Abstract
Collagen deposition is observed in a diverse set of pulmonary diseases, and the unraveling of the molecular signaling pathways that facilitate collagen deposition represents an ongoing area of investigation. The stress-activated protein kinase, c-Jun N-terminal kinase 1 (JNK1), is activated by a large variety of cellular stresses and environmental insults. Recent work from our laboratory demonstrated the critical role of JNK1 in epithelial to mesenchymal transition. The goal of the present study was to examine the involvement of JNK1 in subepithelial collagen deposition in mice subjected to models of allergic airways disease and interstitial pulmonary fibrosis. Activation of JNK was slightly enhanced in lungs from mice subjected to sensitization and challenge with ovalbumin (Ova), and predominant localization of phospho-JNK was observed in the bronchial epithelium. While mice lacking JNK1 (JNK1−/− mice) displayed enhanced lung inflammation and cytokine production compared with wild-type (WT) mice, JNK1−/− mice accumulated less subepithelial collagen deposition in response to antigen, and showed decreased expression of profibrotic genes compared with WT animals. Furthermore, transforming growth factor (TGF)-β1 content in the bronchoalveolar lavage was diminished in JNK1−/− mice compared with WT animals subjected to antigen. Finally, we demonstrated that mice lacking JNK1 were protected against TGF-β1 and bleomycin-induced pro-fibrotic gene expression and pulmonary fibrosis. Collectively, these findings demonstrate an important requirement for JNK1 in promoting collagen deposition in multiple models of fibrosis.
Keywords: TGF-β, ovalbumin, asthma, fibrosis, bleomycin
CLINICAL RELEVANCE
These findings demonstrate an important requirement for JNK1 in promoting collagen deposition in models of airway and interstitial fibrosis. Unraveling of the molecular mechanisms that facilitate collagen deposition could lead to novel therapies.
Fibrosis of the lung is characterized by increased expression of mesenchymal genes and collagen deposition, and can lead to tissue stiffening and impaired gas exchange (1). The cytokine, transforming growth factor (TGF)-β1, has been implicated as a key regulator of collagen deposition, and TGF-β1 pathway activation occurs in the airways of patients with pulmonary fibrosis, asthma, and chronic obstructive pulmonary disease (COPD) (2–7). Airway remodeling in idiopathic pulmonary fibrosis (IPF) and allergic airway disease is believed to occur as a result of ongoing chronic inflammation, and may lead to irreversible changes in lung structure, in part due to collagen deposition (8–11). The decline in forced expiratory volume in 1 second (FEV1), characteristic of patients with asthma, has been correlated to the extent of subepithelial fibrosis around the airways (12, 13). Similarly, in the ovalbumin (Ova) model of allergic airway disease in the mouse, enhanced deposition of collagen occurs around the airways (14), and methacholine responsiveness has been related to the level of subepithelial collagen deposition (15, 16). The progression of airway remodeling and fibrosis in asthma and IPF is believed to represent a critical indicator of disease severity.
c-Jun N-terminal kinase (JNK), a member of the mitogen-associated protein kinase (MAPK) family, is encoded by three genes termed JNK1, JNK2, and JNK3. JNK1 and JNK2 are ubiquitously expressed, while JNK3 is limited to the testis, heart, and brain (17). JNK is activated in response to a wide variety of stresses, and in turn phosphorylates several transcription factors including c-Jun, JunB, JunD, and ATF-2 on specific serine and threonine residues (18). A number of observations suggest a potential role for JNK in allergic airway disease and fibrosis. Studies in T cells lacking JNK1 or JNK2 demonstrated its critical role in T cell differentiation (19). JNK activation also has been linked to the enhancement of glucocorticoid-induced apoptosis of eosinophils, although conversely, JNK activation in epithelial cells was implicated in contributing to steroid resistance (20). Importantly, in rats, the JNK inhibitor SP600125 significantly dampened airway inflammatory responses and bromodeoxyuridine incorporation in airway epithelial and smooth muscle cells induced by antigen, but failed to alter airway mechanics measured by whole body plethysmography (21). Conversely, in mice subjected to the Ova model, increases in AHR were attenuated by the same JNK inhibitor (22). A broader role for JNK in fibrosis is suggested by observations demonstrating that patients with IPF showed elevated phosphorylation of JNK in the airway epithelium and pulmonary endothelium (23, 24). Finally, a recent study from our laboratory demonstrated that JNK1 plays a causal role in TGF-β1–induced epithelial to mesenchymal transition (EMT) and profibrotic gene expression, while JNK2 appears to play a minor role (25).
The goal of the present study was to determine the role of JNK1 in subepithelial collagen deposition and pulmonary fibrosis. We therefore measured the extent and localization of JNK activation in the Ova model of allergic airways disease, and in TGF-β1– or bleomycin-induced pulmonary fibrosis. We then evaluated the impact of JNK1 gene ablation on collagen accumulation in these models. Our findings indicate a critical role for JNK1 in promoting collagen deposition in multiple models of fibrosis.
MATERIALS AND METHODS
Animals and Reagents
Two- to four-month-old C57BL/6 mice were purchased from Charles River Laboratories (Ste. Constant, PQ, Canada). JNK1−/− mice were backcrossed more than 10 generations onto the C57BL/6 background and have been previously described (19). All chemicals used were purchased from Sigma-Aldrich (St. Louis, MO) unless otherwise noted. All animal studies were approved by the Institutional Animal Care and Use Committee at the University of Vermont. Anti-Smad2 antibody was purchased from Cell Signaling Technology (Danvers, MA). Antibodies to JNK1, phosho-c-Jun, c-Jun, β-actin, and α-SMA were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Pan-cytokeratin antibody was purchased from Zymed (San Francisco, CA).
Models of Pulmonary Fibrosis
Allergic airway disease was induced by intraperitoneal injection of mice with 40 μg of the antigen Ova with the adjuvant aluminum hydroxide (Alum) (Pierce Chemical, Rockford, IL) on Days 1 and 7 to induce sensitization. Sham-sensitized mice received Alum alone. Mice were then exposed to an aerosolized 1% Ova solution in sterile phosphate-buffered saline (PBS) for 30 minutes on Days 14 through 19. Lung tissues were harvested 2 days (Day 21) after the final Ova challenge. In the study in which cytokines and TGF-β1 were assayed in the bronchoalveolar lavage (BAL) fluid, mice were challenged with Ova on Days 14 through 16, and harvested on Day 18.
TGF-β1–induced pulmonary fibrosis was generated by instilling TGF-β1 into airways (26) by oropharyngeal aspiration (40 μl). Mice received four doses of 200 ng of recombinant human TGF-β1 (R&D Systems, Minneapolis, MN) in 4 mM HCl diluted in sterile PBS, or PBS plus vehicle alone, on Days 1, 2, 4, and 7, and were killed on Day 14 for evaluation of gene expression changes and assessment of phospho-Smad2.
Interstitial pulmonary fibrosis was induced after administration of bleomycin, 7.5 U/kg (Gensia Sicor Pharmaceuticals, Irvine, CA) in sterile PBS, by oropharyngeal aspiration (40 μl), and evaluation of lung tissues on Day 21, a time point at which enhanced collagen deposition occurs (27).
