Abstract
Introduction
In this study, we assessed whether the likelihood of a positive overjet 5 to 10 years after Class III surgery was affected by age at the surgery or the type of surgery and evaluated the amount and pattern of postsurgical growth.
Methods
Cephalometric measurements including overjet were evaluated from immediately postsurgery and long-term recall cephalograms of 104 patients who had had surgical Class III correction and at least 5-year recalls. The patients were classified as younger (<age 18 years for females at the surgery or 20 years for males) or older and by type of surgery (maxilla only vs mandibular only or 2 jaw). For the younger patients, the timing of treatment was based largely on serial cephalometric radiographs that eventually showed minimal or no mandibular growth.
Results
Long-term changes in overjet and other cephalometric characteristics in the younger and the older patients were similar. No patients in the sample had negative overjet in the long term, but zero overjet (<1 mm) was observed in some patients in all groups. Patients who had mandibular setback at any age were 2.6 times more likely to have zero overjet in the long term (P = .003) than those with maxillary surgery alone. For the younger patients, the likelihood of zero overjet in the long term was not significantly different from patients who were treated later (P = .87), with or without mandibular surgery.
Conclusions
The data support the use of serial cephalometric radiographs, with surgery deferred until little or no mandibular growth is observed, to determine the timing of Class III surgery in younger patients.
The timing of surgical correction of skeletal Class III problems for younger patients is complicated by 2 competing goals: (1) teenage patients, especially girls, often believe that their appearance creates psychosocial problems and are eager to complete their treatment,1,2 but (2) continued mandibular growth after early surgery is likely and can cause the problem to return.3 If psychosocial issues in adolescence are severe enough, early surgery followed by a second later procedure might be indicated.
For most young patients, however, Class III surgery is delayed until serial cephalometric radiographs show minimal mandibular growth. In the University of North Carolina (UNC) patient population, serial cephalometric radiographs that showed little or no continued mandibular growth were used to indicate that it should be safe to proceed with surgery. The purpose of this study was to evaluate the likelihood of unfavorable long-term changes after surgery that led to loss of positive overjet at the 5-year or longer recall in younger and older patients.
MATERIAL AND METHODS
From the UNC data base, cephalometric radiographs of all 104 patients who had been recalled between 5 and 10 years after surgical correction of a skeletal Class III problem were used to evaluate changes from postsurgery to long-term recall. The objectives were to test the hypothesis that the chance of loss of positive overjet (defined as zero or negative overjet measured cephalometrically at the long-term recall) would be greater in the younger patients and to compare the percentages of patients with changes by surgery type and age.
The characteristics of the patients are summarized in Table I. Of the 104 patients (of whom 60 were female), only a few (n = 16) had an isolated mandibular setback. This reflects the strong trend in recent years toward maxillary or 2-jaw surgery in Class III treatment.4 Because forward growth of the mandible after surgery could be more likely in patients whose Class III problem had a component of mandibular prognathism, the patients were categorized into 2 surgical groups: those who had maxillary advancement only (n = 55) and those who had mandibular setback with or without maxillary advancement (n = 49).
Table I.
Sample characteristics of Class III surgery patients with 5−10 year recall
| Maxilla only |
Mandible only or 2-jaw |
|||
|---|---|---|---|---|
| Younger n = 25 | Older n = 30 | Younger n = 24 | Older n = 25 | |
| Female (%) | 68 | 32 | 67 | 33 |
| Genioplasty (%) | 24 | 10 | 33 | 16 |
| Age at surgery (y) | ||||
| Mean | 16.6 | 32.6 | 16.8 | 29.4 |
| SD | 1.1 | 10.2 | 1.3 | 10.2 |
| Follow-up (y) | ||||
| Mean | 6.6 | 6.3 | 6.2 | 6.8 |
| SD | 1.9 | 1.8 | 1.8 | 2.0 |
The subjects also were classified into 2 categories based on age at the time of surgery. The younger group consisted of females below the age of 18 at the surgery and males below the age of 20, and the older group included females 18 or older and males 20 or older. The age limits for the younger group represent ages below which mandibular growth might still be expected. The decision to proceed with surgery for these patients was made largely on the basis of serial cephalometric radiographs that showed little or no mandibular growth.
