Abstract
In Canada, the education of pharmacists is built upon a foundation of strong, research-intensive publicly funded universities and a universal health-care system that balances government and private financing for prescription medications. The evolution of pharmacy education and practice in Canada has laid the foundation for a variety of emerging trends related to expanded roles for pharmacists, increasing interprofessional collaboration for patient-centered care, and emergence of pharmacy technicians as a soon-to-be regulated professional group in parts of the country. Current challenges include the need to better integrate internationally educated pharmacists within the domestic workforce and tools to ensure continuous professional development and maintenance of competency of practitioners. Academic pharmacy is currently debating how best to manage the need to enhance the pharmacy curriculum to meet current and future skills needs, and whether a doctor of pharmacy (PharmD) degree ought to become the standard entry-to-practice qualification for pharmacists in Canada.
Keywords: Canada, comparative education, international pharmacy education
BACKGROUND
Since the 1980s, successive studies and reports have noted that pharmacists are an “underutilized profession” and that pharmacists represent an “untapped resource” of health care.1,2 In an environment of greater awareness of patient safety, greater emphasis on rational use of limited health resources, and greater need for accountability for outcomes, pharmacy practice in Canada continues to move from a product focus to a patient focus.3
The Canadian system for pharmacy education has undergone significant evolution over the past decade, and will continue to evolve to meet and anticipate changing roles for pharmacists within the health care system.4 The Canadian system for health professional education is characterized by 4 key elements: (1) a strong, research-intensive public university system with no private stand-alone schools of pharmacy; (2) a government-funded universal health care system with no private (for-profit) hospitals and relatively circumscribed private health care delivery; (3) a regulatory system for health care professionals built upon the “college” system, similar to the United Kingdom; and (4) independent but highly collaborative educational, regulatory, and advocacy groups. To understand why the Canadian system of pharmacy education exists as it does today, it is essential to recognize the importance of these 4 key elements in shaping educational practices and policies.
These elements have fundamentally shaped the nature of pharmacy education in Canada for over 40 years and have contributed to several significant emerging trends including: (1) an unusually high reliance on international pharmacy graduates (foreign-trained pharmacists) to complement the domestically educated workforce5; (2) government-mandated and supported adoption of interprofessional practices (including pending changes in liability allocation)6; and (3) regulatory changes linked to scope of practice for pharmacists as well as other health care professionals.7
Educational System
In Canada, there are constitutionally defined separation of powers between the federal (national) and provincial governments. Provinces are responsible for administering health care and post-secondary education, while the federal government is responsible for establishing standards for health care and, in many cases, providing financial support. As a result, a patchwork of different regulations and educational and licensure requirements exist; in some cases it might be easier and quicker for a pharmacist educated in British Columbia to become licensed in Washington State than for that pharmacist to become licensed in the province of Quebec.
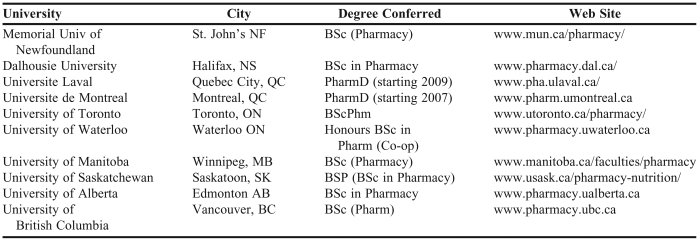
Currently in Canada (with a population of approximately 35 million), there are 10 accredited schools of pharmacy, 8 offer degree programs in English and 2 schools in Quebec offer programs in French (Table 1). All pharmacy schools are located within comprehensive, research-intensive universities located in urban centers, and all are directly affiliated with medical and other health care professional programs within the university structure.
Table 1.
Schools of Pharmacy in Canada
Association of Faculties of Pharmacy of Canada website: www.afpc.info
All pharmacy programs in Canada are accredited by the Canadian Council for Accreditation of Pharmacy Programs (CCAPP), an arms-length body responsible for developing and evaluating educational standards.8 CCAPP undertakes regular accreditation reviews of all schools of pharmacy to ensure compliance with standards. Standards are developed collaboratively with academics, practitioners, regulators, employers, and other stakeholders, and are reviewed and updated on a regular basis to account for changes in practice and education. Full accreditation with CCAPP means an institution is not required to undertake another full review for a maximum time of 6 years.
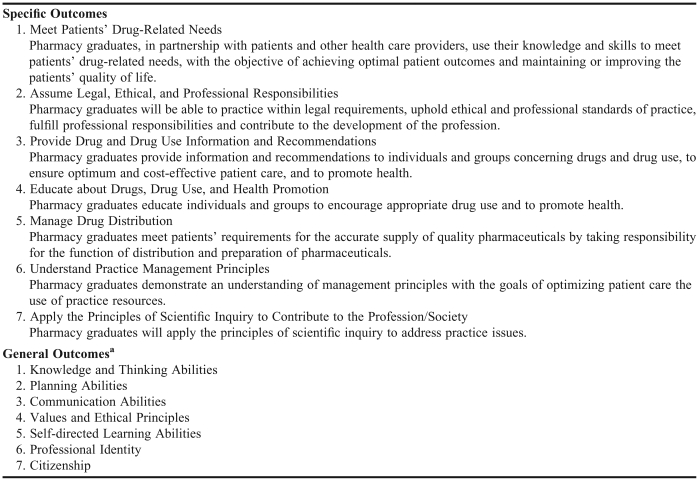
CCAPP utilizes its accreditation standards document as the basis for approving universities to offer the entry-to-practice degree in pharmacy.9 These standards in turn are built upon outcomes for educational programs articulated by the Association of Faculties of Pharmacy of Canada (AFPC, representing the schools of pharmacy across the country and similar in mandate to the American Association of Colleges of Pharmacy). This document (summarized in Table 2) outlines both the pharmacy-specific and general (ie, for university graduates) outcomes of a pharmacy education.10 While each school of pharmacy is free to develop its own curriculum, teaching philosophy, and pedagogical methods, all programs are required to demonstrate that their graduates meet all outcomes at specified levels and ranges of competency. The accreditation review process is an intensive one requiring production of copious documentation and outcomes data to support attainment of goals and objectives.
