Abstract
OBJECTIVE
The goal of this study was to determine the prevalence of Severe Nausea and Vomiting of pregnancy/Hyperemesis Gravidarum among relatives of affected individuals.
STUDY DESIGN
Family history data were obtained on 1224 self-reported cases of hyperemesis gravidarum. Cases completed an online survey administered by the Hyperemesis Education and Research Foundation between 2003–2006.
RESULTS
Approximately 28% of cases reported their mother had severe nausea and vomiting or hyperemesis gravidarum while pregnant with them. Of the 721 sisters with a pregnancy history, 137 (19%) had hyperemesis gravidarum. Among the most severe cases, those requiring total parenteral nutrition or nasogastric feeding tube, the proportion of affected sisters was even higher, 49/198 (25%). Nine percent of cases reported having at least 2 affected relatives including sister(s), mother, grandmother, daughters, aunt(s), and cousin(s).
CONCLUSION
There is a high prevalence of severe nausea and vomiting of pregnancy/hyperemesis gravidarum among relatives of hyperemesis gravidarum cases in this study population. Because the incidence of hyperemesis gravidarum is most commonly reported to be 0.5%, this study provides strong but preliminary evidence for a genetic component to extreme nausea and vomiting of pregnancy.
Keywords: hyperemesis gravidarum, nausea, vomiting, pregnancy, genetic
INTRODUCTION
Hyperemesis Gravidarum (HG), severe nausea and vomiting of pregnancy, hospitalizes more than 59,000 pregnant women in the U.S. annually, with most authors reporting an incidence of 0.5%.1, 2 Estimates of severe nausea and vomiting of pregnancy vary greatly and range from 0.3% in a Swedish registry to as high as 10.8% in a Chinese registry of pregnant women.3, 4 Recent large population studies support ethnic variation in the incidence of HG. A Norwegian study of the Medical Birth Registry of Norway from 1967–2005, defined HG as persistent nausea and vomiting in pregnancy associated with ketosis and weight loss >5% of pre-pregnancy weight, and revealed an overall prevalence of 0.9%, but when broken down by ethnicity, found HG in 2.2% of 3,927 Pakastani women and 1.9% of 1,997 Turkish women, both more than twice the incidence of 0.9% in 798,311 Norwegian women.5 A study of California birth and death certificates after 20 weeks gestation linked to neonatal hospital discharge data in 1999 with the primary diagnosis of hyperemesis found an incidence 0.5% (2,466 cases out of 520,739 births), and women with HG were reportedly significantly less likely to be white or hispanic compared to non-whites or non-hispanics.6 A Canadian study found HG in 1,270 (0.8%) out of 156,091 of women with singleton deliveries between 1988 and 2002.7 This rate was confirmed in a second Canadian study during the same timeframe of the population-based Nova Scotia Atlee Perinatal Database of deliveries at 20 weeks gestation, that found 1,301 (0.8%) out of 157,922 pregnancies.8 Asian populations tend to have higher incidence rates. For example, a Malaysian study identified 192 recorded cases (3.9%) out of 4,937 maternities.9 Additionally, a study of 3,350 singleton deliveries in an Eastern Asian population observed HG in 119 (3.6%) of the population.10 As mentioned, a study of 1,867 singleton live births revealed the highest rate of severe nausea and vomiting of pregnancy in Shanghai, China, from 1986 to 1987, with an incidence of 10.8%. However, unlike the other studies mentioned, this study was based on a clinical record of severe vomiting on prenatal care cards, rather than hospitalization for HG, did not limit itself to a primary diagnosis of HG and included, for example, women with chronic liver disease, chronic hypertension, chronic renal illness, and preeclampsia.4
Hyperemesis Gravidarum is the most common cause of hospitalization in the first half of pregnancy and is second only to preterm labor for pregnancy overall.11 HG can be associated with serious maternal and fetal morbidity such as Wernicke’s encephalopathy12, fetal growth restriction, and even maternal and fetal death.6,13
A biologic component to the condition has been suggested from animal studies. Anorexia of early pregnancy has been observed in various mammals including monkeys.14 In dogs, anorexia can be accompanied by vomiting and can be severe enough to require pregnancy termination.15
Several lines of evidence support a genetic predisposition to nausea and vomiting in pregnancy (NVP). Firstly, in the only study of NVP in twins, concordance rates were more than twice as high for monozygotic compared to dizygotic twins.16 Secondly, several investigators have noted that siblings and mothers of patients affected with NVP are more likely to be affected than siblings and mothers of unaffected individuals.17,18 Thirdly, the higher frequency of severe NVP in patients with certain genetically-determined conditions such as defects in taste sensation,19,20 glycoprotein hormone receptor defects,21–23 or latent disorders in fatty acid transport or mitochondrial oxidation, 24,25 suggests that some portion of HG cases may be related to discrete, genetically transmitted disease states that are unmasked or exacerbated in pregnancy. Overall, these data suggest that genetic predisposition may play a role in the development of nausea and vomiting of pregnancy.
