Abstract
AIM:
To determine whether a shortened 13C urea breath test (13C UBT) (breath collection time of 10 min) is as reliable as the standard assay (30 min).
METHODS:
Two hundred ninety-seven patients (mean ± SD: 53±16 years, 57% female) completed a 13C UBT. Breath samples were obtained at baseline and at 5 min intervals up to 30 min. Sixty-seven patients also underwent endoscopic biopsy. Cluster analysis was performed on the 13C UBT data to determine the optimal cut-off point at each time interval. Sensitivity and specificity of the 13C UBT at all intervals compared with histology and culture and against the standard 30 min interval were determined.
RESULTS:
The calculated optimal cut-off points for each time interval (T), expressed as delta over baseline (δ‰), were 3.29 δ‰ at T5, 3.15 δ‰ at T10, 3.42 δ‰ at T15, 3.17 δ‰ at T20, 2.99 δ‰ at T25 and 2.82 δ ‰ at T30. Except at T5, the risk of false-positive and false-negative test results at each time interval was lower than 2.3% using these cut-off points. When replacing the cut-off points with 3.0 δ‰, the risk of error was still lower than 2.3%. The test at T10 showed 98.6% sensitivity and 98.6% specificity compared with T30. T10 and T30 showed 100% sensitivity and 96% specificity compared with histology and culture.
CONCLUSIONS:
The 13C UBT is an accurate, noninvasive test, even when the breath sample interval is reduced to 10 min. The present study confirms the validity of a cut-off point of 3.0 δ‰ for the 10 min and 30 min 13C UBT.
Keywords: 13C urea breath test, Cut-off point, Helicobacter pylori
Abstract
OBJECTIF :
Déterminer si un test respiratoire à l’urée marquée au 13C (TRUM 13C) moins long (prélèvement d’air expiré de 10 minutes) est aussi fiable que le test standard (30 minutes).
MÉTHODOLOGIE :
Deux cent quatre-vingt-dix-sept patients (âge moyen de 53±16 ans, 57 % de sexe féminin) ont subi un TRUM 13C. On a prélevé l’air expiré au début du test, puis à intervalles de cinq minutes jusqu’à 30 minutes. Soixante-sept patients ont également subi une biopsie endoscopique. On a exécuté une analyse typologique des données du TRUM 13C pour déterminer la limite d’inclusion optimale à chaque intervalle. On a également déterminé la sensibilité et la spécificité du TRUM 13C à chaque intervalle par rapport à l’histologie, à la culture et à l’intervalle de 30 minutes.
RÉSULTATS :
Les limites d’inclusion optimales calculées à chaque intervalle (T), exprimées à titre de coefficient delta sur le temps de base (߉) étaient de 3,29 δ‰ au T5, de 3,15 δ‰ au T10, de 3,42 δ‰ au T15, de 3,17 δ‰ au T20, de 2,99 δ‰ au T25 et de 2,82 δ‰ au T30. D’après ces limites d’inclusion, sauf au T5, le risque de résultats faux positifs ou faux négatifs à chaque intervalle était inférieur à 2,3 %. Lorsqu’on remplaçait les limites d’inclusion par 3,0 δ‰, le risque d’erreur demeurait inférieur à 2,3 %. Le test au T10 a révélé une sensibilité de 98,6 % et une spécificité de 98,6 % par rapport au T30. Les tests aux T10 et T30 ont révélé une sensibilité de 100 % et une spécificité de 96 % par rapport à l’histologie et à la culture.
CONCLUSIONS :
Le TRUM 13C est un test précis et non effractif, même lorsque l’intervalle de prélèvement d’air expiré est réduit à 10 minutes. La présente étude confirme la validité d’utiliser une limite d’inclusion de 3,0 δ‰ pour le TRUM 13C à 10 minutes et à 30 minutes.
Helicobacter pylori infection is one of the most common human infections worldwide (1). Although the prevalence of H pylori is falling in the western world, the prevalence in Canada still remains in the range of 20% to 40% (2,3). Since the discovery of the H pylori association with chronic gastritis, peptic ulcers, gastric lymphoma and gastric adenocarcinoma (4–6), several diagnostic tests, both invasive and noninvasive, have been developed. The development of the 13C urea breath test (13C UBT), which has a specificity of 98% and a sensitivity of 97%, allows the determination of H pylori status without the need for costly invasive endoscopies (7). The 13C UBT has become the noninvasive test of choice for both diagnosis and for confirmation of H pylori eradication after treatment, as recommended by a number of clinical guidelines (8–10). The 13C UBT is a practical and accurate test on which to base a ‘test and treat’ strategy for dyspepsia management (11,12) and its clinical performance has recently been validated in Canada in a community laboratory setting ( pages 770–774 in the current issue of the Journal).
