Abstract
Background
The use of the prehospital electrocardiogram (ECG) to identify patients with ST‐segment elevation myocardial infarction (STEMI), coupled with a centralised system to alert the cardiac catheterisation team in preparation for prompt intervention, has been shown to reduce door‐to‐balloon times (DBT) effectively. A confounding variable in prolonging the recommended 90 min DBT is the time of day or day of the week of patient presentation. We postulated that use of the prehospital ECG, coupled with an emergency department initiated “Cath Alert” system, could neutralise DBT delays related to time of day or day of week.
Methods
A prospective study was conducted on 167 consecutive patients presenting to our emergency department with acute STEMI. All patients were treated with primary percutaneous coronary intervention. Patients were grouped according to time of presentation: during regular hours (Monday to Friday 08:00 to 17:00) vs off hours (after 17:00 on weekdays and all hours on weekends). Baseline recorded variables included mode of presentation, transmission of prehospital ECG, and activation of Cath Alert system.
Results
Overall, the mean (SD) DBT was 69 (35) mins, with the majority of patients (n = 131, 78%) achieving the recommended DBT of 90 mins. The shortest DBT occurred in patients who arrived by emergency medical services with use of the prehospital ECG and Cath Alert system (53 (21) min), while those who arrived as a walk‐in without use of emergency medical services had the longest DBT (105 (38) min; p<0.001). Compared to regular hours, presentation during off hours prolonged DBT in patients presenting via emergency medical services (75 (16) vs 53 (18) min, p = 0.03). With transmission of the prehospital ECG, the delay in DBT was improved among those presenting off hours, nullifying the adverse effect of off hour presentation (54 (21) vs 49 (22) min; p = 0.26).
Conclusion
Variables such as time of day and mode of presentation have an impact on achieving currently recommended DBT in patients with STEMI. With the addition of each prehospital variable in succession—that is, arrival by emergency medical services, Cath Alert system, and the prehospital ECG—the DBT can be progressively shortened and the adverse “off hour effect” nullified.
Cardiovascular disease is a source of significant mortality, causing up to one third of all deaths in the United States. Coronary heart disease accounts for one in five deaths, with the incidence of ST segment elevation myocardial infarction (STEMI) representing 30–45% of all acute coronary syndromes.1 The importance of prompt treatment of STEMI has been highlighted in many studies both to preserve cardiac function and reduce mortality.2,3 It is estimated that every 30 min of delay in reperfusion therapy increases 1 year mortality by 7.5%.4 Prior trials have shown that primary percutaneous coronary intervention (PCI) remains superior to fibrinolytic treatment and is the preferred mode of reperfusion in acute STEMI.5,6
The American College of Cardiology/American Heart Association (ACC/AHA) has provided guidelines for the diagnosis and management of STEMI. Despite their recommendations for the management of patients with STEMI that PCI should be performed within 90 min of presentation, less than half of patients receive reperfusion therapy within this time period.7,8 This has led to various strategies to improve the hospital door‐to‐balloon time (DBT) in patients receiving primary PCI. The use of the prehospital electrocardiogram (ECG) to identify patients with STEMI, coupled with a centralised system to alert the cardiac catheterisation team in preparation for prompt intervention, has been shown to reduce DBT effectively when adopted by hospitals and emergency medical services personnel.9,10 The ACC/AHA thus recommends that advanced cardiac life support providers perform and evaluate 12 lead ECG routinely on chest pain patients suspected of STEMI.7
A confounding variable in meeting the ACC/AHA guidelines on DBT is the time of day or day of the week of patient presentation. A cohort study using the National Registry of Myocardial Infarction database demonstrated a difference of 21.3 min in meeting DBT between patients presenting during regular hours compared to off hours.11 We hypothesised that use of the prehospital ECG coupled with a centralised emergency department initiated “Cath Alert” hospital system could neutralise DBT delays related to time of day or day of the week. To test our hypothesis, we prospectively analysed our acute STEMI protocol, and examined the effect of off‐hours presentation on DBT. The acute STEMI protocol consists of a prehospital 12 lead ECG identifying ST segment elevation, transmission of ECG while the patient is en route to a receiving station in the emergency department, and a centralised single‐page notification of the cardiac catheterisation team (Cath Alert) initiated by the emergency department physician.