The presurgery, immediately postsurgery, and long-term recall cephalometric radiographs were traced and digitized by using UNC's 139-point model. All patients had at least 2 mm of surgical change in the position of the maxilla or the mandible. As in our previous reports6-11 of postsurgical stability, a horizontal line through sella and nasion rotated down 6° anteriorly, approximately parallel to true horizontal, was established as the x-axis, and a vertical line through sella perpendicular to it as the y-axis. The primary outcome was defined as the presence or absence of positive overjet (<1 mm) at the long-term recall. Surgical and postsurgical changes in the x and y coordinate distances were calculated for A-point, B-point, condylion, gonion, and pogonion. Changes in overjet, overbite, ramus height (Co-Go), and mandibular length (Co-Pg) were also calculated, as were the mandibular plane angle (Go-Gn to SN) and the palatal plane angle (ANSPNS to SN).
By using logistic regression with the generalized logit function to provide an exact test of the parameters, the effect of age at surgery (younger vs older) and type of surgery (maxillary only vs mandibular) on the likelihood of positive overjet 5 to 10 years after surgical Class III correction was assessed. The level of significance was set at .05.
RESULTS
The characteristics of the patient sample are shown in Table I. There were more older males with maxillary advancement only; this probably reflects the perception that a strong chin is more esthetically acceptable in men. The younger patients were more likely than the older ones to have further chin repositioning by genioplasty.
For Class III treatment, overjet is a good indicator of long-term clinical success. Table II shows presurgery, immediately postsurgery, and long-term recall data for overjet in the younger and older groups by type of surgery. In all patients, the jaw surgery changed negative overjet to positive overjet immediately after treatment. At the long-term recall, no patient had a negative overjet. As Table III shows, in the older maxillary advancement group, 8 (27%) of the patients no longer had positive overjet—ie, were end-to-end with zero overjet. Four (17%) of the younger maxillary advancement patients, 12 (50%) of the younger mandibular setback patients, and 9 (36%) of the older mandibular setback patients had zero overjet. There was no statistically significant difference in the likelihood of loss of positive overjet between the younger and older patients as defined in this study (odds ratio: 1.1; 95% CI: 0.46, 2.5). Those who had mandibular surgery were 2.6 times more likely to have zero overjet at the long-term recall (odds ratio: 2.6; 95% CI: 1.1, 6.2).
Table II.
Descriptive statistics for presurgery, immediately postsurgery, and long-term overjet (mm)
| Presurgery |
Immediately postsurgery |
Long term |
|||||
|---|---|---|---|---|---|---|---|
| n | Mean | SD | Mean | SD | Mean | SD | |
| Maxilla only | |||||||
| Younger | 25 | 0.3 | 3.3 | 3.1 | 1.2 | 2.1 | 1.3 |
| Older | 30 | −1.2 | 2.5 | 2.9 | 1.7 | 2.3 | 1.5 |
| Mandible* | |||||||
| Younger | 24 | −3.0 | 3.5 | 2.8 | 1.1 | 1.2 | 1.4 |
| Older | 25 | −3.7 | 2.9 | 2.4 | 1.2 | 1.3 | 1.4 |
With or without maxillary procedure.
Table III.
Percentage of subjects with zero and positive overjet at long-term recall
| Zero (<1 mm) |
Positive (≥1 mm) |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Maxilla only | ||||
| Younger | 4 | 16 | 21 | 84 |
| Older | 8 | 27 | 22 | 73 |
| Mandible* | ||||
| Younger | 12 | 50 | 12 | 50 |
| Older | 9 | 36 | 16 | 64 |
With or without maxillary procedure.
On average, changes in landmark positions for both the older and the younger groups were mainly in forward and somewhat downward directions (Table IV). The average increases in mandibular length (Co-Pg) were 2.1 mm in the younger maxillary surgery group and 2.4 mm in the younger mandibular surgery group, vs 0.7 mm in the older maxillary surgery group and 2.0 mm in the older mandibular surgery group. A mean upward movement of the maxilla and the chin, also with a large standard deviation, was noted in the older patients but not in the younger patients. Patients with mandibular surgery at any age had a greater increase in the mandibular plane angle than those with only maxillary surgery, because gonion tended to move up (shortening ramus height) and Point B often moved down (increasing anterior face height). For all groups, however, large standard deviations reflected the considerable variation in dimensional changes. This was also true for landmark positions.
Table IV.
