Abstract
Cancer is one of the major leading causes of death all over the world. Primary and secondary bone tumors can significantly deteriorate the quality of life (QOL) and the activity of daily living (ADL) of the patients. These unwelcome diseases become a social and economic burden seriously. Thus, more effective therapies for both primary and secondary bone tumors are actually required. Bone homeostasis depends on the strictly balanced activities between bone formation by osteoblasts and bone resorption by osteoclasts. Imbalance of bone formation and resorption results in various bone diseases. Both primary and secondary bone tumors develop in the unique environment bone, it is therefore necessary to understand bone cell biology in tumoral bone environment. Recent findings strongly revealed the significant involvement of the receptor activator of nuclear factor κB ligand (RANKL)/RANK/osteoprotegerin (OPG) triad, the key regulators of bone remodeling in bone oncology. Indeed, RANKL/RANK blocking successfully prevented the development of bone metastases. Furthermore, some cancer cells express RANK which is involved in tumor cell migration. Thus, the regulation of this triad will be a rational, encouraged therapeutic hot spot in bone oncology. In this review, we summarize the accumulating knowledge of the RANKL/RANK/OPG triad and discuss about its therapeutic capability in primary and secondary bone tumors.
Keywords: Bone Neoplasms, drug therapy, metabolism, pathology, secondary, Humans, Osteoprotegerin, physiology, RANK Ligand, physiology, Receptor Activator of Nuclear Factor-kappa B, physiology
Keywords: RANKL, RANK, OPG, Cancer, Bone Metastasis, Osteoclast, Vicious Cycle, Osteosarcoma
Introduction
Nowadays, cancer is one of the major leading causes of death worldwide. Because of the improvement of primary cancer site control by significant advance in the treatment, cancer bone metastases become significant problem for patients with cancers. Bone is well-known target organ of cancer metastasis as well as the lungs and the liver. Indeed, around 350,000 patients with bone metastases die annually in the United States [1]. Bone metastases result in severe pain, pathological fractures, nerve palsy, and hypercalcemia [2] that can markedly deteriorate the quality of life (QOL) and the activity of daily living (ADL) of the patients. Once tumors metastasize to bone, they are usually incurable. For example, only 20 % of patients with breast cancer are still alive in 5-year time point after the discovery of bone metastasis [3]. Thus, the social and economic burden of this disease is increasing steadily. We therefore consider that one of the main targets of cancer treatment in the near future is the control of bone metastases. Primary bone tumors such as osteosarcoma are also significant concerns as well as secondary one (metastases). The survival of osteosarcoma patients is closely associated with the response of the tumor cells to anti-mitotic drugs and the presence of pulmonary metastasis [4–7].
Thus, more effective and more safety therapies for both primary and secondary bone tumors are badly required. Both primary and secondary bone tumors develop in the unique environment bone, it is therefore necessary to understand bone cell biology in tumoral bone environment.
Bone is always and continuously remodeled. The bone homeostasis depends on the strictly balanced activities between bone formation by osteoblasts and bone resorption by osteoclasts [8, 9]. The discovery of the key factors involved in bone remodeling has moved bone research into a new era. Most notable of these factors belong to the tumor necrosis factor (TNF)/TNF receptor family are receptor activator of nuclear factor κB ligand (RANKL/TNFSF11), its cognate receptor RANK (TNFRSF11A) and decoy receptor for RANKL, osteoprotegerin (OPG/TNFRSF11B) [10–13]. Consequently, RANKL mediates osteoclastogenesis and activates mature osteoclasts, whereas OPG negatively regulates RANKL binding to RANK, reduces the half-life of membranous RANKL, therefore inhibits bone resorption induced by osteoclasts [14]. Current findings have revealed that the RANKL/RANK/OPG triad is the key regulator not only for normal but also pathological bone metabolism [14–26]. Thus, the RANKL level is increased in osteolytic lesions associated with malignant tumors [22], whereas the OPG level is increased in osteoblastic lesions [23]. In fine, local RANKL/OPG ratio determines local bone feature.
Bone is a good environment for the colonization and progression of bone metastases. It has been suggested that cancer cells produce soluble factors that activate directly (RANKL) or indirectly via osteoblasts [parathyroid hormone-related peptide (PTH-rP), IL-8, etc.] osteoclast differentiation and maturation [27–30]. During the bone degradation, osteoclasts release tumor supportive growth factors stocked in the mineralized bone matrix (insulin-like growth factor-1, fibroblast growth factor, etc.) [31]. This vicious cycle has been proposed to explain the tumor development in bone [32]. Together with the essential role of the RANKL/RANK/OPG triad in osteoclastogenesis, inhibition of osteoclastogenesis and osteoclast activities by RANKL/RANK blocking constitutes a potential novel approach to maintain skeletal integrity. Indeed, RANKL/RANK blocking by soluble RANK (sRANK) or OPG successfully prevented the development of bone metastases [12, 13].
Alternatively, it has very recently reported functional RANK expression on some bone-associated tumor cells [33–38]. Indeed, the migration of RANK-positive tumor cells was induced by RANKL stimulation [20, 36, 39–41]. Taken together, these observations suggest that increased RANKL expression in tumoral bone environment may be a promoting factor of bone tumor development. Anatomically, immune and bone cells interact and influence each other in the bone marrow cavity. Recently, the term ‘osteoimmunology’ was coined to identify the collaboration field of bone biology and immunology [42]. ‘Osteoimmunology’ is remarkably noted and more and more important to understand the pathogenesis and to build up new therapies of bone disease. We therefore consider that the RANKL/RANK/OPG triad is a hot spot as a therapeutic device in the field of bone oncology.
In this review, we summarize the accumulating knowledge of the RANKL/RANK/OPG triad and discuss about its therapeutic capability in bone tumors.
1. Primary bone tumors
1.1. Giant Cell Tumor
Giant cell tumor (GCT), a rare primary osteolytic neoplasm, is characterized by bone destruction [43]. It consists of osteoclast-like giant cells, stromal cells and CD68+ monocytes [44, 45]. The stromal cells are considered as a neoplastic factor of GCT, since they keep proliferation in culture and positive for the proliferation marker, Ki67 [45]. The stromal cells are one of the osteoblastic lineages [45–47] and are thought to support the recruitment and formation of mature osteoclasts from its precursor cells [33]. The bone resorption by osteoclasts causes the destructive osteolysis and results in morbidity in patients with GCT [48]. Previous studies have shown that the spindle-shaped stromal-like mononuclear cells of GCT are the most likely candidate cells for the tumor’s neoplastic component [43, 49–51]. In addition, RANK expression was confined ~60% of CD45+CD14+ cells in GCT, strongly implying that these are committed as osteoclast precursors [33]. However, there is no significant evidence that tumor cells of GCT themselves can induce bone destruction [52]. Instead, tumor cells of GCT recruits multinucleated osteoclast-like giant cells and consequently promotes tumor-induced osteolysis [43, 53–55]. RANKL mRNA expression has been detected in GCT using RT-PCR, in situ hybridization [33, 56] and immunofluorescence staining [57]. The stromal cells within GCT samples had increased RANKL/OPG ratio compared to that of non-osteolytic bone tumors [33]. Moreover, addition of exogenous OPG to cultured GCT cells inhibited bone resorption and osteoclast formation [57]. Thus, GCT represent a paradigm for the direct promotion of both osteoclast formation and activity by tumor cells via the RANKL/RANK/OPG system [56, 57]. The RANKL/RANK/OPG system will be an appropriate therapeutic target for inhibiting bone resorption peculiar to the patients with GCT.
