Abstract
Tourniquets are an effective means of arresting life‐threatening external haemorrhage from limb injury. Their use has not previously been accepted practice for pre‐hospital civilian trauma care because of significant concerns regarding the potential complications. However, in a few rare situations tourniquet application will be necessary and life‐saving. This review explores the potential problems and mistrust of tourniquet use; explains the reasons why civilian pre‐hospital tourniquet use may be necessary; defines the clear indications for tourniquet use in external haemorrhage control; and provides practical information on tourniquet application and removal. Practitioners need to familiarise themselves with commercial pre‐hospital tourniquets and be prepared to use one without irrational fear of complications in the appropriate cases.
Tourniquets are an effective means of arresting life‐threatening external haemorrhage from limb injury. However, their use remains a subject of much debate, with many unanswered questions and significant concerns regarding the potential complications from their use.1 For these reasons tourniquets are often discouraged in contemporary pre‐hospital civilian trauma care.
The first reported use of a tourniquet for haemorrhage control after wounding was by a French army surgeon called Etienne Morel in 1674. The term tourniquet originated from the French “tourner” meaning “to turn”. Before this, tight bandages proximal to wounds were being used by surgeons as an aid to amputation as early as 1517.2
In 1874 Lister described the use of a tourniquet in elective civilian practice to obtain a bloodless field during the excision of a tuberculous wrist joint.2 Indeed the majority of knowledge today regarding tourniquet use comes from elective theatre cases for orthopaedic or vascular surgery.
By 1916 the complications of tourniquet use were being identified and the Royal Army Medical Corp Journal stated “we are inclined to think that tourniquets are an invention of the Evil One”.3 However, recent military data have estimated that 10% of all battlefield deaths are caused by extremity haemorrhage (accounting for 60% of preventable deaths)4 and analysis of data from the Vietnam war found that 7% of combat deaths may have been prevented by the use of a limb tourniquet.5 In a 4 year period of tourniquet use by the Israeli Defence Force there were no reported deaths from uncontrolled limb haemorrhage among 550 injured patients.6
Even in civilian traditional teaching, Advanced Trauma Life Support (ATLS) recommends that in the presence of major arterial haemorrhage “the judicious use of a pneumatic tourniquet may be helpful and lifesaving”.7
This article aims to:
explore the potential problems and mistrust of tourniquet use
offer reasons why civilian pre‐hospital tourniquet use may be necessary
define the clear indications for tourniquet use in external haemorrhage control
provide practical information on tourniquet application and removal.
SEARCH STRATEGY
Ovid Medline (R) 1966 to August Week 1 2006 using terms exp Tourniquets/AND [exp Hemorrhage/OR haemorrhage.mp OR bleeding.mp OR exsanguination.mp] AND limit to (Humans and English language). PubMed using the mesh terms “Tourniquets” AND “Hemorrhage”. The Cochrane Database of Systematic Reviews 2006 Issue 3 using term “Tourniquets” found no relevant articles.
PROBLEMS WITH TOURNIQUET USE
It is likely that the use of tourniquets for external haemorrhage control may have fallen out of vogue for the following reasons:
The majority of external haemorrhage can be controlled by direct pressure.
Previously tourniquets have been used inappropriately when not clinically indicated—for example, for all gunshot wounds of the limbs—so the risks have outweighed the benefits. In a recent paper of military tourniquet use 47% of 110 tourniquet applications were not clinically indicated.6
Preventing arterial blood flow to a limb will result in ischaemia. Continuous application for longer than 2 h can result in permanent nerve injury, muscle injury (including contractures, rhabdomyolysis and compartment syndrome), vascular injury and skin necrosis.8 Muscle damage is nearly complete by 6 hours, with likely required amputation. Numerous studies have been performed to determine the maximum duration of tourniquet use before complications. The general conclusion is that a tourniquet can be left in place for 2 h with little risk of permanent ischaemic injury. However, the majority of the literature looks at pneumatic tourniquets in elective theatre cases with normovolaemic patients. In hypovolaemic trauma patients with non‐pneumatic tourniquets these figures may not be applicable. There is very little data on the complication rate of clinically indicated pre‐hospital tourniquet application and therefore there is no safe tourniquet time. Lakstein identified that 5.5% of 110 pre‐hospital tourniquet applications resulted in neurological complications, with an ischaemic time between 109–187 min. None of these resulted in limb loss. The mean ischaemic time for use of a tourniquet with no complications was 78 minutes.6
Reperfusion injury may also result from tourniquet use. Reperfusion of hypoperfused tissues causes inflammation‐induced damage of local areas, and inflammatory mediators may systemically affect the vital organs. The reperfusion damage may occur after 60 min of local low flow.9
An incorrectly applied tourniquet will actually cause increased bleeding from distal soft tissue injuries and damaged arteries if there is occlusion of the lower pressure venous outflow, but inadequate occlusion of arterial blood flow.10
In instances where a tourniquet has been applied to a hypotensive patient before resuscitation, haemorrhage may stop. However, when the patient is resuscitated to a higher systolic blood pressure the bleeding may restart despite the continued use of a tourniquet. This problem can be avoided by adhering to principles of hypotensive resuscitation for non‐compressible haemorrhage11 and by tightening the tourniquet until control is re‐achieved.10
A policy of periodic loosening of a tourniquet in an attempt to reduce limb ischaemia has often led to incremental exsanguination and death.12
Historically the effectiveness and complication profile of different types of tourniquet was never tested before operational use. Tourniquets were often improvised, whereas commercial devices that have undergone clinical trials are in contemporary US and UK military use.12
A properly applied tourniquet is painful and this has experientially led to inadequate tightening or inappropriate pre‐hospital removal. The patient will require strong analgesia (for example, opiate or ketamine intravenously) after stabilisation of vital signs.