The 13C UBT detects gastric H pylori urease activity by measuring 13C enrichment in expired breath samples after ingestion of 13C-labelled urea. There is general agreement on the use of two breath samples, one collected before and another 30 min after urea ingestion, regardless of the dosage of the isotope administered.
In view of the increasing application of 13C UBT due to the large number of individuals who may have an H pylori infection, a rapid performance of 13C UBT may be advantageous to patients and health services to reduce costs and personnel utilization.
The aim of the present study was to compare the accuracy of a 10 min breath collection with the standard 30 min breath collection for the 13C UBT, and to compare the short-course 13C UBT with histology and culture.
PATIENTS AND METHODS
The study protocol was approved by the McMaster University Research Ethics Board. The 13C UBT was performed in 297 patients (mean age ± SD: 53±16 years, 57% female) who had various gastrointestinal symptoms. One hundred twenty-two patients were tested to evaluate the primary diagnosis of H pylori infection (diagnosis group) and 60 were tested for confirmation of eradication after therapy (post-treatment group); 115 patients were referred without being categorized in either group.
Patients were asked about their use of antibiotics and acid-suppressive treatment during the four weeks before the testing and about previous eradication therapy. Exclusion criteria included the use of proton-pump inhibitors, bismuth compounds or antibiotics within 14 days before the 13C UBT.
After an overnight fast, patients performed the 13C UBT by providing breath samples at baseline (T0) and at 5 min intervals up to 30 min (T5, T10, T15, T20, T25 and T30) after oral ingestion of 75 mg 13C-labelled urea (Helikit, Isotechnika Diagnostics, Canada) in 100 mL of citric acid solution. All samples were analyzed by a gas isotope ratio mass spectrometer (BreathMAT, Finnigan MAT GmbH, Germany). The difference between the values at T5, T10, T15, T20, T25 and T30 and those at T0 are expressed as delta over baseline (DOB, δ‰). Based on prior validation (13), the cut-off point for the diagnostic test was defined as 3.0 δ‰.
Data were examined visually by plotting the logarithmic transformation of measurements taken from the 13C UBT at T5, T10, T15, T20, T25 and T30. The distribution of the natural logarithms (logn) of the DOB values at each breath sample test interval identified two normally distributed subpopulations that were considered to represent H pylori-positive and H pylori-negative patients. The normal distribution of the positive and negative populations enabled cluster analysis to be performed on these data to determine the minimal intraclass variance, and thus, the logn (Tsample interval –T0) value, which best separated the presumed H pylori-negative and H pylori-positive populations. Thereafter, the parameters (mean DOB and SD) of the H pylori-negative and H pylori-positive populations were established. The cut-off value was calculated as the point equidistant from the means of H pylori-negative and H pylori-positive populations. Thus, the probability an H pylori-negative patient producing a 13C UBT result with a value greater than the cut-off point (ie, a false-positive result), and the probability of an H pylori-positive patient producing a 13C UBT result with a smaller value than the cut-off point (ie, a false-negative result) were determined. This analysis was performed on the total patient group and on the diagnosis and post-treatment subgroups at each breath sample test interval. Sensitivity (true-positives/[true-positives + false-negatives]δ100) and specificity (true-negatives/[true-negatives + false-positives]δ100) at T5 to T25 were calculated and compared with those of the T30 samples (the ‘gold standard’).
Upper gastrointestinal endoscopy was performed on 67 patients (35 female, 32 male) before the 13C UBT. During the examination, three biopsy specimens each from the gastric antrum and corpus were obtained for histology and bacterial culture. Silver staining (Warthin-Starry) was used to identify H pylori in the biopsy specimens. Culture samples were inoculated in Brucella blood agar, Mueller-Hinton sheep blood agar and egg yolk emulsion; all plates were incubated at 35°C for four days. H pylori growth was confirmed by Gram staining, a rapid urea test, an oxidase test and a wet preparation for motility. Negative cultures were reincubated and examined seven to 10 days later. Infection status was determined when both methods (histology and culture) produced concordant results. Sensitivity and specificity for all time intervals were calculated and compared with histology and culture.