Table 2.
Statement of Educational Outcomes for a Baccalaureate Pharmacy Graduate in Canada (from the Association of Faculties of Pharmacy of Canada)
General outcomes required of a university graduate and educated citizen and necessary for fulfillment of the professional outcomes required of pharmacy graduates
With only 10 publicly funded university-based pharmacy programs across the country and no real ability for private schools to open and be accredited in Canada, competition for entry into pharmacy programs is intense. For example, at the University of Toronto (Canada's largest pharmacy school), more than 2,000 individuals applied in 2007 for only 240 places. Thus, many individuals who may meet minimum published admission requirements do not gain admission to a pharmacy program. Each year, approximately 1,400 first-year seats are available in pharmacy programs across Canada.
Each school of pharmacy prescribes its unique prerequisites for entry to the program. These requirements represent a minimum threshold and in no way guarantee admission. All programs require a minimum of 5 years of postsecondary education prior to attainment of the bachelor of science in pharmacy, BSc(Pharm) or BScPhm, degree, which is currently the entry-level degree for the profession. Most schools utilize a 1+4 model, in which 1 year of general science courses (chemistry, calculus, biology, etc) is required prior to admission to the program, although some schools utilize a 2 + 4 model (in which more basic science prerequisites are required).
The content of the “+4” (ie, the professional years) varies considerably across the country. Each school of pharmacy has a distinctive character and pedagogical philosophy and utilizes different methods. Some schools tend to utilize a more traditional “building blocks” approach to curriculum, emphasizing foundational subjects such as pharmaceutics, medicinal chemistry, and pharmacology in the early years of the program, followed by more clinical coursework in later years. Other schools, such as Dalhousie University in Halifax, have adopted more problem-based curricular design, opting for small-group tutorial discussions and a more modularized and integrated curriculum.11 Experiential education is a common (and required) feature of all curricula, and occurs in all years of the professional program (to a greater or lesser degree in individual schools). While all schools meet the same outcomes and educational goals and objectives, the way in which they do so varies considerably across the country and is linked to specific local needs and availability of resources.
Until 2007, all pharmacy programs in Canada offered the BScPhm degree as the entry-level degree for the profession. Over the past decade there has been considerable discussion and debate within the profession and the faculties about the need or desirability of changing the entry-level degree to the PharmD. This discussion is complicated by the fact that degree-granting institutions in Canada are all required to report to provincial governments. Across most of Canada (with the exception of Quebec), provincial ministries in charge of higher education have indicated their concern related to “credential creep,” or the ongoing upward drift in degree requirements for entry to professional fields. Provincial ministries (with the exception of Quebec) have informally agreed to enforce uniform policies to discourage academic institutions from such upward drift, and as a result, there is strong pressure in most provinces to retain the BScPhm as the entry-level degree for the profession.
Quebec, owing to its distinctive historical, linguistic, and cultural roots, has not been part of this agreement. In large part due to sweeping changes in provincial legislation that has expanded the role and scope of pharmacists in that province, the 2 pharmacy schools in Quebec have indicated they will move to the entry-level PharmD degree in order to enhance their curricula and appropriately recognize the increased education and skills required in Quebec to practice pharmacy. In 2007, the Universite de Montreal moved to an entry-level PharmD; Universite Laval in Quebec City is expected to enter its first entry-level PharmD class in 2009.
In all provinces, completion of a pharmacy degree (whether it is a BSc, BScPhm, or PharmD) does not automatically qualify an individual for licensure. In most cases, a postgraduation (preregistration) inservice training period (often referred to as “internship” and regulated by the provincial licensing body rather than the local educational institution) is required. The length of this internship varies across the country, but is generally 3-4 months in duration. In addition to this inservice training period, candidates for licensure are required to complete a series of provincial and national examinations.
The Pharmacy Examining Board of Canada (PEBC, similar to the NABP in the United States) is responsible for the national entry-to-practice examination for pharmacists. Since 2001, the Qualifying Examination has consisted of 2 parts. Part I consists of a 2-day case-based multiple-choice test of clinical and therapeutic knowledge. Part II consists of a 16-station objective structured clinical examination (OSCE) administered twice annually in cities across Canada.12 Candidates for licensure are required to complete both parts successfully in order to qualify for licensure within their province.
