Abstract
Objective
To longitudinally assess pharmacy and medical students' attitudes toward the medically underserved.
Methods
The Medical Students' Attitudes Toward the Underserved (MSATU) survey was administered to the entering classes at the schools of pharmacy and medicine at 2 universities in the South. This self-report measure was then completed by these students in each year of the professional curriculum. Data were compared longitudinally to assess students' attitudes toward the underserved.
Results
Pharmacy students' attitude scores towards the underserved remained relatively stable over time (MSATU attitudes scores: Year 1 = 45.2, Year 2 = 48.3, Year 4 = 45.7), while medical students' attitude scores declined significantly (MSATU attitudes scores: Year 1 = 55.5, Year 2 = 52.4, Year 4 = 46.4). No differences in scores were associated with gender.
Conclusion
This initial study comparing pharmacy and medical students' attitudes toward the underserved can serve as a baseline as healthcare professionals seek for solutions to better care for the medically underserved.
Keywords: attitudes, medical students, pharmacy students, underserved
INTRODUCTION
The 2006 Annual Social and Economic Supplement to the Current Population Survey reported that 47 million people (8.7 million children) were without health insurance.1 The statistics for uninsured non-Hispanic whites did not change significantly from 2005. However, the rates and numbers for uninsured African Americans and Hispanics increased. Minority populations, especially those with lower socioeconomic status, have poorer health outcomes.2-4 Academic health centers, although economically stressed, have a social contract to train competent professionals, improve health care access and quality, and grow their research enterprises prudently.5 Nurturing a commitment to service as part of medical professionalism is essential if we hope to address the health of those who have been marginalized in our health care system. Thus, educators must consider how service-learning experiences within the formal curricula can promote “responsible professionalism and personal sacrifice” fundamental to the practice of medicine.6,7
Because health care professionals frequently interact with uninsured or indigent patients, it is important to uncover explicit attitudes towards vulnerable groups before learners begin their professional careers and to determine when educational experiences should be implemented to influence positive change.7 Attention must be paid to the students' intention to perform services for these vulnerable patients and how these intentions are influenced by underlying attitudes. The theory of planned behavior, which is well supported by empirical evidence, espouses that “intentions to perform behaviors of different kinds can be predicted with high accuracy from attitudes toward the behavior, subjective norms, and perceived behavioral control…”8 However, the relationship between attitudes and clinical decision-making has not been well studied.
Pharmacy students' attitudes have been assessed concerning the elderly,9 mental illness,10 human immunodeficiency virus (HIV),11 pharmaceutical care,12 and changes resulting from the educational process itself.13-15 Twenty-five years ago, third-, fourth- and fifth-year pharmacy students' attitudes were assessed on various social factors: determinants of patients' health and illness, interpersonal relationships between health professional and patient, government's involvement in health care costs, and views on social problems outside of medicine.16 Each subsequent year, students' attitudes declined in concern for patients as individuals and increased in cynicism and anxiety. Although the study was cross-sectional, it illustrated that students' attitudes were less favorable in succeeding years.
Medical students' attitudes differ from entry to graduation,17 with considerable declines in idealism and tolerance after the first 2 years.7,18 Historically, interpretations of these findings have differed, although most educators would agree that medical school “constitutes a strong socializing experience.”19-23
Several studies have assessed medical students' attitudes about the elderly,24,25 patients with HIV,26,27 educational process changes,28-31 comprehensive medical care effects,32 and expectations of values and behaviors.33 There have been investigations by international colleagues concerning medical students' attitudes about social issues in medicine.34-39 Outcomes of these studies imply that attitudes toward social issues are global.
