Patients who are in pain, anxious or acutely disturbed are seen frequently in the accident and emergency department. Good personal management will do much to assist with their treatment, but many patients will require additional treatment with drugs. The word “sedation” is often used generically to encompass relief from both pain (analgesia) and anxiety, but it must be recognised that they are separate processes, even though many patients require both. The therapeutic goals of sedation are relief of anxiety, reduction in psychological stress, and amnesia for procedures or traumatic events. The therapeutic goal of analgesia is to provide relief (complete whenever possible) of pain due to injury or of a potentially painful procedure. It is usually necessary to treat with separate agents to achieve these goals, and it is important to understand the potentially synergistic effects of the drugs used.
All drugs that depress the central nervous system have the potential to produce cardiovascular or respiratory complications. Endoscopy has a reported morbidity rate of 1 in 200 and a mortality of 1 in 2000.1 These adverse events are closely linked to high doses of sedatives and lack of monitoring. An audit of bronchoscopy practice and sedation in the UK in 1997 found deficiencies in patient monitoring and staff training.2 A similar survey of sedation for transoesophageal echocardiography in November 2000 found that 29% of practitioners did not use oximetry, 4% did not even have an oxygen supply in the room and 74% had never received formal training in sedation.3
Although sedation in elective circumstances is clearly challenging, sedation in the emergency department may be further complicated because patients often present in less than ideal circumstances and with comorbidity. Such patients often require immediate interventions and therefore cannot always be thoroughly prepared. A complete medical assessment may not be available and preparation such as fasting may be compromised.
A report commissioned by the UK Academy of Medical Royal Colleges and Faculties4 restated the generally accepted principles of the use of analgesic and anxiolytic drugs. These apply to all settings including emergency departments. Clearly, emergency physicians are involved in providing sedation and analgesia for a group of patients in whom there may be considerable risk of an adverse event.
It is therefore important that staff receive adequate training in the safe practice of sedation. This paper describes a course that aims to provide such training for specialist registrars in emergency medicine, based in a high‐fidelity simulation (HFS) centre. We also present the results of a satisfaction survey completed by course participants.
Course development
A one‐day simulation course was designed by a panel of experienced emergency medicine practitioners in association with an expert in the discipline of sedation administration. The course uses a mixture of HFS (using the patient simulator) and low‐fidelity simulation (using actors as simulated patients, with whom the candidates interact but whose physiological profile is produced by the computer and can be manipulated by facilitators). HFS consists of a simulated resuscitation room with all necessary equipment, and a life size Meti HPS version D manikin (Medical Education Technologies Inc., Florida, USA) whose physiological signals are computer generated and displayed on standard monitors. The response is dynamic and dependent on how the candidate manages the patient. The performances are video recorded and used for review during the debriefing session that follows. This allows the candidate to observe his or her own performance.
Box 1 outlines the educational objectives that were initially defined.
Box 1 Six scenarios developed to deal with these learning objectives and piloted by the faculty so that each facilitator had the opportunity to experience them personally
Improved knowledge of drugs used for pain/anxiety relief in the emergency department
Safe patient preparation and adequate clinical assessment
Safe preparation of the environment/choice of equipment
Understanding of levels of monitoring for safe sedation
Safe practice in drug administration
Recognition and management of complications of sedation
Demonstration of assessment for safe patient discharge
Without describing specific scenario content, they cover the principles of sedation for a variety of clinical challenges that present to the emergency department, including simple manipulations, medical emergencies, the agitated patient and the complications of sedation.
Precourse material is made available to each candidate, outlining the pharmacological background of sedation so that a basic level of knowledge is assumed on starting the course. Before beginning the scenarios, an introductory presentation covers a variety of topics, including levels of sedation, preparation for sedation, drugs and aftercare.