Lung Histology and Immunofluorescence
Lungs were inflated and fixed with 4% paraformaldehyde in PBS followed by paraffin imbedding. Paraffin blocks were cut into 5-μm sections and mounted to slides. Tissue histopathology and inflammation were assessed by hematoxylin and eosin staining. Mucus metaplasia was determined by periodic acid Schiff staining (PAS), and quantified by scoring airway PAS reactivity using a scale of 0 to 3 (0 representing no positive staining and 3 being the highest intensity) by two independent, blinded observers. Slides were scored twice by each investigator and the cumulative score from each mouse was then averaged according to treatment group. Immunofluoresence for phospho-Smad2 was performed after deparaffinization, rehydration, and antigen retrieval at more than 95°C for 30 minutes (Cell Signaling Technology). Immunofluoresence for phospho-JNK1 was performed on frozen lung blocks inflated with PBS/Optimal Cutting Temperature (OCT) medium (1:1 ratio). Frozen lung blocks were then cut into 10-μm sections, and were permeabilized with 1% Triton-X-100. Primary antibodies were incubated overnight at 4°C. AlexaFluor secondary antibodies (Molecular Probes, Eugene, OR) were then incubated for 1 hour at room temperature. Subsequent nuclear counterstaining was performed with Sytox Green (Molecular Probes) for 5 minutes at room temperature. Stained lung sections were assessed by confocal laser scanning microscopy (Bio-Rad MRC 1024ES; Carl Zeiss Microimaging, Thornwood, NY). Staining intensity was determined by measuring pixel density using the NIH Image J software package.
Lung Homogenizing and Western Blotting
Protein lysates were prepared by mincing lung tissue in cold lysis buffer (50 mM Tris, 150 mM NaCl, 10% [vol/vol] glycerol, 0.5% [vol/vol] Nonidet P-40, 1 mM EDTA, 1 mM DTT, 1 mM Na3VO4, 1 mM PMSF, 10 μg/ml leupeptin, 1 mM β-glycerophoshate, 1 mM Na-pyro-PO4, and 1% [vol/vol] aprotinin) immediately followed by homogenization. Lysates were incubated on ice for 30 minutes, followed by 30 minutes of centrifugation at 16,000 × g. A portion of the supernatant was saved for protein determination, before the addition of 4× Laemmli sample buffer (0.25M Tris-HCl pH 6.8, 8% [wt/vol] SDS, 40% [vol/vol] glycerol, 0.4 M DTT and 0.04% [wt/vol] Bromophenol Blue). Total protein was assessed by the Bio-Rad DC Protein Assay kit (Bio-Rad, Hercules, CA) according to manufacturer's instructions. Phospho c-Jun (P-c-Jun), c-Jun, and β-actin protein abundance was evaluated by Western blotting.
TGF-β1 Immunohistochemistry
TGF-β1 staining was performed on lung sections after antigen retrieval by incubation of slides for 20 minutes in 0.01 M sodium citrate pH 6.0 at 95°C. Slides were then blocked with 2% normal goat serum for 30 minutes. Successive incubations in avidin for 20 minutes and biotin for 20 minutes were then performed to eliminate endogenous biotin activity. Sections were then incubated with polyclonal rabbit antibody against TGF-β1 (1:100 dilutions; Santa Cruz Biotechnology, Santa Cruz, CA) overnight at 4°C. Biotinylated anti-rabbit IgG was then applied for 30 minutes at room temperature, followed by addition of the avidin-biotin-complex-alkaline phosphatase (Vectastain ABC-AP, Vector Laboratories, Burlingame, CA) for another 30 minutes at room temperature. After rinsing the sections in PBS, the substrate, Vector Red (Vector Laboratories), was added for 20 minutes. The Vector Red reacts with the bound alkaline phosphatase, producing an intense red color.
Assessment of Pulmonary Fibrosis
Lung sections of 5 μm were stained with picosirius red reagent that selectively stains collagen, and were visualized under polarized light (28). Slides were scored using a scale of 0 to 3 (0 being the least stain intensity, 3 the highest intensity) for airway-associated collagen deposition by two independent, blinded investigators. The cumulative score from each mouse was then averaged according to treatment group. Total lung collagen was measured in the upper right lobe of the lung after overnight digestion with 10 mg pepsin in 0.5 M acetic acid using the Sircol Assay (Accurate Chemical and Scientific Corp., Westbury, NY).
Measurement of Gene Expression
RNA was extracted from pulverized lung tissue by standard procedures. RNase protection assays were used to measure fibrotic or inflammatory gene expression using custom designed RNA templates (BD Pharmingen, San Diego, CA).
Bronchoalveolar Lavage Fluid Analyses
At the time of harvest, mouse lungs were lavaged once with 1 ml of sterile PBS. Resultant BAL fluid was then centrifuged at 2,000 rpm for 6 minutes to remove cells and debris and was then snap-frozen in liquid N2. BAL cytokine levels were determined by the Bioplex System and a 20-plex cytokine array (Bio-Rad Laboratories). Total TGF-β1 protein levels were determined by a Quantikine ELISA kit (R&D Systems), as directed by the manufacturer.
Evaluation of JNK1 Activity
JNK1 activity was assessed by an in vitro kinase assay as follows (29). JNK1 was immunoprecipitated from whole lung homogenates using anti-JNK1 antibody (Santa Cruz Biotechnology). Immunoprecipitated JNK1 was then incubated with GST-c-Jun fusion substrate protein in the presence of P32-ATP for 30 minutes at 30°C. Phosphorylated GST-c-Jun was then visualized by SDS-PAGE followed by autoradiography. Band intensity was quantified by measuring pixel density of the captured digital images using NIH Image J software.
Statistical Analyses
Data were analyzed by one-way ANOVA, using the Tukey test to adjust for multiple comparisons. Analyses with resultant P < 0.05 were accepted as statistically significant. All statistics were performed using the Microsoft Excel software package (Redmond, WA). Data from each experiment are presented as mean value ± SEM, and all experiments were repeated at least two times. Staining studies (airway inflammation, collagen deposition, TGF-β1, PAS, phospho-JNK, phospho-SMAD, and α-SMA) were conducted on lung sections from a minimum of three mice per group and a minimum of three airways per slide.
RESULTS
JNK Is Activated in the Airway Epithelium of Antigen-Sensitized and -Challenged Mice
To identify a role of JNK in allergic airway disease, C57BL/6 mice were sensitized and challenged with antigen, and phosphorylated JNK (phospho-JNK), which is reflective of JNK activation, was assessed by immunofluoresence. Phospho-JNK was largely localized to the airway epithelium of antigen-sensitized and -challenged mice (Figure 1A). Furthermore, evaluation of JNK1 activation in homogenized lung tissue, via an in vitro kinase assay demonstrated small increases in activity of JNK1 in mice subjected to sensitization and challenge with antigen (Figure 1B), although this increase was not statistically significant. These data show that JNK1 is activated in the mouse model of allergic airway disease, and that increases occur predominantly in the airway epithelium. The best known substrate for phosphorylation by JNK1 is c-Jun. We next determined whether phosphorylation of c-Jun was increased in lung homogenates from mice with allergic inflammation. Results in Figure 1C demonstrate slight increases in phospho-c-Jun in mice sensitized and challenged with antigen, as compared with the nonsensitized control group.
Figure 1.
Activation of c-Jun N-terminal kinase (JNK), and phosphorylation of c-Jun in lungs of mice with allergic airway or fibrotic lung disease. (A) Assessment of JNK phosphorylation in control or ovalbumin (Ova)-sensitized and -challenged (Ova/Ova) mice via assessment by confocal laser scanning cytometry. Red staining represents phospho-JNK, green staining depicts nuclei, and yellow denotes overlap (n = 4). Alum/Ova denotes mice that were not sensitized to ovalbumin (n = 4), but were challenged. (B) Assessment of JNK1 activity in homogenized lung tissue from Ova-challenged mice. JNK1 activity was determined using a JNK1-specific antibody by an in vitro kinase assay. Each lane represents results from an individual mouse. Top lane: JNK1-dependent phosphorylation of GST-c-Jun substrate in vitro. Lower lanes show total content of JNK1 and 2 by Western blotting as a loading control. Lower graph: Quantification of JNK activity in panel B by image analysis. (C) Evaluation of c-Jun phosphorylation in homogenized lung tissue from mice with Ova-induced allergic airway disease (n = 3). Lower lanes show total content of c-Jun and β-actin by Western blotting as loading controls. Numbers reflect fold increases in c-Jun phosphorylation over total c-Jun, compared with the respective control groups after densitometric evaluation of the Western blots.