METHODS
Study subjects were women who completed an online survey administered by the Hyperemesis Education and Research (HER) Foundation (www.HelpHER.org) between 2003 and 2006 and who reported that they had experienced HG during one or more pregnancies. Study subjects were required to register for the survey by answering the question “Have you ever experienced severe nausea or vomiting (HG) while pregnant? HG is characterized by significant weight loss and debility, and typically requires medications and/or IV fluids for treatment.” Subjects that answered “YES” to this question and also answered that they lost weight below their pre-pregnancy weight were included in the study. Survey participants who answered “NO” to this question and/or participants who reported no weight loss in any pregnancy were excluded.
The survey included questions on demographics (age, ethnicity, level of education), diagnoses made by a physician or midwife (HG, morning sickness, other), treatments (including total parenteral nutrition (TPN), nasogastric feeding (NG) tube, and intravenous (IV) fluids), and family history (including number of biological sisters who had been pregnant, number who had hyperemesis, other relatives who had HG or severe NVP, and the experience of the participant’s mother (classified as HG, severe NVP, normal NVP, no NVP, or unknown) while pregnant with the participant.
The prevalence of HG among participants’ sisters was calculated as the number of sisters with HG divided by the number of sisters who had ever been pregnant. Sisters were stratified based on treatment received by the participant as a proxy for disease severity. The prevalence of HG among sisters of participants with more vs. less severe disease was compared by reporting p-values from a logistic model with standard errors adjusted for intra-family correlation.
This study was approved by the Institutional Review Board of the University of Southern California.
RESULTS
Demographic characteristics of the 1224 participants are shown in Table 1. The vast majority of participants were non-Hispanic white with at least some college education. Nearly all resided in an English-speaking country, with the majority (78%) in the United States. Age at survey ranged from 20 to 62, with the average being 32 years. Most participants were within five years of their most recent birth at the time of completion of the survey.
Table 1.
Respondants to the HER Survey: 1224 self-reported cases of HG
| Demographics | ||
|---|---|---|
| Race/ethnicity | ||
| White | 1075 (88%) | |
| African | 41 (3%) | |
| Hispanic | 47 (4%) | |
| Asian | 15 (1%) | |
| Mixed/other | 46 (4%) | |
| Country of Residence | ||
| USA | 952 (78%) | |
| Great Britain / Ireland | 109 (9%) | |
| Australia / New Zealand | 65 (5%) | |
| Canada | 45 (4%) | |
| Other | 51 (4%) | |
| Education | ||
| High School or less | 103 (8%) | |
| Some College | 391 (32%) | |
| College Degree | 395 (32%) | |
| Pursing Grad degree | 99 (8%) | |
| Masters Degree | 181 (15%) | |
| Doctoral Degree | 55 (4%) | |
| Age at Survey | ||
| mean (SD) | 32.2 (5.5) | |
| range | 20 – 62 | |
| Years post last birth at Survey | ||
| < 1 year | 258 (21%) | |
| 1 year | 313 (26%) | |
| 2 – 4 years | 415 (34%) | |
| 5 – 9 years | 161 (13%) | |
| 10 or more years | 77 (6%) | |
Among the 1224 participants reporting a history of HG, 1025 (84%) reported having been diagnosed with HG by a medical professional. Most were treated for severe nausea and vomiting, either by IV fluids (925/1224, 76%), feeding tube (292/1224, 24%), and/or by hospitalization (766/1224, 63%). These clinical characteristics are summarized in Table 2.