Although there is considerable interest in the health professions concerning lack of available care to underserved populations, there has been no longitudinal comparison of health professionals' attitudes toward this group. Because attitudes may predict behavior (intention to provide care), the objective of this study was to longitudinally assess pharmacy and medical students' attitudes toward the underserved. The primary research questions were: What are the attitudes of pharmacy and medical students toward the underserved? Do attitudes toward the underserved change as students progress through their respective professional programs? A secondary question was: Do women and men within each profession have different attitudes?18,40
METHODS
Participants were students enrolled in a school of pharmacy (n = 109) and a school of medicine (n = 110) at 2 southern universities. Students voluntarily completed the Medical Student Attitudes Toward the Underserved (MSATU) questionnaire at the beginning of the year in 1997 (Year 1) and 1998 (Year 2), and immediately prior to graduation in 2001 (Year 4). Unique identifiers were provided by students in both groups to ensure confidentiality and to enable investigators to match responses across the 3 administrations. Both institutions obtained Institutional Review Board approval to conduct this study. Some of the data pertaining to medical students was previously published in a paper that compared problem-based to traditional curricula.7
The MSATU, which assesses attitudes about medical care and underserved populations, is the only known reliable instrument that addresses the topic.40 Reliability, validity, factor analysis, and internal consistency coefficients for this instrument are reported elsewhere.18, 40 Minimal changes were made to the questionnaire given to the pharmacy students: the word medical was changed to pharmacy and physicians to pharmacists where appropriate. Total baseline scores for pharmacy students were within the range of those for medical students, suggesting that the instrument performed the same among these 2 health professions.
The MSATU instrument contains 2 subscales that use a 5-point Likert scale indicating the extent to which respondents agree or disagree with the statements (5 = strongly agree, 1 = strongly disagree). The subscales assess:
attitudes (23 items) regarding professional role or responsibility, organizational role or responsibility, and personal (student) role or responsibility. This subscale's factors are: societal expectations and professional responsibility.
services (14 items) ranging from basic to extensive care to which individuals should have access regardless of their ability to pay. This subscale's factors are: basic services and expensive procedures.18
The total MSATU score is the combined score of the attitudes and services subscales. In past analyses, locus of control and social desirability measures were embedded in the MSATU.7 These measures have never correlated with responses so they are not addressed in this paper. Sample items from the questionnaire are given in Table 1. Negatively stated items are reverse coded; higher scores indicate more favorable attitudes. Scores are standardized to T-scores to provide a basis for comparing the magnitude of the effects. For this study, T-scores have a mean of 50, and a standard deviation of 10. (A score of 43 is 0.7 of a standard deviation below the mean.)
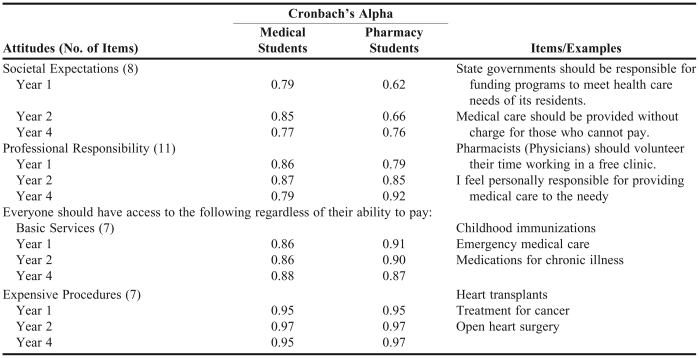
Table 1.
Medical Students' Attitudes Toward the Medically Underserved Scale Items and Longitudinal Internal Consistency Estimates
Data were entered into SPSS, Version 15.0 (SPSS, Chicago, Ill). All scores were calculated using established scoring methods.18 For the attitudes and services subscales, factors were analyzed and reported separately. Baseline descriptive statistics were calculated to look for differences between groups for age, gender, and race. Independent t tests, including and excluding outliers, were used to determine whether there were differences at baseline between groups. Results were not influenced by the inclusion of outliers and subsequent analyses included all data. A repeated measures ANOVA was used to analyze longitudinal data for students who completed the MSATU at all 3 administrations. This procedure controls for baseline differences for these subjects.
Pharmacy and medical students' data could not be compared in Year 3 due to a poor response rate from the medical students at that time point.7 Thus, the final analyses included data from 3 years. Students' data were omitted from the data set if they did not graduate with the class into which they matriculated (“dropouts”). Dropouts included students who were lost to their entering class (eg, repeating a year, dropping out of school, graduation delay).