RESULTS
Data were examined visually by plotting the logarithmic transformation of the DOB values from 297 13C UBT results for T5 to T30. It was evident that the normal distribution of the DOB values for each time interval could describe two distinct classes: H pylori-negative and H pylori-positive populations (Figure 1). From this, the mean and SD DOB values of logn (Tsample interval –T0) for the presumed subpopulations were calculated. The point equidistant between the mean values of the subpopulations was calculated for each breath sample test interval. The optimal cut-off points determined for each time interval were 3.29 δ‰ for T5, 3.15 δ‰ for T10, 3.42 δ‰ for T15, 3.17 δ‰ for T20, 2.99 δ‰ for T25 and 2.82 δ‰ for T30 (Table 1). The difference (normal deviate) between the cut-off points and the means of normal H pylori-negative and H pylori-positive distributions were 1.90 SD for T5, 2.21 SD for T10, 2.38 SD for T15, 2.41 SD for T20, 2.36 SD for T25 and 2.17 SD for T30.These normal deviates were found to be greater than 2 SD for all time intervals except for T5 (Figure 2), indicating that, by comparison of these values with the table of the proportions of the normal curve, the proportions of H pylori-negative and H pylori-positive populations producing a 13C UBT result greater or smaller than the cut-off point were always lower than 2.3%. Thus, except for T5, the risks of false-positive or false-negative results from the 13C UBT for a diagnosis of H pylori infection were lower than 2.3% when using these cut-off points. When the cut-off points determined for T10 to T30 were replaced with a practical cut-off determined for T10 to T30 were replaced with a practical cut-off point of 3.0 δ‰, the corresponding normal deviates for H pylori-negative and H pylori-positive distributions were greater than 2 SD in all cases. Thus, according to the table of the proportions of the normal curve, the risk of error was still lower than 2.3%. When a cut-off point of 3.0 δ‰ was used, 25.6% of patients had positive results for H pylori infection.
Figure 1).
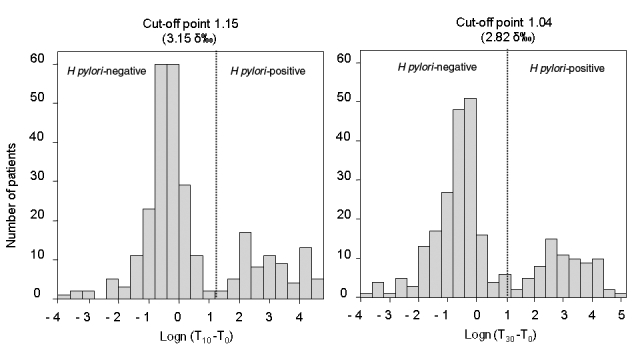
Cluster analysis. The histogram of the logarithmically transformed 13C urea breath sample values at 10 min past baseline and 30 min past baseline showed two distinct populations: Helicobacter pylori-negative and H pylori-positive. The cut-off value for each sample interval was calculated as the point equidistant between the means of the H pylori-negative and H pylori-positive populations
TABLE 1.
Calculated cut-off point for each sample interval
| 13C UBT sample interval | Log-transformed cut-off point (δ‰) | Cut-off point (δ‰) |
|---|---|---|
| T5 | 1.19 | 3.29 |
| T10 | 1.15 | 3.15 |
| T15 | 1.23 | 3.42 |
| T20 | 1.15 | 3.17 |
| T25 | 1.09 | 2.99 |
| T30 | 1.04 | 2.82 |
T Time past baseline (min); UBT Urea breath test
Figure 2).
