Abstract
OBJECTIVE
To quantify the incremental survival benefit of the pancreas allograft in simultaneous pancreas-kidney (SPK) transplant recipients.
RESEARCH DESIGN AND METHODS
Data from the national transplant database from 2000 to 2007 were analyzed. SPK recipients who had functioning allografts to 1-year post transplant (n = 3,304) were compared with those who had failure of the renal (n = 233) or pancreatic (n = 112) graft. The main outcome was a projection of 10 life-years of patient survival beyond the first transplant anniversary.
RESULTS
Recipients with function of both organs accrued 9.4 life-years following transplantation. Projected survival in patients with kidney failure was reduced to 2.5 life-years. Pancreas failure reduced predicted survival to 8 life-years. Renal allograft failure impacts life expectancy significantly (adjusted hazard ratio [aHR] 12.13). However, pancreas allograft failure was also associated with reduced survival (aHR 2.62).
CONCLUSIONS
Although the majority of the survival benefit of SPK transplant is due to the renal transplant, pancreas allograft function does contribute to patient survival.
The American Diabetes Association considers simultaneous pancreas-kidney (SPK) transplantation the treatment of choice for patients with type 1 diabetes and chronic renal failure (1). Previous studies have questioned the incremental benefit of the pancreas allograft compared with kidney transplant alone for the uremic diabetic patients (2–9). This study aims to quantify the incremental value of the pancreas allograft function to the survival of SPK transplant recipients.
RESEARCH DESIGN AND METHODS
A retrospective cohort study of all SPK transplant recipients between 1 January 2000 and 31 December 2007 was performed utilizing data from the Organ Procurement and Transplantation Network (OPTN) research files. Adult (age >18 years), first-SPK transplant recipients with chronic renal failure due to type 1 diabetes were included. The primary outcome was projected incremental life-years attributed to each allograft's function based on data from recipients of SPK transplantation with dual function (n = 3,304), isolated kidney graft failure (n = 233), or pancreas graft failure (n = 112) (10).
Perioperative mortality risk increases the hazard of death early after transplant, complicating the projection of long-term survival with a single mathematical function. We utilized a two-part strategy to quantify the implications of organ-specific allograft failure on patient survival. First, we estimated the independent associations of kidney and pancreas failure with relative mortality risk (adjusted hazard ratio [aHR]) by multivariable Cox regression, using 5 years of observed registry data. We then computed long-term survival expectations by parametric regression assuming a Weibull survival function. Survival expectation of patients who sustained function of both organs was estimated as the reference by censoring of time to death at the first occurrence of kidney or pancreas failure, and the area under a 10-year survival projection beyond the first transplant anniversary was computed as the life-years expectancy over 10 years. The daily mortality hazard in the reference group was computed as the difference in projected survival between day x and day x + 1. Survival expectations with organ-specific graft failure were quantified by multiplying reference group daily hazards by the associated relative hazard ratio computed for graft failure using Cox regression analysis and sequentially subtracting estimated survival decrements at each day over 10 years.
RESULTS
Survival was projected for 3,649 SPK recipients who survived with functioning allografts to the first anniversary following SPK over a possible 10-year time horizon. The long-term mortality impact of transplant failure is substantially greater following kidney failure (aHR 12.13 for death >30 days after organ failure) than after pancreas failure (aHR 2.62 for death >30 days after organ failure).
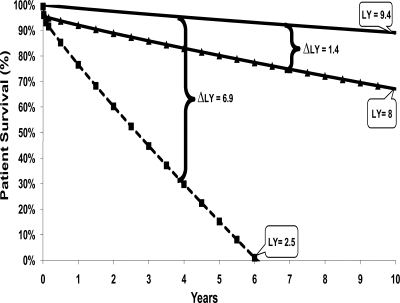
In our projection, loss of both kidney and pancreas allograft function had a substantial impact on the estimated survival for SPK patients over the 10 years post transplantation (Fig. 1). Overall, recipients of SPK transplants who had kidney allograft failure lost 6.9 of the 9.4 life-years expected for patients with preserved function of both organs. Pancreas allograft failure was associated with a reduction of 1.4 of the 9.4 life-years expected after SPK transplantation with long-term sustained function of both grafts. Thus, kidney failure reduced expected survival by 85%, while pancreas loss reduced projected survival by 15% among SPK recipients.