1.2. Osteosarcoma
Osteosarcoma, the most frequent primary malignant bone tumor is defined as a malignant tumor originates from mesenchymal cells characterized by the direct malignant osteoid and/or woven bone formation by tumor cells [58], approximately 1000 new cases are seen per year in North America and a similar number in Europe [59]. Although several important pathogenetic roles of p53, RB and mdm2 have been already reported [60], the pathogenesis of osteosarcoma and the role of the osteosarcoma in bone microenvironment are not fully understood. The survival of the patients with osteosarcoma has significantly improved over the past several decades by aggressive chemotherapy treatment [4]. Indeed, survival of osteosarcoma patients estimates around 60–70% in the non-metastatic condition [4]; however 20–30% with metastatic [5], and 10–30% in the relapse or recurrent conditions [6, 7]. Thus, understanding of the biological mechanisms that govern osteosarcoma growth at the molecule level should be essential for the devising new strategies. Similarly to other bone tumors, osteosarcoma is strongly associated with deregulated RANKL/RANK/OPG balance that leads to pathological bone futures [61, 62]. Indeed, Grimaud et al. demonstrated an increase of the serum RANKL/OPG ratio in the patients with high grade osteosarcoma [62]. In recent attractive study, OPG treatment achieved not only the prevention of osteosarcoma-induced osteolysis but also the inhibition of associated tumor development that improved survival rate in OPG-treated animals [63]. This study failed to demonstrate direct effect of OPG on tumor cells; the authors concluded that the anti-tumor effect of OPG was indirect effect. Contraly, functional RANK expression in osteosarcoma has been recently reported in a mouse osteosarcoma cell line (POS-1 cells) [34] and several human osteosarcoma cell lines (Saos-2, MG-63 and MNNG/HOS) [35]. One of the likely explanations of this discrepancy may be a heterogynous population of osteosarcoma cells used in these studies. Interestingly, RANKL directly and significantly modulated cancer-related genes expression in RANK-positive Saos-2 cells without change of tumor cells migration and proliferation [36]. RANK is also detected in more than 50% of human osteosarcoma specimens studied with a preferential expression on osteosarcoma developed in bad responders to chemotherapy evaluated by Huvos score [35]. These all findings indicate that the RANKL/RANK/OPG triad is strongly involved in osteosarcoma biology. RANKL-induced cancer-related gene modulations in osteosarcoma cell line, Saos-2 included both tumor supportive and tumor protective one. In addition, except for the direct effect of RANKL on RANK-positive osteosarcoma cells, RANKL could protect tumor development, since it can act as a potent immune activator by inhibiting dendritic cell apoptosis [64]. Further experiments are needed to determine the real impact of RANKL on osteosarcoma; however RANK is undoubtedly hopeful and unprecedented therapeutic target of RANK-positive osteosarcoma.
2. Metastatic bone tumors
Metastatic cancer is the most common type of bone malignancy, and the skeleton is the third most common site for metastases following the liver and the lungs [65, 66]. Malignant bone lesions may be characterized by abnormal bone formation, bone loss or both [3, 66]; however osteolytic pattern is more common in patients suffering from bone metastases.
2.1. Multiple Myeloma
Multiple myeloma (MM), a plasma cell malignancy is the second most common adult hematologic malignancy, and is the most common cancer with skeleton as its primary site. MM affects 70,000 people in the United States, with 15,000 new cases accruing yearly, accounts for 1 to 2% of cancer-related death [67]. MM induces osteolysis and shifts the balance of bone remodeling toward bone resorption [68]. The pure osteolytic feature observed in MM is very different from other cancer bone metastases in which bone destruction is followed by new bone formation. Even if MM patients response to anti-MM therapies, they may still have progression of skeletal events without repair of osteolytic lesions [69, 70]. These patients frequently require radiation therapy, surgery and use of analgesics to overcome pain as well as improve their QOL. As a result, diffuse osteopenia, focal osteolytic lesions, pathologic fractures and hypercalcemia are represented clinical manifestations in patients with MM and are key causes of morbidity and mortality [71]. Thus, the control of osteolysis is very important in MM treatment.
Current reports suggested that the RANKL/RANK/OPG triad is significantly involved in myeloma bone disease. Recent characterization of osteoclast-activating factors (OAFs), Dickkopf-1 and the RANKL/RANK/OPG triad have provided a better understanding of myeloma bone disease at the molecular level. These OAFs include interleukin (IL)-1, IL-6, IL-11, TNF, macrophage inflammatory protein-1, hepatocyte growth factor (HGF), PTH-rP and others [72–78]. There is still considerable debate whether these bone-resorbing cytokines are produced by the tumor cells, accessory cells or both [67]. MM has been shown to exhibit high levels of RANKL and low levels of OPG [69]. Together with HGF and PTH-rP, OAFs increase expression of RANKL on the marrow stromal cell surface. The potent stimulatory effects of RANKL on osteoclastogenesis are usually counteracted by secreted OPG, which acts as a safeguard mechanism for bone destruction; however OPG mRNA expression is markedly decreased in MM. Several reports revealed that cell-cell contact of myeloma cells with both bone marrow stromal cells and osteoblasts suppress mRNA and protein expression of OPG [79, 80]. Finally, the balance between RANKL and OPG shifts in favor of bone resorption. Thus, improving RANKL/OPG ratio toward normal ratio and/or RANKL/RANK blocking will prevent pure osteolytic feature seen in the MM patients and contribute to improve their QOL.