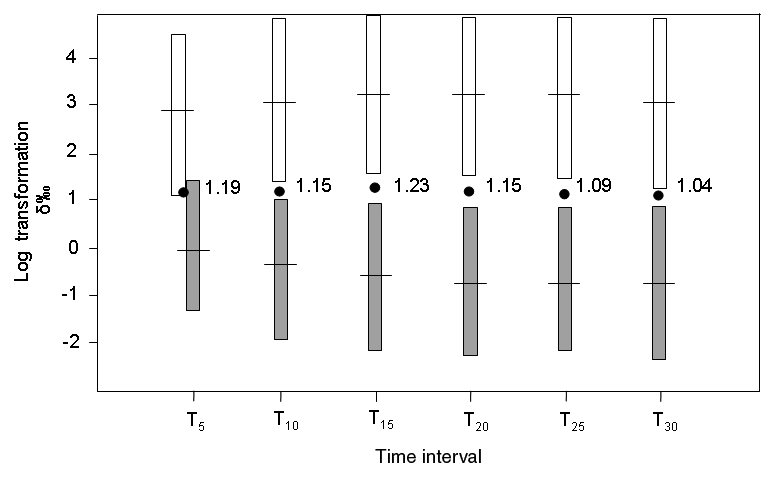
The distance between the cut-off point (black circles) and the means of the Helicobacter pylori-positive (white bars: mean ± 2 SD) and H pylori-negative (grey bars: mean ± 2 SD) populations was greater than 2 SD for all sample intervals except for the time interval at 5 min past baseline (T5). Log Logarithmic
These calculations were also performed for the two subgroups (diagnosis and confirmation of eradication). When the cut-off points obtained in the two groups were replaced with 3.0 δ‰ for 13C UBT T10 to T30, as determined for the whole population, the normal deviates for H pylori-positive and H pylori-negative distributions in both groups were greater than 1.94 SD in all cases for all time intervals from 10 min to 30 min, showing a risk lower than 3% of false-positive or false-negative results. T10 was chosen for further comparisons because it was the shortest time interval that showed a risk of error lower than 2.3%.
13C UBT results at T10 were compared with those of T30, (the standard time interval). T10 results showed 98.6% sensitivity and 98.6% specificity compared with T30 results using a cut-off point of 3.0 δ‰.
In a group of 67 patients, the T10 and T30 13C UBT results at a cut-off point of 3.0 δ‰ were compared with histology and culture (the gold standard). The T30 13C UBT showed sensitivity of 100% and specificity of 96% and the T10 13C UBT showed sensitivity of 100% and specificity of 96%. Based on an H pylori prevalence of 20% to 40% in the Canadian population (2,3), the positive predictive value for the T10 13C UBT would be between 94.6% and 97.9% and the negative predictive value would be between 99.6% and 99% (Figure 3).
Figure 3).
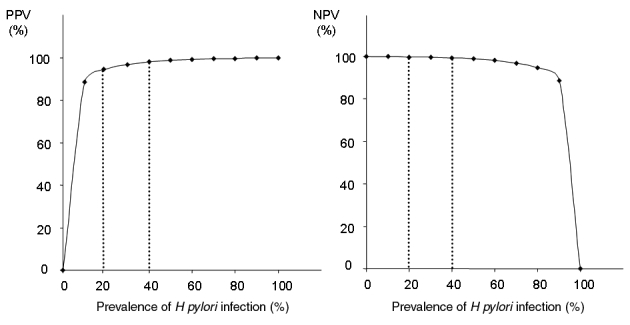
Positive predictive values (PPV) and negative PV (NPV) for the 13C urea breath test at 10 min past baseline. Based on a Helicobacter pylori prevalence of 20% to 40% in the Canadian population, the PPV at 10 min past baseline would be between 94.6% and 97.9% and the NPV would be between 99.6% and 99%
DISCUSSION
H pylori has been shown to infect over 50% of the world’s population, with an incidence of up to 80% in developing countries (1). Because of the pivotal role of H pylori in many human gastroduodenal pathologies, it has been recommended that patients with abdominal discomfort undergo a rapid, noninvasive screening for H pylori infection (8). The 13C UBT is now widely used to document H pylori infection (13) and has been recommended as the preferred method for epidemiological studies and for screening patients with dyspeptic symptoms. It has also been acknowledged as the best noninvasive test to assess the efficacy of anti-H pylori treatments (14,15).
To render the test less expensive and more rapid, we proposed to reduce the sample interval from the standard 30 min to 10 min, with the aim of shortening sampling time to improve patient compliance and optimize personnel employment.
Using cluster analysis, we determined the cut-off points for the T10 and T30 samples. We found that the optimal cut-off point in our population was 3.15 δ‰ for T10 and 2.82 δ‰ for T30. We previously validated (pages 770–774 in the current issue of the Journal) a cut-off point of 3.0 δ‰ in a large data set data (n=2232) in a Canadian community laboratory setting. The present study indicates a lower cut-off point than that reported in previous studies (T30–T0=5.0 δ‰) (16,17), but it has been confirmed by others in comparison with histology (18) and by cluster analysis (19). The risk of a false-negative or false-positive response is less than 2.3% when using a cut-off point of 3.0 δ‰ for the T10 and the T30 samples. The risk of error was also less than 3% if the same cut-off point was used in the groups that came for diagnosis and for confirmation of cure; thus, depending on the clinical situation (before or after treatment), it appears unnecessary to use different cut-off points. Like others (19), we recommend an indeterminate zone (2.5 δ‰ and 3.5 δ‰) for the 13C UBT, in which a second test would be recommended to assess the patient’s H pylori status more accurately rather than using a very strict cut-off point. Only one (of 297) result of the T10 samples and two (of 297) results of the T30 samples fell into this indeterminate zone.