Ova-Induced Allergic Airway Inflammation Is Enhanced in JNK1−/− Mice
To address the impact of gene deletion of JNK1 on allergic airway disease, wild-type (WT, C57BL/6) or JNK1−/− mice were sensitized and challenged with antigen. Antigen-induced inflammation measured by inflammatory cells in BAL fluid was significantly higher in JNK1−/− compared with WT mice (184.2 ± 48.8 versus 100.1 ± 18.8 cells/ml, P < 0.05), and increased numbers of eosinophils and lymphocytes were observed in JNK1−/− mice in response to antigen, compared with WT mice (Figure 2A), although profiles of peribronchial inflammation were similar in WT and JNK1−/− mice (Figure 2B). Analyses of mRNA expression of proinflammatory mediators in lung tissue in mice subjected to antigen demonstrated increases in IL-2, -5, -10, and -13 mRNA compared with sham-sensitized controls (Figure 3A). Similar increases in mRNA expression were observed in antigen-exposed JNK1−/− mice, although decreased mRNA expression of IL-10 was observed compared with WT mice. As expected, levels of inflammatory cytokines in the BAL fluid were markedly elevated in WT mice in response to antigen (Figure 3B), and more pronounced increases in content of IL-1α, IL-5, IL-6, G-CSF, and GM-CSF occurred in JNK1−/− mice subjected to antigen compared with WT mice. These data indicate that antigen-induced inflammation is worsened in JNK1−/− mice compared with WT controls.
Figure 2.
Evaluation of airway inflammation after Ova sensitization and challenge in JNK1−/− and wild-type (WT) (C57BL/6) mice. (A) Inflammatory cell profile in bronchoalveolar lavage (BAL) fluid after Ova challenge. Alum/Ova denotes mice that were not sensitized to Ova (n = 11), but were challenged, Ova/Ova denotes Ova-sensitized and -challenged mice (n = 10 WT, 11 JNK1−/−). *P < 0.05, ANOVA versus Alum/Ova; †P < 0.05, ANOVA versus WT Ova/Ova. (B) Representative photographs of lung histopathology in Ova-challenged WT or JNK1−/− mice (n = 3) (magnification: ×200).
Figure 3.
Assessment of inflammatory mediators in lungs of WT or JNK1−/− mice subjected to sensitization and challenge with Ova. (A) mRNA expression of inflammatory cytokines in homogenized lung tissue from WT and JNK1−/− mice after sensitization and challenge with Ova. Alum/Ova denotes mice that were not sensitized to Ova (n = 3) but were challenged, Ova/Ova denotes Ova-sensitized and -challenged mice (n = 3). *P < 0.05, ANOVA versus Alum/Ova; †P < 0.05, ANOVA versus WT Ova/Ova. (B) Measurement of cytokines in BAL fluid in WT or JNK1−/− mice subjected to sensitization and challenge with Ova (n = 3 Alum/Ova, 4 Ova/Ova). *P < 0.05, ANOVA versus Alum/Ova controls; †P < 0.05, ANOVA between WT and JNK1−/− Ova/Ova groups.
Antigen-Induced Mucus Metaplasia Does Not Require JNK1
The development of mucus metaplasia represents a critical clinical manifestation of allergic airway disease in asthma (30). To determine whether JNK1 is required for mucus metaplasia, WT or JNK1−/− mice were sensitized and challenged with antigen and mucus levels were assessed by PAS staining. Antigen induced PAS positivity to a comparable extent in WT and JNK1−/− mice (Figures 4A and 4B), indicating that JNK1 is not essential for airway epithelial mucus production, consistent with our previous observations (25).
Figure 4.
Assessment of mucus metaplasia after Ova sensitization and challenge in JNK1−/− and WT (C57BL/6) mice. (A) Periodic Acid-Schiff staining of airway mucus after Ova sensitization and challenge (magnification: ×200). Alum/Ova denotes mice that were not sensitized to Ova (n = 4) but were challenged, Ova/Ova denotes Ova-sensitized and -challenged mice (n = 4). (B) Quantification of airway mucus staining intensity after scoring of slides by two blinded investigators (n = 4).
JNK1 Is Required for Antigen-Induced Fibrotic Gene Expression and Subepithelial Collagen Deposition
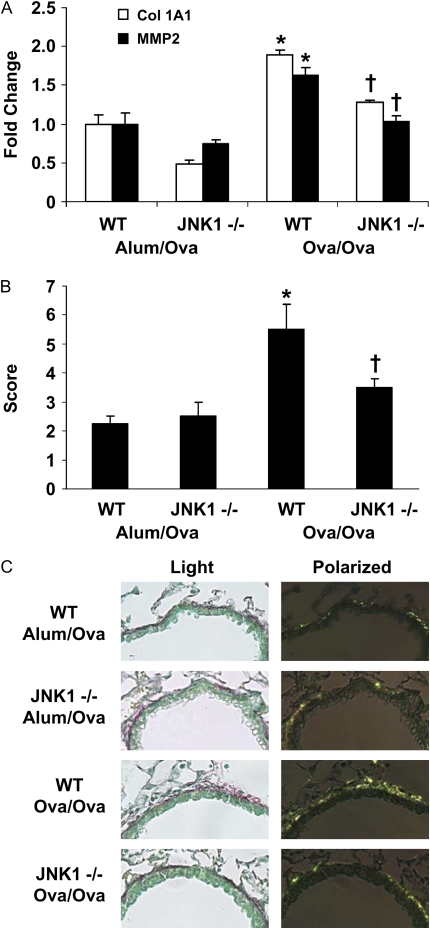
To test whether JNK1 is necessary for expression of profibrotic genes, total RNA was isolated in whole lung homogenates from antigen-exposed WT and JNK1−/− mice. Expression of collagen type 1a1 and matrix metalloproteinase (MMP) 2 mRNAs was increased by antigen in WT mice (Figure 5A). In contrast, significantly decreased expression of collagen type 1A1 and MMP2 mRNAs were apparent in JNK1−/− mice compared with WT mice, and these decreases were apparent both in sham-sensitized mice as well as after antigen challenge.
Figure 5.
Assessment of peribronchial fibrosis in WT and JNK1−/− mice subjected to sensitization and challenge with Ova. (A) mRNA expression of profibrotic mediators in lung homogenates from WT and JNK1−/− mice after sensitization and challenge with Ova. Alum/Ova denotes mice that were not sensitized to Ova (n = 3) but were challenged, Ova/Ova denotes Ova-sensitized and -challenged mice (n = 3). *P < 0.05 (ANOVA) versus Alum/Ova; †P < 0.05 (ANOVA) versus WT Ova/Ova. (B) Histologic scoring of subepithelial collagen deposition by blinded investigators (n = 4). *P < 0.05 ANOVA versus Alum/Ova; †P < 0.05 ANOVA versus WT Ova/Ova. (C) Representative images of subepithelial collagen deposition in lung sections stained with picosirius red, and visualized under polarized light microscopy (magnification: ×400). Note the increased subepithelial collagen staining in Ova/Ova WT mice, which is attenuated in JNK1−/− mice.
We next evaluated subepithelial collagen deposition, a feature of allergic airways disease (1). Lung sections from Ova-exposed WT or JNK1−/− mice were stained with picosirius red reagent, which selectively stains collagen, and were visualized under polarized light. While antigen induced significantly increased collagen deposition in WT mice, JNK1−/− mice sensitized and challenged with Ova failed to accumulate increased subepithelial collagen content (Figures 5B and 5C), illustrating the functional importance of JNK1 in antigen-induced subepithelial fibrosis.