Methods
This study was undertaken at Cleveland Clinic Florida, a primary receiving hospital serving a large suburban community. Primary PCI is the preferred method of reperfusion and is performed on all eligible patients presenting with acute STEMI. The hospital has a 24 h on‐call cardiac catheterisation team comprising an interventional cardiologist, a cardiology fellow, specialised nurses, and transport personnel. The cardiac catheterisation laboratory is located in the same building as the emergency department. Two coronary angiography suites are available simultaneously.
Study population
From October 2001 to November 2004, 167 consecutive patients presented to the emergency department with an acute STEMI and were eligible for primary PCI. Patients excluded from the study were inter‐hospital transfers and patients with prior fibrinolytic treatment. The emergency medical services personnel involved were trained in the identification of ECG criteria for STEMI (>1 mm ST elevation in two contiguous leads or two adjacent limb leads). Upon arrival at the patient's location by emergency medical services, a 12 lead ECG was obtained if the history suggested an acute coronary syndrome. If the ECG is indicative of STEMI, it is immediately transmitted electronically to a LifeNet receiving station (Medtronic, Inc, Minneapolis, Minnesota, USA) in the emergency department. The emergency department physician then evaluates the ECG and corroborates the analysis from the field. The emergency department physician, using a centralised single‐page system (Cath Alert), directly contacts all cardiac catheterisation team members, activating the cardiac catheterisation laboratory.
Data collection and mode of presentation
Patient demographic and clinical information were collected upon arrival to the emergency department. Clinical data recorded included the following: date and time (hour and minute) of presentation; availability of prehospital 12 lead ECG; location of STEMI (anterior, non‐anterior); and ejection fraction (determined by two‐dimensional echocardiography or angiography). Patients arrived at the emergency department via emergency medical services or as a walk‐in. Of those who arrived via emergency medical services, there were three modes of presentation, which were independently identified for DBT measures: emergency medical services only; emergency medical services activated Cath Alert system; and emergency medical services activated Cath Alert system with prehospital 12 lead ECG. The time from arrival in the emergency department to first inflation of balloon PCI was measured in all patients. Patients were stratified based on their mode of presentation and time of presentation. Time of presentation was defined as regular hours described as between 08:00 to 17:00 weekdays, and off‐hours between 17:00 to 08:00 on weekdays and all hours on weekend days. We assessed the number of patients who met the ACC/AHA recommended guidelines for DBT for PCI (within 90 min).
This study was done with the approval of the Institutional Review Board and ethics committee from our centre. Continuous variables were compared using the Student t test and nominal variables by using the χ2 and Fisher's exact test. Values of p⩽0.05 were considered significant.
Results
During the study period, a total of 167 patients presented to the emergency department with acute STEMI and met our inclusion criteria. Baseline characteristics are shown in table 1. Overall, the mean (SD) DBT was 69 (35) min, with 78% (n = 131/167) of the cohort achieving the recommend DBT of <90 min. The majority of patients (n = 123, 74%) were brought via emergency medical services, while the remaining (n = 44, 26%) were walk‐ins to the emergency department. Of those presenting via emergency medical services, 81% (n = 100) had a prehospital 12 lead ECG and a Cath Alert system activated; 15% (n = 18) had no prehospital ECG but activated a Cath Alert system; 4% (n = 5) had neither a prehospital ECG nor a Cath Alert system activated.
Table 1 Baseline patient characteristics and mode of presentation.
| Overall cohort (n = 167) | Regular hours (n = 116) | Off hours (n = 51) | |
|---|---|---|---|
| Demographics | |||
| Mean (SD) age (years) | 61 (13) | 63 (12) | 60 (13) |
| Male gender (%) | 86 | 84 | 87 |
| Anterior infarct location (%) | 40 | 37 | 41 |
| Mean (SD) ejection fraction (%) | 50 (9) | 51 (6) | 50 (10) |
| Mode of presentation (n) | |||
| Prehospital ECG, Cath Alert | 100 | 30 | 70 |
| Cath Alert only | 18 | 6 | 12 |
| EMS, no Cath Alert | 5 | 1 | 4 |
| Walk‐ins | 44 | 14 | 30 |
ECG, electrocardiogram; EMS, emergency medical services.