In a group of 67 patients, the T10 and T30 13C UBT results at a cut-off point of 3.0 δ‰ were compared with histology and culture. The T30 13C UBT showed sensitivity of 100% and specificity of 96%, while the T10 13C UBT showed sensitivity of 100% and specificity of 96%.
Overall, the T10 13C UBT protocol in 297 individuals showed 98.6% sensitivity and 98.6% specificity compared with the 30 min 13C UBT protocol. This is consistent with the results of a previous study (20) that showed absolute concordance between results obtained at 10 min in comparison with the standard results obtained at 30 min using a cut-off point of 5.0 δ‰. In the present study, this diagnostic accuracy was maintained even with a lower cut-off point of 3.0 δ‰. Based on an H pylori prevalence of 20% to 40% in the Canadian population (1,2,21), the positive predictive value for the 10 min 13C UBT would be between 94.6% and 97.9% and the negative predictive value would be between 99.6% and 99% (Figure 3).
We conclude that the 10 min sample 13C UBT is an accurate, noninvasive test of active H pylori infection. The use of a shorter test protocol has the potential to facilitate routine clinical practice and increase patient acceptance with no loss of test performance for H pylori management. The present study confirms the validity of the (T30–T0) and (T10–T0)=3.0 δ‰ cut-off point for the diagnosis and confirmation of eradication of H pylori infection and underlines the necessity of an indeterminate zone between 2.5 δ‰ and 3.5 δ‰ in which the risk of error in this test is maximal.
Acknowledgments
The authors thank Dr Fiona Smaill and Pamela Lyn for their invaluable assistance with this work. The work of the author Markad Kamath was supported by the DeGroote Foundation and the Natural Sciences and Engineering Research Council of Canada (NSERC).
REFERENCES
- 1.The EUROGAST Study Group Epidemiology of, and risk factors for, Helicobacter pylori infection among 3194 asymptomatic subjects in 17 populations. Gut. 1993;34:1672–6. doi: 10.1136/gut.34.12.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiba N, Veldhuyzen Van Zanten SJ, Escobedo S, et al. Economic evaluation of Helicobacter pylori eradication in the CADET-Hp randomized controlled trial of H. pylori-positive primary care patients with uninvestigated dyspepsia. Aliment Pharmacol Ther. 2004;19:349–58. doi: 10.1111/j.1365-2036.2004.01865.x. [DOI] [PubMed] [Google Scholar]
- 3.Thomson AB, Barkun AN, Armstrong D, et al. The prevalence of clinically significant endoscopic findings in primary care patients with uninvestigated dyspepsia: The Canadian Adult Dyspepsia Empiric Treatment – Prompt Endoscopy (CADET-PE) study. Aliment Pharmacol Ther. 2003;17:1481–91. doi: 10.1046/j.1365-2036.2003.01646.x. [DOI] [PubMed] [Google Scholar]
- 4.Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347:1175–86. doi: 10.1056/NEJMra020542. [DOI] [PubMed] [Google Scholar]
- 5.Rothenbacher D, Brenner H. Burden of Helicobacter pylori and H. pylori-related diseases in developed countries: Recent developments and future implications. Microbes Infect. 2003;5:693–703. doi: 10.1016/s1286-4579(03)00111-4. [DOI] [PubMed] [Google Scholar]
- 6.Frenck RW, Jr, Clemens J. Helicobacter in the developing world. Microbes Infect. 2003;5:705–13. doi: 10.1016/s1286-4579(03)00112-6. [DOI] [PubMed] [Google Scholar]
- 7.Logan RP. Boca Raton: CRC Press; 1993. Breath tests used to detect Helicobacter pylori. In: Goodwin CS, Worsley BW, eds. Helicobacter pylori: Biology and Clinical Practice; pp. 307–27. [Google Scholar]