Figure 1.
Survival plot among patients with long-term sustained function of both allografts compared with expected survival with organ-specific graft failure.* SPK recipient with no graft failure (n = 3,304) (solid line); SPK recipient with pancreas allograft failure and sustained kidney allograft function (n = 233) (▴); and SPK recipient with kidney allograft failure and sustained pancreas allograft function (n = 112) (■). Δ, the difference in patient survival (in life-years) caused by loss of a graft; LY, life-year. *Depicted scenarios assume that allograft failures occur at day 365 after SPK transplant (at time zero on the survival plot).
CONCLUSIONS
Understanding the independent value of the pancreas allograft is vital to the assessment of the benefits of SPK transplantation and assessment of allocation policy. We chose to begin the analysis after 1 year to avoid the initial postoperative period, when most surgical and medical complications often occur but most of the benefits have not yet accrued (8,11). The timing of graft failure events might impact the calculation of life-years gained from a transplant; however, in our pilot studies, it did not modify the main results herein presented.
We have demonstrated that although the likelihood of death after allograft failure is substantially greater following kidney failure, pancreas loss does have a detrimental impact on patient survival. This analysis is limited by our inability to determine whether the reduction in survival was the result of a complication from the graft loss itself or from the loss of function over time. The natural experiment observed using this method eliminated the major weaknesses of previous studies: selection bias of comparison of SPK and isolated renal transplant recipients who may differ in both patient and donor characteristics (2–9). One could argue that the independent value of each allograft might be difficult to isolate because of the interactive processes between both organs (such as a reduction in rejection due to the presence of an additional organ). However, we did not find any data documenting this effect.
We estimated the kidney and pancreas allograft function to contribute ∼85 and 15%, respectively, to the expected patient life-years survival benefit of SPK transplantation. There is clearly an identifiable, independent life-years benefit from the pancreas allograft. Based on our data, launching of new allocation policies that will augment the volume of SPK transplantation should be supported.
In addition to the known limitations of retrospective registry studies, our findings have other limitations. The OPTN Registry does not carry indexes of glycemic control. This prevents analysis of the relationship between strict normoglycemia and pancreas allograft life-years gain. We have not included the impact on quality of life produced by differential allograft survival in specific clinic scenarios, such as patients with brittle diabetes (12). Finally, there are inherent methodological limitations of any attempt to predict future outcomes based on available data and assumptions. However, similar projections have performed well compared with actual outcomes, suggesting that this method is robust.
In summary, the majority of life-years gained following SPK is related to preserved renal allograft function. The pancreas allograft appears to have an important, but smaller, independent role in adding life-years for type 1 diabetic patients with chronic renal failure.
Acknowledgments
P.R.S. is supported by a grant from the American Society of Transplantation. K.L.L. is supported by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (K08-0730306). The data reported here have been supplied by the United Network for Organ Sharing as the contractor for the Organ Procurement and Transplantation Network. No other potential conflicts of interest relevant to this article were reported.
Parts of this study were presented in abstract form at the American Transplant Congress, Toronto, Canada, 31 May–4 June 2008.
We thank Connie Davis, MD, and Ian de Boer, MD, for revising the manuscript.