TGF-β1 Expression Is Similar in Control and JNK1-Null Mice
Since TGF-β1 has been shown to be critical to the induction of subepithelial fibrosis in the lung (4, 5), we examined the expression of TGF-β1 protein in the lungs of WT and JNK1−/− mice. Immunohistochemistry revealed that TGF-β1 was highly expressed in the airway epithelium of sham-sensitized WT or JNK1−/− mice (Figure 6A). In antigen-sensitized and -challenged WT or JNK1−/− mice, TGF-β1 expression in airway epithelium was markedly decreased, presumably indicating secretion of the protein, as previously reported (31). After antigen sensitization and challenge, TGF-β1 levels were significantly increased in the BAL fluid of both WT and JNK1−/− mice (Figure 6B), although diminutions of TGF-β1 levels in BAL were apparent in JNK1−/− mice compared with WT animals.
Figure 6.
Expression of TGF-β1 in lungs of control WT or JNK1−/− mice, and after sensitization and challenge with Ova. (A) Evaluation of TGF-β1 protein content via immunohistochemistry in Ova-challenged mice (magnification: ×200). Alum/Ova denotes mice that were not sensitized to Ova (n = 4) but were challenged, Ova/Ova denotes Ova-sensitized and -challenged mice (n = 4). (B) TGF-β1 protein in BAL fluid from WT or JNK1−/− mice after Ova challenge, as measured by ELISA. *P < 0.05 (ANOVA) versus Alum/Ova; †P < 0.05 (ANOVA) versus WT Ova/Ova.
JNK1 Is Required for Expression of Profibrotic Genes Induced by TGF-β1 Instillation
Previous work from this laboratory has shown that JNK1 is required for TGF-β1–induced profibrotic gene expression and EMT in primary airway epithelial cells (25). To directly test whether JNK1 is required for TGF-β1–induced profibrotic signaling in vivo, we evaluated the extent of profibrotic gene expression in WT and JNK1−/− mice after TGF-β1 instillation. While TGF-β1 caused increased expression of pro-fibrotic genes in whole lung homogenates from WT mice, these increases were not observed in mice lacking JNK1 (Figure 7A). Evaluation of the mesenchymal protein, α-smooth muscle actin (α-SMA), in situ demonstrated marked increased in α-SMA immunoreactivity in the bronchial epithelium and parenchyma of WT mice that received TGF-β1. In contrast, increases in α-SMA reactivity were almost completely abrogated in JNK1−/− mice exposed to TGF-β1 (Figure 7B). In aggregate, these data demonstrate that JNK1−/− mice have attenuated responsiveness to the profibrotic cytokine TGF-β1 in vivo.
Figure 7.
Assessment of profibrotic mediators in lung tissue from WT or JNK1−/− mice after administration of TGF-β1. (A) mRNA expression of profibrotic mediators in lung homogenates from WT and JNK1−/− mice after administration of TGF-β1. Results were obtained via real-time PCR analyses, and data expressed as fold change from PBS controls (n = 3). *P < 0.05 (ANOVA) compared with the WT TGF-β1 group. Col 1A1, collagen type 1A1; α-SMA, α-smooth muscle actin; PAI 1, plasminogen activator inhibitor 1. (B) Evaluation of α-SMA expression in lung tissue from WT or JNK1−/− mice after administration of TGF-β1, via confocal laser scanning microscopy (n = 2 PBS, 3 TGF-β1) (magnification: ×200). Red denotes α-SMA, green denotes pan-cytokeratin, and yellow indicates overlap in fluorophores.
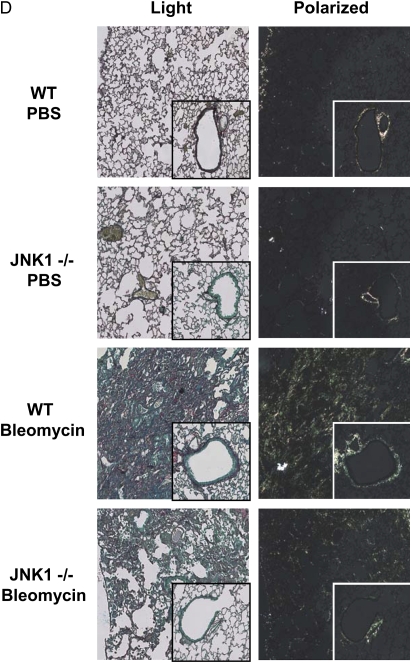
JNK1 Is Required for Bleomycin-Induced Pulmonary Lung Fibrosis
Administration of the chemotherapeutic drug, bleomycin, represents a well-characterized model of pulmonary fibrosis in mice (32, 33), and bleomycin-induced fibrosis requires TGF-β1 signaling (34, 35). We therefore assessed whether JNK1 is also required for bleomycin-induced fibrosis. Deletion of JNK1 had no impact on recruitment of inflammatory cells observed after administration of bleomycin (Figure 8A). As expected instillation of bleomycin into lungs of WT mice resulted in enhanced collagen content (Figure 8B). However, the overall content of collagen in lungs of JNK1−/− mice in response to bleomycin was significantly lower compared with WT mice. We also observed that collagen content in JNK1−/− controls that received PBS was lower than WT mice subjected to PBS administration. Analysis of lung histopathology also demonstrated a decrease in total lung collagen accumulation, and subepithelial collagen deposition in JNK1−/− mice versus WT controls (Figures 8C and 8D), demonstrating that JNK1 is required for bleomycin-induced pulmonary fibrosis.
Figure 8.
Assessment of bleomycin-induced fibrosis in WT and JNK1−/− mice. (A) Differential cell counts in BAL from WT or JNK1−/− mice 21 days after administration of PBS or bleomycin (n = 7, 6, 4, 5, respectively). (B) Assessment of total collagen content in the upper right lobe of mice after administration of bleomycin (n = 7, 6, 5, 6, respectively). *P < 0.05 (ANOVA) versus PBS; †P < 0.05 (ANOVA) versus WT bleomycin. (C) Scoring of subepithelial collagen deposition in lung sections from bleomycin treated WT or JNK1−/− mice that were stained with Picosirius red (n = 4, 6, 3, 6, respectively). *P < 0.05 (ANOVA) versus PBS; †P < 0.05 ANOVA versus WT bleomycin. (D) Visualization of collagen deposition in lung sections from bleomycin-exposed WT or JNK1−/− mice (magnification: ×100) after staining with picosirius red, and visualization under polarized light (n = 4, 6, 3, 6, respectively). Note the marked collagen deposition in parenchymal regions in WT mice exposed to bleomycin, and diminution of reactivity in JNK1−/− mice. Inset: Evaluation of collagen deposition in subepithelial regions.
Proximal TGF-β1 Pathway Activation Is Not Altered in JNK1−/− Airways
JNK1 has previously been implicated in the facilitation of TGF-β1 signaling, via multiple potential mechanisms (25, 36, 37). Exposure of cells to TGF-β1 results in phosphorylation of the receptor Smad, Smad2 via activation of TGF-β1 receptor I. Evaluation of lung sections from WT and JNK1−/− mice subjected to sensitization and challenge with antigen, or to administration of TGF-β1, demonstrated significant increases in phosphorylation of Smad2 that were similar in WT and JNK1−/− mice (Figure 9), similar to previous results in primary tracheal epithelial cell cultures (pixel densities: 18.8 ± 1.1 versus 27.0 ± 1.2 for WT, 21.0 ± 1.9 versus 24.2 ± 1.5 for JNK1−/− in the Ova study; 23.3 ± 1.8 versus 28.5 ± 1.9 for WT, 16.6 ± 1.4 versus 31.1 ± 1.3 for JNK1 −/− in the TGF-β1 study) (25). These data suggest that proximal TGF-β1 receptor induced signaling is intact in the absence of JNK1, and that the attenuation of fibrogenesis may occur either independent or downstream of Smad phosphorylation.