Cephalometric changes, postsurgery to >5-year recall
| Maxilla only |
Mandible* |
|||||||
|---|---|---|---|---|---|---|---|---|
| Younger n = 25 |
Older n = 30 |
Younger n = 24 |
Older n = 25 |
|||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Horizontal | ||||||||
| Point A (mm) | −0.9 | 1.88 | −0.8 | 2.01 | −0.1 | 1.29 | −0.8 | 2.43 |
| Point B (mm) | 3.0 | 3.31 | 4.0 | 3.36 | 3.1 | 2.21 | 2.5 | 3.50 |
| Gonion (mm) | 2.8 | 2.42 | 3.3 | 2.93 | 2.4 | 2.86 | 3.0 | 4.29 |
| Pogonion (mm) | 3.5 | 4.72 | 4.9 | 4.03 | 3.2 | 2.29 | 3.0 | 3.50 |
| Condylion (mm) | 0.6 | 1.55 | 0.0 | 1.80 | 0.4 | 1.18 | −0.2 | 2.07 |
| Vertical | ||||||||
| Point A (mm) | −1.3 | 2.48 | −3.0 | 3.35 | −0.5 | 1.73 | −0.9 | 1.80 |
| Point B (mm) | −0.9 | 2.45 | −3.2 | 3.18 | 0.0 | 3.31 | −1.6 | 2.84 |
| Gonion (mm) | 1.2 | 2.58 | 0.2 | 2.02 | −0.8 | 3.19 | −3.4 | 2.94 |
| Pogonion (mm) | 0.1 | 3.82 | −3.4 | 3.51 | 0.1 | 2.71 | −1.5 | 2.92 |
| Condylion (mm) | −0.2 | 1.85 | 0.0 | 1.98 | −0.6 | 1.80 | −1.2 | 2.01 |
| Dimensions | ||||||||
| Overjet (mm) | −1.0 | 1.24 | −0.6 | 1.44 | −1.6 | 0.87 | −1.1 | 1.22 |
| Overbite (mm) | 1.6 | 2.14 | 1.9 | 1.79 | 1.0 | 1.65 | 2.1 | 1.53 |
| Co-Pg (mm) | 2.1 | 3.26 | 0.7 | 1.46 | 2.4 | 2.39 | 2.0 | 3.43 |
| Co-Gn (mm) | 1.6 | 3.20 | 0.7 | 2.41 | 0.1 | 3.72 | −1.6 | 3.15 |
| Mandibular plane (°) | −2.3 | 2.43 | −3.0 | 2.58 | 0.1 | 2.91 | 1.1 | 2.46 |
| Palatal plane (°) | −1.6 | 3.99 | −2.6 | 3.52 | −0.8 | 2.08 | −0.6 | 2.31 |
With or without maxillary procedure.
Because most of the changes occurred in some of the patients, the percentages of patients with change outside the range of cephalometric error (2−4 mm) and change that definitely would be clinically significant (>4 mm) give a clearer picture of the general pattern of postsurgical change. Figures 1 and 2 show the percentages of patients with horizontal and vertical changes in the position of Points A and B; Figure 3 shows changes in mandibular length (Co-Pg) and overjet. Note the similarity in the 4 groups in the numbers of patients with changes. The percentages of patients with changes in other landmarks and dimensions reflect the same pattern of continued forward-downward mandibular growth in many subjects in each group, but similar changes in the younger and older groups.
Fig 1.
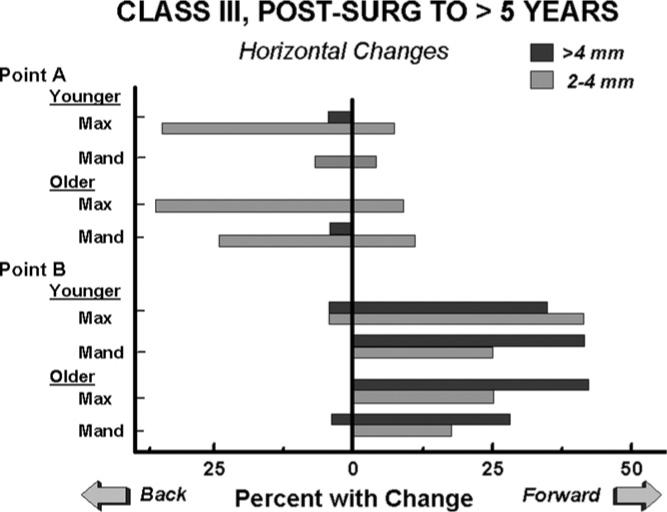
Percentages of patients with horizontal change in the positions of Points A and B. Point A remained stable in 90% of the younger patients with mandibular or 2-jaw surgery and in over 60% of the patients in the other 3 groups, in which 25% to 30% had some backward movement due to long-term remodeling of this area. In all 4 groups, most patients had forward movement of Point B, and 28% to 42% had >4 mm of forward movement. The patterns of change in the younger and older groups were similar.
Fig 2.