2.2. Other solid Cancers
Breast cancer is the major cause of death among women in worldwide [81]. Bone metastasis occurs in 16–73% of breast cancer patients. Breast cancer keenly metastasizes to bone and forms osteolytic lesions, but the factors supporting breast cancer growth in bone remain unknown. Bone destruction seen in breast cancer bone metastases is mediated either directly by tumor cells or indirectly by osteoclasts [82, 83]. Contrary, prostate cancer is the most common cancer diagnosed in men, currently the major leading cause of cancer death in men [1, 84]. Prostate cancer bone metastases are observed in approximately 80% of the patients with prostate cancer and represent the most serious complication of advanced stage, frequently causing significant morbidity and mortality [1, 84]. Unlike other solid tumors that are associated with osteolytic features, prostate cancer bone metastases present an overall increase in both bone remodeling and bone volume [73]. Recent findings strongly suggested the importance of osteoclast function in osteoblastic tumors as well as osteolytic tumors [74–79]; however the mechanisms underlining these processes are not fully determined.
Accumulating data clearly revealed the significant involvement of the RANKL/RANK/OPG triad in metastatic bone cancers including breast and prostate cancer bone metastases [16, 20, 41, 88, 93, 94–97]. Indeed, current studies have disclosed that blocking of RANKL/RANK interaction prevented the progression of both breast and prostate cancer in bone [88–91, 92, 93]. These anti-tumor effects were uniquely observed in bone, not in other tissues such as subcutaneous [88, 89]. Thus, it has been considered that the anti-tumor effect of RANKL/RANK blocking results of the inhibition of osteoclast activity [41].
Interestingly, breast and prostate cancer bone metastases preferentially present respectively osteolytic and osteoblastic features, however both cancer cells express functional RANK [37, 36–8]. We [41] and Jones et al. [36] demonstrated that human breast cancer cellss (MDA-MB231, Hs578T, MCF7) and human prostate cancer cells (DU145, PC3, LNCaP) express functional RANK. Moreover, mouse melanoma cell line (B16F10), originate from another cell lineage also express functional RANK [36]. RANK expressed on these cancer cells does not change cancer cell proliferation; however it clearly induces cancer cell migration [20, 36, 39, 41, 96]. Thus, it is possible that bone-specific anti-tumor effect by RANKL/RANK blocking in breast and prostate cancer bone metastases is, at least in part, the result of direct effect on these RANK-positive tumor cells. In breast cancer, a positive correlation has been reported between constant expression of RANK with decreased/absent expression of RANKL and a high metastatic phenotype [40]. Taken together, RANK-positive cells are starving RANKL and preferentially attracted by RANKL rich bone environment, where RANKL acts as a ‘soil’ factor that facilitates bone metastases development by activating both kinds of RANK-positive cells (osteoclasts/osteoclast precursors and RANK-positive cancer cells). These findings are all consistent with a high trend of breast and prostate cancer bone metastases. RANKL/RANK blocking should be recommended as a therapeutic target even if they have no influence on cell proliferation or survival, since these agents can inhibit tumor cell migration. The therapeutic benefits of bitherapy associating anti-bone resorption and anti-tumoral agents in abrogating tumor recurrence have been reported in bone metastases and primary bone tumors [98, 99]. RANK expressed on these tumor cells therefore appeared as a novel therapeutic target.
Summary and future trends
As above mentioned, tumor and bone cells significantly interact each other and result in pathological bone features. In this process, bone degradation by osteoclasts plays a crucial role in bone tumor development and control of local osteoclast activity can provide a potential therapeutic strategy. There is no doubt that the cytotoxic drugs inducing direct tumor cell death and surgery remains the first line for debulking tumors. However, new therapy targeting the RANK/RANKL/OPG triad will provide anti-tumor effect via different pathways, mainly blocking vicious cycle which resides between bone degradation and tumor cells. Such therapy may be used in combined setting with conventional therapeutic approaches (Fig. 1).
Figure 1.
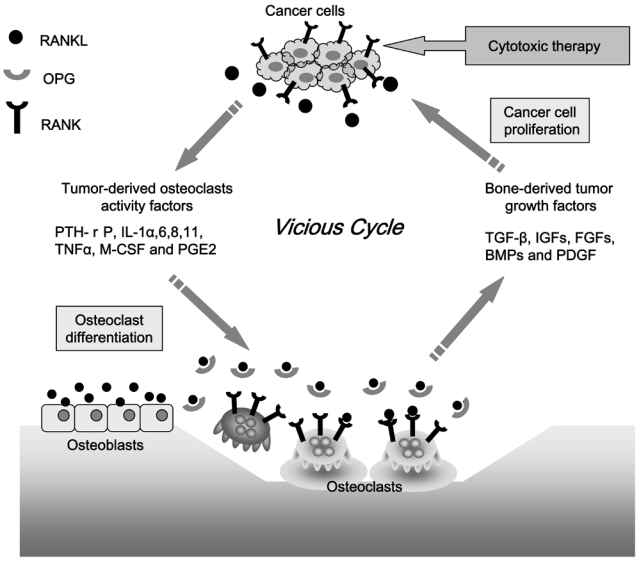
The vicious cycle accelerates osteolysis and cancer cell proliferation. Cancer cells (A) increase the expression of RANKL in osteoblasts by secreting parathyroid hormone-related peptide (PTH-rP), (B) directly express RANKL and (C) secrete osteoblast activity factors such as interleukin (IL)-1α, 6, 8, 11, tumor necrosis factor-α (TNF-α), macrophage colony-stimulating factor (M-CSF), and prostaglandin E2 (PGE2). In bone resorption, growth factors like insulin-like growth factors (IGFs), fibroblast growth factors (FGFs), platelet-derived growth factor (PDGF) and bone morphogenetic proteins (BMPs) released from the bone matrix promote cancer cell proliferation. In addition to the cytotoxic drugs and surgery, a new therapy targeting the RANKL/RANK/OPG triad can show direct or indirect anti-tumor effect by blocking vicious cycle between osteolysis and cancer cells.
Since Paget has suggested his ‘seed and soil’ theory in 1880’s [100], the specific involving factors have been unknown for a long time. We suggest that, at least in bone metastases, RANKL acts as a ‘soil’ factor that facilitates bone metastases development by activating both kinds of RANK-positive cells (osteoclasts/osteoclast precursors and RANK-positive cancer cells) in tumoral bone environment. However, further studies are needed to determine how RANKL is involved in the recruitment of RANK-positive tumor cells to RANKL rich bone environment. Concerning primary tumors like osteosarcoma, it appears that the biological function of RANK expressed on tumor cells is different from that of metastatic one and remains to be determined.
