Abstract
Aim
To outline the efficacy of a steroid injection in treating trigger finger. Our study defines the anatomy of the A1 pulley, and suggests methods for simple and safe flexor sheath injection for trigger finger and thumb.
Method
Systematic review of published literature on trigger finger and thumb and its treatment, particularly steroid injection. The use of the knowledge of the superficial landmarks of the A1 pulley with the techniques described were combined to provide a comprehensive guide to injecting steroids in patients with trigger finger and thumb.
Results
Several studies are outlined, which provided evidence to suggest that a steroid injection into the flexor sheath of the affected digit is successful in treating most of the patients. Methods of identifying the superficial landmarks of the A1 pulley and of approaching the pulley without injury to surrounding structures are also outlined in the literature. Two different techniques used to infiltrate the flexor sheath were described.
Conclusion
Steroid injection in the flexor sheath at the level of the A1 pulley is an effective method of treating patients with trigger finger and should be considered as the preferred treatment. Specific anatomical landmarks and methods allow the procedure to be carried out without fear of inadvertent damage to surrounding structures.
Keywords: steroid injection, trigger finger, techniques
A corticosteroid injection, if given appropriately and correctly, is an effective method of dealing with several disorders of the upper limb. To give the injection correctly and safely into the affected structures, the practitioner requires knowledge of the local anatomy and a technique that minimises risk and maximises benefit.
Trigger finger is a common condition causing pain and disability in the hand and accounts for a large number of patients referred to a hand unit. The condition presents with discomfort in the palm during movement of the involved digits. Gradually, or occasionally, acutely, the flexor tendon causes painful popping or snapping as the patient flexes and extends the digit. As the condition progresses, the digit may begin to lock in a particular position, more often flexion, which may require gentle passive manipulation into full extension. Trigger finger arises through a discrepancy in the diameter of the flexor tendon and its sheath at the level of the metacarpal head known as the A1 pulley. This thickening of the sheath can result in a narrowed tunnel for tendon excursion and ultimately result in a block to tendon excursion. However, the flexors are usually powerful enough to overcome this obstruction, whereas the weaker extensors are less able to counteract the block, resulting in the finger being locked in flexion.
A steroid injection into the flexor sheath at the level of A1 pulley, of the affected digit, during the early stages of the disease can be very effective. This can be carried out in a clinic environment—either a hospital or community setting.
In this paper, we define the efficacy of a steroid injection for the treatment of trigger finger and thumb in the adult population, as well as defining the anatomy of the flexor sheath and the relevant surrounding structures. We also describe two methods of accurately infiltrating the flexor sheath and illustrate methods of avoiding damage to the surrounding structures.
Methods
We used Medline and PubMed to search for relevant English language literature. We used the search terms “trigger finger”, “stenosing tenosynovitis” and “A1 pulley anatomy”. From these, we identified literature that discussed the efficacy of steroid injections to treat trigger finger, outlined techniques for injection for trigger finger and thumb and also those that explored the anatomy of the A1 pulley. Additional literature was identified from the references of these papers.
Results
Efficacy of steroid injection for trigger finger
We identified six studies that, while assessing the efficacy of steroid injections in the treatment of adult trigger finger, also clearly stated the number of treatments required to obtain cure and followed up patients for >1 year (table 1).
Table 1 The studies that assessed the efficacy of steroid injections for trigger finger .