Table 2.
Respondants to the HER Survey: 1224 self-reported cases of HG
| Clinical characteristics | ||
|---|---|---|
| Diagnosed with HG by a Health Professional* | ||
| Yes | 1025 (84%) | |
| No | 199 (16%) | |
| Hospitalized* | ||
| Yes | 766 (63%) | |
| No | 458 (37%) | |
| IV fluids* | ||
| Yes | 925 (76%) | |
| No | 299 (24%) | |
| NG tube or TPN* | ||
| Yes | 292 (24%) | |
| No | 932 (76%) | |
For any of the woman's pregnancies
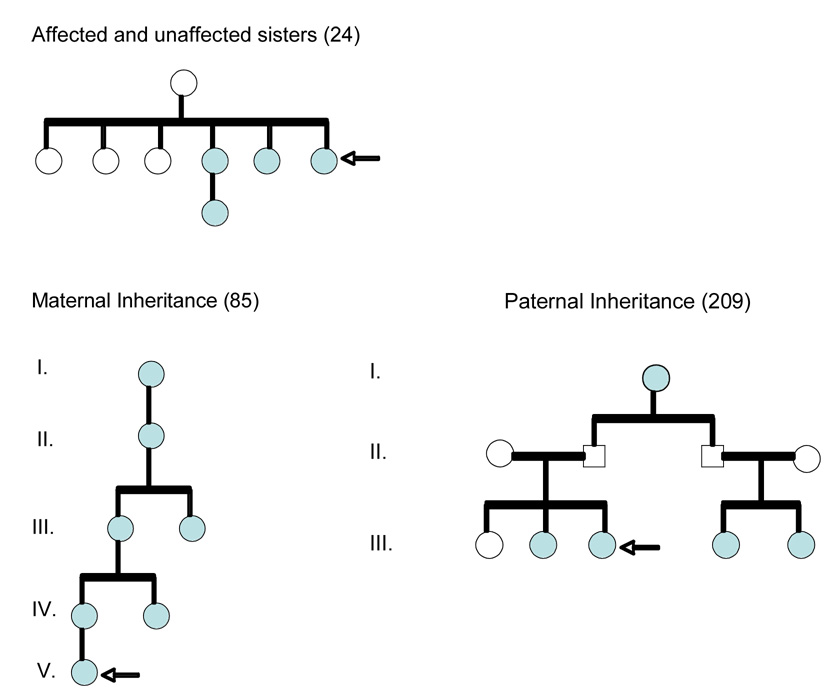
Twenty-eight percent (348/1224) of participants reported that their mother had experienced severe NVP or HG while pregnant with them. A strong family history of HG (two or more affected relatives) was reported by 109/1224 (9%) of participants. Some examples of pedigrees are shown in Figure 1. The survey did not ask participants specifically to distinguish between maternal or paternal secondary relatives with HG (eg. affected aunts, cousins), but approximately equal numbers of cases volunteered in a text box, the maternal (N=19) or paternal (N=21) lineage of their affected secondary relatives.
Figure 1.
Family 24 shows 3 out of 6 sisters affected, and one niece. Families 85 and 209 suggest HG can be inherited through the maternal or the paternal line. Arrows point to the affected proband and filled circles are family members reportedly affected with HG.
Of the 1224 participants, 504 had at least one sister with a prior pregnancy. The 504 women reported on the following pre-existing conditions: 36% reported premenstrual syndrome, 30% allergies, 30% motion sensitivity (car sickness), 21% migraines, 11% chronic depression, 7% infertility, 7% chronic anxiety, 6% inner ear disorder, 2% eating disorder, and 2% reported gall bladder disease. None of the pre-existing conditions correlated significantly with having a family history of HG. Among these participants, 266 commented on the week of pregnancy they were first treated for HG by hospitalization and/or medication. The average gestational age at time of first treatment in the first pregnancy reported was 8.6 weeks. In addition to hyperemesis gravidarum, several pregnancy conditions were reported in the first reported pregnancy including hypersalivation (25%), gastrointestinal reflux disease (22%), anemia (18%), severe constipation (18%), vomiting blood (15%), and neurologic symptoms (difficulty walking, talking, balance; 7%). None of the reported pregnancy conditions correlated significantly with family history. Among the 504 informative women, 331 reported more than one pregnancy, and among these, 307 (96%) reported at least one recurrence, with 84% (1104 pregnancies out of 1309 pregnancies) reported to be HG pregnancies.