As in the United States, pharmacists in Canada are not licensed nationally. Instead, each provincial licensing body (generally referred to as a “College of Pharmacists,” not to be confused with an educational institution) registers a pharmacist within one province, after completion of provincial requirements, including a provincial jurisprudence examination. Registration as a pharmacist in one province does not automatically confer the right to practice pharmacy in another province. With the proclamation of a Mutual Recognition Agreement in the late 1990s, labor mobility for pharmacists (and other professionals) in Canada improved significantly, and there are currently fewer barriers for pharmacists wishing to move from one province to another than in the past. However, each case is judged individually, based on criteria such as year of graduation/initial licensure as a pharmacist, educational background, whether an OSCE was completed as part of the licensure process, etc. In some cases, provincial jurisprudence or even English or French language fluency testing may be required. Although labor mobility for pharmacists has improved significantly over the past decade, it is still not a seamless process and regulatory barriers to the free flow of professionals across provincial borders continues to be an issue.
Currently, only 2 Canadian schools, the University of British Columbia (UBC)13 and the University of Toronto (UT),14 offer a 2-year post-baccalaureate PharmD degree; UT also offers a part-time post-baccalaureate PharmD program. Licensure requirements are the same regardless of degree (BScPhm or post-baccalaureate PharmD); only the curricula differ. In the post-baccalaureate PharmD program, the first year (8 months for UBC and 12 months for UT) consists of advanced graduate-level courses and the second year (12 four-week rotations for UBC and 11 months of rotations for UT) consists of experiential clerkships.13,14 Both post-baccalaureate PharmD programs are designed to provide advanced education in clinical pharmacy practice. The UBC program focuses on training individuals to fulfill “advanced clinical pharmacy practice roles in hospitals, ambulatory care or community-based sites, primary care, academia, managed care, government, consulting, industry and in health care agencies.”13 Similarly, the UT program trains individuals to “provide and promote excellence in patient-focused care based on the philosophy of pharmaceutical care.”14 Class size at each school has generally been limited to 6 to 9 students per year and admission is competitive. Applicants must have a BScPhm degree and be a licensed pharmacist in Canada. In general, admission is based on grades, experience, references, and interviews. To date, all successful applicants have had either work or residency experience or both. Like their BScPhm counterparts, both the UBC and UT post-baccalaureate PharmD programs are accredited by CCAPP. The CCAPP accreditation for the post-baccalaureate PharmD degree is also based on a set of standards and guidelines and educational outcomes.15
Pharmacists' Opportunities for Practice in Canada
Pharmacists in Canada practice in a wide array of fields, ranging from dispensary to community to ambulatory to primary/secondary/tertiary care settings.16 There are significant opportunities for pharmacists to find practices that align with their personal interests and objectives.
While there has been significant attention paid to the strong demand for pharmacists across the country over the past decade, we appear now to be moving towards a more balanced supply-demand situation, particularly in urban areas. The geography and population patterns of Canada mean that the majority of citizens reside in urban centers, usually less than 100 miles away from the American border. For structural reasons related to geography, Northern and rural parts of Canada are constantly under-serviced with respect to health care professionals. Given the public nature of the health care system in Canada, governments have traditionally opted for incentive schemes to encourage individuals to move out of urban centers into underserviced locations. Recently, a Northern school of medicine and health professions was developed in Ontario (there are plans to connect it with the pharmacy program at the University of Waterloo), with the goal of attracting and retaining students from the North within their own communities. Despite incentive attempts and creation of new educational facilities, an urban-rural (southern-northern) health service divide continues to exist in Canada.
The vast majority (>75%) of pharmacy graduates from Canadian schools move on to work in community pharmacy settings.16 Due to supply-demand imbalances in the pharmacy workforce, recent graduates electing to work in community pharmacy were provided with very lucrative signing bonuses and other incentives, particularly if they would be willing to relocate to rural or Northern locations. Starting salaries approaching $100,000/year (plus comprehensive benefits including pensions) were not unusual in these situations. However, as the supply-demand situation re-equilibrates, such offers are becoming less common.
Within community practice, pharmacists usually work in staff, manager, or owner positions. The community practice of pharmacists involves a high reliance on technology (computerized databases, drug-interaction checking, generation of drug information, as well as online adjudication of insurance claims, etc). Community pharmacy also relies heavily upon pharmacy technicians and assistants to liberate pharmacists from technical activities so that they may concentrate on cognitive activities related to patient care. Across Canada, there are moves to more formally regulate pharmacy technicians as quasi-independent health professionals.17 The province of Ontario, for example, has recently passed legislation authorizing regulation of pharmacy technicians including uniform postsecondary education requirements, entry-to-practice/licensing examinations, and maintenance of competency. Regulated technicians will then be able to formally assume greater responsibility for drug distribution in community pharmacies, including the ability to dispense medications authorized by a pharmacist without the need for a pharmacist to double-check the product (in this scenario, another registered technician may perform the double-check function).18
The independent pharmacy sector is contracting rapidly in Canada, as the market share and clout of large chain pharmacies (including grocery stores and other outlets) continue to grow.19 This has raised some concerns within the profession as to who controls the future of pharmacy: pharmacists or corporate decision makers with little or no allegiance to the profession? While this trend has caused concern in some quarters, most recent graduates appear relatively content to become staff pharmacists or managers, and concentrate on their patient care activities rather than assume additional worries related to operating a business.