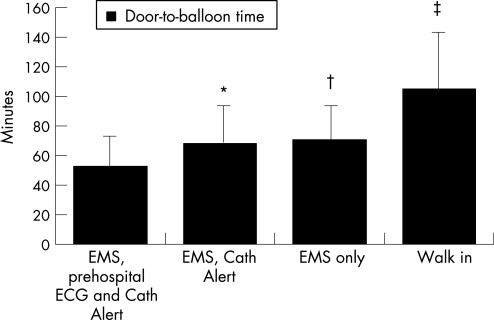
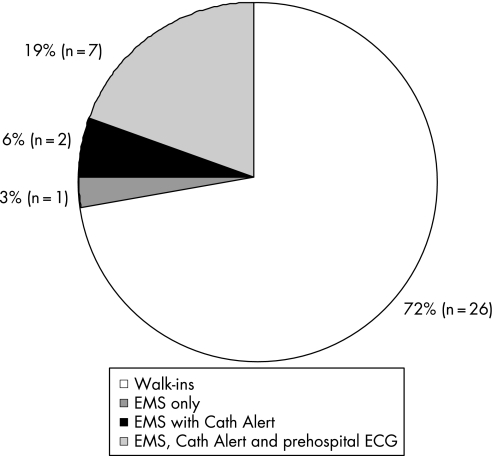
Patient DBT based on mode of presentation are shown in fig 1. Patients who arrived to the emergency department as a walk‐in had a significantly longer DBT compared to those presenting via emergency medical services (mean (SD) 105 (38) vs 56 (22) min; p<0.001). Among those presenting via emergency medical services, the shortest DBT were achieved in patients who transmitted the prehospital ECG and activated the Cath Alert system, followed by those who presented in the same manner but without the prehospital ECG (53 (21) vs 68 (20) min; p = 0.007). Of the 22% of patients (n = 36) who failed to achieve the recommended 90 min DBT, the majority presented as a walk‐in to the emergency department (fig 2).
Figure 1 Mean (SD) door‐to‐balloon times shown based on mode of presentation. *p = 0.007 for prehospital electrocardiogram (ECG) and Cath Alert vs Cath Alert without prehospital ECG; †p = 0.06 for prehospital ECG and Cath Alert vs emergency medical services (EMS) only; ‡p<0.001 for prehospital ECG and Cath Alert vs walk in.
Figure 2 Patients who failed to meet the recommended 90 min door‐to‐balloon time based on mode of presentation. ECG, electrocardiogram; EMS, emergency medical services.
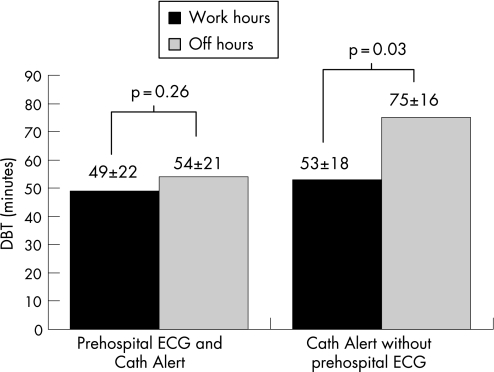
Testing our main hypothesis, patients were grouped according to time of presentation, regular versus off hours. The majority of patients (n = 116, 69%) presented to the emergency department during off hours compared to 31% (n = 51) presenting during regular hours. Overall there was no significant difference in DBT among patients arriving during regular hours versus off hours (69 (42) vs 69 (31); p = 0.98). Based on mode of presentation, the longest DBT were noted for the walk‐in patients during regular hours (118 (44) min). Among those who presented during off hours, the prehospital ECG and Cath Alert system led to a shorter DBT compared to Cath Alert alone patients (54 (21) vs 75 (16); p<0.001) and to walk‐ins (54 (21) vs 99 (33); p<0.001). Although DBT were greater during off hours versus regular hours in those who arrived via emergency medical services with Cath Alert activation, the use of the prehospital ECG along with Cath Alert negated the effect of off hour presentation and significantly shortened the DBT (fig 3). In both groups, the addition of the prehospital ECG to the Cath Alert reduced DBT by an average of 4 min during regular hours and 21 min during off hours.
Figure 3 Mean (SD) door‐to‐balloon times (DBT) during regular hours versus off hours for those who arrived via emergency medical services with Cath Alert activation only compared to those with the prehospital electrocardiogram (ECG) along with Cath Alert activation. The addition of the prehospital ECG negated the delay effect of off hour presentation and significantly reduced the DBT.