Alternatively, sRANK or OPG have been used to block RANKL/RANK signaling; however it should be prudent to use OPG. Since OPG is also a decoy receptor for TNF-related apoptosis inducing ligand (TRAIL), it exerts inhibitory effect on TRAIL-induced cancer cell apoptosis. OPG thus represents a survival factor for prostate cancer cells [25]. In this context, a fully human monoclonal antibody directed RANKL, denosumab (named AMG 162) has been developed and currently under phase III clinical trials. After the confirmation of the efficacy and safety of denosumab, this agent will be applicable to the RANKL/RANK blocking in cancer bone metastases therapy. Furthermore, RANKL/RANK/OPG triad has an impact on immune response. Thus, RANKL/RANK signaling is essential for lymph node organogenesis [101]. RANKL/OPG are also strongly associated with the biology of dendritic cells expressing RANK. RANKL inhibits dramatically the apoptosis of dendritic cells and induces T lymphocyte proliferation [102], while OPG might contribute to this control since OPG is expressed in dendritic cells and its expression is increased with their maturation [103]. Overall, the published data demonstrated that RANKL/OPG are key regulators of T lymphocyte – dendritic cell communications, modulating immunity and bone remodeling through dendritic cells [104]. Thus, the immunomodulatory functions of of OPG/RANK/RANKL also participate to their therapeutic interests.
In conclusion, the RANKL/RANK/OPG triad and its signaling hold a great promise for the treatment of malignant bone tumors. Further studies are needed to determine orchestrated anti-tumor effect of these agents by inhibiting osteoclast activity, tumor migration and immunomodulation as well as those safeties.
References
- 1.Mundy GR. Metastasis to bone: Causes, consequences and therapeutic opportunities. Nat Rev Cancer. 2002;2:584–93. doi: 10.1038/nrc867. [DOI] [PubMed] [Google Scholar]
- 2.Coleman RE. Skeletal complications of malignancy. Cancer. 1997;80:1588–94. doi: 10.1002/(sici)1097-0142(19971015)80:8+<1588::aid-cncr9>3.3.co;2-z. [DOI] [PubMed] [Google Scholar]
- 3.Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27:165–76. doi: 10.1053/ctrv.2000.0210. [DOI] [PubMed] [Google Scholar]
- 4.Meyers PA, Schwartz CL, Krailo M, Kleinerman ES, Betcher D, Bernstein ML, Conrad E, Ferquson W, et al. Osteosarcoma: a randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J Clin Oncol. 2005;23(9):2004–11. doi: 10.1200/JCO.2005.06.031. ** The pivotal clinical trial in osteosarcoma with L-MTP-PE that demonstrated safety, efficacy of L-MTP-PE. [DOI] [PubMed] [Google Scholar]
- 5.Bielack SS, Kempf-Bielack B, Delling G, Exner GU, Fleqe S, Helmke K, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Cli Oncol. 2002;20(3):776–90. doi: 10.1200/JCO.2002.20.3.776. [DOI] [PubMed] [Google Scholar]
- 6.Hawkins DS, Arndt CA. Pattern of disease recurrence and prognostic factors in patients with osteosarcoma treated with contemporary chemotherapy. Cancer. 2003;98(11):2447–56. doi: 10.1002/cncr.11799. [DOI] [PubMed] [Google Scholar]
- 7.Anderson P. Osteosarcoma relapse: expect the worst, but hope for the best. Pediatr Blood Cancer. 2006;47(3):231. doi: 10.1002/pbc.20615. [DOI] [PubMed] [Google Scholar]
- 8.Felix R, Hofstetter W, Cecchini MG. Recent developments in the understanding of the pathophysiology of osteopetrosis. Eur J Endocrinol. 1996;134:143–56. doi: 10.1530/eje.0.1340143. [DOI] [PubMed] [Google Scholar]
- 9.Karsent G, Wagner EF. Reaching a genetic and molecular understanding of skeletal development. Dev Cell. 2002;2:389–406. doi: 10.1016/s1534-5807(02)00157-0. [DOI] [PubMed] [Google Scholar]
- 10.Yasuda H, Shima N, Nakagawa N, Yamaguchi K, Kinosaki M, Mochizuki S, Tomoyasu A, Yano K, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci USA. 1998;95:3597–3602. doi: 10.1073/pnas.95.7.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93:165–76. doi: 10.1016/s0092-8674(00)81569-x. [DOI] [PubMed] [Google Scholar]
- 12.Anderson DM, Maraskovsky E, Billingsley WL, Dougall WC, Tometsko ME, Roux ER, Teepe MC, DuBose RF, et al. A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature. 1997;390:175–9. doi: 10.1038/36593. [DOI] [PubMed] [Google Scholar]
- 13.Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Luthy R, Nguyen HQ, Wooden S, et al. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997;89:309–19. doi: 10.1016/s0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]
- 14.Tat SK, Padrines M, Theoleyre S, Couillaud-Battaglia S, Heymann D, Rédini F, Fortun Y. OPG/membranous-RANKL complex is internalized via the clathrin pathway before a lysosomal and a proteasomal degradation. Bone. 2006;39:706–15. doi: 10.1016/j.bone.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 15.Goltzman D. Osteolysis and cancer. J Clin Invest. 2001;107:1219–20. doi: 10.1172/JCI13073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown JM, Corey E, Lee ZD, True LD, Yun TJ, Tondravi M, Vessella RL. Osteoprotegerin and rank ligand expression in prostate cancer. Urology. 2001;57:611–6. doi: 10.1016/s0090-4295(00)01122-5. [DOI] [PubMed] [Google Scholar]
- 17.Granchi D, Amato I, Battistelli L, Avnet S, Capaccioli S, Papucci L, Donnini M, Pellacani A, et al. In vitro blockade of receptor activator of nuclear factor-kappaB ligand prevents osteoclastogenesis induced by neuroblastoma cells. Int J Cancer. 2004;111:829–38. doi: 10.1002/ijc.20308. [DOI] [PubMed] [Google Scholar]
- 18.Farrugia AN, Atkins GJ, To LB, Pan B, Horvath N, Kostakis P, Findlay DM, Bardy P, et al. Receptor activator of nuclear factorkappaB ligand expression by human myeloma cells mediates osteoclast formation in vitro and correlates with bone destruction in vivo. Cancer Res. 2003;63:5438–45. [PubMed] [Google Scholar]