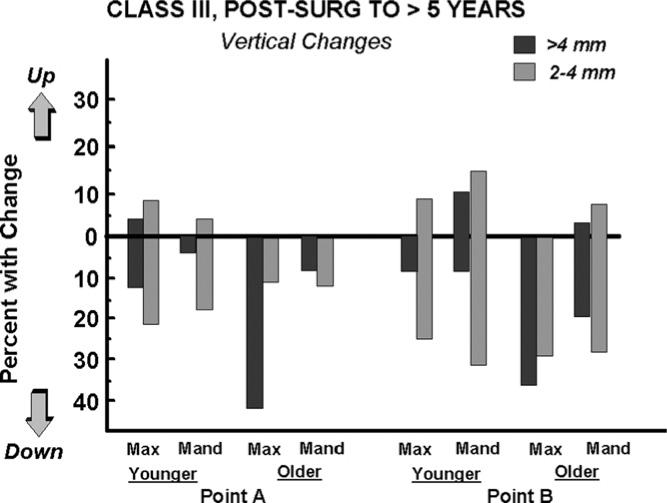
Percentages of patients with vertical change in the positions of Points A and B. The vertical position of Point A was stable in two thirds or more of the patients in all groups except the older maxillary surgery patients, in whom downward movement occurred in over half (53%), and 43% had >4 mm of downward movement. The vertical position of Point B showed changes in half or more of the patients in all groups. Downward movement occurred in 63% of the older maxillary surgery patients, 33% of whom had >4 mm of movement. Upward movement occurred in 25% of the younger mandibular or 2-jaw group, primarily in the 2-jaw patients in whom Point A also moved up. The patterns of change were similar in the younger and older patients, with a higher percentage with change in the older groups.
Fig 3.
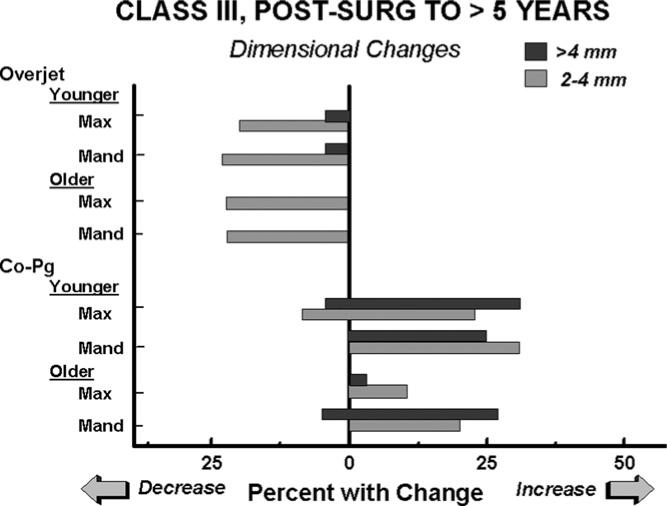
Percentages of patients with changes in overjet and mandibular length (Co-Pg). Overjet decreased 2−4 mm in about 25% of the patients in all groups. A decrease of >4 mm occurred in 1 patient (4%) in each younger group. Mandibular length increased in slightly over half of the younger patients in both surgery groups and in nearly half (48%) of the older mandibular surgery group. Only 13% of the older maxillary surgery patients had an increase in mandibular length. The percentages of change in the older and younger patients with mandibular surgery were similar.
DISCUSSION
Previous studies of long-term (>5 years) changes after jaw surgery showed that, although surgical healing is completed well before 1 year later, a surprisingly large number of Class II open bite and Class III patients who have 1- or 2-jaw surgery have long-term changes 1 year postsurgery, but not necessarily in the direction of relapse.5-11 These long-term changes are not due just to instability during surgical healing or the remodeling changes in the jaws that occur in untreated adults as the years pass. On average, postsurgery changes in patients are greater than those seen in untreated adults or in adults who had nonsurgical orthodontic treatment.12-13 It appears that postsurgical growth, in the pattern that produced the problem initially, occurs beyond 1 year postsurgery in many adults. For the patients in this study, postsurgical instability could have contributed to the changes, but, from comparison of these patients with the previous studies,6-11 it seems likely that long-term growth was the major factor.