Discussion
In this cohort of acute STEMI patients undergoing primary PCI, the use of the prehospital ECG and a Cath Alert system led to the shortest DBT (53 (21) min). This benefit was evident for patients presenting both during regular hours and off hours. Less than a quarter of the cohort failed to meet the recommended 90 min DBT, and of those nearly 75% failed to use emergency medical services. These observations support the practice of the prehospital ECG and its transmission coupled with an emergency department initiated Cath Alert system.
Longer DBT have been associated with increased in‐hospital mortality regardless of time of symptom onset or presence of high risk factors.12 To this end, studies have identified strategies that are associated with improved outcomes in achieving better DBT. An integrated multidisciplinary approach including the use of the prehospital ECG transmitted by emergency medical services to the emergency department physician, and centralised activation of the cardiac catheterisation team, has been identified in top performing hospitals as a tool for meeting ACC/AHA guidelines.9,13 Data from the National Registry of Myocardial Infarction showed substantial variation in DBT among hospitals. However, in subinterval analysis of times that constitute DBT, the greatest delay was noted in ECG‐to‐catheterisation lab time across all hospital groups. This comprises the time from performance of the ECG to arrival at the catheterisation laboratory, and includes the time to diagnoses of STEMI, making the decision to treat, and preparation for PCI. This delay was noted on average to be almost 50 min.14 Thus, the potential for considerable improvement remains in the sequential hospital processes within this area.
Prehospital ECG in earlier studies has been shown to shorten DBT significantly in patients with STEMI.15 The application and interpretation of these prehospital ECGs by trained emergency medical services personnel in the field has been found to be accurate and comparable to the emergency department physician's interpretation.16 The ECG, once obtained, can then set off the cascade of events involved in the management of STEMI. In our study the addition of the prehospital ECG to other variables resulted in a statistically significant drop in DBT in all groups of patients. It has, however, been shown that it is not the mere performance of the prehospital ECG but its transmission and use to activate a Cath Alert that has an impact on DBT.9 This approach in our hospital shortened DBT for patients up to 50%, regardless of mode or time of presentation. In an integrated approach, the involvement of the emergency department physician in initiating a decision for primary PCI has also been shown to reduce outcome measures including DBT, subsequent hospital interventions and length of stay.17
The mode of presentation to the emergency department also affects time to reperfusion in patients with STEMI. Faster DBT have been achieved in patients who present to the emergency department via emergency medical services versus self‐transport.18 Our data showed that the longest DBT was indeed in patients who presented to the emergency department as walk‐ins. A prolongation in all subinterval times, especially in triage and obtaining the ECG, is a likely explanation for this delay. Interestingly, in our hospital, patients who presented during off hours as walk‐ins had a shorter DBT compared to those presenting during regular hours. This may be explained based on the lower patient volume during off hours enabling a more rapid patient triage.
Our data did not monitor the time from Cath Alert activation to transfer to the catheterisation lab, which would have shed light on the response time of the catheterisation team. A response time of 20 min after activation of the Cath Alert has been proposed as ideal by Bradley et al to shorten DBT.9 The subinterval time from ECG completion to catheterisation lab arrival was shown to be longer during off hours in a prior study.11 That was attributed to a longer catheterisation lab activation time, a subinterval that also includes the diagnosis of the STEMI. In our study, patients with Cath Alert activation in the absence of the prehospital ECG during off hours had an average DBT 22 min longer compared to those presenting during regular hours. This delay was eliminated with the use of the prehospital ECG and thus negated the “off hour effect” on DBT delays (fig 3).
Though our study was not powered to evaluate mortality, in‐hospital mortality has been shown to be higher in patients who presented during off‐hours. Centres that perform a high volume of primary PCI for STEMI (>50 per year) have been identified as having improved DBT, as have hospitals that consistently use one reperfusion strategy (>90% of the time).8 Attainment of these benchmarks may help explain how >75% of our cohort achieved the recommended 90 min DBT.
Conclusion
The steps to primary PCI for acute STEMI are complex and interspersed with several processes and factors. These multiple steps have the potential to be shortened so as to become as efficient as possible. Strategies have been identified to reduce DBT effectively. This study highlights the effects that variables such as time of day and mode of presentation can have in patients with STEMI in achieving currently recommended DBT. Our data demonstrate the benefits of more information being made available to the medical team before patient's arrival. With the addition of each prehospital variable in succession—that is, arrival by emergency medical services, Cath Alert system, prehospital ECG—the DBT can be progressively shortened and the adverse “off hour effect” nullified.