- 19.Nosaka K, Miyamoto T, Sakai T, Mitsuya H, Suda T, Matsuoka M. Mechanism of hypercalcemia in adult T-cell leukemia: Overexpression of receptor activator of nuclear factor kappaB ligand on adult T-cell leukemia cells. Blood. 2002;99:634–40. doi: 10.1182/blood.v99.2.634. [DOI] [PubMed] [Google Scholar]
- 20.Chen G, Sircar K, Aprikian A, Potti A, Goltzman D, Rabbani SA. Expression of RANKL/RANK/OPG in primary and metastatic human prostate cancer as markers of disease stage and functional regulation. Cancer. 2006;107:289–98. doi: 10.1002/cncr.21978. [DOI] [PubMed] [Google Scholar]
- 21.Perez-Martinez FC, Alonso V, Sarasa JL, Nam-Cha SG, Vela-Navarrete R, Manzarbeitia F, Callahora FJ, Esbrit P. Immunohistochemical analysis of low-grade and high-grade prostate carcinoma: Relative changes of PTHrP and its PTH1 receptor, osteoprotegerin and receptor activator of nuclear factor kb ligand. J Clin Pathol. 2007;60(3):290–4. doi: 10.1136/jcp.2006.037853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michigami T, Ihara-Watanabe M, Yamazaki M, Ozono K. Receptor activator of nuclear factor kappaB ligand (RANKL) is a key molecule of osteoclast formation for bone metastasis in a newly developed model of human neuroblastoma. Cancer Res. 2001;61:1637–44. [PubMed] [Google Scholar]
- 23.Lee Y, Schwarz E, Davies M, Jo M, Gates J, Wu J, Zhang X, Lieberman JR. Differences in the cytokine profiles associated with prostate cancer cell induced osteoblastic and osteolytic lesions in bone. J Orthop Res. 2003;21:62–72. doi: 10.1016/S0736-0266(02)00095-5. [DOI] [PubMed] [Google Scholar]
- 24.Holen I, Cross SS, Neville-Webbe HL, Cross NA, Balasubramanian SP, Croucher PI, Evans CA, Lippitt JM, et al. Osteoprotegerin (OPG) expression by breast cancer cells in vitro and breast tumours in vivo—a role in tumour cell survival? Breast Cancer Res Treat. 2005;92:207–15. doi: 10.1007/s10549-005-2419-8. [DOI] [PubMed] [Google Scholar]
- 25.Holen I, Croucher PI, Hamdy FC, Eaton CL. Osteoprotegerin (OPG) is a survival factor for human prostate cancer cells. Cancer Res. 2002;62:1619–23. [PubMed] [Google Scholar]
- 26.Van Poznak C, Cross SS, Saggese M, Hudis C, Panageas KS, Norton L, Coleman RE, Holen I. Expression of osteoprotegerin (OPG), TNF related apoptosis inducing ligand (TRAIL), and receptor activator of nuclear factor {kappa}B ligand (RANKL) in human breast tumours. J Clin Pathol. 2006;59:56–63. doi: 10.1136/jcp.2005.026534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grano M, Mori G, Minielli V, Cantatore FP, Colucci S, Zallone AZ. Breast cancer cell line MDA-231 stimulates osteoclastogenesis and bone resorption in human osteoclasts. Biochem Biophys Res Commun. 2000;270:1097–100. doi: 10.1006/bbrc.2000.2569. [DOI] [PubMed] [Google Scholar]
- 28.Wani MR, Fuller K, Kim NS, Choi Y, Chambers T. Prostaglandin E2 cooperates with TRANCE in osteoclast induction from hemopoietic precursors: synergistic activation of differentiation, cell spreading, and fusion. Endocrinology. 1999;140:1927–35. doi: 10.1210/endo.140.4.6647. [DOI] [PubMed] [Google Scholar]
- 29.Guise TA, Yin JJ, Taylor SD, Kumagai Y, Dallas M, Boyce BF, Yoneda T, Mundy GR. Evidence for a causal role of parathyroid hormone- related protein in the pathogenesis of human breast cancer-mediated osteolysis. J Clin Invest. 1996;98:1544–9. doi: 10.1172/JCI118947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shen X, Falzon M. PTH-related protein modulates PC-3 prostate cancer cell adhesion and integrin subunit profile. Mol Cell Endocrinol. 2003;199:165–77. doi: 10.1016/s0303-7207(02)00287-3. [DOI] [PubMed] [Google Scholar]
- 31.Pfeilschifter J, Mundy GR. Modulation of type β transforming growth factor activity in bone cultures by osteotropic hormones. Proc Natl Acad Sci USA. 1987;84:2024–8. doi: 10.1073/pnas.84.7.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Halvorson KG, Sevcik MA, Ghilardi JR, Rosol TJ, Mantyh PW. Similarities and differences in tumor growth, skeletal remodeling and pain an osteolytic and osteoblastic model of bone cancer. Clin J Pain. 2006;22:587–600. doi: 10.1097/01.ajp.0000210902.67849.e6. [DOI] [PubMed] [Google Scholar]
- 33.Atkins GJ, Hayes DR, Graves SE, Evadokiou A, Hay S, Bouralexis S, Findlay DM. Expression of osteoclast differentiation signals by stromal elements of giant cell tumors. J Bone Miner Res. 2000;15:640–9. doi: 10.1359/jbmr.2000.15.4.640. [DOI] [PubMed] [Google Scholar]
- 34.Wittrant Y, Lamoureux F, Mori K, Riet A, Kamijo A, Heymann D, Rédini F. RANKL directly induces bone morphogenetic protein-2 expression in RANK-expressing POS-1 osteosarcoma cells. Int J Oncol. 2006;28:261–9. [PubMed] [Google Scholar]
- 35.Mori K, Le Goff B, Berreur M, Riet A, Moreau A, Blanchard F, Chevalier C, Guisle-Marsollier I, et al. Human osteosarcoma cells express functional receptor activator nuclear factor-kappaB. J Pathol. 2007;211:555–62. doi: 10.1002/path.2140. [DOI] [PubMed] [Google Scholar]
- 36.Jones DH, Nakashima T, Sanchez OH, Kozieradzki I, Komarova SV, Sarosi I, Morony S, Rubin E, et al. Regulation of cancer cell migration and bone metastasis by RANKL. Nature. 2006;440:692–6. doi: 10.1038/nature04524. [DOI] [PubMed] [Google Scholar]
- 37.Thomas RJ, Guise TA, Yin JJ, Elliott J, Horwood NJ, Martin TJ, Gillespie MT. Breast cancer cells interact with osteoblasts to support osteoclast formation. Endocrinology. 1999;140:4451–8. doi: 10.1210/endo.140.10.7037. [DOI] [PubMed] [Google Scholar]