Students who completed the MSATU at each administration (completers; 55 medical/85 pharmacy) were compared with students who did not (non-completers; 36 medical/13 pharmacy) for baseline demographics and the subscale and factor scores.
RESULTS
Over the 4-year period, there were 11 pharmacy class dropouts and 19 medical class dropouts, which resulted in 98 pharmacy and 91 medical students at baseline. The only significant differences found between completers and non-completers were that more medical student “completers” were female (completers = 62%; non-completers = 39%; χ2 = 4.590, p < 0.05) and had a significantly higher score for professional responsibility (completers = 57.2; non-completers = 52.0; t = −2.481, p < 0.05).
The scores for the MSATU scales and factors were internally consistent across all 3 administrations. Internal consistency coefficients (Cronbach's alpha) ranged from 0.62 to 0.97. Individual coefficients for each factor across the 3 administrations by student group are presented in Table 1.
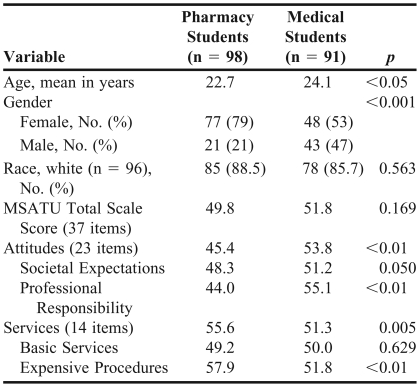
Table 2 shows that pharmacy students were younger (22.7 years, t = 2.306, p < 0.05), which was expected since most enter their professional program before obtaining a bachelor's degree. More pharmacy students were female (79%, χ2 = 14.051, p < 0.01). Both groups were primarily white. Age did not correlate with the MSATU for any of the 3 administrations; thus, age was not used as a covariate in subsequent analyses.
Table 2.
Baseline Demographics and Medical Students' Attitudes Toward the Medically Underserved T-Scores
Research Question 1.
At baseline, there was no difference in the MSATU total score between pharmacy (49.8) and medical (51.8) students (Table 2). Medical students scored significantly higher on the attitudes, societal expectations, and professional responsibility sections of the questionnaire. Pharmacy students scored significantly higher on the items regarding services and expensive procedures. There was no difference between the 2 groups' scores on basic services items.
Research Question 2.
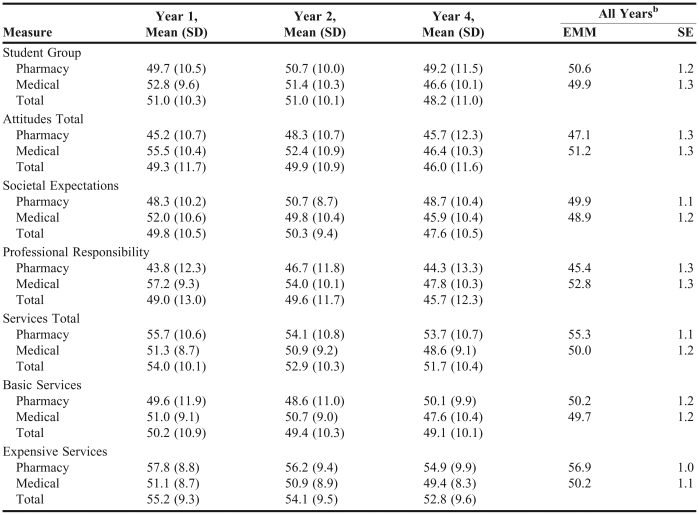
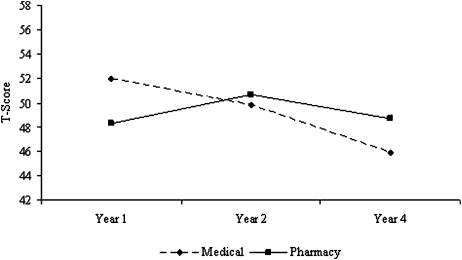
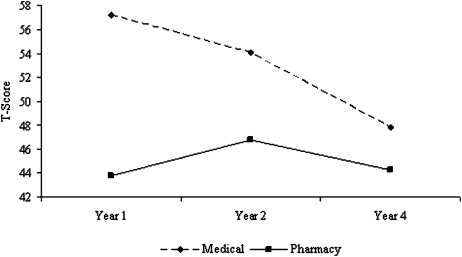
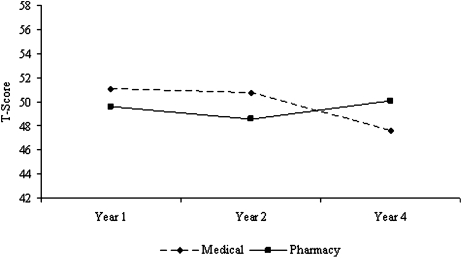