Figure 9.
Assessment of proximal activation of the TGF-β1 pathway in WT or JNK1−/− mice subjected to sensitization and challenge with Ova or administration of TGF-β1. Immunofluorescence staining for phosphorylation of Smad2 was assessed in situ via immunofluorescence and confocal laser scanning microscopy (magnification: ×200). Red signal represents phospho-Smad2, green signal depicts nuclei. Alum/Ova denotes mice that were not sensitized to Ova (n = 4) but were challenged with Ova; Ova/Ova denotes Ova-sensitized and -challenged mice (n = 4). PBS denotes mice that were instilled with PBS plus vehicle, 4 mM HCl (n = 4), while TGF-β1 represents mice exposed to TGF-β1.
DISCUSSION
The molecular mechanisms responsible for the increases in collagen deposition in lungs from patients with pulmonary diseases that include asthma, COPD, and IPF remain unclear. The TGF-β1 signaling pathway has been highlighted as cardinal mediator in these processes, although it is likely that additional contributing molecular cascades remain unidentified. In this study, we reveal the pivotal and functional importance of the JNK1 signaling pathway in augmenting the expression of profibrotic mediators and fibrosis in three distinct model systems. Specifically we demonstrate here that JNK1−/− mice were substantially protected against antigen, bleomycin, and TGF-β1–induced profibrotic mediator expression and fibrosis compared with WT animals. In each of these models, TGF-β1 signaling has been shown to be required for the fibrotic phenotype (34, 38).
Multiple observations highlight the importance of TGF-β as a key regulator of airway remodeling and fibrosis (39). A TGF-β1 promoter polymorphism has been associated with asthma susceptibility (40). Patients with asthma express higher levels of TGF-β1, IL-4, and IL-13 after segmental allergen challenge (41), and TGF-β1 levels correlate directly to airway basement membrane thickness (42). Administration or overexpression of IL-13 in airways is sufficient to elicit fibrosis, which has been attributed to the activation of latent TGF-β1 (43), and overexpression of active TGF-β1 itself is sufficient to cause pulmonary fibrosis (44). TGF-β stimulates production of additional growth factors, collagen, and MMPs (39, 45), which play key roles in airway fibrosis and remodeling, characteristic of allergic airway disease and IPF. The source of TGF-β in lung tissue and the cells that respond to TGF-β1 during the pathogenesis of tissue fibrosis is unclear, and likely depend on the nature or locale of the insults. Expression of TGF-β occurs in the bronchial epithelium and submucosa of patients with asthma, chronic bronchitis, and fibrosis (42, 46). In mice and humans with IPF, the airway epithelium has been suggested to be a major source of TGF-β1 (47, 48), although other studies have reported that eosinophils and fibroblasts are a source of TGF-β1 in allergic airway disease (13, 49, 50). In the present study, TGF-β1 expression was largely observed within the airway epithelium of control mice, while after sensitization and challenge with antigen, TGF-β1 content diminished, perhaps indicating release of the protein, as previously observed (31). Regardless of the cell type that produces TGF-β, the role of this cytokine in promoting fibrosis is clear.
Active TGF-β initiates signaling via binding to its heterodimeric receptor and subsequent TGF-β receptor I (ALK5)-induced phosphorylation of receptor Smads (rSmads), including Smad2 and 3 in the carboxyterminal region (51). Phospho-Smad2 or 3 then associate with the co-activator Smad, Smad4, to form the TGF-β−induced transcriptional regulatory complex. Evidence of increases in Smad phosphorylation in lung disease has been reported. Elevated phospho-Smad2 levels occur in bronchial epithelium and fibroblasts of individuals with asthma (6, 52), and increases in Smad2 phosphorylation in the epithelium, endothelium, smooth muscle, and fibroblasts occur in the Ova model of allergic airway disease (38, 53, 54). The functional significance of Smads as downstream effectors of TGF-β1 signaling is apparent from knockout studies, as Smad3-null mice are resistant to TGF-β1–induced pulmonary fibrosis (55). Embryonic fibroblasts from Smad3-null mice fail to auto-induce TGF-β, and also do not induce c-jun and c-fos in response to TGF-β, the latter genes being important in the regulation of collagen production (56), and similar observations have been made in cells lacking Smad2 (57, 58).
Numerous studies underscore the potential role for JNK1 in fibrosis. As was mentioned above, elevated phosphorylation of JNK is present in the airway epithelium and pulmonary endothelium from patients with IPF (23, 24) and in mice subjected to bleomycin-induced fibrosis (24). Constitutive activation of JNK in fibrotic lung fibroblasts is important in the activation and autocrine regulation of endothelin-1, a critical molecule in the induction of matrix protein production (59). JNK1 activation occurs as a result of decreases in expression of caveolin-1, which is a critical event in the pathogenesis of pulmonary fibrosis (24). The present study, which demonstrates the requirement of JNK1 in pulmonary fibrosis, in multiple TGF-β1–dependent models, suggests that JNK1 intersects with the TGF-β1 pathway. Indeed, numerous reports suggest that the activation of JNK1 regulates the outcome of TGF-β1 signaling. TGF-β1 and 3 can directly stimulate activation of JNK via a phosphorylation-dependent mechanism (60, 61). JNK phosphorylation has been suggested to require TGF-β receptor II, but not TGF-β receptor I, and may involve phosphoinositol-3 kinase, TGF-β–activated kinase, and Rho kinase activity (60, 62–64). JNK in turn has been linked to phosphorylation of Smad2/3, and is required for TGF-β−induced transcriptional activation (24, 63, 65). A recent study highlighted that JNK can phosphorylate Smad2 and 3 in linker domains at proline-flanked serines, and that linker phosphorylation promotes the association of Smad2/3 with Smad4 and augments PAI-1 expression (36). Furthermore, Smad3 can also cooperate with c-Jun, a known target of JNK, to activate TGF-β−induced transcription (66), although c-Jun–dependent, but Smad-independent regulation of fibronectin expression is also apparent (67). Altogether, these studies indicate a requirement for JNK in the augmentation of TGF-β−induced transcription of mesenchymal effector genes, and they also highlight the possibility that this may occur through multiple phosphorylation events. It is important to point out that collagen content, Col 1A1 mRNA expression, and TGF-β1 levels were lower in control JNK1−/− mice, as compared with littermate controls, suggesting that intrinsic mechanistic links exist between JNK1 and the collagen pathway, which will require additional studies to unravel. It is tempting to speculate that lowered TGF-β1 content in JNK1−/− mice dampens the extent of collagen deposition. A recent study that demonstrated the development of pulmonary fibrosis as a result of transgenic expression the Fos-related antigen-2 (Fra-2) (68), a member of the AP-1 transcription factor family, highlights the alternative possibility that JNK1 may control fibrogenesis via its well-known ability to regulate the function of AP1, a scenario that also remains to be tested.
Despite the requirement for JNK1 in promoting collagen deposition in response to antigen, JNK1−/− mice produced elevated levels of TGF-β1, and induced similar levels of phospho-Smad2 compared with WT mice, indicative of unimpaired proximal TGF-β1 signaling. These data suggest that in the Ova model, JNK1 may function in parallel with, or downstream to TGF-β1 receptor activation. The latter possibility is consistent with our previous observations in tracheal epithelial cells which demonstrated that in the absence of JNK1, TGF-β1–induced Smad carboxyterminal phosphorylation and nuclear translocation were intact, but that binding of Smad complexes to the Smad DNA response element was diminished, suggesting that the TGF-β1 pathway was affected in JNK1−/− cells distal to Smad carboxyterminal phosphorylation (25). These data are in direct contrast to a recent study in lung fibroblasts which demonstrated that absence of JNK1 decreased TGF-β1–induced carboxyterminal phosphorylation of rSmads (24). The reasons for these disparate observations remain to be unraveled, but may reflect cell type–specific responses to TGF-β1.
