p<0.001).
Table 1 Uptake of the first dose of mumps, measles and rubella vaccine in each ethnicity category from the 2001 census.
| Asian | Black | White | Other | NCA | Total | |
|---|---|---|---|---|---|---|
| Total n (in data) | 1081 | 1192 | 1241 | 640 | 2290 | 6444 |
| Proportion of Brent total (%) | 16.9 | 18.5 | 19.3 | 9.9 | 35.5 | 100 |
| MMR1 vaccine acceptors (n) | 927 | 930 | 805 | 506 | 1667 | 4835 |
| Proportion of uptake (%, 95% CI)* | 85.7 (83.5 to 88.0) | 78.0 (75.3 to 80.7) | 64.9 (61.3 to 68.5) | 79.1 (76.0 to 82.3) | 72.8 (70.6 to 74.9) | 75.0 (74.0 to 75.1) |
MMR1, first dose of mumps, measles and rubella; NCA, no category assigned.
Table 2 shows that the Asian category had the fewest subjects classified within the most deprived quintile (1) and the largest proportion of people in the most affluent quintile (5), and conversely for the Black ethnic category. The White ethnic category fell between these. The relationship between ethnicity and socioeconomic status was highly significant (χ2 = 179.2, df = 12, p<0.001).
Table 2 Percentage of ethnic category in each Index of Material Deprivation quintile.
| Ethnic group | IMD quintile | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 and 5 | Number per group | |
| Asian | 35.2 | 54.2 | 7.1 | 3.5 | 1059 |
| Black | 60.8 | 33.6 | 4.8 | 0.7 | 1158 |
| White | 43.9 | 49.1 | 5.3 | 1.8 | 1217 |
| Other | 47.3 | 42.6 | 8 | 2.1 | 622 |
| NCA | 48.7 | 43.7 | 6.2 | 1.3 | 2226 |
IMD, Index of Material Deprivation; NCA, no category assigned.
Table 3 shows uptake of MMR1 vaccine according to socioeconomic status, indicated by quintile of IMD. We could not assign a quintile for 162 subjects (2.5% of the data), as their postcode was not recorded. Most (92.1%) of the subjects were in the two most deprived quintiles. There was no significant relationship between uptake of MMR1 vaccine and quintile of IMD (χ2 = 3.8, df = 3, p>0.3).
Table 3 Uptake of the first dose of mumps, measles and rubella vaccine in each Index of Material Deprivation quintile.
| IMD quintile | 1 | 2 | 3 | 4 and 5 | Total |
|---|---|---|---|---|---|
| Total n (in data) | 2991 | 2798 | 383 | 110 | 6282 |
| Proportion of Brent total (%) | 47.6 | 44.5 | 6.1 | 1.8 | 100 |
| MMR1 vaccine acceptors (n) | 2234 | 2102 | 290 | 91 | 4717 |
| Proportion of uptake (%) | 74.7 | 75.1 | 75.7 | 82.7 | 75.0 |
IMD, Index of Material Deprivation; MMR1, first dose of mumps, measles and rubella.
Using a multiple logistic model, it was seen that all ethnic groups had significantly higher uptake of MMR vaccine than Whites (used as the reference group; table 4).
Table 4 Uptake of mumps, measles and rubella vaccine by ethnic group relative to the White ethnic group.
| Ethnic group | OR (SE, 95% CI) |
|---|---|
| African | 2.68 (0.32, 2.07 to 3.35) |
| Afro‐Caribbean | 1.62 (0.20, 1.27 to 2.06) |
| Asian | 3.44 (0.38, 2.77 to 4.27) |
| Other | 2.06 (0.21, 1.69 to 2.52) |
| NCA | 1.07 (1.07, 1.24 to 1.67) |
NCA, no category assigned.
In this model, the summary statistics were not statistically significant, OR = 1.07, 95% CI 0.99 to 1.16.
The next model divided the quintiles into constituent strata. A clear gradient was seen across the quintiles, showing that uptake of MMR vaccine was greater in higher socioeconomic quintiles. Quintile 1 (least affluent) odds ratio (OR) = 1.10, 95% CI 0.77 to 1.59, quintile 2 OR = 1.14, 95% CI 0.79 to 1.63, quintile 3 OR = 1.21, 95% CI 0.79 to 1.86, quintile 4 OR = 1.96, 95% CI 1.05 to 3.66 and quintile 5 (most affluent) OR = 0.43, 95% CI 0.02 to 7.12. The result for quintile 5 was not unexpected because of the few subjects within this category.
Lastly, effect modification was looked for—that is, whether the relationship between ethnic group and uptake of MMR vaccine was different in different socioeconomic quintiles.