PRESENT DAY USE
The military have been at the forefront of reintroducing tourniquet use into modern practice. The new military trauma paradigm teaches that control of catastrophic haemorrhage takes priority over airway and breathing assessment.13 Effective modern combat body armour means that extremity trauma now accounts for the highest anatomical distribution of injury. In the combat setting high velocity penetrating trauma and blast injury are common, resulting in extensive wounding and mangled extremities.14 Soldiers require a rapid system of haemorrhage control which can be self applied while under fire. The requirement for continued use of a tourniquet is then reassessed when the fire‐fight is won.
In contrast in civilian practice the medical practitioner is generally working in a safe environment (not “under fire”) with early access to definitive care; furthermore, the common mechanisms of non‐battle injury do not normally produce catastrophic external haemorrhage.
However, there are a number of examples where tourniquet use may be applicable in civilian practice:
Penetrating trauma from firearms and stabbings. Home Office figures (England and Wales) show a 16% increase in firearms offences resulting in serious injury in 2005/06 compared to 2004/05.15
Firearms police officers working in tactical environments who may benefit from a self‐applied tourniquet for “care under fire”.
Terrorist incidents with penetrating and/or blast injury to limbs.
Rural incidents or wilderness medicine where there are limited resources and delayed, often unconventional, transport to definitive care.
Industrial accidents. From personal communication there are a number of examples of tourniquet use to prevent haemorrhage from limbs following entrapment or shredding by industrial or farming machinery (http://www.marsbasics.co.uk/)
INDICATIONS FOR USE
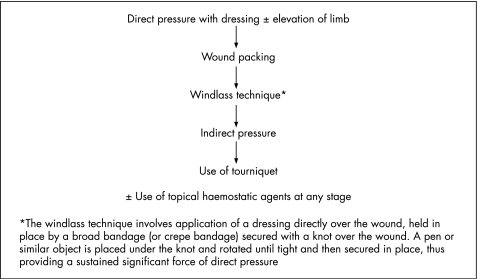
Indications for tourniquet use will be rare in the civilian pre‐hospital environment. In the majority of cases external haemorrhage will be controlled by applying a stepwise approach (fig 1).
Figure 1 Stepwise approach to haemorrhage control.
However, immediate application of a tourniquet may be justifiable in the following examples:
Extreme life‐threatening limb haemorrhage, or limb amputation/mangled limb with multiple bleeding points, to allow immediate management of airway and breathing problems. (Following treatment of any airway or breathing problems the need for a tourniquet can be reassessed in the circulatory assessment and may be converted to a simple method of haemorrhage control.)
or
Life threatening limb haemorrhage not controlled by simple methods.
or
Point of significant haemorrhage from limb is not peripherally accessible due to entrapment (and therefore it is not possible to initiate simple methods of haemorrhage control such as direct pressure).
or
Major incident or multiple casualties with extremity haemorrhage and lack of resources to maintain simple methods of haemorrhage control.
and
Benefits of preventing death from hypovolaemic shock by cessation of ongoing external haemorrhage are greater than the risk of limb damage or loss from ischaemia caused by tourniquet use.
PRINCIPLES OF TOURNIQUET APPLICATION
The pre‐hospital practitioner should be familiar with a particular commercial tourniquet that has been proven in studies to be effective, rather than using an improvised device that has been demonstrated to take more time to apply or may lead to an increased risk of complications.16,17,18
With a wide availability of commercial tourniquets there have been several experimental studies using human volunteers comparing different types.16,17,18,19 User characteristics such as ease of self‐application under fire are largely inapplicable in the civilian pre‐hospital setting (the exception being tactical firearms police).