- 38.Tometsko M, Armstrong A, Miller R, Jones J, Chaisson M, Branstetter D. RANK ligand directly induces osteoclastogenic, angiogenic, chemoattractive and invasive factors on RANK-expressing human cancer cells MDAMB-231 and PC3. J Bone Miner Res. 2004;19(S25) [Google Scholar]
- 39.Mori K, Berreur M, Blanchard F, Chevalier C, Guisle-Marsollier I, Masson M, Rédini F, Heymann D. Receptor activator nuclear factor-κB ligand (RANKL) directly modulates the gene expression profile of RANK-positive Saos-2 human osteosarcoma cells. Oncol Rep. 2007;18(6):1365–71. [PubMed] [Google Scholar]
- 40.Bhatia P, Sanders MM, Hansen MF. Expression of receptor activator of nuclear factor-kappaB is inversely correlated with metastatic phenotype in breast carcinoma. Clin Cancer Res. 2005;11:162–5. [PubMed] [Google Scholar]
- 41.Mori K, Goff BL, Charrier C, Battaglia S, Heymann D, Rédini F. DU145 human prostate cancer cells express functional receptor activator of NFκB: New insights in the prostate cancer bone metastasis process. Bone. 2007;40:981–90. doi: 10.1016/j.bone.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 42.Arron JR, Choi Y. Bone versus immune system. Nature. 2000;408:535–6. doi: 10.1038/35046196. [DOI] [PubMed] [Google Scholar]
- 43.Zheng MH, Fan Y, Wysocki S, Lau ATT, Robertson T, Beilharz M, Wood DJ, Papadimitriou JM. Gene expression of transforming growth factor-β and its type II receptor in giant cell tumor of bone. Am J Pathol. 1994;145:1095–104. [PMC free article] [PubMed] [Google Scholar]
- 44.Golding SR, Roelke MS, Petrison KK, Bhan AK. Human giant cell tumor of bone: identification and characterisation of cell types. J Clin Invest. 1987;79:483–91. doi: 10.1172/JCI112838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wulling M, Kaiser E. The origin of the neoplastic stromal cell in giant cell tumor of bone. Hum Pathol. 2003;34:983–93. doi: 10.1053/s0046-8177(03)00413-1. [DOI] [PubMed] [Google Scholar]
- 46.Joyner CJ, Quinn JM, Triffit JT, Owen ME, Athanasou NA. Phenotypic characterisation of mononuclear and multinucleated cells of giant cell tumor of bone. Bone Miner. 1992;16:37–48. doi: 10.1016/0169-6009(92)90820-4. [DOI] [PubMed] [Google Scholar]
- 47.James IE, Dodds RA, Olivera DL, Nuttall ME, Gowen M. Human osteoclastoma-derived stromal cells: correlation of the ability to form mineralized nodules in vitro with formation of bone in vivo. J Bone Miner Res. 1996;11:1453–60. doi: 10.1002/jbmr.5650111012. [DOI] [PubMed] [Google Scholar]
- 48.Boyle WJ, Simonet SW, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423:337–42. doi: 10.1038/nature01658. [DOI] [PubMed] [Google Scholar]
- 49.Golding SR, Roelke MS, Petrison KK, Bhan AK. Human giant cell tumor of bone: identification and characterisation of cell types. J Clin Invest. 1987;79:483–91. doi: 10.1172/JCI112838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Athanasou NA, Bliss E, Gatter KC, Heryet A, Wood CG, McGee JOD. An immunohistological study of giant cell tumor of bone: evidence for an osteoclast origin of the giant cells. J Pathol. 1985;147:153–8. doi: 10.1002/path.1711470302. [DOI] [PubMed] [Google Scholar]
- 51.Zheng MH, Siu P, Papadimitriou JM, Wood DJ, Murch A. Telomeric fusion is a major cytogenetic aberration of spindle-shaped mononuclear cells derived from giant cell tumor of bone. Pathology. 1999;31:373–8. doi: 10.1080/003130299104756. [DOI] [PubMed] [Google Scholar]
- 52.Zheng MH, Fan Y, Wysocki S, Wood DJ, Papadimitriou JM. Detection of mRNA carbonic anhydrase II in human osteoclast-like cells by in situ hybridisation. J Bone Miner Res. 1993;8:113–8. doi: 10.1002/jbmr.5650080114. [DOI] [PubMed] [Google Scholar]
- 53.Zheng MH, Fan Y, Smith A, Wysocki S, Papadimitriou JM, Wood DJ. Gene expression of monocyte chemoattractant protein-1 in giant cell tumors of bone osteoclastoma: possible involvement in CD681 macrophage- like cell migration. J Cell Biochem. 1998;70:121–9. [PubMed] [Google Scholar]
- 54.Rosai J. In: Ackerman’s Surgical Pathology. 8. Rosai J, editor. St. Louis: Mosby; 1957. pp. 61–1996. [Google Scholar]
- 55.Wittrant Y, Theoleyre S, Chipoy C, Padrines M, Blanchard F, Heymann D, Rédini F. RANKL/RANK/OPG: new therapeutic targets in bone tumours and associated osteolysis. Biochimica et Biophysica Acta. 2004;1704:49–57. doi: 10.1016/j.bbcan.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 56.Huang L, Xu J, Wood DJ, Zheng MH. Gene expression of osteoprotegerin ligand, osteoprotegerin, and receptor activator of NF-kappa B in giant cell tumor of bone: possible involvement in tumor cell-induced osteoclast-like cell formation. Am J Pathol. 2000;156:761–7. doi: 10.1016/s0002-9440(10)64942-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atkins GJ, Bouralexis S, Haynes DR, Graves SE, Geary SM, Evdokiou A, Zannettino AC, Hay S, et al. Osteoprotegerin inhibits osteoclast formation and bone resorbing activity in giant cell tumors of bone. Bone. 2001;28:370–7. doi: 10.1016/s8756-3282(01)00404-5. [DOI] [PubMed] [Google Scholar]
- 58.Herzog CE. Overview of sarcomas in the adolescent and young adult population. J Pediatr Hematol Oncol. 2005;27(4):215–8. doi: 10.1097/01.mph.0000161762.53175.e4. [DOI] [PubMed] [Google Scholar]
- 59.Stiller CA, Bielack SS, Jundt G, Steliarova-Foucher E. Bone tumours in European children and adolescents, 1978–1997. Report from the Automated Childhood Cancer Information System project. Eur J Cancer. 2006;42(13):2124–35. doi: 10.1016/j.ejca.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 60.Miller CW, Aslo A, Won A, Tan M, Lampkin B, Koeffler HP. Alterations of the p53, Rb and MDM2 genes in osteosarcoma. J Cavcer Res Clin Oncol. 1996;122:559–65. doi: 10.1007/BF01213553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Terpos E, Szydlo R, Apprley JF, Hatjiharissi E, Politou M, Meletis J, Viniou N, Yataganas X, et al. Soluble receptor activator of nuclear factor kappaB ligand-osteoprotegerin ratio predicts survival in multiple myeloma: proposal for a novel prognostic index. Blood. 2003;102:1064–9. doi: 10.1182/blood-2003-02-0380. [DOI] [PubMed] [Google Scholar]