The 504 participants reported on the pregnancy history of 721 sisters. With respect to sisters, the questionnaire specifically asked about hyperemesis gravidarum (in contrast to severe NVP). Prevalence of HG among sisters of participants was 19%, with 137/721 affected sisters (Table 3). When stratifying based on treatment received by the participant, prevalence was highest for sisters of those who were treated with total parenteral nutrition (TPN) or nasogastric feeding (NG) (49/198, 25%). Three out of three sets of identical twins reported their twin also had HG.
Table 3.
Prevalence of HG in sisters with a pregnancy history
| Respondants | Prevalence | P value |
|---|---|---|
| All | 137/721 = 19% | |
| HG dx | 115/595 = 19% | |
| No HG dx | 22/126 = 17% | 0.68 |
| Hospitalized | 103/490 = 21% | |
| Not Hospitalized | 34/231 = 15% | 0.09 |
| IV fluids | 108/562 = 19% | |
| No IV fluids | 29/159 = 18% | 0.81 |
| NG or TPN | 49/198=25% | |
| No NG or TPN | 88/523 = 17% | 0.09 |
COMMENT
This study demonstrates a remarkably high prevalence of HG among relatives of HG cases. The prevalence is higher among sisters of cases that require more aggressive treatments, suggesting affected familial prevalence increases with the severity of nausea and vomiting of pregnancy. Although we realize that shared environmental risk factors can also contribute to the observed high prevalence of affected family members, to our knowledge no such factors have been identified. In addition, although sisters commonly have a similar in-utero and childhood environment, it is unlikely that they share the same environment during their own pregnancy, when HG occurs. This study also suggests mothers and daughters commonly share severe nausea of pregnancy and it is unlikely that this can be entirely explained by shared cross-generational environmental factors. Reports in this study of half-siblings reared in separate states and identical twins pregnant and diagnosed with HG while residing in different countries, although anecdotal, lend further support to a role for genetics. The pedigrees presented in this study, the fact that mothers and sisters are commonly affected, and the relatively equal numbers of maternal and paternal secondary relatives affected, suggest that, HG may be inherited in an autosomal dominant manner with incomplete penetrance, although other modes of inheritance in some families can not be ruled out. Regardless of the mode of inheritance, this is the first report to show a high prevalence of affected family members for hyperemesis gravidarum, and along with a previous study showing higher concordance for nausea and vomiting in monozygotic vs. dizygotic twins16 provides support for a genetic contribution to severe nausea and vomiting of pregnancy.
HG often leads to extreme weight loss and may result in a state of nutrient deprivation, malnutrition, and starvation for both the mother and the developing fetus. Fetal outcome remains controversial. Some studies suggest infants exposed to HG in utero are significantly more likely to be born earlier, weigh less, be small for gestational age, and die between 24–30 weeks gestation than infants not so exposed.6 Other studies show that these associated outcomes are only significant in cases with hyperemesis and low pregnancy weight gain7, and that, if treated early, severe nausea may be associated with a protective effect against major malformations.26 While few long-term studies of HG offspring have been conducted, there is a body of literature on starvation in pregnancy in humans and animals, providing convincing evidence that nutritional deprivation in utero, can have lasting or lifelong significance.27 These data, along with the evidence of a familial component to HG, suggest that healthcare providers should be vigilant in identifying and treating women with a family history of HG.