However, the physical characteristics of a tourniquet are relevant. The tourniquet must completely and consistently occlude arterial blood flow. The pressure required to occlude blood flow in a limb increases exponentially with the circumference of the limb. For this reason significantly more tension is required to occlude the arterial blood supply of a leg compared to an arm.
There is also an inverse relationship between tourniquet width and the minimal pressure required to occlude arterial blood flow. However, as width increases the amount of tissue that must be compressed increases, requiring an increased effort to produce tension. Also, as the width of the strap increases, the strap tends to bow, transmitting relatively more pressure to the centre rather than the edges and therefore reducing functional width.20
The UK Defence Medical Services selected the Combat Application Tourniquet (CAT, North American Rescue Products, Inc, USA) for operational use after experimental studies showed 100% effectiveness in occluding distal arterial flow using human volunteers.16Figure 2 shows the CAT tourniquet applied to the lower limb.
Figure 2 The Combat Application Tourniquet applied to the lower limb.
Principles of tourniquet application include: placement of the tourniquet as distal as possible, but at least 5 cm proximal to injury; sparing joints as much as possible; and ideally applied directly onto exposed skin to avoid slipping.6
Effectiveness of tourniquet use will be determined by cessation of external haemorrhage and not by the presence or absence of a distal pulse. If it is ineffective the tourniquet should be tightened or repositioned. If the tourniquet is still ineffective (unlikely) the health care provider may consider a second tourniquet placed just proximal to the first. Slight oozing may still occur in a limb amputation despite effective application if there is medullary bone blood flow.20
The time of application should be recorded and handed over to the receiving emergency department staff.
The practice of exposing the limb to cold environmental temperatures was credited for successful limb salvages after prolonged tourniquet applications (>8 h) in the second world war.21 Local hypothermia has been studied experimentally and suggested as a method to prolong tourniquet times before muscle ischaemia in elective models of tourniquet use in limb surgery.22 In animal studies on rats reducing the limb temperature to 4°C by application of cold gel packs was found to protect against tourniquet neuropathy after 3 h of tourniquet use.23 In animal studies on pigs, in the group with skin temperatures reduced to a mean of 9.3°C and muscle temperatures reduced to a mean of 16°C, after 3 h tourniquet application, a reduction in muscle damage was found in the local hypothermia group.24 Exposing the limb with a tourniquet to the environment to allow cooling or artificially trying to achieve local hypothermia may therefore be a consideration in situations with prolonged evacuation times to definitive care.
REMOVAL OF THE TOURNIQUET
Assuming that the tourniquet has been applied for the correct indications a decision will need to be made regarding its continued use. This will depend on several factors including: whether the external haemorrhage is from an isolated injury; if the other injuries have been stabilised; the current haemodynamic status of the patient; estimated journey time to hospital; and the medical resources available. If transit time is expected to be <1 h, the tourniquet should remain in situ until the patient is in the operating theatre where direct surgical control of haemorrhage can be undertaken.
If the transit time is >1 h and if there is an isolated injury (or the other life‐threatening injuries have been managed adequately) and the patient has stable vital signs, a “trial of tourniquet conversion” may be attempted. It is possible that after a period of time of reduced arterial flow from tourniquet use, clotting will have occurred sufficiently to arrest haemorrhage, allowing simpler methods to be effective and reducing the complications from continued tourniquet use. Before release of the tourniquet the practitioner should have secured wound packing (including haemostatic agents) and application of direct pressure over the bleeding point (with windlass dressing). If careful release of the tourniquet then results in a return of uncontrollable external haemorrhage, the tourniquet should be replaced and not removed until the patient is in the operating theatre (a “tourniquet of last resort”).
TRANSPORT AND HANDOVER
The practitioner should select the most appropriate hospital for the patient and relay an alert message to the emergency department to facilitate expeditious transfer to the operating theatre if necessary. Remember to give the time of tourniquet application in handover and remind the emergency department that it is present, particularly in patients with multiple injuries. Hospital staff should be strongly discouraged from removing the tourniquet until the patient is in theatre.
Any amputated limb should ideally be transported with the patient to hospital even if it appears unsalvageable as tissue may be utilised for skin cover and reconstruction of the stump (this will rarely be practical or appropriate in the military setting).
