This article provides an overview of the current status of pharmacy education in the United Kingdom. A characteristic program is described which is based on the master of pharmacy (MPharm) model, which is an “undergraduate” master's degree. The type and length of training, numbers entering and leaving the profession, and criteria for admission are discussed, and an overview of the curriculum, which is normally based over 4 years, is given. The career opportunities of UK pharmacy graduates are discussed, as well as educational challenges such as plagiarism and the changing profile of schools of pharmacy, which is affecting supply and demand of pharmacists. The changing face of the profession in the UK is then addressed, including the advent of the prescribing pharmacist.
PHARMACY DEGREE
Historically, entrance to the pharmacy profession required successful completion of a 3-year Bachelor of Science (BSc) degree followed by 1 year preregistration work under appropriate supervision. Since the turn of the century, however, the recognized qualification that permits registration with the Royal Pharmaceutical Society of Great Britain (RPSGB) has been the 4-year MPharm program, followed by the compulsory 1-year work program prior to application for registration as a pharmacist. Under the Bologna agreement for educational equivalence across Europe, this is classed as an “undergraduate masters program,” which is a lesser qualification than the traditional MSc degree1; the reason being that possession of a bachelor's degree is not necessary for application to the program. Within mainland Europe, pharmacy degree programs typically are 5 to 6 years. The United Kingdom's 4-year degree is the shortest of the European pharmacy degrees. The MPharm programs fulfill all of the criteria required under European regulations concerning equivalence of qualifications: a European Union citizen achieving an MPharm degree is thus eligible to apply for registration in any of the European member states having completed their work placement experience. However, most member states impose some additional language requirements and the need to work under supervision for the first 3 to 6 months after taking up their new post. A non-European Union citizen qualifying as a pharmacist in one member state is not automatically eligible to apply for registration as a pharmacist in another member state since legislation applying to mutual recognition of qualifications applies to European Union citizens only.2
There is some lack of consistency concerning requirements for “currency of knowledge” prior to graduation. There is a limited timeframe during which MPharm students must complete their program. Most UK schools of pharmacy require students to graduate from the MPharm program within 6 years of commencing, which allows for illness, pregnancy, etc, or even failure and repetition of some stages of the program. The argument proffered for this limit is that the material taught early in the program is outdated if the student graduates more than 3 years after they commence their studies. This limit, however, is not mandatory, and thus not applied in all UK programs. Each case is assessed on merit by the RPSGB when the student applies for training prior to application for entry onto the register of pharmacists. Students, however, are not obliged to undertake their preregistration training immediately following graduation; thus, a student who graduates in 4 years may decide to delay preregistration training. There are cases where graduates have applied for preregistration training more than 10 years after graduation. Using the argument of “currency of knowledge,” it has now been suggested that graduates should be required to begin their preregistration training within 3 years of graduation. This has yet to be legislated. The 12-month preregistration training culminates with a national registration examination. Students are allowed 3 attempts to pass this assessment if needed, with an additional 12-month period of training enforced after the second failure. The “standard” student is therefore expected to enter the Register of Pharmaceutical Chemists following completion of a 4-year university program and 1-year workplace training. Prior to October 2007, the maximum duration to achieve registration was 11 years from commencement of studies (6 years MPharm, 3 years career break, and 2 years preregistration training), although this was perceived as “stretching” the “currency of knowledge” argument to its limits. However, things changed in 2007 when a European directive concerning pharmacy qualifications began permitting part-time study. Whereas prior to October 2007 students were required to study full time for at least 4 years at a university, the requirement changed to “the equivalent of at least 4 years, full-time study.” How the issue of prolonged, part-time study and “currency of knowledge” is to be reconciled has yet to be decided.
The only other route which bestows eligibility for registration with the RPSGB is the Overseas Pharmacist Accreditation Program (OSPAP). Qualified non-European Union pharmacists may apply to the RPSGB for entry to an OSPAP program. Practicing pharmacists from outside the European Union or non-European Union citizens who have qualified within the European Union, who satisfy various criteria, including English language qualifications and the content of the program from which they have graduated, may then be referred to one of 4 universities providing the OSPAP program. This is a 1-year postgraduate program, which following successful completion of the 1-year preregistration training, permits application for entry onto the Register of Pharmaceutical Chemists.