Within the hospital sector, pharmacists assume a variety of roles and responsibilities commensurate with their experience and education. Within the hospital setting, PharmD graduates often assume clinical specialist roles, particularly in teaching and research-intensive hospitals. Many hospitals offer the 1-year post-baccalaureate pharmacy residency program to provide BScPhm graduates with additional clinical experience and the opportunity to undertake independent research in preparation for more responsible positions. Hospital residency programs in Canada are accredited by the Hospital Pharmacy Residency Accreditation Board.20
In many hospitals, pharmacy departments have adopted “tech check tech” programs in which the majority of technical functions related to drug distribution are managed by pharmacy technicians. This allows pharmacists greater time to assume enhanced clinical responsibilities for monitoring patients' drug therapy and working with physicians and other health professionals as part of multidisciplinary teams.21 With changes to the health care system in Canada resulting in shorter hospital admissions and greater emphasis on ambulatory care, pharmacists in hospital settings are increasingly involved with patients who may be residing in their homes but who access the hospital for a variety of services (including “day hospitals,” clinics, etc).
A rapidly growing area of practice for pharmacists in Canada is in the area of primary care, particularly in the context of family health teams.22 Many provinces have introduced programs to encourage community-based family physicians to work collaboratively and in many cases co-locate their practices with other health professionals, including pharmacists. Within family health teams, many pharmacists assume virtually no drug distribution responsibilities and instead will spend their time educating and monitoring patients, advising and educating prescribers, and instituting clinical audits of the practice to ensure patients of the team are being managed appropriately with respect to medication treatments.23 In this regard, the University of Saskatchewan is involved in a variety of interprofessional education, research, and practice initiatives, as is Memorial University of Newfoundland.
Beyond patient care in community, hospital, and primary settings, some pharmacists elect to work in areas such as the pharmaceutical industry, research, government, and academia. Canada's pharmaceutical industry is balanced between so-called research-intensive and generic companies (although the distinction between the 2 is increasingly blurred). Pharmacists in the industry work in a variety of fields, notably sales and marketing, medical information, and quality assurance/product formulation. Given the prominent role of the government (both federal and provincial) in the Canadian health care system, it is not surprising that pharmacists also work within provincial or federal ministries of health, in areas related to pharmaceutical policy (eg, formulary decision making, policy, etc). As in other countries, academic pharmacy continues to struggle in attempting to recruit pharmacists into university-based teaching and research positions. Within the Canadian university system, tenure for clinical faculty members is not commonplace,24 and consequently such faculty members generally do not enjoy the same level of reward or recognition as their tenured colleagues. While many pharmacists enjoy teaching students, and participate as teaching assistants and laboratory demonstrators, most do so only on a part-time, ad-hoc basis. In order to compete successfully for a tenure-track position in most Canadian universities, postgraduate education and a track record of successful independent research (including receipt of competitive grants and research contracts) is usually required.
Currently, employment opportunities for PharmD-trained individuals surpass the number of graduates from Canada's 2 post-baccalaureate PharmD programs, thereby providing graduates with an opportunity to be selective and carve their own practice niche. Typically, PharmD students secure positions well prior to graduation. While most graduates practice as specialists in a hospital setting and have some type of faculty affiliation, a significant number have advanced clinical pharmacy practice roles in consulting, community-based sites, primary care, managed care, government, industry, other health care agencies, and academia. The UBC Web site features an Alumni Profiles page (http://www.pharmacy.ubc.ca/pharmdprogram/alumni.htm) that describes each graduate's practice site.
Current State of Practice in Canada
As discussed previously, pharmacy practice in Canada is currently in a significant state of flux. Because most health care delivery in the country is governed by provinces (but required to meet minimal federal standards), some differences are starting to emerge across the country in the scope of practice of pharmacists. This coupled with differences in the health care infrastructure (particularly the use of electronic health records and access to centralized databases) means that despite minimal federal requirements, the practice of pharmacy may vary considerably from province to province. While all pharmacists nationwide have adopted pharmaceutical care as the guiding principle for the profession, and assume responsibility for the detection, prevention, and resolution of actual or potential drug-related problems, the specific tools available for pharmacists to accomplish this task vary from province to province.
A major area of contention within all health professions in Canada at the current time relates to rigidly defined scopes of practice. For pharmacists, this has been most applicable in the context of decisions related to prescribing medicines. The drug scheduling system in Canada has been (more or less) harmonized nationwide and is divided into a variety of schedules. Drugs that are most potent and pose the greatest risk for harm (including narcotics, benzodiazepines, and most antibiotics) are assigned to a drug schedule that generally requires prescription from an authorized health care professional, while other medications that are appropriate for self-care may be sold only in pharmacies after consultation with a pharmacist (and not in any other kind of retail setting). In jurisdictions where pharmacists are now allowed to prescribe (such as Alberta), provincial regulations have been modified to allow for this expansion in role and scope of practice. In other jurisdictions (such as Ontario), alternative mechanisms (such as collaborative prescribing protocols) have been developed that maintain existing legal prescribing privileges within certain professional groups, but which allow (through protocols) pharmacists to engage in prescribing activities under specified circumstances.