While our data implicate a strong maternal genetic component, other observations suggest that additional risk factors may influence severity of NVP. An increased incidence of HG has been reported with multiple gestations, gestational trophoblastic disease, fetal chromosomal abnormalities and central nervous system malformations, and for mothers of female offspring.8,28 While smoking during pregnancy was recently reported to decrease the risk of hyperemesis, smoking by the partner was reported to increase the risk.4,8 Other than second-hand smoke, to our knowledge, no environmental factors have been identified that increase risk. Non-genetic maternal factors such as advanced maternal age have been associated with decreased risk, and adolescent pregnancy with increased risk for HG.29,30 Finally, evidence for a paternal and fetal contribution are controversial. While one study suggested that HG recurrence decreases with a change in partner, suggesting paternal genes expressed in the fetus may play a role, this conclusion was recently refuted by a separate study.31,32 Additionally, a consanguinity study also found no increased risk of HG, suggesting recessive fetal genes may not be involved in HG risk.5
A major strength of this study stems from the collaboration with the HER Foundation, which allowed collection of family history information on a large sample of women affected by HG. To date, most studies of hyperemesis gravidarum have been small case series or population studies relying on hospital databases with no information on family history. Thus this study is the first report of its kind.
Admittedly, this study has some methodological concerns. One potential limitation arises from the use of an internet-based survey. While internet-based research is quickly becoming scientifically recognized as a reliable recruiting tool, the study population consists only of cases with internet-access, and thus may represent women of higher education and income. We feel, however, that the generalizability of our study results should be reasonably good since we have no reason to suspect that education level and income would affect the likelihood of having a family history of HG.
Another limitation is that both proband HG status and family history of HG were based on self-reports, which can lead to misclassification of disease status and/or family history. However, we believe it would be highly unlikely for women in the most severe subgroup that required TPN or NG tube to misclassify their disease status and that of affected family members, and the results in this group were even stronger (25% sisters affected) than the participants as a whole (19% sisters affected).
Finally, the Internet-based survey on the HER Foundation website selected for participation only women self-reporting HG, without recruiting a control group. Thus, this study relies on comparing the reported incidence of family history to previous published reports. Because the incidence of hyperemesis gravidarum is most commonly reported to be 0.5%, this study provides strong but preliminary evidence for a genetic component to extreme nausea and vomiting of pregnancy. Future studies using a control group are warranted to determine the true familial relative risk of HG.
In summary, this study provides strong, but preliminary, evidence that maternal genetic susceptibility plays a role in the development of severe nausea and vomiting of pregnancy. This report is meant to serve as preliminary evidence of a familial component to HG and to focus needed attention on this incapacitating condition of pregnancy. Future work should focus on reproducing these results in other populations and on the identification of genetic variants that may contribute to HG susceptibility. Identification of genetic factors will elucidate the biology of nausea and vomiting in pregnancy and allow novel therapeutics to be developed to treat the cause of the disease rather than the symptoms.