PHARMACY PROGRAMS
There are 22 schools of pharmacy in the United Kingdom offering MPharm degrees, of which 4 also offer the OSPAP. A further 4 universities are currently in negotiation with RPSGB regarding possible accreditation of new MPharm programs. Each school admits an average of 150 students to their MPharm program each year; thus, the United Kingdom provides approximately 3300 undergraduate pharmacy places per year (for a total population of about 60 million); this may rise in the future. In addition there are about 120 places available on OSPAP programs per year. Under the current UK system, students applying for university entrance can apply to a maximum of 5 courses, which may be at the same or different universities. In the case of medical school, students can apply to 4 medical programs only, plus 1 other non-medicine program. The majority of students applying for pharmacy apply exclusively to pharmacy programs, although approximately 20% list pharmacy as their fifth choice after the 4 medicine applications.3 On average, each school of pharmacy receives approximately 8-10 applicants for each place on their MPharm program, but taking into account that each applicant has applied to 4 other schools of pharmacy, this translates to 10,000 applicants for the 3,300 places across the UK per year. OSPAP programs are also over-subscribed with waiting lists for applications, the current undercapacity in number of places resulting in 3 applicants for each place.
ENTRY QUALIFICATIONS
Entry qualifications vary slightly across the 22 UK schools of pharmacy, but the most important deciding factor for most applicants is performance in the national school-leaving examinations (Advanced Levels also known as A-Levels). A-Levels are the final examinations taken by 18-year-old school-leavers. The 3 subjects normally studied at A-Level before applying for the MPharm program are chemistry, math, and biology. Typical entry qualifications would approximate to 3 A grades at A-Level or 1 A grade and 2 B grades; invariably A-level chemistry is mandatory. Other equivalent qualifications are acceptable, but heretofore, 15%-20% of entrants already hold a bachelor's degree (graduate entry). Typically graduates would be expected to have achieved an upper-second class honors degree (ie, >60% average) if they are to be offered a place on the program. The practice regarding the interviewing of applicants also differs. Some schools of pharmacy place great emphasis on performance at interview and use this as an important factor in their selection process. Other schools have abandoned interviews on the grounds that a 15-minute interview provides no information additional to the entry qualification grades, the applicant's written “personal statement,” and their academic referee's comments. Other disincentives to interviews are the person-hours required to interview up to 800 applicants (800 × 0.25 h × 2 interviewers) and the threat of judicial review by unsuccessful applicants if it is shown that each applicant did not have an identical “experience” (ie, the same interviewers) with the same structured interview. At least one school has adopted a “middle-way” in utilizing a written entrance examination as part of their selection process.
A further criterion for entry to an MPharm or OSPAP program is “fitness to practice.” Although, formally, universities provide an academic qualification while the RPSGB controls professional registration, it is deemed unethical to knowingly admit a student to a program if it is clear that the student would later be barred from registration due to “fitness to practice” issues. Each university is therefore required to ensure that the applicant does not suffer from any disability or illness that may prevent registration, and that there is no history of criminal conviction that may prevent registration. Although RPSGB expects the individual universities to make such decisions, they have recently offered to assist with the decision-making process where the outcome is unclear or borderline. A similar process could occur should a student already registered in a program commit an offence or become ill or disabled; the decision would need to be made as to whether to exclude the student from the MPharm program.