CONCLUSION
In rare situations tourniquet application will be necessary and lifesaving in the civilian pre‐hospital setting. Tourniquets are no longer only considered as a “last resort” device. Practitioners should familiarise themselves with this simple piece of equipment and be prepared to use it in appropriate cases without an irrational fear of complications.
Footnotes
Competing interests: None declared
References
- 1.Navein J, Coupland R, Dunn R. The tourniquet controversy. J Trauma 200354(5 Suppl)S219–S220. [DOI] [PubMed] [Google Scholar]
- 2.Mabry R L. Tourniquet use on the battlefield. Mil Med 2006171352–356. [DOI] [PubMed] [Google Scholar]
- 3.Blackwood M. Treatment of wounds from fire trench to field ambulance 1916. J R Army Med Corp 2001147230–235. [PubMed] [Google Scholar]
- 4.Champion H R, Bellamy R F, Roberts P.et al A profile of combat injury. J Trauma 200354S13–S19. [DOI] [PubMed] [Google Scholar]
- 5.Bellamy R F. Combat trauma overview. In: Zajtchuk R, Grande CM, eds. Textbook of military medicine part IV: surgical combat casualty care. Office of the Surgeon General, US Army 2005
- 6.Lakstein D, Blumenfield A, Sokolov T.et al Tourniquets for hemorrhage control on the battlefield: a 4 year accumulated experience. J Trauma 200354(5 Suppl)S221–S225. [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons Advanced trauma life support, 7th ed. Location: American College of Surgeons, Chicago, USA, 2004
- 8.Wakai A, Winter D C, Street J T.et al Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg 20019345–351. [DOI] [PubMed] [Google Scholar]
- 9.Husum H, Gilbert M, Wisborg T.et al Prehospital tourniquets: there should be no controversy [comment]. J Trauma 200456214–215. [DOI] [PubMed] [Google Scholar]
- 10.Starnes B W, Beekley A C, Sebesta J A.et al Extremity vascular injuries on the battlefield: tips for surgeons deploying to war. J Trauma 200660432–442. [DOI] [PubMed] [Google Scholar]
- 11.Revell M, Porter K, Greaves I. Fluid Resuscitation in prehospital trauma care: a consensus view. Emerg Med J 200219494–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clifford C C. Treating traumatic bleeding in a combat setting. Mil Med 2004169(12 Suppl)8–10. [DOI] [PubMed] [Google Scholar]
- 13.Hodgetts T J, Mahoney P F, Russell M Q.et al ABC to <C>ABC: redefining the military trauma paradigm. EMJ 200623745–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hodgetts T, Mahoney P, Evans G.et alBattlefield advanced trauma life support, 3rd ed. Location: Defence Medical Education and Training Agency, Joint Service Publication 570, 2006
- 15.Walker A, Kershaw C, Nicholas S.Home Office Statistical Bulletin. Crime in England and Wales 2005/06. London: Home Office, July, 2006
- 16.King R B, Filips D, Blitz S.et al Evaluation of a possible tourniquet system for use in the Canadian Forces. J Trauma 2006601061–1071. [DOI] [PubMed] [Google Scholar]
- 17.Wencke J C, Walters T J, Greydanus D J.et al Physiological evaluation of the U.S. Army one‐handed tourniquet. Mil Med 2005170776–781. [DOI] [PubMed] [Google Scholar]
- 18.Calkins D, Snow C, Costello M.et al Evaluation of possible battlefield tourniquet systems for the far‐forward setting. Mil Med 2000165379–384. [PubMed] [Google Scholar]
- 19.Walters T J, Wenke J C, Kauvar D S.et al Effectiveness of self‐applied tourniquets in human volunteers. Prehosp Emerg Care 20059416–422. [DOI] [PubMed] [Google Scholar]
- 20.Walters T J, Mabry R L. Issues related to use of tourniquets on the battlefield. Mil Med 2005170770–775. [DOI] [PubMed] [Google Scholar]
- 21.Wolff L, Adkins T. Tourniquet problems in war injuries. Bull US Army Med Dep 19458777–84. [Google Scholar]
- 22.Swanson A B, Livengood L C, Sattel A B. Local hypothermia to prolong safe tourniquet time. Clin Orthop Relat Res 1991264200–208. [PubMed] [Google Scholar]
- 23.Kelly C, Creagh T, Grace P A.et al Regional hypothermia protects against tourniquet neuropathy. Eur J Vasc Surg 19926288–292. [DOI] [PubMed] [Google Scholar]
- 24.Irving G A, Noakes T D. The protective role of local hypothermia in tourniquet‐induced ischaemia of muscle. J Bone Jt Surg 198567297–301. [DOI] [PubMed] [Google Scholar]