Table 3 shows the outcomes of repeated measures for pharmacy and medical students for Years 1, 2, and 4. There was a significant interaction effect of “year in school” and “student type” for the total scale (p < 0.01), attitudes subscale (p < 0.01) and the societal expectations (p < 0.01) and professional responsibility (p < 0.01) factors. Although pharmacy student attitudes became more favorable from Year 1 to Year 2, they returned to baseline at the end of Year 4 (attitudes scores: Year 1 = 45.2, Year 2 = 48.3, Year 4 = 45.7). In contrast, medical students' scores on the attitudes items declined significantly each year (attitudes scores: Year 1 = 55.5, Year 2 = 52.4, Year 4 = 46.4). For medical students, the differences in means from Year 1 to Year 4 for these 4 dependent variables ranged from 6.0 (societal expectations) to 9.4 (professional responsibility) points (ie, 0.60 to 0.93 standard deviation decline). Figures 1 and 2 illustrate the change in scores over time for the societal expectations and professional responsibility items.
Table 3.
Medical Students' Attitudes Toward the Medically Underserved Subscales and Factors by Student Type and Year of Traininga
Repeated measures analysis of variance with the repeated measures variable of year of training and the between subject variables of student type and gender. No significant effects of gender or any interactions of gender*year of training or gender*student type were found
Emm = estimated marginal mean, se = standard error
Figure 1.
Attitudes by year in school and student type: societal expectations
Figure 2.
Attitudes by year in school and student type: professional responsibility
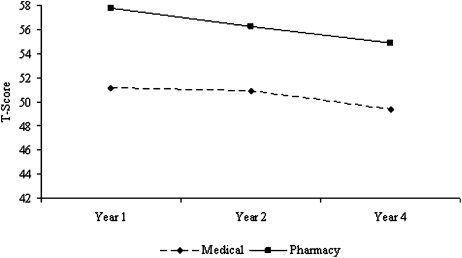
For the services subscale, there were main effects of “student type” and “year in school.” Although pharmacy student attitudes across the 4 years were more favorable (55.3, 50.0, p < 0.01), attitudes for all students combined declined significantly from Year 1 to Year 4 (54.0, 51.7, p < 0.05). There were no differences over time for scores on basic services items. However, there was a main effect of “student type” for expensive procedures (p < 0.01). Although scores on this factor remained fairly stable for both groups, at each point in time, pharmacy students' scores were more favorable. Figures 3 and 4 illustrate the change in scores over time for basic services and expensive procedures items.
Figure 3.
Attitudes by year in school and student type: basic services
Figure 4.
Attitudes by year in school and student type: expensive procedures
In regards to the secondary question of whether women and men within each profession have different attitudes, gender differences were not apparent, as there were no gender main effects or interactions with “year in school” or “student type” for any of the analyses.