EDUCATION COSTS
In recent years, funding of UK higher education has changed. Thirty years ago higher education was free to all qualified UK applicants, and the government paid a means-tested allowance to cover accommodation and subsistence. Non-UK entrants paid the full costs of the program. This changed so that tuition fees were paid, but living expenses had to be funded by means of an interest-free loan from the Government's Student Loan Company, which was repayable when the eventual graduate reached a threshold salary. At about the same time, a reciprocal arrangement within the EU meant that EU citizens were eligible for free tuition. Approximately 10 years ago the government introduced a subsidized tuition fee for all UK and EU students of approximately £1000 per year (£1 = $2.00 approximately) which had to be paid on registration with the university. Three years ago the system became more complicated with the introduction of “top-up” fees. The government decreed that universities would no longer receive the £1000 student contribution, but that universities may opt to charge a fee of up to £3000 per year, which would be payable in installments by students after graduation when they reached a threshold salary. This applied to UK and EU citizens; thus, in theory, a student from Greece attending university in the United Kingdom and then returning to employment in Greece would be monitored by UK authorities and invoiced when they achieved the euro equivalent to the salary threshold. Universities almost unanimously opted to charge the full £3000 discretionary fee. UK and EU students attending university in England therefore accumulate debts of £3000 per year tuition fees for 4 years, together with the costs of accommodation and subsistence. However, the Welsh and Scottish regional governments have chosen not to impose the top-up fees; thus, tuition is free for Scottish, Welsh, or other EU students, but £3000 per year for English students studying in Scotland or Wales.
The latest development in UK higher education concerns “equivalent or lower qualifications” (ELQs). In 2008, the government announced that the £3000 top-up fees apply only to first degrees; thus, any graduate seeking entry to another bachelors program will be required to pay the full cost of tuition/education upon registration, typically £8,000-£10,000 (approximately $16,000-$20,000) per year. Interestingly medicine, nursing, and teaching programs are exempt from this decision because the 3 subjects are funded directly from other government departments. Pharmacy, although a masters degree program, is able to admit bachelors degree program graduates, but they are required to pay the full cost of tuition since pharmacy programs are funded from an overarching government university-funding agency, the Higher Education Funding Council for England (HEFCE), rather than directly from an autonomous government department (as is the case with medicine, nursing, and teaching).
PROGRAM CONTENT
MPharm programs are all accredited by the RPSGB, typically on a 5-year basis. The programs are assessed against a list of 50 criteria relating to the environment and management and a further 51 criteria regarding curriculum content. The specified curriculum is firmly based on the European required syllabus. Examples of the general environment and management criteria are:
Students undertake at least 3,000 hours of directed study of pharmaceutically relevant subjects within a full-time 4-year degree program.
Those components of the degree program that collectively deal with the actions and uses of medications occupy no less than 35% of the curriculum, irrespective of the extent of specialization in the final year.
At least 35% of those parts of the degree program common to all students involve the students preparing and analyzing the outcomes of experiments, exercises, or observations wherein they reach their own findings or conclusions.
During the processes of curriculum review and development, academic staff properly taking account of major advances and developments potentially impacting on pharmacy.
Has pharmacy undergraduate teaching taken place alongside, and with reference to, research and other postgraduate studies?
For the purposes of proper ethos, quality assurance, and scientific/professional leadership, the program should be controlled and delivered by an autonomous school of pharmacy.
The school of pharmacy has within its academic staff at least one pharmacist who is a professor or of equivalent authority in the institution.
During the final year, students are required to pass an assessment of knowledge and understanding of any important recent changes in pharmacy law and/or professional requirements.
The indicative syllabus (curriculum content) is much less prescriptive with generic requirements such as the teaching of:
Etiology and epidemiology of major diseases and the principles of drug treatment.
Molecular basis of drug action and the actions of drugs within living systems; molecular, cellular, biological, and physical aspects.
Physico-chemical aspects of drugs and biological systems, including thermodynamics and chemical kinetics.
Analytical methods: principles, design, validation and application.
Sale and supply of medicines, including evaluation and management of risk and provision of advice.
Codes, standards, and systems of governance and practice; risk management; and personal accountability, to include the need for, and means of, continuing professional development.