None of the combinations was found to be statistically significant, suggesting no interaction between socioeconomic quintile and ethnicity.
Policy implications
There is a need to develop and test interventions to boost coverage by the mumps, measles and rubella vaccination that take into account ethnicity and factors related to it.
What this paper adds
The paper demonstrates that ethnicity is an important correlate of uptake of the mumps, measles and rubella (MMR) vaccine, and one that is independent of socioeconomic status.
There are significant differences between ethnic groups in sources and perceived credibility of advice relating to risks and benefits of vaccination and, through differences in the use of English‐language media, in exposure to the controversy surrounding MMR vaccination specifically.
Qualitative data
The focus group discussions with 37 mothers (6 mothers per focus group, with 7 in one of the White focus groups) and their questionnaire responses supported the findings from the routine data.
It was clear that members of both the Indian groups followed their cultural tradition of consulting their elders, especially the mother‐in‐law, for advice about immunisation:
Our elders have seen the diseases in their countries … they push us more towards immunising our children.
Such key decision makers were reported as being very pro‐immunisation, and it is widely accepted in this group that immunisation is beneficial, possibly influencing their uptake, which is very high. The Asian mothers were also most likely to consult their general practitioner for advice and, more importantly, were most trusting of such advice. This was strongly highlighted by one mother who said:
The health visitor or the doctor will always say something which is beneficial to us so we accept the advice.
With healthcare professionals strongly advocating use of the MMR vaccination, especially in light of the recent decline in uptake, it seems reasonable that individuals who trust such advice will be those who have the highest uptake of the MMR vaccine. By contrast, the Afro‐Caribbean, and especially the White mothers were more likely to question the pro‐MMR vaccination advice given by healthcare professionals, which is consistent with the lower uptake seen in these groups. This was exemplified by one White mother who said:
I don't really trust anyone anymore to be honest! Even the health professionals unless I know them personally.
The general media were an important source of information for all mothers, but were also noted as causing the mothers' initial concerns about the safety of the MMR vaccination. However, the Gujarati group was unable to read English, and the Indian newspapers had little coverage of the MMR vaccination debate in the UK. Such “shielding” from adverse coverage, arising as a result of language barriers and different levels of integration into the British culture, may have contributed to the high level of immunisation within this group. The Afro‐Caribbean group did not show the same trend, as mothers from this community stated that they were more likely to read English papers.
Discussion
This study shows that there are significant differences in uptake of MMR1 vaccine between ethnic groups in Brent. Indian children show the highest uptake of MMR1 vaccine (87.1%), followed by Afro‐Caribbeans (74.7%), and Whites (57.5%) have among the lowest levels of uptake. It is important to note, however, that none of the groups achieve the 95% uptake required for herd immunity.
The focus groups revealed very few differences of opinion among mothers from the same ethnic background. The only exception was the Gujarati‐speaking mothers and English‐speaking Asian mothers, who highlighted differences in terms of the mass media to which they are exposed. This otherwise intergroup consensus is important evidence of internal validity within the project, especially as the two groups representative of a particular ethnic background were recruited for the research independently of each other.
Trust in healthcare professionals' advice seemed to contribute to many Asian mothers being unaware of alternatives to the MMR vaccination, such as the single vaccination. By contrast, in the group drawn from the population with the lowest uptake of vaccination, the Whites, this topic was a very prominent feature of discussion.
The White mothers were far better informed about the MMR vaccination debate than those in the other groups, and the Asian women seemed to be the least informed. Better‐informed health service users are likely to make the best healthcare decisions, but, where the scientific and medical community is divided, those most aware of the debate will in turn be divided, something that is clearly reflected among our White informants. Although being less aware of health matters is generally considered disadvantageous, in the case of MMR immunisation, it might paradoxically have benefits.
It is important to reflect upon the selection biases in the study. The sample was a convenience sample, with mothers invited to attend by nurses and health visitors in an opportunistic manner. It could be argued that by attending such focus group discussion, only the views of the most motivated and those most likely to take up vaccination will be captured. However, there were mothers in each group who had declined vaccination and the selection method was truly random. One improvement would have been to sample the views of healthcare professionals involved in this field. However, the dynamics of the groups would have been totally different and mothers' answers may have not have been so open and honest when addressing concerns about the vaccination.
A further consideration is that 35% of the children in the dataset had no ethnicity assigned. This reflects a problem with data collection and input into the database, which relies heavily upon communication between general practitioners and health visitors in the PCT. Should the study be repeated, better records of ethnicity for each child would be required in order to obtain a fuller picture of the vaccination trends within the PCT.