Health care professionals and the public have long complained that this rigid delineation of scope of practice has unnecessarily hampered effective and efficient health care delivery.25 For example, a pharmacist who knows a patient well is not authorized to dispense a chronic medication to a patient who has run out of “refills” on the prescription. Technically, to dispense without this authorization is seen as prescribing, and this goes beyond the traditional scope of practice for pharmacists. Recognizing the inefficiency and ineffectiveness of arcane legislation such as this, most provinces have long appreciated the pharmacist's professional judgment to extend a supply of a chronic medication to a patient in such a situation. However, many provinces are increasingly recognizing that this informal system needs to be formalized and extended further in order to acknowledge the contributions pharmacists can make to health care of patients.
For example, in the province of Ontario, recent changes have allowed for development of medical directives, a dependent prescribing model in which another health care professional delegates (in writing) responsibility for prescribing, dose modification, therapeutic drug monitoring, etc, to a pharmacist who can then proceed with this work in an unsupervised quasi-autonomous manner.26 The medical directive system, for example, would allow a pharmacist in a family health team to independently monitor and modify doses of medications such as lithium or phenytoin, based on laboratory tests ordered by the pharmacist in the community. Medical directives may also extend to prescribing of prescription-only drugs to patients in certain circumstances, or establishing starting doses of antihypertensive medications with the pharmacist responsible for ongoing monitoring and dose adjustment. Under the medical directive system, pharmacists are not “automatically” authorized to undertake these activities (all of which are technically considered as prescribing), but can do so under “one-off” arrangements with prescribers (usually physicians).
In the provinces of Quebec and British Columbia, pharmacists have significant prescribing discretion in order to enforce provincial formulary decisions and optimize drug therapy of patients.27 In these provinces, pharmacists are able to make therapeutic substitutions of prescribed medications without seeking physician authorization, provided these are outlined within the provincial formularies. Formulary choices are well established and evidence based and aim to ensure rational cost-effective pharmacotherapy. In addition, the province of Quebec has extended the role of the pharmacist to include the “pharmaceutical opinion,” a process by which a pharmacist is paid to render and document his/her professional opinion on the quality of pharmacotherapy of a patient, regardless of whether a medication is actually dispensed.28 Similar to this system, the province of Ontario recently instituted the provincially funded MedCheck system, in which any patient in Ontario receiving 3 or more medications can make an annual 30-minute appointment with a pharmacist, have a comprehensive review of medications (prescription and non-prescription) and general health status, and receive personalized education aimed at improving adherence and understanding.29 Pharmacists who provide MedCheck bill the provincial government directly for this service.
Arguably, the province of Alberta has moved the furthest in the area of extending the scope of pharmacists’ activities. In April 2007, pharmacists in Alberta were given new rights to independently prescribe medications, despite significant opposition from local medical associations.27,30 How this new right has been implemented by pharmacists is currently under study. In most cases, pharmacists appear to be exercising their right to prescribe in a relatively cautious, judicious, and appropriate manner, mindful of their own limitations. In most cases, pharmacists are prescribing by making independent dose modification decisions, starting prescription medications in relatively unambiguous situations where diagnosis and course of action are relatively straightforward, and extending chronic medications while monitoring for side effects and efficacy. For example, within the province of Manitoba, it is possible for pharmacists to be identified as clinical associates of physicians and consequently be granted a variety of extended rights and responsibilities with respect to management of patients' medications. Faculty members from the University of Manitoba are in the forefront of such initiatives. New educational programs are being developed to assist pharmacists in further leveraging new tools at their disposal, in order to optimize patients' health care.
Current Challenges and Future Directions in Pharmacy Education
There are several significant issues currently facing academic pharmacy in Canada, including: (1) enhancement of existing bachelor's degree programs; (2) integration of internationally educated pharmacists into the Canadian health care system; (3) developing continuing professional development programs to ensure the current pharmacy workforce is “fit for purpose”; and (4) finding and training the next generation of academic pharmacists.
Enhancement of Existing Bachelor's Degree Programs
As discussed previously, Canada is currently grappling with the need to expand, enhance, and improve existing education programs for pharmacy students in light of expanding roles and responsibilities for pharmacists. For some academics, the current BScPhm model that exists throughout English Canada is insufficient to prepare pharmacy students for a lifetime of professional practice; for others, enhancements to the existing BScPhm programs should be sufficient to ensure relevancy of the curriculum.
There is no consensus within the profession or academic pharmacy in English Canada as to the need or desirability to proceed with an entry-level PharmD program despite the fact that the province of Quebec has declared it will opt for this model. This lack of consensus, coupled with real doubts as to whether provincial ministries of higher education would even approve such a move has resulted in confusion within academic and practice circles. Several universities have publicly begun planning for entry-level PharmD programs with the expectation that once a cogent proposal is formulated and agreed upon by the profession, government approval will follow. Other schools are concerned about resource implications and the issue of what to do with those BScPhm graduates who would like to upgrade; thus, they are publicly opposed to this change. Some have even mused about a potential hybrid route – a move to an MPharm similar to the United Kingdom, which may be somewhat more palatable.
Within the next few years, 2 or 3 schools in English Canada will likely develop proposals for entry-level PharmD programs and attempt to have them approved by their respective provincial governments. It is not clear how these governments will respond. Equally unclear is how it will be possible for some provinces to be entry-level PharmD and other provinces to be entry-level BScPhm and still maintain the mutual recognition necessary to foster labor mobility.