We recently demonstrated, using primary cultures of mouse tracheal epithelial cells, that JNK1 was required for TGF-β1–induced EMT (25). In the current study we demonstrate that JNK1−/− mice fail to induce mesenchymal protein markers such as collagen type 1A1 and α-SMA in vivo. TGF-β1 administration to WT mice induced marked reactivity of α-SMA in airway epithelial cells, indicative of epithelial plasticity associated with EMT. Significantly, this response was largely absent in lung from JNK1−/− mice. The emerging role of EMT in pulmonary fibrosis has recently been suggested (69, 70), and compelling observations that EMT occurs in the bleomycin model of fibrosis that were based upon lineage tracing have been published (71). However, recent studies have failed to support a role for EMT in IPF or the bleomycin model of fibrosis (72). The reasons for these discrepancies are unclear and warrant further investigation. It is interesting to speculate that the JNK plays a role in the pathogenesis of fibrosis in the mouse models used here by promoting EMT.
The data presented in this study identify a novel molecular pathway involved in the pathogenesis of fibrosis. Using separate models that cause increases in collagen deposition through unique mediators, we demonstrate the requirement of JNK1 in profibrotic gene expression and subepithelial collagen deposition. Additional work will be required to elucidate the mechanistic link between TGF-β1 and JNK1 signaling cascades in the lung, and to unveil the significance of JNK1 and EMT in vivo. Unraveling of these molecular details may offer novel therapeutic targets for treatment of pulmonary fibrosis, a progressive disease that currently lacks effective or curative therapy.
Acknowledgments
The authors dedicate this manuscript to the memory of Dr. Kenneth Cutroneo, a beloved mentor and colleague, whose scientific career laid the foundation for the present study. The authors thank the University of Vermont Cell Imaging and DNA Facilities for assistance with confocal laser scanning microscopy and performing the Taqman analyses, Stacie Beuschel for animal breeding and technical assistance, and Joshua Holt for providing technical assistance.
This work was supported by National Institutes of Health grants R01 HL-60014 (Y.J.-H.), R01 HL-079331 (Y.J.-H.), F32 HL-082121 (J.F.A.), and P20 RL 15557 NCRR COBRE (C.G.I.).
Originally Published in Press as DOI: 10.1165/rcmb.2008-0174OC on October 3, 2008
Conflict of Interest Statement: None of the authors has a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Elias JA, Zhu Z, Chupp G, Homer RJ. Airway remodeling in asthma. J Clin Invest 1999;104:1001–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boxall C, Holgate ST, Davies DE. The contribution of transforming growth factor-beta and epidermal growth factor signalling to airway remodelling in chronic asthma. Eur Respir J 2006;27:208–229. [DOI] [PubMed] [Google Scholar]
- 3.Ask K, Martin GE, Kolb M, Gauldie J. Targeting genes for treatment in idiopathic pulmonary fibrosis: challenges and opportunities, promises and pitfalls. Proc Am Thorac Soc 2006;3:389–393. [DOI] [PubMed] [Google Scholar]
- 4.Leask A, Abraham DJ. TGF-beta signaling and the fibrotic response. FASEB J 2004;18:816–827. [DOI] [PubMed] [Google Scholar]
- 5.Sheppard D. Transforming growth factor beta: a central modulator of pulmonary and airway inflammation and fibrosis. Proc Am Thorac Soc 2006;3:413–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sagara H, Okada T, Okumura K, Ogawa H, Ra C, Fukuda T, Nakao A. Activation of TGF-beta/Smad2 signaling is associated with airway remodeling in asthma. J Allergy Clin Immunol 2002;110:249–254. [DOI] [PubMed] [Google Scholar]
- 7.Davies DE, Wicks J, Powell RM, Puddicombe SM, Holgate ST. Airway remodeling in asthma: new insights. J Allergy Clin Immunol 2003;111:215–225. (quiz 226). [DOI] [PubMed] [Google Scholar]
- 8.Wynn TA. Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat Rev Immunol 2004;4:583–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wills-Karp M. Interleukin-13 in asthma pathogenesis. Immunol Rev 2004;202:175–190. [DOI] [PubMed] [Google Scholar]
- 10.Maher TM, Wells AU, Laurent GJ. Idiopathic pulmonary fibrosis: multiple causes and multiple mechanisms? Eur Respir J 2007;30:835–839. [DOI] [PubMed] [Google Scholar]
- 11.Bringardner BD, Baran CP, Eubank TD, Marsh CB. The role of inflammation in the pathogenesis of idiopathic pulmonary fibrosis. Antioxid Redox Signal 2008;10:287–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chetta A, Foresi A, Del Donno M, Bertorelli G, Pesci A, Olivieri D. Airways remodeling is a distinctive feature of asthma and is related to severity of disease. Chest 1997;111:852–857. [DOI] [PubMed] [Google Scholar]
- 13.Minshall EM, Leung DY, Martin RJ, Song YL, Cameron L, Ernst P, Hamid Q. Eosinophil-associated TGF-beta1 mRNA expression and airways fibrosis in bronchial asthma. Am J Respir Cell Mol Biol 1997;17:326–333. [DOI] [PubMed] [Google Scholar]
- 14.Ramos-Barbon D, Ludwig MS, Martin JG. Airway remodeling: lessons from animal models. Clin Rev Allergy Immunol 2004;27:3–21. [DOI] [PubMed] [Google Scholar]
- 15.Boulet L, Belanger M, Carrier G. Airway responsiveness and bronchial-wall thickness in asthma with or without fixed airflow obstruction. Am J Respir Crit Care Med 1995;152:865–871. [DOI] [PubMed] [Google Scholar]
- 16.Hoshino M, Nakamura Y, Sim JJ. Expression of growth factors and remodelling of the airway wall in bronchial asthma. Thorax 1998;53:21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson GL, Nakamura K. The c-jun kinase/stress-activated pathway: regulation, function and role in human disease. Biochim Biophys Acta 2007;1773:1341–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smeal T, Binetruy B, Mercola DA, Birrer M, Karin M. Oncogenic and transcriptional cooperation with Ha-Ras requires phosphorylation of c-Jun on serines 63 and 73. Nature 1991;354:494–496. [DOI] [PubMed] [Google Scholar]
- 19.Dong C, Yang DD, Wysk M, Whitmarsh AJ, Davis RJ, Flavell RA. Defective T cell differentiation in the absence of Jnk1. Science 1998;282:2092–2095. [DOI] [PubMed] [Google Scholar]
- 20.Sousa AR, Lane SJ, Soh C, Lee TH. In vivo resistance to corticosteroids in bronchial asthma is associated with enhanced phosyphorylation of JUN N-terminal kinase and failure of prednisolone to inhibit JUN N-terminal kinase phosphorylation. J Allergy Clin Immunol 1999;104:565–574. [DOI] [PubMed] [Google Scholar]