| Year | No of patients | No of digits | Cure after one treatment (%) | Total cure rate after ⩾1 treatments (%) | Average follow‐up (months) | |
|---|---|---|---|---|---|---|
| Clark et al1 | 1973 | 50 | 76 | 55 | 82 | 44 |
| Rhodes2 | 1984 | 39 | 53 | 66 | 72 | 25 |
| Marks and Gunther3 | 1989 | 71 | 104 | 84 | 93 | 41 |
| Newport et al4 | 1990 | 235 | 302 | 49 | 73 | 35 |
| Anderson and Kaye5 | 1991 | 58 | 77 | 61 | 88 | 55 |
| Benson and Ptaszek6 | 1992 | 102 | 109 | 60 | 76 | 18 |
Howard et al7 advocated the injection of steroids into the flexor sheath as a method of treatment in 1953. Success rates vary between the studies; however, all the studies showed a successful outcome in a large proportion of their patients after a single steroid injection (table 1). Some of the authors define factors within a population that affected the outcome, and these help to explain reasons for some for the variations in outcome. Poorer outcomes are seen in patients with coexisting systemic illnesses, such as patients with diabetes mellitus and rheumatoid arthritis, and those with multiple‐digit involvement.2,4,8 Higher success rates are seen when the steroid is injected into the thumb, in the female population, and in patients in whom, clinically, a well‐defined nodule was palpable or in whom symptom duration was <4–6 months.2,3,4,9
In the studies reviewed, a second steroid injection offers benefits when given to patients in whom symptoms had resolved, but later recurred in the same digit. Recurrence occurred between an average of 3 and 37 months after the initial treatment.1,3,5,6,9 The efficacy of a second injection given after primary failure is less well defined.
All the literature described so far refer to injections being given or attempted to be given into the flexor sheath of the affected digit. A study that assessed the accuracy of injection into the flexor sheath found that successful intrasheath injection occurred in only 49% of patients.10 A further study showed that steroids placed subcutaneously around the A1 pulley also proved to be successful in treating the condition.11
The main complication is self‐limiting pain at the injection site; other complications are rare, but include dermal or subcutaneous atrophy, hypopigmentation of the skin, infection of the flexor sheath and, in one rare case, rupture of the tendon.5,6 People with diabetes should expect erratic glucose levels for up to 1 week after the injection.
Anatomy
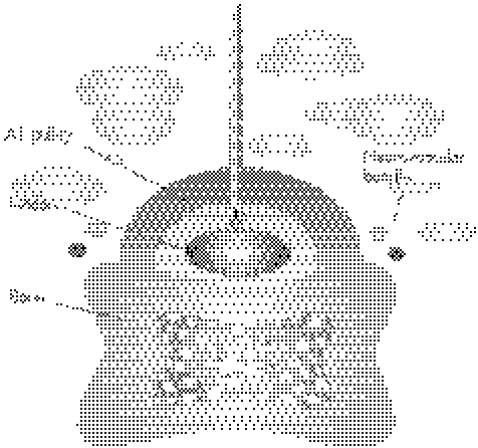
The flexor sheath is a membranous structure that surrounds the flexor tendons from the metacarpal neck to the volar plate of the distal interphalangeal joint. It is attached longitudinally to the underlying bony structures. The sheath is thick over the bones (the annular pulley portion of the system) and thin (cruciform pulley portion) in areas overlying the joints, to allow digital flexion. The A1 pulley marks the proximal border of the flexor sheath and overlies the metacarpal neck. The proximal border can be roughly defined by the distal palmar crease (fig 1); however, this point can be more accurately defined using the findings of cadaver studies, which showed that the proximal border of the A1 pulley can be located by measuring the distance between the proximal digital crease (fig 1) and the proximal interphalangeal joint crease. This value can be used to measure the same distance proximally from the proximal digital crease. The mean (standard deviation (SD)) length of the A1 pulley has been found to be 1.17 (0.02) cm for the adult index, middle and ring fingers, and 0.98 (0.02) cm for the adult little finger.12
Figure 1 Diagram outlining surface landmarks of the hand.
In the thumb, middle and ring fingers, the neurovascular bundles to the respective digits pass longitudinally lateral to the borders of the A1 pulley. However, in the border digits (index and little fingers), the border neurovascular bundle may pass close to, and occasionally across, the path of the respective digit's A1 pulley (fig 2).
Figure 2 Axis of safety to the A1 pulleys of the little and index fingers.