Acknowledgements
We thank Dr. Frederic Paik Schoenberg, UCLA Dept of Statistics, for his valuable contribution to the creation and implementation of the original survey instrument. This research was supported (in part) by the Intramural Research Program of the National Institute of Child Health and Human Development, NIH, DHHS.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONDENSATION
This report demonstrates a high prevalence of severe nausea and vomiting among relatives of hyperemesis gravidarum cases suggesting a genetic component to the pregnancy condition.
REFERENCES
- 1.Jiang HG, Elixhauser A, Nicholas J, Steiner C, Reyes C, Brierman AS. Care of women in U.S. Hospitals, 2000. Rockville, MD: Agency for Healthcare Research and Quality; 2002. HCUP Fact Book No. 3. AHRQ Pub. No. 02-0044. [Google Scholar]
- 2.Verberg MF, Gillott DJ, Al-Fardan N, Grudzinskas JG. Hyperemesis gravidarum, a literature review. Hum Reprod Update. 2005 Sep–Oct;11(5):527–539. doi: 10.1093/humupd/dmi021. [DOI] [PubMed] [Google Scholar]
- 3.Kallen B. Hyperemesis during pregnancy and delivery outcome: a registry study. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 1987;26(4):291–302. doi: 10.1016/0028-2243(87)90127-4. [DOI] [PubMed] [Google Scholar]
- 4.Zhang J, Cai WW. Severe vomiting during pregnancy: antenatal correlates and fetal outcomes. Epidemiology. 1991 Nov;2(6):454–457. [PubMed] [Google Scholar]
- 5.Grjibovski AM, Vikanes A, Stoltenberg C, Magnus P. Consanguinity and the risk of hyperemesis gravidarum in Norway. Acta Obstet Gynecol Scand. 2007 Oct;12:1–6. doi: 10.1080/00016340701709273. [DOI] [PubMed] [Google Scholar]
- 6.Bailit JL. Hyperemesis gravidarum: Epidemiologic findings from a large cohort. American Journal of Obstetrics and Gynecology. 2005;193:811–814. doi: 10.1016/j.ajog.2005.02.132. [DOI] [PubMed] [Google Scholar]
- 7.Dodds L, Fell DB, Joseph KS, Allen VM, Butler B. Outcomes of pregnancies complicated by hyperemesis gravidarum. Obstet Gynecol. 2006 Feb;107(2 Pt 1):285–292. doi: 10.1097/01.AOG.0000195060.22832.cd. [DOI] [PubMed] [Google Scholar]
- 8.Fell DB, Dodds L, Joseph KS, Allen VM, Butler B. Risk factors for hyperemesis gravidarum requiring hospital admission during pregnancy. Obstetrics and Gynecology. 2006;107(2):277–284. doi: 10.1097/01.AOG.0000195059.82029.74. Part 1. [DOI] [PubMed] [Google Scholar]
- 9.Tan PC, Jacob R, Quek KF, Omar SZ. The fetal sex ratio and metabolic, biochemical, haematological and clinical indicators of severity of hyperemesis gravidarum. BJOG. 2006 Jun;113(6):733–737. doi: 10.1111/j.1471-0528.2006.00947.x. [DOI] [PubMed] [Google Scholar]
- 10.Matsuo K, Ushioda N, Nagamatsu M, Kimura T. Hyperemesis gravidarum in Eastern Asian population. Gynecol Obstet Invest. 2007;64(4):213–216. doi: 10.1159/000106493. [DOI] [PubMed] [Google Scholar]
- 11.Gazmararian JA, Petersen R, Jamieson DJ, Schild L, Adams MM, Deshpande AD, Franks AL. Hospitalizations during pregnancy among managed care enrollees. Obstetrics and Gynecology. 2002;100:94–100. doi: 10.1016/s0029-7844(02)02024-0. [DOI] [PubMed] [Google Scholar]
- 12.Chiossi G, Neri I, Cavazutti M, Basso G, Fucchinetti F. Hyperemesis gravidarum complicated by Wernicke’s encephalopathy: background, case report and review of the literature. Obstetrics and Gynecology Survey. 2006;61:255–268. doi: 10.1097/01.ogx.0000206336.08794.65. [DOI] [PubMed] [Google Scholar]
- 13.Fairweather DVI. Nausea and vomiting in pregnancy. American Journal of Obstetrics and Gynecology. 1968;102(1):135–175. doi: 10.1016/0002-9378(68)90445-6. [DOI] [PubMed] [Google Scholar]
- 14.Czaja JA. Food rejection by female rhesus monkeys during the menstrual cycle and early pregnancy. Physiology and Behavior. 1975;14(5):579–587. doi: 10.1016/0031-9384(75)90185-7. [DOI] [PubMed] [Google Scholar]
- 15.Hoskins J. How to manage the pregnant bitch. DVM News. 2003 Retrieved from http://www.dvmnewsmagazine.com/dvm/article/articleDetail.jsp?id=70328&pageID=2.