Footnotes
The interpretation and reporting of these data are the sole responsibility of the authors and should in no way be seen as representing the official policy of or interpretation by the Organ Procurement and Transplantation Network, the American Society of Transplantation, or the U.S. government.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1. American Diabetes Association: Pancreas transplantation for patients with type 1 diabetes. Diabetes Care 23. ( Suppl. 1): S85, 2000 [PubMed] [Google Scholar]
- 2. Venstrom JM, McBride MA, Rother KI, Hirshberg B, Orchard TJ, Harlan DM: Survival after pancreas transplantation in patients with diabetes and preserved kidney function. JAMA 290: 2817– 2823, 2003 [DOI] [PubMed] [Google Scholar]
- 3. Manske CL, Wang Y, Thomas W: Mortality of cadaveric kidney transplantation versus combined kidney-pancreas transplantation in diabetic patients. Lancet 346: 1658– 1662, 1995 [DOI] [PubMed] [Google Scholar]
- 4. Rayhill SC, D'Alessandro AM, Odorico JS, Knechtle SJ, Pirsch JD, Heisey DM, Kirk AD, Van der Werf W, Sollinger HW: Simultaneous pancreas-kidney transplantation and living related donor renal transplantation in patients with diabetes: is there a difference in survival? Ann Surg 231: 417– 423, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Smets YF, Westendorp RG, van der Pijl JW, de Charro FT, Ringers J, de Fitjer JW, Lemkes HH: Effect of simultaneous pancreas-kidney transplantation on mortality of patients with type 1 diabetes mellitus and end-stage renal failure. Lancet 353: 1915– 1919, 1999 [DOI] [PubMed] [Google Scholar]
- 6. Bunnapradist S, Cho YW, Cecka JM, Wilkinson A, Danovitch GM: Kidney allograft and patient survival in type I diabetic recipients of cadaveric kidney alone versus simultaneous pancreas kidney transplants: a multivariate analysis of the UNOS database. J Am Soc Nephrol 14: 208– 213, 2003 [DOI] [PubMed] [Google Scholar]
- 7. Gutiérrez P, Marrero D, Hernandez D, Vivancos S, Perez-Tamajon L, Rodriguez de Vera JM, Alarco A, Gonzalez-Posada JM: Surgical complications and renal function after kidney alone or simultaneous pancreas-kidney transplantation: a matched comparative study. Nephrol Dial Transplant 22: 1451– 1455, 2007 [DOI] [PubMed] [Google Scholar]
- 8. Ojo AO, Meier-Kriesche HU, Hanson JA, Leichtman AB, Magee JC, Wolfe RA, Port FK, Agodoa L, Kaufman DB, Kaplan B: The impact of simultaneous pancreas-kidney transplantation on long-term patient survival. Transplantation 71: 82– 90, 2001 [DOI] [PubMed] [Google Scholar]
- 9. Mohan P, Safi K, Little DM, Donohoe J, Conlon P, Walshe JJ, O'Kelly P, Thompson CJ, Hickey DP: Improved patient survival in recipients of simultaneous pancreas-kidney transplant compared with kidney transplant alone in patients with type 1 diabetes mellitus and end-stage renal disease. Br J Surg 90: 1137– 1141, 2003 [DOI] [PubMed] [Google Scholar]
- 10. Wolfe RA, McCullough KP, Schaubel DE, Kalbfleisch JD, Murray S, Stegall MD, Leichtman AB: Calculating life years from transplant (LYFT): methods for kidney and kidney-pancreas candidates. Am J Transplant 8: 997– 1011, 2008 [DOI] [PubMed] [Google Scholar]
- 11. Troppmann C, Gruessner AC, Dunn DL, Sutherland DE, Gruessner RW: Surgical complications requiring early relaparotomy after pancreas transplantation: a multivariate risk factor and economic impact analysis of the cyclosporine era. Ann Surg 227: 255– 268, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gruessner RW, Sutherland DE, Kandaswamy R, Gruessner AC: Over 500 solitary pancreas transplants in nonuremic patients with brittle diabetes mellitus. Transplantation 85: 42– 47, 2008 [DOI] [PubMed] [Google Scholar]