- 62.Grimaud E, Soubigou L, Couillaud S, Coipeau P, Moreau A, Passuti N, Gouin F, Rédini F, et al. Receptor activator of nuclear factor kappaB ligand (RANKL)/osteoprotegerin (OPG) ratio is increased in severe osteolysis. Am J Pathol. 2003;163:2021–31. doi: 10.1016/s0002-9440(10)63560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lamoureux F, Richard P, Wittrant Y, Battaglia S, Pilet P, Trichet V, Blanchard F, Gouin F, et al. Therapeutic relevance of osteoprotegerin gene therapy in osteosarcoma: blockade of the vicious cycle between tumor cell proliferation and bone resorption. Cancer Res. 2007;67(15):7308–18. doi: 10.1158/0008-5472.CAN-06-4130. [DOI] [PubMed] [Google Scholar]
- 64.Wong BR, Josien R, Lee SY, Sauter B, Li HL, Steinman RM, Choi Y. TRANCE [tumor necrosis factor (TNF)-related activation-induced cytokine], a new TNF family member predominantly expressed in T cells, is a dendritic cell-specific survival factor. J Exp Med. 1997;186:2075–80. doi: 10.1084/jem.186.12.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am. 2000;31:515–28. doi: 10.1016/s0030-5898(05)70171-1. [DOI] [PubMed] [Google Scholar]
- 66.Clines GA, Guise TA. Hypercalcaemia of malignancy and basic research on mechanisms responsible for osteolytic and osteoblastic metastasis to bone. Endocr Relat Cancer. 2005;12:549–83. doi: 10.1677/erc.1.00543. [DOI] [PubMed] [Google Scholar]
- 67.Oyajobi BO. Multiple myeloma/hypercalcemia. Arthritis Res Ther. 2007;9(Suppl 1):S4. doi: 10.1186/ar2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mundy GR, Bertoline DR. Bone destruction and hypercalcemia in plasma cell myeloma. Semin Oncol. 1986;13:291–9. [PubMed] [Google Scholar]
- 69.Belch AR, Bergsagel DE, Wilson K, O’Reilly S, Wilson J, Sutton D, Pater J, Johnston D, et al. Effect of daily etidronate on the osteolysis of multiple myeloma. J Clin Oncol. 1991;9:1397–402. doi: 10.1200/JCO.1991.9.8.1397. [DOI] [PubMed] [Google Scholar]
- 70.Kyle RA, Jowsey J, Kelly PJ, Taves DR. Multiple-myeloma bone disease. The comparative effect of sodium fluoride and calcium carbonate or placebo. N Engl J Med. 1975;293:1334–8. doi: 10.1056/NEJM197512252932602. [DOI] [PubMed] [Google Scholar]
- 71.Kyle RA. Multiple myeloma, review of 869 cases. Mayo Clin Proc. 1975;50:29–40. [PubMed] [Google Scholar]
- 72.Cozzolino F, Torcia M, Aldinucci D, Rubartelli A, Miliani A, Shaw AR, Lansdorp PM, Di Guglielmo R. Production of interleukin-1 by bone marrow myeloma cells. Blood. 1989;74(1):380–7. [PubMed] [Google Scholar]
- 73.Kawano M, Tanaka H, Ishikawa H, Nobuyoshi M, Iwato K, Asaoku H, Tanabe O, Kuramoto A. Interleukin-1 accelerates autocrine growth of myeloma cells through interleukin-6 in human myeloma. Blood. 1989;73(8):2145–8. [PubMed] [Google Scholar]
- 74.Choi SJ, Cruz JC, Craig F, Chung H, Devlin RD, Roodman GD, Alsina M. Macrophage inflammatory protein 1-alpha is a potential osteoclast stimulatory factor in multiple myeloma. Blood. 2000;96:671. [PubMed] [Google Scholar]
- 75.Han JH, Choi SJ, Kurihara N, Koide M, Oba Y, Roodman GD. Macrophage inflammatory protein-1alpha is an osteoclastogenic factor in myeloma that is independent of receptor activator of nuclear factor κB ligand. Blood. 2001;97:3349–53. doi: 10.1182/blood.v97.11.3349. [DOI] [PubMed] [Google Scholar]
- 76.Abe M, Hiura K, Wilde J, Moriyama K, Hashimoto T, Ozaki S, Wakatsuki S, Kosaka M, et al. Role for macrophage inflammatory protein (MIP)-1alpha and MIP-1beta in the development of osteolytic lesions in multiple myeloma. Blood. 2002;100:2195–202. [PubMed] [Google Scholar]
- 77.Bataille R, Jourdan M, Zhang XG, Klein B. Serum levels of interleukin-6, a potent myeloma cell growth factor, as a reflection of disease severity in plasma cell dyscrasias. J Clin Invest. 1989;84:2008–11. doi: 10.1172/JCI114392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Seidel C, Borset M, Turesson I, Abildgaard N, Sundan A, Waage A. Elevated serum concentrations of hepatocyte growth factor in patients with multiple myeloma. Blood. 1998;91(806):12–2098. [PubMed] [Google Scholar]
- 79.Pearse RN, Sordillo EM, Yaccoby S, Wong BR, Liau DF, Colman N, Michaeli J, Epstein J, et al. Multiple myeloma disrupts the TRANCE/osteoprotegerin cytokine axis to trigger bone destruction and promote tumor progression. Proc Natl Acad Sci USA. 2001;98(20):11581–6. doi: 10.1073/pnas.201394498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Giuliani N, Bataille R, Mancini C, Lazzaretti M, Barille S. Myeloma cells induce imbalance in the osteoprotegerin/osteoprotegerin ligand system in the human bone marrow environment. Blood. 2001;98(13):3527–33. doi: 10.1182/blood.v98.13.3527. [DOI] [PubMed] [Google Scholar]
- 81.Ries LAG, Eisner MP, Kosary CL, et al. SEER cancer statistics review 1975–2000. Bethesda (MD): National Cancer Institute; 2003. [Google Scholar]
- 82.Kakonen SM, Mundy GR. Mechanism of osteolytic bone metastases in breast carcinoma. Cancer. 2003;97:834–9. doi: 10.1002/cncr.11132. [DOI] [PubMed] [Google Scholar]
- 83.Guise TA. Molecular mechanism of osteolytic bone metastases. Cancer. 2000;88:2892–8. doi: 10.1002/1097-0142(20000615)88:12+<2892::aid-cncr2>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 84.Landis SH, Murray T, Bolden S, Wingo PA. Cancer statistics. CA Cancer J Clin. 1999;49:8–31. doi: 10.3322/canjclin.49.1.8. [DOI] [PubMed] [Google Scholar]