- 16.Corey LA, Berg K, Solaas MH, Nance WE. The epidemiology of pregnancy complications and outcome in a Norwegian twin population. Obstetrics and Gynecology. 1992;80(6):989–994. [PubMed] [Google Scholar]
- 17.Gadsby R, Barnie-Adshead AM, Jagger C. Pregnancy nausea related to women’s obstetric and personal histories. Gynec Obstet Invest. 1997;43:108–111. doi: 10.1159/000291833. [DOI] [PubMed] [Google Scholar]
- 18.Vellacott ID, Cooke EJA, James CE. Nausea and vomiting in early pregnancy. International Journal of Gynecology and Obstetrics. 1988;27:57–62. doi: 10.1016/0020-7292(88)90088-4. [DOI] [PubMed] [Google Scholar]
- 19.Sipiora ML, Murtaugh MA, Gregoire MD, Duffy VB. Bitter taste perception and severe vomiting in pregnancy. Physiology and Behavior. 2000;69:259–267. doi: 10.1016/s0031-9384(00)00223-7. [DOI] [PubMed] [Google Scholar]
- 20.Bartoshuk LM, Duffy VB, Reed D, Williams A. Supertasting, ear-aches,and head injury: genetics and pathology alter our taste worlds. Appetite. 2002;38:45–51. doi: 10.1016/0149-7634(95)00042-d. [DOI] [PubMed] [Google Scholar]
- 21.Rodien P, Jordan N, Lefevre A, Royer J, Vasseur C, Savagner F, Bourdelot A, Rohmer V. Abnormal stimulation of the thyrotrophin receptor during gestation. Human Reproductive Update. 2004;10:95–105. doi: 10.1093/humupd/dmh008. [DOI] [PubMed] [Google Scholar]
- 22.Rodien P, Bremont C, Raffin Sanson M, Parma J, Van Sande J, Costalgia S, Luton J, Vassart G, Duprez L. Familial gestational hyperthyroidism caused by a mutant thyrotropin receptor hypersensitive to human chorionic gonadotropin. New England Journal of Medicine. 1998;339(25):1823–1826. doi: 10.1056/NEJM199812173392505. [DOI] [PubMed] [Google Scholar]
- 23.Akerman FM, Zhenmin L, Rao CV, Nakajim ST. A case of spontaneous ovarian hyperstimulation syndrome with a potential mutation in the hCG receptor gene. Fertility and Sterility. 2000;74:403–404. doi: 10.1016/s0015-0282(00)00628-2. [DOI] [PubMed] [Google Scholar]
- 24.Innes AM, Seargeant LE, Balachandra K, Roe CR, Wanders RJ, Ruiter JP, Casiro O, Grewar DA, Greenberg CR. Hepatic carnitine palmitoyltransferase I deficiency presenting as maternal illness in pregnancy. Pediatric Research. 2000;47:43–45. doi: 10.1203/00006450-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Outlaw WM, Ibdah JA. Impaired fatty acid oxidation as a cause for liver disease associated with hyperemesis gravidarum. Medical Hypotheses. 2005;65:1150–1153. doi: 10.1016/j.mehy.2005.05.035. [DOI] [PubMed] [Google Scholar]
- 26.Seto A, Einarson T, Koren G. Pregnancy outcome following first trimester exposure to antihistamines: meta-analysis. Am J Perinatol. 1997 Mar;14(3):119–124. doi: 10.1055/s-2007-994110. [DOI] [PubMed] [Google Scholar]
- 27.Painter RC, Roseboom TJ, Bleker OP. Prenatal exposure to the Dutch famine and disease in later life: an overview. Reproductive Toxicology. 2005;20:345–352. doi: 10.1016/j.reprotox.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 28.Eliakim R. Hyperemesis Gravidarum: a current review. American Journal of Perinatology. 2000;17(4):207–218. doi: 10.1055/s-2000-9424. [DOI] [PubMed] [Google Scholar]
- 29.Klebanoff MA, Koslowe PA, Kaslow R, Rhodes GG. Epidemiology of vomiting in early pregnancy. Obstetrics and Gynecology. 1985;66:612–616. [PubMed] [Google Scholar]
- 30.Depue RH, Bernstein L, Ross RK, Judd HL, Henderson BE. Hyperemesis gravidarum in relation to estradiol levels, pregnancy outcome, and other maternal factors: a seroepidemiologic study. American Journal of Obstetrics and Gynecology. 1987;156:1137–1141. doi: 10.1016/0002-9378(87)90126-8. [DOI] [PubMed] [Google Scholar]
- 31.Trogstad LI, Stoltenberg C, Magnus P, Skjaerven R, Irgens LM. Recurrence risk in hyperemesis gravidarum. British Journal of Obstetrics and Gynecology. 2005 Dec;112(12):1641–1645. doi: 10.1111/j.1471-0528.2005.00765.x. [DOI] [PubMed] [Google Scholar]
- 32.Einarson TR, Navioz Y, Maltepe C, Einarson A, Koren G. Existence and severity of nausea and vomiting in pregnancy (NVP) with different partners. J Obstet Gynaecol. 2007 May;27(4):360–362. doi: 10.1080/01443610701327362. [DOI] [PubMed] [Google Scholar]