DISCUSSION
At baseline, medical students had more favorable attitudes concerning their professional responsibility to provide care. These attitudes may reflect the premise that beginning medical students enter into their professional program highly idealistic and with a critical sense of duty to patients.28,30 Perhaps pharmacy students enter into their professional education thinking that they will not be as directly responsible as other health care professionals for patient care outcomes.41 Research conducted outside the United States is relevant to our findings. For example, researchers in New Zealand showed that entering medical students believed clinical work should be the responsibility of individuals; conversely, entering pharmacy students believed in a more team-based approach.42,43
Interestingly, pharmacy students' overall attitudes and professional responsibility scores increased from Year 1 to Year 2, while these scores decreased in medical students during this time. Both schools incorporate concepts of professionalism in the first year curricula, so it is difficult to explain the change unequivocally. The medical school was revising the professionalism and communications portions of the curriculum at the time of this study, while the first-year pharmacy curriculum emphasized the responsibility of providing pharmaceutical care and the importance of taking care of patients holistically. Many pharmacy students worked in pharmacy settings outside of school and all had an early practice experience in patient care during the last month of their first professional year. Perhaps this early curricular instruction, coupled with helping patients at their work or practice site, contributed to this increased sense of responsibility. However, in another study, only 37% of fourth-year pharmacy students agreed that they would be willing to take the “initiative to get approval to offer the Medicare Medication Therapy Management Program if their employer did not plan to offer MTMS.”41
Entering pharmacy students were more favorable concerning the provision of expensive procedures regardless of an individual's ability to pay for them. However, both pharmacy students' and medical students' scores in this factor decreased as they progressed in their respective professional programs and as they learned more about the complexities of health care economics.
While a factor analysis comparing the factor structure of the MSATU for medical and pharmacy students would certainly illuminate both the similarities and the differences between the 2 student types concerning their attitudes towards the medically underserved, unfortunately there were not enough subjects to perform this analysis. A multisite study involving several health professions schools, which will allow for such comparisons, is in the early stages of recruitment and data collection.
Comparing Year 1 with Years 2 and 4, pharmacy students' attitudes as a whole remained quite stable. Alternatively, medical students' attitudes became significantly less favorable. Differences could be related to several issues. Pharmacy students have most of their patient contact in their fourth year; consequently, they do not see as many underserved patients. Many uninsured or underserved patients are cared for by providers at academic health centers, exposing medical students more consistently to the challenges of caring for vulnerable patient populations during their third and fourth year clinical rotations.18 The more dramatic changes in medical students' attitudes, especially regarding professional responsibility (0.94 standard deviation decline) might be related to their developing feelings of helplessness in caring for the medically underserved.44
Gilligan espoused that women are oriented to an “ethic of care” and men to an “ethic of justice,” suggesting that women would have more favorable attitudes toward caring for the underserved.45 Inconsistent with previous studies, no significant differences between men and women were found.18, 40 However, differences may have been found if we had obtained equal responses for men and women at all 3 administrations for the medical students and if there had been more males in the pharmacy class. While the exact nature of these differences is not known, research in this area suggests that declining attitudes would be more pronounced if a greater number of men had participated. Additionally, other factors such as student stress may contribute to declining attitudes.28 A greater percentage of pharmacy students completed all 3 administrations of the MSATU (87% versus 60%). There were more women in the pharmacy group and evidence suggests that women are more likely to complete questionnaires.46
With the exception of gender effects, the results obtained in this study are consistent with those of previous studies. This is the first known longitudinal study addressing both pharmacy and medical students' attitudes toward the underserved. The results of this study compel us to attend to curriculum in the health professions. Encouraging preliminary evidence suggests that well-designed, longitudinal educational experiences positively influence attitudes toward caring for underserved and vulnerable patients.47,48 In 2006, the American Association of Colleges of Pharmacy formed The Providing Care for the Underserved Curriculum Task Force to develop a curricular framework and educational resources to assist faculty in preparing students and pharmacists to provide pharmacy services to the medically underserved.
A limitation to this study was the difficulty in obtaining Year 3 data from medical students. Once they enter clinical rotations, medical students are rarely together as a group for questionnaire administration. In our experience, students are less willing to complete and return survey instruments via campus mail or online, making data collection a challenge. With the onset of required clinical rotations in Year 3, one could speculate that constant encounters with patients would influence attitudes. However, previous research does not support this claim.18 Further studies to elucidate the influence of clinical experiences on attitudes and behaviors are warranted.