The candidates are then given the opportunity to be team leader in one of the six scenarios, which are arranged in order of increasing complexity. Candidate numbers are limited to six so that each person has the opportunity to lead the team, which is made up of the remaining candidates. Two instructors and a staff member from the simulation centre observe and facilitate each scenario. Once the scenario is completed, debriefing begins, allowing reflection on all the events that have occurred. Facilitators review performances using the video recording, which allows candidates to see for themselves how the scenario developed. Although discussion around the topic can identify levels of knowledge in how to treat certain conditions, observing the behaviour in how the scenario is managed incorporates the importance of non‐technical skills required by emergency clinicians. Part of the debriefing is aimed at highlighting skills such as decision making, situational awareness, teamwork, prioritisation, communication and leadership.
Outcome
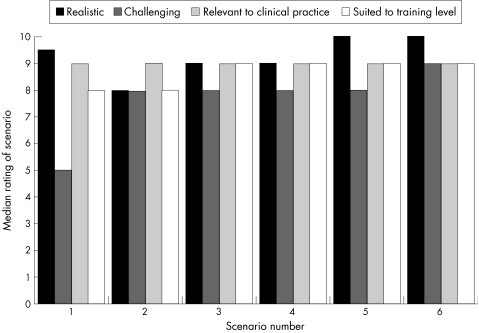
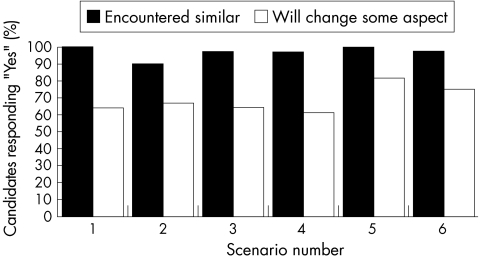
The course was first run in January 2003, and by September 2004, 36 participants from the senior health officer (SHO) III (middle grade SHO) level to fifth year specialist registrars from across Scotland had participated. All those attending have completed a questionnaire scoring aspects of the course and the content of the scenarios. Responses to the questionnaire have been positive. The results are shown in fig 1 and 2. Figure 1 summarises the ratings (scoring from 1 to 10) that participants gave each scenario. It reflects the increasing complexities and challenges of the scenarios as the course progresses. Realism and relevance were scored highly by all participants. Figure 2 shows the percentage of registrars who responded positively when asked whether they had encountered situations similar to the scenarios and whether they would now change some aspect of clinical practice.
Figure 1 Median scenario ratings (rated 1–10).
Figure 2 Percentage of trainees who had encountered similar problems and would change some aspect of their management.
Discussion
The UK Academy of Medical Royal Colleges and Faculties guidelines were published in response to concerns about the safety of sedation techniques by non‐anaesthetists. The authors emphasise the need to “incorporate the necessary instruction and assessment into training and revalidation programmes of those specialities that use sedation techniques”.4
Accident and emergency practitioners have previously shown proficiency in advanced airway techniques,5 but a survey of the knowledge of sedation guidelines and drugs published in 1994 produced disappointing results.6 Fifty doctors from SHO to senior registrar level, undertaking sedation procedures in two emergency departments, responded to the questionnaire. 54% were unable to name the antagonist to benzodiazepines, 6% could not name an opiate antagonist and 88% did not know the correct dose. Only one respondent used pulse oximetry during sedation procedures. None of those responding had received formal training in sedation techniques.
This course has been designed for specialist registrars in emergency medicine and deals with the problems of sedation in an emergency setting. The focus is on preparation, situational awareness, management and concepts of sedation techniques.
