Transhepatic intubation, hepaticostomy, has been reported as an excellent palliative procedure for adenocarcinoma of the hepatic ducts. Hepaticostomy has also been advocated for benign strictures of the biliary ducts. Prolonged hepatic intubation has been extensively used at the University of Colorado and has been reported previously.
Customary techniques require either resection of the constricting lesion or dilation with Bakes dilators. The hepatic duct or ducts must then accommodate a large Bakes dilator, olive tipped stylet or Randall stone forceps. One of these instruments is then advanced along the dilated hepatic duct and finally pushed through the thinned hepatic parenchyma, existing through Glisson’s capsule. A Silastic, silicone rubber, tube is then attached and the dilator or forceps withdrawn back through the liver. The tubing then usually emerges from the hepatic duct trailing shreds of damaged duct. False passages or splitting of the duct at the hilus are particular hazards with this technique.
A most challenging patient with a constricted biliary tree secondary to a diffuse sclerosing adenocarcinoma of the bile duct necessitated the need for the technique to be described. We have since placed 15 tubes by this technique and have been impressed by its simplicity and ease in an otherwise rather disruptive procedure.
Instead of widely dilating the obstructing lesion, we will only dilate to a 3 millimeter Bakes dilator. This is primarily to locate the intrahepatic ducts. At this point, a Council stylet, which is malleable but slightly stiffer than a Bakes dilator, is bent into the same configuration as the Bakes dilator used in probing. The Council stylet is a basic urologic tool and readily available in all operating rooms. The stylet is then passed through the obstruction, out an appropriate duct and finally pushed through the thinned parenchyma and capsule. A filiform catheter is then screwed to the tip of the Council stylet and withdrawn back through the liver (Fig. 1). If more than one duct is to be intubated, a second filiform is placed in the appropriate duct in a similar manner at this time. The presence of the first existing filiform does not impair manipulation of the stylet in the hilum to the extent that the full sized hepaticostomy tube would.
Fig. 1.
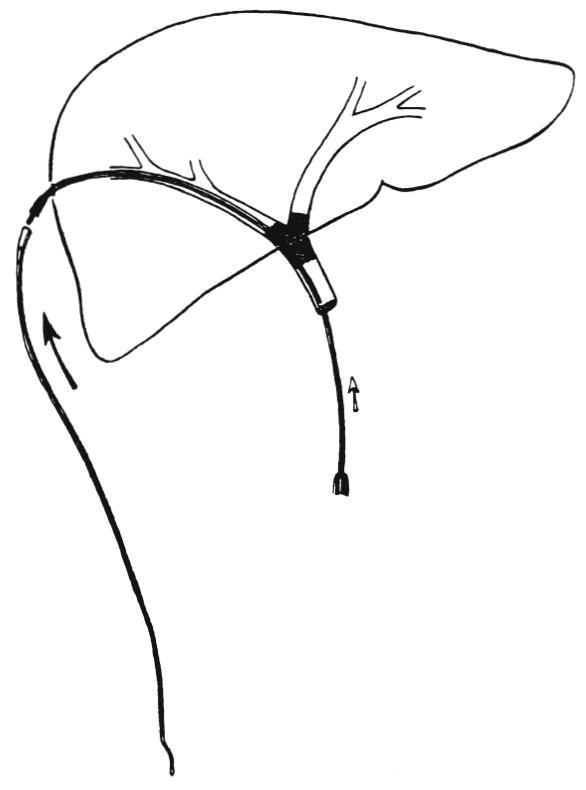
Council stylet is advanced out the hepatic duct and through thinned hepatic parenchyma. The filiform catheter is then attached to the tip of the stylet and withdrawn back through the liver.
With the filiform or filiforms in place, a urethral follower of appropriate size to accommodate the desired permanent tubing in its flared base is selected. This has usually been of 12F to 16F. The tubing is then secured within the base of the follower by a heavy suture transfixing both follower and tubing. The follower and attached tubing are then screwed into the filiform. By pulling the filiform through the liver, the follower gradually dilates the obstruction and the attached tubing glides through (Fig. 2). The filiform is usually threaded through the eye of a sponge forceps which is held over the exit site on Glisson’s capsule. This prevents the cutting of the parenchyma of the liver by inferior traction on the filiform.
Fig. 2.

The filiform follower and attached Silastic tubing are screwed into the base of the filiform. Filiform, follower and tubing are then pulled out through the hepatic parenchyma.
This technique, using readily available instruments, has permitted safe dilation and intubation of normal or even sclerotic ducts. The ability to place the two filiforms prior to placements of the larger tube has greatly facilitated insertion of the U tube or of multiple tubes.
Acknowledgments
This work was supported by research Grant Nos. MRIS 8118-01 and 7227-01 from the Veterans Administration, by Grant Nos. AM-17260 and AM-07772 from the National Institutes of Health and by Grant Nos. RR-00051 and RR-00069 from the General Clinical Research Centers Program of the Division of Research Resources, National Institutes of Health.
References
- Beart RW, Jr, Putnam CW, Starzl TE. Use of a U tube in the treatment of biliary disease. Surg Gynecol Obstet. 1976;142:913. [PMC free article] [PubMed] [Google Scholar]