CONCLUSION
As students progressed through school, pharmacy student attitudes toward the medically underserved remained relatively stable while medical student attitudes significantly declined. Exposure to the challenges of caring for underserved patients without the benefit of positive professional role models and well-designed educational experiences may do more harm than good. Educators must enhance and support interprofessional role modeling, longitudinal curricula, and experiential practice sites in order to fulfill this social contract. Research is needed to study the effects of new curricular efforts. Examining student attitudes as a result of these initiatives is an essential aspect of raising awareness about the number of uninsured Americans and increasing access to care for the vulnerable populations in our society.
ACKNOWLEDGEMENT
The authors wish to acknowledge Jonell Hudson, PharmD, BCPS, for the original conception of this research, and Karen Klein, MA, ELS (Research Support Core, WFUHS) for her editorial contributions to this manuscript. Some of the data pertaining to medical students was previously published in an article in Advances in Health Sciences Education.7
REFERENCES
- 1.DeNavas-Walt C, Proctor BD, Smith J. Income, Poverty, and Health Insurance Coverage in the United States: 2006. Washington, DC: US Department of Commerce; 2007. Available at: http://www.census.gov/prod/2006pubs/p60-231.pdf Accessed November 20, 2008.
- 2.Fiscella K, Holt K. Impact of primary care patient visits on racial and ethnic disparities in preventive care in the United States. J Am Board Fam Med. 2007;20:587–97. doi: 10.3122/jabfm.2007.06.070053. [DOI] [PubMed] [Google Scholar]
- 3.Smedley BD, Stith AY, Nelson AR. Washington DC: National Academies Press; 2003. Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment Confronting Racial and Ethnic Disparities in Health Care . [PubMed] [Google Scholar]
- 4.National Healthcare Disparities Report, 2003. Full Report. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.ahrq.gov/qual/nhdr03/fullreport/. Accessed November 20, 2008.
- 5.Iglehart J. Forum on the future of academic medicine: Session VI–Issues of change and quality in U.S. health care. Acad Med. 1999;74:764–72. doi: 10.1097/00001888-199907000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Ring JJ. The right road for medicine. Professionalism and the new American Medical Association. JAMA. 1991;266:1694. [PubMed] [Google Scholar]
- 7.Crandall SJ, Reboussin BA, Michielutte R, Anthony JE, Naughton MJ. Medical students' attitudes toward underserved patients: a longitudinal comparison of problem-based and traditional medical curricula. Adv Health Sci Educ Theory Pract. 2007;12:71–86. doi: 10.1007/s10459-005-2297-1. [DOI] [PubMed] [Google Scholar]
- 8.Ajzen I. The Theory of Planned Behavior. Organ Behav Hum Decis Proc. 1991;50:179–211. [Google Scholar]
- 9.Shepherd MD, Erwin G. An examination of students' attitudes toward the elderly. Am J Pharm Educ. 1983;47:35–8. [PubMed] [Google Scholar]
- 10.Crismon ML, Jermain DM, Torian SJ. Attitudes of pharmacy students toward mental illness. Am J Hosp Pharm. 1990;47:1369–73. [PubMed] [Google Scholar]
- 11.Sheridan J, Bates IP, Webb DG, Barber ND. Educational intervention in pharmacy students' attitudes to HIV/AIDS and drug misuse. Med Educ. 1994;28:492–500. doi: 10.1111/j.1365-2923.1994.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 12.Chisholm MA, Wade WE. Factors influencing students' attitudes toward pharmaceutical care. Am J Health-Syst Pharm. 1999;56:2330–5. doi: 10.1093/ajhp/56.22.2330. [DOI] [PubMed] [Google Scholar]