Acknowledgements
We wish to acknowledge the steady efforts of the Department of Cardiology, cardiac catheterisation team, Emergency Department physicians, and Emergency Medical Services.
Abbreviations
ACC/AHA - American College of Cardiology/American Heart Association
Cath Alert - catheterisation team activation
DBT - door‐to‐balloon times
ECG - electrocardiogram
PCI - percutaneous coronary intervention
STEMI - ST segment elevation myocardial infarction
Footnotes
Competing interests: None declared.
References
- 1.Thom T, Haase N, Rosamond W.et al Heart disease and stroke statistics–2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2006113e85–151. [DOI] [PubMed] [Google Scholar]
- 2.Boersma E, Maas A C P, Deckers J W.et al Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet 1996348771. [DOI] [PubMed] [Google Scholar]
- 3.Cannon C P, Gibson C M, Lambrew C T.et al Relationship of symptom‐onset‐to‐balloon time and door‐to‐balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 20002832941–2947. [DOI] [PubMed] [Google Scholar]
- 4.De luca G, Suryapranata H, Ottervanger J P.et al Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 20041091223–1225. [DOI] [PubMed] [Google Scholar]
- 5.Grines C L, Browne K F, Marco J, for the Primary Angioplasty in Myocardial Infarction Study Group et al A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. N Engl J Med 1993328673–679. [DOI] [PubMed] [Google Scholar]
- 6.Zijlstra F, Hoorntje J C, de Boer M J.et al Long‐term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med 19993411413–1419. [DOI] [PubMed] [Google Scholar]
- 7.Antman E M, Anbe D T, Armstrong P W.et al ACC/AHA guidelines for the management of patients with ST‐elevation myocardial infarction‐‐executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004110588–636. [DOI] [PubMed] [Google Scholar]
- 8.McNamara R L, Herrin J, Bradley E H.et al Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol 20064745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradley E, Herrin J, Wang Y.et al Strategies for reducing the door‐to‐balloon time in acute myocardial infarction. N Engl J Med 20063552308–2320. [DOI] [PubMed] [Google Scholar]
- 10.Canto J G, Rogers W J, Bowlby L J.et al The prehospital electrocardiogram in acute myocardial infarction: is its full potential being realized? National Registry of Myocardial Infarction 2 Investigators. J Am Coll Cardiol 199729498–505. [DOI] [PubMed] [Google Scholar]
- 11.Majid D J, Wang Y, Herrin J.et al Relationship between time of day, day of week, timeliness of reperfusion, and in‐hospital mortality for patients with acute ST‐segment elevation myocardial infarction. JAMA 2005294803–812. [DOI] [PubMed] [Google Scholar]
- 12.McNamara R L, Wang Y, Herrin J.et al Effect of door‐to‐balloon time on mortality in patients with ST‐segment elevation myocardial infarction. J Am Coll Cardiol 2006472180–2186. [DOI] [PubMed] [Google Scholar]
- 13.Bradley E H, Roumanis S A, Radford M J.et al Achieving door‐to‐balloon times that meet quality guidelines: how do successful hospitals do it? J Am Coll Cardiol 2005461236–1241. [DOI] [PubMed] [Google Scholar]
- 14.Bradley E H, Herrin J, Wang Y.et al Door‐to‐drug and door‐to‐balloon times: where can we improve? Time to reperfusion therapy in patients with ST‐segment elevation myocardial infarction (STEMI). Am Heart J 20061511281–1287. [DOI] [PubMed] [Google Scholar]
- 15.Keriakes D J, Gibler B, Martin L H.et al Relative importance of emergency medical system transport and the prehospital electrocardiogram on reducing hospital time delay to therapy for acute myocardial infarction: a preliminary report from the Cincinnati Heart Project. Am Heart J 1992123(4 Pt 1)835–840. [DOI] [PubMed] [Google Scholar]
- 16.Feldman J A, Brinsfield K, Bernard S.et al Real‐time paramedic compared with blinded physician identification of ST‐segment elevation myocardial infarction: results of an observational study. Am J Emerg Med 200523443–448. [DOI] [PubMed] [Google Scholar]
- 17.Thatcher J L, Gilseth T A, Adlis S. Improved efficiency in acute myocardial infarction care through commitment to emergency department initiated primary PCI. J Invasive Cardiol 200315693–698. [PubMed] [Google Scholar]
- 18.Canto J G, Zalenski R K, Ornato, et al Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation 20021063018–3023. [DOI] [PubMed] [Google Scholar]