What is clear and agreed upon in all circles is the need to update and refresh the current curriculum and outcomes for the pharmacy degree (whether it is a BScPhm or a PharmD). Increasing the extent and quality of experiential education and introducing more varied pedagogical techniques, including new coursework in emerging areas such as pharmacogenomics, are pushing the current program to its limits. Nonetheless, in order to ensure that the current high quality standards of undergraduate pharmacy education are maintained, these changes are necessary.
Integration of Internationally Educated Pharmacists in the Workforce
The public nature of higher education in Canada means that university programs require government approval prior to opening. As a result, in the last 30 years, only 1 new school of pharmacy has opened in Canada. Given the ongoing strong demand for pharmacists, employers have sought to address human resources issues through immigration.
Like other countries, Canada is a country built upon immigration, and most Canadians are open to the notion that skills shortages in professions can be filled by qualified immigrants. The unique nature of the Canadian education and health care system has meant that Canadian pharmacy is unusually dependent upon international pharmacy graduates to complement the domestically educated workforce. For example, in the province of Ontario, close to 40% of all pharmacists licensed annually come from outside Canada or the United States, a proportion not seen in other health professions in other jurisdictions across North America.31 Across Canada, graduates of American schools of pharmacy are not considered “international pharmacy graduates” due to the significant similarities in the culture and context of practice and education. Pharmacy graduates from accredited American programs are generally required to complete the same pre-licensure activities (examinations, inservice training period, etc) as Canadian graduates.
While the importance of immigration is well accepted conceptually, practical concerns have been expressed regarding the ways international pharmacy graduates (IPGs) integrate into the Canadian workforce. One published study demonstrated that, despite accounting for only 25% of all licensed pharmacists in Ontario, IPGs accounted for close to 68% of all complaints and disciplinary processes.5 Anecdotal evidence suggests additional tools are required to facilitate knowledge and skills acquisition of foreign-trained pharmacists to ensure they are prepared for the realities of Canadian practice.
Canada has been a leader in the development of government-funded bridging programs to assist new immigrants in meeting professional standards of practice. These programs typically consist of 4-6 month university-based education focusing on pharmacy practice and therapeutics, complemented by a 6-12 month inservice training component.31 Since most new immigrants to Canada come from countries where English (or French) is not the first language, additional pharmacy-specific English-as-a-second-language courses have been developed to assist individuals in meeting fluency and cultural competency requirements prior to beginning to bridge education. Currently, bridging programs for international pharmacy graduates are available in British Columbia, Alberta, Ontario, and Quebec—the 4 provinces which most frequently receive immigrants.
The strategy of connecting immigrants to their profession via postsecondary education institutions before they become licensed appears to be of value in optimizing integration of pharmacists in the Canadian workforce. Going forward, challenges remain in developing vehicles and incentives to encourage these individuals to move out of urban areas and into Northern or rural areas where need for their skills is greater.
Developing a “Fit-for-Purpose” Workforce
The significant changes that have occurred in pharmacy practice over the past 20 years in Canada have raised awareness of the need to develop more formalized mechanisms for continuing professional development (CPD). Currently, there is no consistency across the country with respect to mandatory continuing education (CE). Some provinces (such as Ontario) have adopted a CPD rather than mandatory CE model, while other provinces continue to require completion of specified hours of approved CE as a precondition for renewal of annual registration as a pharmacist. Pharmacists – like all other professionals – need to maintain their competency over a lifetime of practice; thus, the undergraduate degree (BScPhm or PharmD) is often perceived as just the beginning of this process. Traditionally, universities have not been as formally involved in the continuing professional development of practitioners, but this is changing rapidly.
The University of British Columbia has been a pioneer in Canada in this area, and has a long-standing tradition of developing programs for pharmacists across the province and country to assist them in maintaining competency. The University of Alberta has developed specific expertise in the area of distance education for pharmacists, and has utilized this platform effectively to assist Alberta pharmacists in adapting to their new reality of prescribing authority. The University of Toronto has worked closely with the Ontario College of Pharmacists (the licensing/regulatory body) to ensure practitioners have access to the education and training necessary to demonstrate their competency as part of Ontario's system of peer review/quality assurance. As part of this system, Ontario pharmacists are randomly selected to demonstrate their competency and success of their individual continuing professional development activities through completion of a case-based multiple-choice written test of clinical knowledge and an objective structured clinical examination. If randomly selected by the College to participate in peer review/quality assurance, practicing pharmacists are required to complete these tests as a condition for annual renewal of registration.32
Across Canada, there is growing recognition that universities have an important – and currently underdeveloped – role to play in ensuring the maintenance of competency of practitioners. Moving beyond simple continuing education, and instead embracing the continuing professional development (CPD) paradigm, university-based CPD programs for pharmacists are emerging as an important part of the educational life cycle for pharmacists at different ages and stages of their careers.
Finding and Training the Next Generation of Pharmacy Academics
Pharmacy academics frequently comment on the demographic time bomb facing schools of pharmacy across Canada. Over the next decade, close to half of existing tenure-track faculty members are expected to retire. Unfortunately, over the past 20 years, little interest has been shown by pharmacy graduates in completing research degrees; consequently, supply of new academics is quite constrained.