It has been shown that experience without feedback increases confidence but not skill.7 In the proceedings of Setting the Educational Agenda and Curriculum for Error Prevention in Emergency Medicine (2000),8 it was acknowledged that there are “extraordinary deficiencies in providing appropriate feedback” to emergency department personnel. HFS offers an environment in which the trainees can critically review their own performance and reflect on it during an in‐depth feedback session. HFS is recommended as a powerful educational technique, which allows the trainee a “way of gaining experience without experience”.8 There are limitations to simulators, in particular in relation to skin colour and general appearance of the unwell patient, but generally candidates overcome this by gauging the severity of illness through the physiology displayed on the monitors. Although the course could be adapted to use lower level simulators, the HFS offers some advantages by allowing greater flexibility to run complex scenarios with minimal intervention from the instructors. The setting of the simulated resuscitation room and the input of dedicated staff in the simulation centre also help to create realistic scenarios, tailored to the responses and interventions of individual candidates. The debriefing session offers the opportunity for discussion between candidates and facilitators about the scenario, the reasons for decisions made during the scenario and probing of the candidates' depth of knowledge about the clinical problem. Although it is difficult to quantify the effect of simulation training over and above traditional teaching methods, it has been shown that simulation can be used to observe and quantify the technical performance of anaesthetic trainees.9
The results shown here are based on subjective feedback from course participants and show high levels of satisfaction with the course among trainees. A striking finding is that there was intent to change practice in 61–81% of the participants across the scenarios, despite having experienced a scenario before and regardless of the fact that some very experienced trainees participated.
It may be expected that if they had previously encountered a scenario, then there would be little to learn. The results clearly indicated that this was not the case with all the participants, indicating that they would change some elements of their clinical practice after at least one of the scenarios. Apparently, the course allows participants to reflect on a clinical scenario in a way different from that seen in day‐to‐day clinical work. This shows the advantage of an environment that is confidential, where issues can be discussed frankly with experienced colleagues to effect a change in practice. The course is aimed at first‐year specialist registrars (SpRs), but clearly has a wider application. Feedback was from emergency medicine trainees with a range of experience from SHO3 level to SpR5, and has shown the course to be just as relevant to more experienced trainees. It is likely to be valuable to other specialists who carry out sedation on a regular basis. In addition, there is potential to develop the course to include professionals from other disciplines who are also exposed to the management of such patients.
However, this excellence in teaching and learning experiences comes at a high cost—that is, a minimum of two specialists in emergency medicine or anaesthesia are required to teach it in addition to a basic cost of approximately £800/day to run and maintain the simulator.
The course now runs as part of several simulator‐based courses in the essential curriculum for SpRs in Scotland. Clinicians interested in taking part in the course can contact the Simulation Centre in the Stirling Royal Infirmary, UK. It is hoped that registrars participating in this course will develop on the skills they have learned, thus ensuring that Academy guidelines are followed in departments throughout Scotland.
Abbreviations
HFS - high‐fidelity simulation
SHO - senior health officer
SpR - specialist registrar
Footnotes
Competing interests: None declared.
References
- 1.Quine M A, Bell G D, McCloy R F.et al Prospective audit of upper gastrointestinal endoscopy in two regions of England: safety, staffing and sedation methods. Gut 199536462–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Honeybourne D, Neumann C S. An audit of bronchoscopy practice in the United Kingdom: a survey of adherence to national guidelines. Thorax 199752709–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sutaria N, Northridge D, Denvir M. A survey of sedation and monitoring practice in the UK: are recommended guidelines being followed? Heart 200084(Suppl II)ii19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Academy of Medical Royal Colleges Implementing and ensuring safe sedation practice for healthcare procedures in adults. Report of an intercollegiate working party chaired by the Royal College of Anaesthetists. London, 2001. http://www.aomrc.org.uk or www.rcoa.ac.uk (accessed 21 Jul 2006)
- 5.Graham C A, Beard D, Oglesby A J.et al Rapid sequence intubation in Scottish urban emergency departments. Emerg Med J 2003203–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hewitt S M, Hartley R H. Manipulation under sedation in the accident and emergency department. J Accid Emerg Med 199411186–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marteau T M, Wynne G, Kaye W.et al Resuscitation: experience without feedback increases confidence but not skill. BMJ 1990300849–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Croskerry P, Wears R L, Binder L S. Setting the Educational Agenda and Curriculum for Error Prevention in Emergency Medicine–proceedings. Acad Emerg Med 200071194–1200. [DOI] [PubMed] [Google Scholar]
- 9.Forrest F C, Taylor M A, Postlethwaite K.et al Use of high‐fidelity simulator to develop testing of the technical performance of novice anaesthetists. Br J Aanesth 200288338–344. [DOI] [PubMed] [Google Scholar]