In this study, socioeconomic status was related to the uptake of MMR1 vaccine, seen through the multiple logistic analysis, although no such relationship between ethnicity and socioeconomic status was seen. There was a highly significant relationship between immunisation and ethnicity that remained significant when the logistic model was applied, taking into account both socioeconomic status and ethnicity.
However, classification of an individual via a ward‐based measure may be too crude an approach, as an individual may not reflect the characteristics of the ward in which he or she resides and may be a key limitation to the study. Alternatively, as nearly 90% of the subjects fall in the two most deprived quintiles, socioeconomic status may not actually have a significant influence upon uptake of MMR1 vaccine in Brent. Rather, ethnicity might be the more important of the two factors in this particular borough, because a larger degree of heterogeneity is associated with individuals' ethnic backgrounds than with their socioeconomic status.
We have shown that cultural background is an independent and important variable in relation to opinions about the MMR vaccine. A number of culturally determined factors influence the decision regarding uptake, independent of socioeconomic status. Hence, ethnicity cannot simply be regarded as a proxy measure for socioeconomic status. However, a more detailed analysis of the importance of socioeconomic status in different ethnic groups is needed to generate a clearer picture of the importance of this factor, compared with ethnicity, as a correlate of opinions about MMR vaccination.
Acknowledgements
We thank all the mothers who participated in this study, the health visitors for their help in arranging the meetings and Kate Woodhouse for her help throughout this project.
Abbreviations
IMD - Index of Material Deprivation
MMR - mumps, measles and rubella
MMR1 - first dose of MMR
PCT - primary care trust
Appendix
Ethnicity codes used on Brent Primary Care Trust database.
| ARA | Arab |
| ASI | Asian |
| BAF | Black African |
| BAN | Bangladeshi |
| BBR | Black British |
| BCA | Black Afro‐Caribbean |
| BLO | Black other |
| CHI | Chinese |
| IND | Indian |
| JAP | Japanese |
| MO | Mixed Other |
| MOR | Moroccan |
| MRA | Mixed Race |
| MUS | Muslim/Islamic |
| NCA | No Category Assigned |
| NR | Not recorded |
| OAB | Other Asian Background |
| OBL | Other Black |
| OTH | Other |
| OWH | Other White |
| PAK | Pakistani |
| SLA | Sri Lankan |
| W | White |
| WA | White and Asian |
| WBA | White and Black African |
| WBC | White and Black Caribbean |
| WESW | White, English, Scottish, Welsh |
| WHO | White other |
| WIR | White Irish |
| WIT | White Italian |
| WPR | White Portuguese |
| WSP | White Spanish |
| WUK | White UK |
Footnotes
Competing interests: None.
References
- 1.Duke T, Mgone C S. Measles—not just another viral exanthem. Lancet 2003361763–773. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization HEALTH21: the health for all policy framework for the WHO European region. Copenhagen: WHO European Office, 1998
- 3.Communicable Disease Surveillance Centre MMR vaccine coverage falls in the United Kingdom. Commun Dis Rep Wkly 1999937. [PubMed] [Google Scholar]
- 4.Wakefield A J, Murch S H, Antony A.et al Ileal‐lymphoid‐nodular‐hyperplasia, non specific colitis, and pervasive developmental disorder in children. Lancet 1998351637–641. [DOI] [PubMed] [Google Scholar]
- 5.Roberts K, Dixon‐Woods, Fitzpatrick R.et al Factors affecting uptake of childhood immunisation: a Bayesian synthesis of qualitative and quantitative evidence. Lancet 20023601596–1599. [DOI] [PubMed] [Google Scholar]
- 6.Baker M R, Bandaranayake R, Schweiger M S. Differences in rate of uptake of immunisation among ethnic groups. BMJ 19842881075–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhopal R S, Samin A K. Immunisation uptake of Glasgow Asian children: paradoxical benefit of communication barriers? Community Med 199810215–220. [DOI] [PubMed] [Google Scholar]
- 8.Martineau A, White M, Bhopal R. No sex differences in immunisation rates of British South Asian children: the effect of migration. BMJ 1997314642–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheikh A, Gatrad A R. Children and young families. In: Kai J, ed. Ethnicity, health and primary care. Oxford: Oxford University Press, 2003151–159.
- 10.Middleton E, Baker D. Comparison of social distribution of immunisation with MMR, England, 1991–2001. BMJ 2003326854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan D L.Focus groups as qualitative research. Sage University paper series on qualitative research methods Beverly Hills, CA: Sage, 1988;16,
- 12.Strauss A L.The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine, 1967