While graduate education (ie, MSc and PhD) programs in pharmacy continue to grow and thrive, by and large, these do not attract pharmacy graduates or pharmacists. Instead, pharmacy graduate programs in the social/administrative sciences tend to attract social sciences graduates, and those in the pharmaceutical sciences tend to attract biochemistry, engineering, or life sciences graduates. Consequently, those graduating from MSc or PhD programs from many Canadian pharmacy schools are not necessarily pharmacists. While this may not compromise their ability to perform excellent research, it does make it more difficult to recruit pharmacist-academics who understand the worlds of both practice and research. Conversely, graduates of post-baccalaureate PharmD programs, although trained to be advanced-level clinical practitioners, require further postdoctoral research training in order to succeed in tenure-track academic positions.
While working conditions in most Canadian universities are generally good, and pharmacy academics are generally well respected within the professional community, graduate training programs have not been able to compete with the rewards of professional practice in luring promising pharmacy graduates into research degree programs. A question emerges: will most newly hired tenure-track faculty members in schools of pharmacy in Canada in the future not be pharmacists, and consequently not have any particular allegiance to or investment in the profession? If so, what are the implications for professional socialization if the tenure-track faculty members teaching students, undertaking research, and running schools of pharmacy are not actually pharmacists themselves? The contribution of non-pharmacists within pharmacy schools is significant and should not be diminished or minimized; non-pharmacist faculty members have contributed important perspectives to the education of pharmacy students. However, the challenge for academic pharmacy going forward will be to find ways to encourage pharmacists to pursue graduate/research training and subsequently take on faculty positions to ensure a balance between pharmacists and non-pharmacists in teaching, research, and scholarship.
Future Directions of the Profession of Pharmacy
The profession of pharmacy in Canada is enjoying a renaissance of sorts. After many years of feeling somewhat marginalized by the health care system, pharmacists are now enjoying recognition and rewards commensurate with their education and abilities. The public nature of Canada's health care system means that once governments make decisions, they can be enacted on a large scale. After years of advocating for expansion of pharmacists’ cognitive skills, governments are paying attention.
As is typical within the Canadian system, individual provinces are experimenting with expanding roles for pharmacists using different models, and in different ways, to meet local needs and concerns. On the surface, this gives the appearance of a disorganized patchwork of systems, practices, and policies without a truly national cohesion. However, from an individual patient perspective, there is great sense in approaching major changes in this way. The dramatic changes leading to prescribing rights for pharmacists in Alberta contrast with the cautious incremental approach of medical directives in Ontario, despite the fact that both achieve similar outcomes in providing pharmacist with new tools to optimize patients’ drug therapy. The nature of Canadian society – including its culture and government – supports this approach. Within pharmacy education, different schools of pharmacy are evolving different competencies and strengths, even though all meet the same accreditation standards and practice expectations.
Going forward, the profession of pharmacy is well positioned to continue to be a major player in health care delivery and policy in Canada. As the nation continues to debate core values related to universal medical care, the need to implement a national Pharmacare system to cover all drug costs for all Canadians, and the move to community-based and primary care continues to accelerate, the knowledge and skills of pharmacists will continue to be in high demand. For many years, surveys in Canada have indicated that pharmacists are among the most trusted of all professionals. Building upon this tradition and foundation, roles for pharmacists are expanding rapidly, and success begets success. The more comfortable patients, physicians, and other health care practitioners feel with these expanded scopes of practice for pharmacists, the more role expansion will likely occur.
CONCLUSIONS
This review of pharmacy education and practice has attempted to identify key trends facing the profession and its educators. While it is difficult to talk about a national educational system or a national health care system in Canada due to our seemingly fragmented provincial-federal system, there are many core values shared by all Canadians with respect to health and education. For most, universal access to health care and a tradition of strong publicly funded research-intensive universities are distinctive and important elements of being Canadian. Pharmacists in Canada have contributed significantly to, and benefited significantly from, these twin ideals.
ACKNOWLEDGEMENT
Thanks to Dr. Frank Abbott, Executive Director of the Association of Faculties of Pharmacy of Canada for his assistance in preparing this manuscript.
REFERENCES
- 1.Gibson E, Baylis F, Lewis S. Dances with the pharmaceutical industry. Can Med Assoc J. 2002;166:448–50. [PMC free article] [PubMed] [Google Scholar]
- 2.Commission on the Future of Health Care in Canada – Final Report; 2002. Available at: http://www.hc-sc.gc.ca/hcs-sss/alt_formats/hpb-dgps/pdf/hhr/romanow-eng.pdf. Accessed November 10, 2008.
- 3.Al-Sukhni M, Ballantyne P. Pharmaceutical-related strategies for health care reform in Canada. Can Pharm J. 2007;140:38–45. [Google Scholar]
- 4.Association of Faculties of Pharmacy of Canada. AFPC educational outcomes for a baccalaureate pharmacy graduate in Canada; 1998. Available at: http://afpc.info/downloads/1/Outcomes_Undergrad_1998.pdf. Accessed October 22, 2008.
- 5.Austin Z. Continuous professional development and foreign trained health care professionals. J Soc Admin Pharm. 2003;20:232–40. [Google Scholar]
- 6.Oandasan I, Reeves S. Key elements of interprofessional education: factors, processes and outcomes. J Interprofessional Care. 2005;5(Suppl 1):39–48. doi: 10.1080/13561820500081703. [DOI] [PubMed] [Google Scholar]
- 7.Curran V. Interprofessional education for collaborative patient-centred practice research synthesis paper. Health Canada; 2005. Available at: http://www.hc-sc.gc.ca/hcs-sss/hhr-rhs/strateg/interprof/synth_e.html. Accessed October 22, 2008.