However, studies on cadaver specimens have allowed mapping of the border digit neurovascular bundles in relationship to their respective A1 pullies. Subsequently, it has become possible to accurately define a longitudinal path along the A1 pulley along which the neurovascular bundle does not cross. This, therefore, identifies a safe axis that will allow any invasive treatment for these digits to be carried out without any inadvertent injury to their associated neurovascular bundles. For the little finger, the longitudinal axis of safety avoiding the neurovascular bundles lies on the line between the midpoint of the proximal digital crease of the little finger and the scaphoid tubercle. For the index finger, the longitudinal axis of safety lies on the line between the midpoint of the proximal digital crease of the index finger and the radial edge of the pisiform13 (fig 2). These landmarks are important when considering protection of neurovascular structures if invasive interventions are under consideration.
Techniques
Two different techniques to infiltrating the flexor sheath for patients with trigger finger and thumb are described in the literature.3,4,5 In this section, we use the knowledge of the surface markings of the A1 pulley, as described earlier, to mark a safe site for injection and then describe the two techniques described in the literature.
The first step is to prepare the skin and then identify the point on the palm where the A1 pulley can safely be injected. This can be achieved by using the landmark guides described earlier. Firstly, mark the proximal and distal borders of the affected A1 pulley, and mark the midpoint between these two landmarks. Now mark the axis of safety on the skin (for the ring and middle fingers, this lies in the line of the digit); for the index and little finger the axis of safety must be plotted using the method described previously. The point at which the axis of safety crosses the A1 pulley will determine the point of steroid injection. Placing the hand in a hyperextended position presents the pulley in a more superficial position, with the neurovascular bundles pushed medially and laterally away from the sheath.14
For the thumb, which lies in a plane at 90° to that of the other fingers, the planning in positioning the hand and the point of injection must be reconsidered. Firstly, draw a straight line longitudinally along the centre of the volar surface of the thumb, ensuring that this line is extended on to the palm; at the point at which this line crosses the proximal crease of the thumb, mark the point of injection. Now position the hand in such a way that the volar surface of the thumb is orientated towards you (fig 3).
Figure 3 Longitudinal axis of the A1 pulley of the thumb.
Draw up 1 ml of depot steroid along with 1 ml of local anaesthetic without epinephrine into a 2.5 ml syringe. Insert a 23‐gauge needle at a 45° angle to the skin at the marked point (figs 3, 4). For the thumb, introduce the needle at 45° to the skin in the line of the longitudinal central markings on the thumb. A common error is to introduce the needle pointing to the radial or ulnar side of the thumb. Two different approaches to infiltrating the flexor sheath are available.
Figure 4 Needle entering into the skin at a 45° angle over the highlighted surface markings of the A1 pulley.
Method 1
Insert the needle through the skin, subcutaneous tissue, tendon sheath and tendon until you reach bone so that the tip of the needle cannot be advanced any further. The opening of the lumen of the hypodermic needle should lie in the flexor sheath between the metacarpal neck and the tendon (fig 5). Aspirate, then gently applying pressure to the plunger on the syringe, so that the infiltrate flows with ease into the flexor sheath. If resistance to flow is encountered, then maintain some pressure on the plunger and gently manoeuvre the needle so that the tip is a fraction of a millimetre either deeper or more superficial to its initial position; when the lumen of the needle lies free in the flexor sheath, the steroid will flow freely.
Figure 5 A cross‐sectional view of the needle entering into the flexor sheath, but not passing through the tendon substance.
This method is a reliable and easy method of infiltrating the sheath. However, in a tight pulley, when there is very little space between tendon and bone, infiltration can prove difficult.
Method 2
Insert the needle through the skin to the bone as previously described, then withdraw the needle by 1 cm; the tip of the needle now lies in the substance of the flexor tendon. Gently remove the syringe from the needle, leaving the needle tip in the tendon substance and ask the patient to slowly partially flex and extend the involved digit. The needle will swing distally and proximally on flexion and extension, confirming that the needle tip is still in the tendon. Withdraw the needle by 1 mm and repeat the process until the needle no longer swings on movement of the digit; at this point, part of the needle tip is in the gap between the tendon and the A1 pulley (fig 6). Gentle pressure on the syringe plunger should allow the infiltrate to pass into the flexor sheath.
Figure 6 A cross‐sectional view of the needle entering into the flexor sheath by passing through the tendon substance.