- 13.Manasse HJ. The Stages and Process of Socialization in the Profession of Pharmacy. Minneapolis: University of Minnesota; 1974. [Google Scholar]
- 14.Schwirian PM, Facchinetti NJ. Professional socialization and disillusionment: the case of pharmacy. Am J Pharm Educ. 1975;39:18–23. [PubMed] [Google Scholar]
- 15.Knapp DE, Knapp DA. Disillusionment in pharmacy students. Soc Sci Med. 1968;1:445–7. [Google Scholar]
- 16.Hatoum H, Smith MC, Sharpe TR. Attitudes of pharmacy students towards psychosocial factors in health care. Soc Sci Med. 1982;16:1239–41. doi: 10.1016/0277-9536(82)90149-6. [DOI] [PubMed] [Google Scholar]
- 17.Satterwhite RC, Satterwhite WM. 3rd, Enarson C. An ethical paradox: the effect of unethical conduct on medical students' values. J Med Ethics. 2000;26:462–5. doi: 10.1136/jme.26.6.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crandall SJ, Volk RJ, Cacy DS. A longitudinal investigation of medical student attitudes toward the medically indigent. Teach Learn Med. 1997;9:254–60. doi: 10.1207/s15328015tlm0904_2. [DOI] [PubMed] [Google Scholar]
- 19.Christie R, Merton RK. Procedures for the sociological study of the value climate of medical schools. J Med Educ. 1958;33:125–53. [PubMed] [Google Scholar]
- 20.Coombs RH. Mastering Medicine. New York: The Free Press; 1978. [Google Scholar]
- 21.Leserman J. Changes in the professional orientation of medical students: A follow-up study. J Med Educ. 1980;55:415–22. doi: 10.1097/00001888-198005000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Parker S. The attitudes of medical students toward their patients: an exploratory study. J Med Educ. 1960;35:849–56. [Google Scholar]
- 23.Patenaude J, Niyonsenga T, Fafard D. Changes in students' moral development during medical school: a cohort study. Can Med Assoc J. 2003;168:840–4. [PMC free article] [PubMed] [Google Scholar]
- 24.Tarbox AR, Connors GJ, Faillace LA. Freshman and senior medical students' attitudes toward the elderly. J Med Educ. 1987;62:582–91. doi: 10.1097/00001888-198707000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Ten Haken JD, Woolliscroft JO, Smith JB, Wolf FM, Calhoun JG. A longitudinal investigation of changes in medical students' attitudes toward the elderly. Teach Learn Med. 1995;7:18–22. [Google Scholar]
- 26.Weyant RJ, Simon MS, Bennett ME. Changes in students' attitudes toward HIV-infected patients as the students progress through medical school. Acad Med. 1993;68:377–9. doi: 10.1097/00001888-199305000-00023. [DOI] [PubMed] [Google Scholar]
- 27.Yedidia MJ, Berry CA, Barr JK. Changes in physicians' attitudes toward AIDS during residency training: a longitudinal study of medical school graduates. J Health Soc Behav. 1996;37:179–91. [PubMed] [Google Scholar]
- 28.Guthrie EA, Black D, Shaw CM, Hamilton J, Creed FH, Tomenson B. Embarking upon a medical career: psychological morbidity in first year medical students. Med Educ. 1995;29:337–41. doi: 10.1111/j.1365-2923.1995.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 29.Eron LD. Effect of medical education on medical students' attitudes. J Med Educ. 1955;30:559–66. [PubMed] [Google Scholar]
- 30.Wolf TM, Balson PM, Faucett JM, Randall HM. A retrospective study of attitude change during medical education. Med Educ. 1989;23:19–23. doi: 10.1111/j.1365-2923.1989.tb00807.x. [DOI] [PubMed] [Google Scholar]
- 31.Griffith CH, 3rd, Wilson JF. The loss of student idealism in the 3rd-year clinical clerkships. Eval Health Prof. 2001;24:61–71. doi: 10.1177/01632780122034795. [DOI] [PubMed] [Google Scholar]
- 32.Miller LB, Erwin EF. Attitude changes in medical students during a comprehensive care program. J Med Educ. 1961;36:422–8. [PubMed] [Google Scholar]