- 8.Malfertheiner P, Megraud F, O’Morain C, et al. European Helicobacter Pylori Study Group Current concepts in the management of Helicobacter pylori infection – The Maastricht 2-2000 Consensus Report. Aliment Pharmacol Ther. 2002;16:167–80. doi: 10.1046/j.1365-2036.2002.01169.x. [DOI] [PubMed] [Google Scholar]
- 9.Hunt RH, Fallone CA, Thomson AB. Canadian Helicobacter pylori Consensus Conference Update: Infections in adults. Canadian Helicobacter Study Group. Can J Gastroenterol. 1999;13:213–7. doi: 10.1155/1999/180751. [DOI] [PubMed] [Google Scholar]
- 10.Veldhuyzen van Zanten SJ, Bradette M, Chiba N, et al. Canadian Dyspepsia Working Group Evidence-based recommendations for short- and long-term management of uninvestigated dyspepsia in primary care: An update of the Canadian Dyspepsia Working Group (CanDys) clinical management tool. Can J Gastroenterol. 2005;19:285–303. doi: 10.1155/2005/674607. [DOI] [PubMed] [Google Scholar]
- 11.Marshall JK, Armstrong D, O’Brien BJ. Test and treat strategies for Helicobacter pylori in uninvestigated dyspepsia: A Canadian economic analysis. Can J Gastroenterol. 2000;14:379–88. doi: 10.1155/2000/978035. [DOI] [PubMed] [Google Scholar]
- 12.Chiba N, Van Zanten SJ, Sinclair P, Ferguson RA, Escobedo S, Grace E. Treating Helicobacter pylori infection in primary care patients with uninvestigated dyspepsia: The Canadian adult dyspepsia empiric treatment-Helicobacter pylori positive (CADET-Hp) randomised controlled trial. BMJ. 2002;324:1012–6. doi: 10.1136/bmj.324.7344.1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atherton J, Spiller RC. The urea breath test for Helicobacter pylori. Gut. 1994;35:723–5. doi: 10.1136/gut.35.6.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Slomianski A, Schubert T, Cutler AF. [13C]urea breath test to confirm eradication of Helicobacter pylori. Am J Gastroenterol. 1995;90:224–6. [PubMed] [Google Scholar]
- 15.Mion F, Rousseau M. Diagnostic test to document Helicobacter pylori eradication. Gastroenterology. 1996;110:324–5. doi: 10.1053/gast.1996.v110.agast960324b. [DOI] [PubMed] [Google Scholar]
- 16.Eggers RH, Kulp A, Tegeler R, et al. A methodological analysis of the 13C-urea breath test for the detection of Helicobacter pylori infections: High sensitivity and specificity with 30 min using 75 mg of 13C-urea. Eur J Gastroenterol Hepatol. 1990;2:437–44. [Google Scholar]
- 17.Logan R, Dill S, Bauer F, et al. The European 13C-urea breath test for the detection of Helicobacter pylori infection. Eur J Gastroenterol Hepatol. 1991;3:915–21. [Google Scholar]
- 18.Mion F, Delecluse HJ, Rosseau M, Berger F, Brazier JL, Minaire Y. [13C-urea breath test for the diagnosis of Helicobacter pylori infection. Comparison with histology] Gastroenterol Clin Biol. 1994;18:1106–11. [PubMed] [Google Scholar]
- 19.Mion F, Rosner G, Rousseau M, Minaire Y. 13C-urea breath test for Helicobacter pylori: Cut-off point determination by cluster analysis. Clinical Science (Lond) 1997;93:3–6. doi: 10.1042/cs0930003. [DOI] [PubMed] [Google Scholar]
- 20.Zambon CF, Basso D, Navaglia F, et al. Non-invasive diagnosis of Helicobacter pylori infection: Simplified 13C-urea breath test, stool antigen testing, or DNA PCR in human feces in a clinical laboratory setting? Clin Biochem. 2004;37:261–7. doi: 10.1016/j.clinbiochem.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 21.Hunt R, Fallone C, Veldhuyzen van Zanten S, et al. CHSG 2004 participants. Canadian Helicobacter Study Group Consensus Conference: Update on the management of Helicobacter pylori – an evidence-based evaluation of six topics relevant to clinical outcomes in patients evaluated for H pylori infection. Can J Gastroenterol. 2004;18:547–54. doi: 10.1155/2004/326767. [DOI] [PubMed] [Google Scholar]