In young Class III patients, ample clinical experience has shown that early surgery, before the cessation of mandibular growth, is likely to be followed by relapse because excessive mandibular growth continues. Because many severely affected Class III patients want their problem corrected as early as possible, a method to determine the earliest safe time for treatment has been sought for many years. The current clinical consensus is that indirect methods, based on hand-wrist radiographs or other indicators of skeletal maturation, do not correlate well enough with the cessation of excessive mandibular growth. Monitoring mandibular growth with serial cephalograms, and waiting until growth has stopped in that patient, usually is judged to be the best method.3
To our knowledge, no previous study has provided long-term data to support this clinical guideline. It would be possible, of course, that the younger patients still have more postsurgical growth than the older ones, and that this would be more likely in those who required mandibular setback as part of their treatment. In this study, only small differences were observed in the long-term changes between Class III patients treated at relatively young vs older ages. On long-term recall, postsurgical growth was observed in many older and younger patients, and those who had mandibular surgery showed more mandibular growth on long-term recall than those with maxillary surgery alone. The key finding, however, was that skeletal and dental changes leading to loss of positive overjet in the long term were not significantly greater in the younger patients, who had surgery only after serial cephalograms showed little or no mandibular growth, with or without mandibular surgery. We concluded that, after little or no mandibular growth is observed in serial cephalograms, younger Class III patients have about the same prognosis for long-term clinical success as older ones in whom less growth might be expected.
Acknowledgments
We thank Debora Price for digitization of the radiographs and application of the SAS statistical analysis (SAS, Cary, NC) procedures, and Dr. Timothy Turvey and the UNC oral-maxillofacial surgery faculty for surgical treatment.
Supported in part by NIH grant DE-05221 from the National Institute of Dental and Craniofacial Research.
REFERENCES
- 1.Shaw WC. The influence of children's dentofacial appearance on their social attractiveness as judged by peers and lay adults. Am J Orthod. 1981;79:399–415. doi: 10.1016/0002-9416(81)90382-1. [DOI] [PubMed] [Google Scholar]
- 2.Helm S, Kreiborg S, Solow B. Psychosocial implications of malocclusion: a 15 year follow-up study in 30-year-old Danes. Am J Orthod. 1985;85:393–400. doi: 10.1016/0002-9416(85)90020-x. [DOI] [PubMed] [Google Scholar]
- 3.Proffit WR, Phillips C. Physiologic responses to treatment and post-surgical stability. In: Proffit WR, White RP Jr, Sarver D, editors. Contemporary treatment of dentofacial deformity. Mosby; St Louis: 2003. [Google Scholar]
- 4.Bailey LJ, Proffit WR, White RP. Trends in surgical Class III treatment. Int J Adult Orthod Orthognath Surg. 1995;10:108–18. [PubMed] [Google Scholar]
- 5.Simmons KE, Turvey TA, Phillips C, Proffit WR. Surgical-orthodontic correction of mandibular deficiency: five year follow-up. Int J Adult Orthod Orthognath Surg. 1992;7:67–80. [PubMed] [Google Scholar]
- 6.Bailey LJ, Phillips C, Proffit WR, Turvey TA. Stability following superior repositioning of the maxilla by LeFort I osteotomy: five year follow-up. Int J Adult Orthod Orthognath Surg. 1994;9:163–74. [PubMed] [Google Scholar]
- 7.Miguel JA, Turvey TA, Phillips C, Proffit WR. Long-term stability of two-jaw surgery for treatment of mandibular deficiency and vertical maxillary excess. Int J Adult Orthod Orthognath Surg. 1995;10:235–45. [PubMed] [Google Scholar]
- 8.Lee DY, Bailey LJ, Proffit WR. Soft tissue changes after repositioning the maxilla by LeFort I osteotomy: five year follow-up. Int J Adult Orthod Orthognath Surg. 1996;11:301–12. [PubMed] [Google Scholar]
- 9.Bailey LJ, Duong HL, Proffit WR. Surgical Class III treatment: long-term stability and patient perceptions of treatment outcome. Int J Adult Orthod Orthognath Surg. 1998;13:35–44. [PubMed] [Google Scholar]
- 10.Proffit WR, Bailey LJ, Phillips C, Turvey TA. Long-term stability of surgical open bite correction by LeFort I osteotomy. Angle Orthod. 2000;70:112–7. doi: 10.1043/0003-3219(2000)070<0112:LTSOSO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Busby BR, Bailey LJ, Proffit WR, Phillips C, White RP. Long-term stability of surgical Class III treatment: a study of 5-year postsurgical results. Int J Adult Orthod Orthognath Surg. 2002;17:159–70. [PubMed] [Google Scholar]
- 12.Schubert P, Bailey LJ, White RP, Proffit WR. Long-term cephalometric changes in untreated adults compared to those treated with orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1999;14:91–9. [PubMed] [Google Scholar]
- 13.Mihalik CA, Proffit WR, Phillips C. Long-term follow-up of Class II adults treated with orthodontic camouflage: a comparison with orthognathic surgery outcomes. Am J Orthod Dentofacial Orthop. 2003;123:266–78. doi: 10.1067/mod.2003.43. [DOI] [PMC free article] [PubMed] [Google Scholar]