- 33.Singleton AF, Chen S. The Medical Student Expectation Scale (MSES): a device for measuring students' expectations of each others' values and behaviours. Med Educ. 1996;30:187–94. doi: 10.1111/j.1365-2923.1996.tb00741.x. [DOI] [PubMed] [Google Scholar]
- 34.Maheux B, Beland F. Changes in students' sociopolitical attitudes during medical school: socialization or maturation effect? Soc Sci Med. 1987;24:619–24. doi: 10.1016/0277-9536(87)90067-0. [DOI] [PubMed] [Google Scholar]
- 35.Maheux B, Beland F, Pineault R. The influence of medical school programs on physicians' attitudes toward universal access to medical care. Med Care. 1987;25:202–9. doi: 10.1097/00005650-198703000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Yiangou C, Wood M, Wright P, et al. Inner city deprivation and medical education: a survey of medical students by medical students. Med Educ. 1988;22:2–7. doi: 10.1111/j.1365-2923.1988.tb00400.x. [DOI] [PubMed] [Google Scholar]
- 37.Ewan C. Social issues in medicine: a follow-up comparison of senior-year medical students' attitudes with contemporaries in non-medical faculties. Med Educ. 1988;22:375–80. doi: 10.1111/j.1365-2923.1988.tb00770.x. [DOI] [PubMed] [Google Scholar]
- 38.Ewan CE. Attitudes to social issues in medicine: a comparison of first-year medical students with first-year students in non-medical faculties. Med Educ. 1987;21:25–31. doi: 10.1111/j.1365-2923.1987.tb00510.x. [DOI] [PubMed] [Google Scholar]
- 39.Sankar U, Jinabhai CC, Munro GD. Health personnel needs and attitudes to rural service in KwaZulu-Natal. S Afr Med J. 1997;87:293–8. [PubMed] [Google Scholar]
- 40.Crandall SJ, Volk RJ, Loemker V. Medical students' attitudes toward providing care for the underserved. Are we training socially responsible physicians? JAMA. 1993;269:2519–23. [PubMed] [Google Scholar]
- 41.Urmie JM, Farris KB, Herbert KE. Pharmacy students' knowledge of the Medicare drug benefit and intention to provide Medicare medication therapy management services. Am J Pharm Educ. 2007;71 doi: 10.5688/aj710341. Article 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Horsburgh M, Lamdin R, Williamson E. Multiprofessional learning: the attitudes of medical, nursing and pharmacy students to shared learning. Med Educ. Sep 2001;35:876–83. doi: 10.1046/j.1365-2923.2001.00959.x. [DOI] [PubMed] [Google Scholar]
- 43.Horsburgh M, Perkins R, Coyle B, Degeling P. The professional subcultures of students entering medicine, nursing and pharmacy programmes. J Interprof Care. 2006;20:425–31. doi: 10.1080/13561820600805233. [DOI] [PubMed] [Google Scholar]
- 44.McMahon AW, Shore MF. Some psychological reactions to working with the poor. Arch Gen Psychiatry. May 1968;18:562–8. doi: 10.1001/archpsyc.1968.01740050050009. [DOI] [PubMed] [Google Scholar]
- 45.Gilligan C. In a Different Voice. Psychological Theory and Women's Development. Cambridge, MA: Harvard University Press; 1982. [Google Scholar]
- 46.Porter S, Whitcomb M. Non-response in student surveys: the role of demographics, engagement and personality. Res Higher Educ. 2005;46:127–52. [Google Scholar]
- 47.Kalishman S, Mines J, Skipper B, Serna L, Skipper E. A study of the relationship of a medical school curriculum to the attitudes of students toward service in medicine. New Orleans, LA: Paper presented at: American Educational Research Association; April, 2002. [Google Scholar]
- 48.Godkin MA, Savageau JA, Fletcher KE. Effect of a global longitudinal pathway on medical students' attitudes toward the medically indigent. Teach Learn Med. 2006;18:226–32. doi: 10.1207/s15328015tlm1803_7. [DOI] [PubMed] [Google Scholar]