- 21.Eynott PR, Xu L, Bennett BL, Noble A, Leung SY, Nath P, Groneberg DA, Adcock IM, Chung KF. Effect of an inhibitor of Jun N-terminal protein kinase, SP600125, in single allergen challenge in sensitized rats. Immunology 2004;112:446–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nath P, Eynott P, Leung SY, Adcock IM, Bennett BL, Chung KF. Potential role of c-Jun NH2-terminal kinase in allergic airway inflammation and remodelling: effects of SP600125. Eur J Pharmacol 2005;506:273–283. [DOI] [PubMed] [Google Scholar]
- 23.Yoshida K, Kuwano K, Hagimoto N, Watanabe K, Matsuba T, Fujita M, Inoshima I, Hara N. MAP kinase activation and apoptosis in lung tissues from patients with idiopathic pulmonary fibrosis. J Pathol 2002;198:388–396. [DOI] [PubMed] [Google Scholar]
- 24.Wang XM, Zhang Y, Kim HP, Zhou Z, Feghali-Bostwick CA, Liu F, Ifedigbo E, Xu X, Oury TD, Kaminski N, et al. Caveolin-1: a critical regulator of lung fibrosis in idiopathic pulmonary fibrosis. J Exp Med 2006;203:2895–2906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alcorn JF, Guala AS, van der Velden J, McElhinney B, Irvin CG, Davis RJ, Janssen-Heininger YM. Jun N-terminal kinase 1 regulates epithelial-to-mesenchymal transition induced by TGF-{beta}1. J Cell Sci 2008;121:1036–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kenyon NJ, Ward RW, McGrew G, Last JA. TGF-beta1 causes airway fibrosis and increased collagen I and III mRNA in mice. Thorax 2003;58:772–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fujita M, Shannon JM, Morikawa O, Gauldie J, Hara N, Mason RJ. Overexpression of tumor necrosis factor-alpha diminishes pulmonary fibrosis induced by bleomycin or transforming growth factor-beta. Am J Respir Cell Mol Biol 2003;29:669–676. [DOI] [PubMed] [Google Scholar]
- 28.Junquiera LC, Junqueira LC, Brentani RR. A simple and sensitive method for the quantitative estimation of collagen. Anal Biochem 1979;94:96–99. [DOI] [PubMed] [Google Scholar]
- 29.Pantano C, Shrivastava P, McElhinney B, Janssen-Heininger Y. Hydrogen peroxide signaling through tumor necrosis factor receptor 1 leads to selective activation of c-Jun N-terminal kinase. J Biol Chem 2003;278:44091–44096. [DOI] [PubMed] [Google Scholar]
- 30.Morcillo EJ, Cortijo J. Mucus and MUC in asthma. Curr Opin Pulm Med 2006;12:1–6. [DOI] [PubMed] [Google Scholar]
- 31.Alcorn JF, Rinaldi LM, Jaffe EF, van Loon M, Bates JH, Janssen-Heininger YM, Irvin CG. Transforming growth factor-beta1 suppresses airway hyperresponsiveness in allergic airway disease. Am J Respir Crit Care Med 2007;176:974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moeller A, Ask K, Warburton D, Gauldie J, Kolb M. The bleomycin animal model: a useful tool to investigate treatment options for idiopathic pulmonary fibrosis? Int J Biochem Cell Biol 2008;40:362–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chua F, Gauldie J, Laurent GJ. Pulmonary fibrosis: searching for model answers. Am J Respir Cell Mol Biol 2005;33:9–13. [DOI] [PubMed] [Google Scholar]
- 34.Cutroneo KR, White SL, Phan SH, Ehrlich HP. Therapies for bleomycin induced lung fibrosis through regulation of TGF-beta1 induced collagen gene expression. J Cell Physiol 2007;211:585–589. [DOI] [PubMed] [Google Scholar]
- 35.Zhao J, Shi W, Wang YL, Chen H, Bringas P Jr, Datto MB, Frederick JP, Wang XF, Warburton D. Smad3 deficiency attenuates bleomycin-induced pulmonary fibrosis in mice. Am J Physiol Lung Cell Mol Physiol 2002;282:L585–L593. [DOI] [PubMed] [Google Scholar]
- 36.Mori S, Matsuzaki K, Yoshida K, Furukawa F, Tahashi Y, Yamagata H, Sekimoto G, Seki T, Matsui H, Nishizawa M, et al. TGF-beta and HGF transmit the signals through JNK-dependent Smad2/3 phosphorylation at the linker regions. Oncogene 2004;23:7416–7429. [DOI] [PubMed] [Google Scholar]
- 37.Hocevar BA, Prunier C, Howe PH. Disabled-2 (Dab2) mediates transforming growth factor beta (TGFbeta)-stimulated fibronectin synthesis through TGFbeta-activated kinase 1 and activation of the JNK pathway. J Biol Chem 2005;280:25920–25927. [DOI] [PubMed] [Google Scholar]
- 38.McMillan SJ, Xanthou G, Lloyd CM. Manipulation of allergen-induced airway remodeling by treatment with anti-TGF-beta antibody: effect on the Smad signaling pathway. J Immunol 2005;174:5774–5780. [DOI] [PubMed] [Google Scholar]
- 39.Bartram U, Speer CP. The role of transforming growth factor beta in lung development and disease. Chest 2004;125:754–765. [DOI] [PubMed] [Google Scholar]
- 40.Silverman ES, Palmer LJ, Subramaniam V, Hallock A, Mathew S, Vallone J, Faffe DS, Shikanai T, Raby BA, Weiss ST, et al. Transforming growth factor-beta1 promoter polymorphism C-509T is associated with asthma. Am J Respir Crit Care Med 2004;169:214–219. [DOI] [PubMed] [Google Scholar]
- 41.Batra V, Musani AI, Hastie AT, Khurana S, Carpenter KA, Zangrilli JG, Peters SP. Bronchoalveolar lavage fluid concentrations of transforming growth factor (TGF)-beta1, TGF-beta2, interleukin (IL)-4 and IL-13 after segmental allergen challenge and their effects on alpha-smooth muscle actin and collagen III synthesis by primary human lung fibroblasts. Clin Exp Allergy 2004;34:437–444. [DOI] [PubMed] [Google Scholar]
- 42.Vignola AM, Chanez P, Chiappara G, Merendino A, Pace E, Rizzo A, la Rocca AM, Bellia V, Bonsignore G, Bousquet J. Transforming growth factor-beta expression in mucosal biopsies in asthma and chronic bronchitis. Am J Respir Crit Care Med 1997;156:591–599. [DOI] [PubMed] [Google Scholar]
- 43.Lee CG, Homer RJ, Zhu Z, Lanone S, Wang X, Koteliansky V, Shipley JM, Gotwals P, Noble P, Chen Q, et al. Interleukin-13 induces tissue fibrosis by selectively stimulating and activating transforming growth factor beta(1). J Exp Med 2001;194:809–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee CG, Cho SJ, Kang MJ, Chapoval SP, Lee PJ, Noble PW, Yehualaeshet T, Lu B, Flavell RA, Milbrandt J, et al. Early growth response gene 1-mediated apoptosis is essential for transforming growth factor beta1-induced pulmonary fibrosis. J Exp Med 2004;200:377–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coker RK, Laurent GJ, Shahzeidi S, Lympany PA, du Bois RM, Jeffery PK, McAnulty RJ. Transforming growth factors-beta 1, -beta 2, and -beta 3 stimulate fibroblast procollagen production in vitro but are differentially expressed during bleomycin-induced lung fibrosis. Am J Pathol 1997;150:981–991. [PMC free article] [PubMed] [Google Scholar]
- 46.Coker RK, Laurent GJ, Jeffery PK, du Bois RM, Black CM, McAnulty RJ. Localisation of transforming growth factor beta1 and beta3 mRNA transcripts in normal and fibrotic human lung. Thorax 2001;56:549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kumar RK, Herbert C, Foster PS. Expression of growth factors by airway epithelial cells in a model of chronic asthma: regulation and relationship to subepithelial fibrosis. Clin Exp Allergy 2004;34:567–575. [DOI] [PubMed] [Google Scholar]