In situations when the A1 pulley is too tight around the flexor sheath to allow intrasheath infiltration, one can enter the flexor sheath further distally at the midpoint between the proximal digital crease (fig 1) and the proximal interphalangeal joint crease, and ensure that the needle bevel points proximally. With this method, some of the steroid will reach the distal border of the A1 pulley.
As the fluid is infiltrated into the flexor sheath, one of three events may occur:
The affected digit will slowly and gently flex as the sheath becomes tense.
One may gain an impression of fluid flowing along the flexor sheath at the level of the proximal phalanx.5
Within seconds of infiltration, the tip of the involved finger may become pale and slightly swollen owing to distension of the blind‐ended flexor sheath distally. This resolves within seconds.15
Conclusion
Steroid injection into the flexor sheath at the level of the A1 pulley is an effective method of treating patients with trigger finger and should be considered as the preferred treatment. Knowledge of local anatomy and a well‐tested technique allows steroid injections to be given safely in a primary care setting to patients with trigger finger or thumb, with minimal risk and maximal benefit.
Footnotes
Competing interests: None declared.
References
- 1.Clark D D, Ricker J H, MacCollum M S. The efficacy of local steroid injection in the treatment of stenosing tenovaginitis. Plast Reconstr Surg 197351179–180. [DOI] [PubMed] [Google Scholar]
- 2.Rhodes C E, Gelberman R H, Manjarris J F. Stenosing tenosynovitis of the fingers and thumb. Clin Orthop 1984190236–238. [PubMed] [Google Scholar]
- 3.Marks M R, Gunther S F. Efficacy of cortisone injection in treatment of trigger fingers and thumbs. J Hand Surg 198914A722–727. [DOI] [PubMed] [Google Scholar]
- 4.Newport M L, Lane L B, Stuchin S A. Treatment of trigger finger by steroid injection. J Hand Surg 199015A748–750. [DOI] [PubMed] [Google Scholar]
- 5.Anderson B, Kaye S. Treatment of flexor tenosynovitis of the hand with corticosteroids. A prospective study of the response to local injection. Arch Intern Med 1991151153–156. [PubMed] [Google Scholar]
- 6.Benson L S, Ptaszek A J. Injection versus surgery in the treatment of trigger finger. J Hand Surg 199722A138–144. [DOI] [PubMed] [Google Scholar]
- 7.Howard L, Pratt D R, Bunnell S. The use of compound F (hydrocotisone) in operative and non‐operative conditions of the hand. J Bone Joint Surg 195235A994–1002. [PubMed] [Google Scholar]
- 8.Kolind‐Sorenson V. Treatment of trigger fingers. Acta Orthop Scand 197041428–432. [DOI] [PubMed] [Google Scholar]
- 9.Freiberg A, Mulholland R S, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg 198914A553–558. [DOI] [PubMed] [Google Scholar]
- 10.Kamhin M, Engel J, Heim M. The fate of injected trigger fingers. Hand 198317218–283. [DOI] [PubMed] [Google Scholar]
- 11.Taras J S, Raphael J S, Pan W T.et al Corticosteroid injections for trigger digits: is intrasheath injection necessary. J Hand Surg (Am) 199823717–722. [DOI] [PubMed] [Google Scholar]
- 12.Wilhelmi B J, Snyder N I V, Verbesey J E.et al Trigger finger release with hand surface landmark ratios: an anatomic and clinical study. Plast Reconstr Surg 2001108908–915. [DOI] [PubMed] [Google Scholar]
- 13.Wilhelmi B J, Mowlavi A, Neumeister M W.et al Safe treatment of trigger finger with longitudinal and transverse landmarks: an anatomic study of the border fingers for percutaneous release. Plast Reconstr Surg 2003112993–999. [DOI] [PubMed] [Google Scholar]
- 14.Bain G I, Turnbull J, Charles M N.et al Percutaneous A1 pulley release: a cadaveric study. J Hand Surg 199520781–784. [DOI] [PubMed] [Google Scholar]
- 15.Murphy D, Failla J M, Koniuch M P. Steroid versus placebo injection for trigger finger. J Hand Surg 199520A628–631. [DOI] [PubMed] [Google Scholar]