- 8.Canadian Council for Accreditation of Pharmacy Programs. Accreditation of Pharmacy Programs in Canada. Available at: http://www.ccapp-accredit.ca/. Accessed October 22, 2008
- 9.Canadian Council for Accreditation of Pharmacy Programs. Accreditation standards for pharmacy programs in Canada. Available at: http://www.ccapp-accredit.ca/standards/. Accessed October 22, 2008.
- 10.AFPC educational outcomes for a baccalaureate pharmacy graduate in Canada. Association of Faculties of Pharmacy of Canada; 1999. Available at: http://www.afpc.info/downloads/1/Outcomes_Undergrad_1998.pdf. Accessed November 10 2008.
- 11.Whelan AM, Mansour S, Farmer P, Yung D. Moving from a lecture-based to a problem-based learning curriculum – perceptions of preparedness for practice. Pharm Educ. 2007;7:239–47. [Google Scholar]
- 12.Austin Z, O'Byrne C, Pugsley J, Queroz L. Development and validation of an objective structured clinical examination (OSCE) for entry-to-practice certification: the Canadian experience. Am J Pharm Educ. 2003;67(3) Article 76. [Google Scholar]
- 13.University of British Columbia. Doctor of Pharmacy (Pharm D) Program. Available at: http://www.pharmacy.ubc.ca/pharmdprogram/index.htm. Accessed October 22, 2008.
- 14.University of Toronto. Leslie Dan Faculty of Pharmacy Doctor of Pharmacy Program. Available at: http://www.pharmacy.utoronto.ca/pharmd/index.jsp. Accessed October 22, 2008.
- 15.Canadian Council for Accreditation of Pharmacy Programs. Accreditation Standards. http://www.ccapp-accredit.ca/standards/. Accessed November 10th 2008.
- 16.Canadian Pharmacists' Association. Pharmacy human resources in Canada: a study of pharmacists and pharmacy technicians. Available at: http://www.pharmacists.ca/content/about_cpha/whats_happening/cpha_in_action/pdf/PharmacyHRStudySummary.pdf Accessed October 22, 2008.
- 17.Macinnis M, Power B, Cooper J. Environmental scan of pharmacy technicians (2006). Accessed at: http://www.pharmacists.ca/content/hcp/Resource_Centre/Practice_Resources/pdf/pharmacy_technicians.pdf. Accessed November 10 2008.
- 18.Vision Research. The pharmacy technician workforce in Canada: roles, demographics, and attitudes. Report prepared for Moving Forward: Pharmacy Human Resources for the Future. March 2007.
- 19.Waldie P, Strauss M. The demise of the corner drug store. The Globe and Mail. November 9, 2007.
- 20.Canadian Society of Hospital Pharmacists. Residency Training. Available at: http://www.cshp.ca/programs/residencyTraining/info_e.asp. Accessed on October 22, 2008.
- 21.Johnson N, Roy M. Medication safety: leading by example? Can Pharm J. 2006;137(4):13. [Google Scholar]
- 22.Ministry of Health and Long Term Care, Government of Ontario. Family Health Teams. Available at: http://www.health.gov.on.ca/transformation/fht/fht_mn.html. Accessed on October 22, 2008.
- 23.Stratford Family Health Teams. Job description for pharmacist working in Family Health Teams. http://qiip.ca/user_files/Pharmacist_Stratford.doc. Accessed November 10th 2008.
- 24.Austin Z, Gregory P. Promotion and tenure: clinical faculty at schools of pharmacy in Canada. Pharm Educ. 2006;6:1–8. [Google Scholar]
- 25.The Health Professions Regulatory Advisory Council of Ontario. Regulation of health professions in Ontario: New directions. http://www.hprac.org/en/reports/resources/New_Directions_April_2006_EN.pdf. Accessed October 22, 2008.
- 26.Federation of Health Regulatory Bodies Ontario. An interprofessional guide on the use of orders, directives and delegation for Regulated health professions. http://mdguide.regulatedhealthprofessions.on.ca/why/default.asp. Accessed November 10 2008.
- 27.Kondro W. Canada's doctors assail pharmacist prescribing. Can Med Assoc J. 2007;177:42–6. doi: 10.1503/cmaj.071212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Traynor K. Pharmacists outside US inch toward independent prescribing. Am J Health-Syst Pharm. 2004;61(14):1429. doi: 10.1093/ajhp/61.14.1429. [DOI] [PubMed] [Google Scholar]
- 29.Ministry of Health and Long Term Care, Government of Ontario. The MedsCheck Program. Available at: http://www.medscheck.ca/ Accessed October 22, 2008.
- 30.Alberta College of Pharmacists. New Legislation: Pharmacists' Prescribing. Accessed November 5th 2007 at: https://pharmacists.ab.ca/nCollege/resource.aspx?id=5761. Accessed November 10 2008.
- 31.Austin Z, Dean M. Bridging education for foreign-trained professionals: the international pharmacy graduate (IPG) program in Canada. Teach Higher Educ. 2006;11:19–32. [Google Scholar]
- 32.Austin Z, Marini A, Croteau D, Violato C. Assessment of pharmacists' patient-care competencies: validity evidence from Ontario (Canada)'s Quality Assurance and Peer Review Process. Pharm Educ. 2003;4:23–32. [Google Scholar]