- 48.Khalil N, O'Connor RN, Flanders KC, Unruh H. TGF-beta 1, but not TGF-beta 2 or TGF-beta 3, is differentially present in epithelial cells of advanced pulmonary fibrosis: an immunohistochemical study. Am J Respir Cell Mol Biol 1996;14:131–138. [DOI] [PubMed] [Google Scholar]
- 49.Tanaka H, Komai M, Nagao K, Ishizaki M, Kajiwara D, Takatsu K, Delespesse G, Nagai H. Role of interleukin-5 and eosinophils in allergen-induced airway remodeling in mice. Am J Respir Cell Mol Biol 2004;31:62–68. [DOI] [PubMed] [Google Scholar]
- 50.Cho JY, Miller M, Baek KJ, Han JW, Nayar J, Lee SY, McElwain K, McElwain S, Friedman S, Broide DH. Inhibition of airway remodeling in IL-5-deficient mice. J Clin Invest 2004;113:551–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Derynck R, Zhang YE. Smad-dependent and Smad-independent pathways in TGF-beta family signalling. Nature 2003;425:577–584. [DOI] [PubMed] [Google Scholar]
- 52.Phipps S, Benyahia F, Ou TT, Barkans J, Robinson DS, Kay AB. Acute allergen-induced airway remodeling in atopic asthma. Am J Respir Cell Mol Biol 2004;31:626–632. [DOI] [PubMed] [Google Scholar]
- 53.Rosendahl A, Checchin D, Fehniger TE, ten Dijke P, Heldin CH, Sideras P. Activation of the TGF-beta/activin-Smad2 pathway during allergic airway inflammation. Am J Respir Cell Mol Biol 2001;25:60–68. [DOI] [PubMed] [Google Scholar]
- 54.Kelly MM, Leigh R, Bonniaud P, Ellis R, Wattie J, Smith MJ, Martin G, Panju M, Inman MD, Gauldie J. Epithelial expression of profibrotic mediators in a model of allergen-induced airway remodeling. Am J Respir Cell Mol Biol 2005;32:99–107. [DOI] [PubMed] [Google Scholar]
- 55.Bonniaud P, Kolb M, Galt T, Robertson J, Robbins C, Stampfli M, Lavery C, Margetts PJ, Roberts AB, Gauldie J. Smad3 null mice develop airspace enlargement and are resistant to TGF-beta-mediated pulmonary fibrosis. J Immunol 2004;173:2099–2108. [DOI] [PubMed] [Google Scholar]
- 56.Roberts AB, Piek E, Bottinger EP, Ashcroft G, Mitchell JB, Flanders KC. Is Smad3 a major player in signal transduction pathways leading to fibrogenesis? Chest 2001;120:43S–47S. [DOI] [PubMed] [Google Scholar]
- 57.Kasai H, Allen JT, Mason RM, Kamimura T, Zhang Z. TGF-beta1 induces human alveolar epithelial to mesenchymal cell transition (EMT). Respir Res 2005;6:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Piek E, Ju WJ, Heyer J, Escalante-Alcalde D, Stewart CL, Weinstein M, Deng C, Kucherlapati R, Bottinger EP, Roberts AB. Functional characterization of transforming growth factor beta signaling in Smad2- and Smad3-deficient fibroblasts. J Biol Chem 2001;276:19945–19953. [DOI] [PubMed] [Google Scholar]
- 59.Shi-Wen X, Rodriguez-Pascual F, Lamas S, Holmes A, Howat S, Pearson JD, Dashwood MR, du Bois RM, Denton CP, Black CM, et al. Constitutive ALK5-independent c-Jun N-terminal kinase activation contributes to endothelin-1 overexpression in pulmonary fibrosis: evidence of an autocrine endothelin loop operating through the endothelin A and B receptors. Mol Cell Biol 2006;26:5518–5527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yue J, Sun B, Liu G, Mulder KM. Requirement of TGF-beta receptor-dependent activation of c-Jun N-terminal kinases (JNKs)/stress-activated protein kinases (Sapks) for TGF-beta up-regulation of the urokinase-type plasminogen activator receptor. J Cell Physiol 2004;199:284–292. [DOI] [PubMed] [Google Scholar]
- 61.Hayashida T, Poncelet AC, Hubchak SC, Schnaper HW. TGF-beta1 activates MAP kinase in human mesangial cells: a possible role in collagen expression. Kidney Int 1999;56:1710–1720. [DOI] [PubMed] [Google Scholar]
- 62.Atfi A, Djelloul S, Chastre E, Davis R, Gespach C. Evidence for a role of Rho-like GTPases and stress-activated protein kinase/c-Jun N-terminal kinase (SAPK/JNK) in transforming growth factor beta-mediated signaling. J Biol Chem 1997;272:1429–1432. [DOI] [PubMed] [Google Scholar]
- 63.Utsugi M, Dobashi K, Ishizuka T, Masubuchi K, Shimizu Y, Nakazawa T, Mori M. C-Jun-NH2-terminal kinase mediates expression of connective tissue growth factor induced by transforming growth factor-beta1 in human lung fibroblasts. Am J Respir Cell Mol Biol 2003;28:754–761. [DOI] [PubMed] [Google Scholar]
- 64.Itoh S, Thorikay M, Kowanetz M, Moustakas A, Itoh F, Heldin CH, ten Dijke P. Elucidation of Smad requirement in transforming growth factor-beta type I receptor-induced responses. J Biol Chem 2003;278:3751–3761. [DOI] [PubMed] [Google Scholar]
- 65.Xie S, Sukkar MB, Issa R, Oltmanns U, Nicholson AG, Chung KF. Regulation of TGF-beta 1-induced connective tissue growth factor expression in airway smooth muscle cells. Am J Physiol Lung Cell Mol Physiol 2005;288:L68–L76. [DOI] [PubMed] [Google Scholar]
- 66.Zhang Y, Feng XH, Derynck R. Smad3 and Smad4 cooperate with c-Jun/c-Fos to mediate TGF-beta-induced transcription. Nature 1998;394:909–913. [DOI] [PubMed] [Google Scholar]
- 67.Hocevar BA, Brown TL, Howe PH. TGF-beta induces fibronectin synthesis through a c-Jun N-terminal kinase-dependent, Smad4-independent pathway. EMBO J 1999;18:1345–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Eferl R, Hasselblatt P, Rath M, Popper H, Zenz R, Komnenovic V, Idarraga MH, Kenner L, Wagner EF. Development of pulmonary fibrosis through a pathway involving the transcription factor Fra-2/AP-1. Proc Natl Acad Sci USA 2008;105:10525–10530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim KK, Kugler MC, Wolters PJ, Robillard L, Galvez MG, Brumwell AN, Sheppard D, Chapman HA. Alveolar epithelial cell mesenchymal transition develops in vivo during pulmonary fibrosis and is regulated by the extracellular matrix. Proc Natl Acad Sci USA 2006;103:13180–13185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Willis BC, Borok Z. TGF-beta-induced EMT: mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol 2007;293:L525–L534. [DOI] [PubMed] [Google Scholar]
- 71.Wu Z, Yang L, Cai L, Zhang M, Cheng X, Yang X, Xu J. Detection of epithelial to mesenchymal transition in airways of a bleomycin induced pulmonary fibrosis model derived from an alpha-smooth muscle actin-Cre transgenic mouse. Respir Res 2007;8:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yamada M, Kuwano K, Maeyama T, Hamada N, Yoshimi M, Nakanishi Y, Kasper M. Dual-immunohistochemistry provides little evidence for epithelial-mesenchymal transition in pulmonary fibrosis. Histochem Cell Biol 2008;129:453–462. [DOI] [PubMed] [Google Scholar]