- 85.Clarke NW, McClure J, George NJ. Morphometric evidence for bone resorption and replacement in prostate cancer. Br J Urol. 1991;68:74–80. doi: 10.1111/j.1464-410x.1991.tb15260.x. [DOI] [PubMed] [Google Scholar]
- 86.Garnero P, Buchs N, Zekri J, Rizzoli R, Coleman RE, Delmas PD. Markers of bone turnover for the management of patients with bone metastases from prostate cancer. Br J Cancer. 2000;82:858–64. doi: 10.1054/bjoc.1999.1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Inoue H, Nishimura K, Oka D, Nakai Y, Shiba M, Tokizane T, Arai Y, Nakayama M, et al. Prostate cancer mediates osteoclastogenesis through two different pathways. Cancer Lett. 2005;223:121–8. doi: 10.1016/j.canlet.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 88.Zhang J, Dai J, Qi Y, Lin DL, Smith P, Strayhorn C, Mizokami A, Fu Z, et al. Osteoprotegerin inhibits prostate cancer-induced osteoclastogenesis and prevents prostate tumor growth in the bone. J Clin Invest. 2001;107:1235–44. doi: 10.1172/JCI11685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang J, Dai J, Yao Z, Lu Y, Dougall W, Keller ET. Soluble receptor activator of nuclear factor κB Fc diminishes prostate cancer progression in bone. Cancer Res. 2003;63:7883–90. [PubMed] [Google Scholar]
- 90.Corey E, Brown LG, Kiefer JA, Quinn JE, Pitts TE, Blair JM, Vessella RL. Osteoprotegerin in prostate cancer bone metastasis. Cancer Res. 2005;65:1710–8. doi: 10.1158/0008-5472.CAN-04-2033. [DOI] [PubMed] [Google Scholar]
- 91.Whang PG, Schwarz EM, Gamradt SC, Dougall WC, Lieberman JR. The effects of RANK blockade and osteoclast depletion in a model of pure osteoblastic prostate cancer metastasis in bone. J Orthop Res. 2005;23:1475–83. doi: 10.1016/j.orthres.2005.05.004.1100230634. [DOI] [PubMed] [Google Scholar]
- 92.Mountzios G, Dimopoulos MA, Bamias A, Papadopoulos G, Kastritis E, Syrigos K, Pavlakis G, Terpos E. Abnormal bone remodeling process is due to an imbalance in the receptor activator of nuclear factor-kappaB ligand (RANKL)/osteoprotegerin (OPG) axis in patients with solid tumors metastatic to the skeleton. Acta Oncol. 2007;46(2):221–9. doi: 10.1080/02841860600635870. [DOI] [PubMed] [Google Scholar]
- 93.Canon JR, Roudier M, Bryant R, Morony S, Stolina M, Kostenuik PJ, Dougall WC. Inhibition of RANKL blocks skeletal tumor progression and improves survival in a mouse model of breast cancer bone metastasis. Clin Exp Metastasis. 2007 doi: 10.1007/s10585-007-9127-1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 94.Park HR, Min SK, Cho HD, Kim DH, Shin HS, Park YE. Expression of osteoprotegerin and RANK ligand in breast cancer bone metastasis. J Korean Med Sci. 2003;18:541–6. doi: 10.3346/jkms.2003.18.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cross SS, Harrison RF, Balasubramanian SP, Lippitt JM, Evans CA, Reed MWR, Holen I. Expression of receptor activator nuclear factor-κB ligand (RANKL) and tumor necrosis factor related, apoptosis inducing ligand (TRAIL) in breast cancer, ND their relations with osteoprotegerin, oestrogen receptor, and clinicopathological variables. J Clin Pathol. 2006;59:716–20. doi: 10.1136/jcp.2005.030031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Armstrong AP, Miller RE, Jones JC, Zhang J, Keller ET, Dougall WC. RANKL acts directly on RANK-expressing prostate tumor cells and mediates migration and expression of tumor metastasis genes. Prostate. 2008;68(1):92–104. doi: 10.1002/pros.20678. [DOI] [PubMed] [Google Scholar]
- 97.Li Y, Kucuk O, Hussain M, Abrams J, Cher ML, Sarkar FH. Antitumor and antimetastatic activities of docetaxel are enhanced by genistein through regulation of osteoprotegerin/receptor activator of nuclear factor-κB(RANK)/RANK ligand/MMP-9 signaling in prostate cancer. Cancer Res. 2006;66(9):4816–25. doi: 10.1158/0008-5472.CAN-05-3752. [DOI] [PubMed] [Google Scholar]
- 98.Holen I, Shipman CM. Role of osteoprotegerin (OPG) in cancer. Clin Sci. 2006;110:279–91. doi: 10.1042/CS20050175. [DOI] [PubMed] [Google Scholar]
- 99.Hiraga T, Ueda A, Tamura D, Hata K, Ikeda F, Williams PJ, Yoneda T. Effects of oral UFT combined with or without zoledronic acid on bone metastasis in the 4T1/luc mouse breast cancer. Int J Cancer. 2003;106:973–9. doi: 10.1002/ijc.11330. [DOI] [PubMed] [Google Scholar]
- 100.Paget S. The distrubution of secondary growths in cancer of the breast. Lancet. 1889;1:571–2. [PubMed] [Google Scholar]
- 101.Kong YY, Feige U, Sarosi I, Bolon B, Tafuri A, Morony S, Capprelli C, Li J, Elliott R, McCabe S, Wong T, Campagnuolo G, Moran E, Bogoch ER, Van G, Nguyen LT, Ohashi PS, Lacey DL, Fish E, Boyle WJ, Penninger JM. Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature. 1999;402:304–9. doi: 10.1038/46303. [DOI] [PubMed] [Google Scholar]
- 102.Wong BR, Josien R, Lee SY, Sauter B, Li HL, Steinman RM, Choi Y. TRANCE (tumor necrosis factor [TNF]-related activation-induced cytokine), a new TNF family member predominantly expressed in T cells, is a dendritic cell-specific survival factor. J Exp Med. 1997;186:2075–2080. doi: 10.1084/jem.186.12.2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schoppet M, Henser S, Ruppert V, Stubig T, Al-Fakhri N, Maisch B, Hofbauer LC. Osteoprotegerin expression in dendritic cells increases with maturation and is NF-kappaB-dependent. J Cell Biochem. 2007;100:1430–1439. doi: 10.1002/jcb.21129. [DOI] [PubMed] [Google Scholar]
- 104.Baud’huin M, Lamoureux F, Duplomb L, Rédini F, Heymann D. RANKL RANK Osteoprotegerin: key partners of osteoimmunology and vascular diseases. Cell Mol Life Sci. 2007;64:2334–2350. doi: 10.1007/s00018-007-7104-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