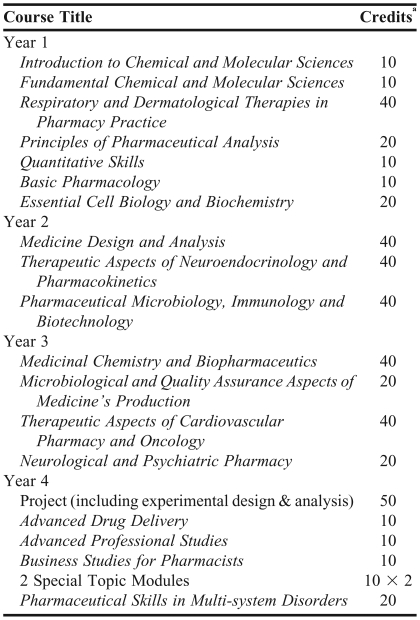
Table 1 lists the typical MPharm program. In practice, most of the UK MPharm programs are broadly similar, although not sufficiently similar to permit easy transfer between programs; thus, a student completing year 1 at a particular school will have difficulty gaining direct transfer to year 2 at another school. The typical program will cover aspects of fundamental chemistry, math, biology, and physiology in year one, together with an introduction to the practice of pharmacy and some guidance on academic or study skills. There is also usually at least 1 half-day visit to a hospital or community pharmacy (in the whole year). Years 2 and 3 then build on this to cover, in more detail, medicinal chemistry mathematics, product formulation, analytical chemistry, and systems-based pharmacology and therapeutics, including pharmacy practice. Again most programs will involve some form of experiential visit and completion of a log-book or training record, typically 1 week per academic year in years 2, 3, and 4. The final year is normally comprised of an extended research project, which must involve some form of generation, analysis, and interpretation of novel data, and some optional in-depth study of selected topics.
Table 1.
Typical RPSGB-accredited MPharm Program Outline
a1 credit=10 hours of study
A minority of schools offer a “sandwich option” in which students take a break in studies following completion of year 3, and take up pharmacy-related, paid employment for 6-12 months. They then return to university to complete their studies. The aim is that the placement counts towards their preregistration training, but more importantly gives them greater insight into the relevance of the subject matter taught at the university. A 6-month sandwich placement would equate to 6 months preregistration training
EXPERIENTIAL EDUCATION
There are no formal requirements for experiential education or clinical placements (which is the term used in the UK) within the MPharm program, but it has become an expectation. Most schools offer at least 1 week total over the 4 years; some offer much more (up to 4 weeks). It is clinical placements that have created most anguish to program leaders over the last few years. Hospitals and some other pharmacists have made it a requirement that students have been fully screened by the UK Criminal Records Bureau (CRB) before being allowed entry to hospital premises. When students have any form of criminal record, (for example shoplifting as a teenager, or cautions for public order offenses) there is the need for an inquiry as to whether they pose a threat to patients. UK health authorities also require that students fulfill various health criteria such as having vaccinations. These requirements have become de facto program requirements, but because health authorities have imposed them abruptly, schools are in a position of having students in latter stages of the program who are unable to complete clinical placements because they do not meet the health criteria introduced after entering the program.
An added complication is that many UK health authorities are levying a fee for providing students with clinical experience. A typical fee might be £50 per student per day. This has arisen partly due to the economic climate and financial accountability of clinical managers, but also because, unlike pharmacy programs, the government pays hospitals to provide a training environment for student doctors and student nurses. Thus, universities are now forced to make the decision of whether to fund the placements to the detriment of other areas of the program (eg, laboratory exercises), or whether to decrease the extent of clinical experiential learning. In mitigation, all schools employ “teacher-practitioners,” practicing pharmacists contracted to teach for 1 or more days per week, who are able to provide relevant, up-to-date clinical examples and case studies.
Assessment within the pharmacy program in all UK schools of pharmacy relies predominantly on performance in written, theoretical examinations. Invariably there is also a contribution from coursework exercises requiring the writing of reports and interpretation of data; the research project falls within this latter category and usually contributes approximately 15%-20% to the final award. Ever more programs are reducing the contribution of coursework assignments due to issues of plagiarism. Detection of plagiarism from Web sites or from students from earlier cohorts now occupies inordinate amounts of academics' time.
Competency-based assessment usually takes the form of a student logbook or portfolio in which the student records that the he/she has taken a patient drug history, or measured a blood pressure appropriately, for example. These are simple pass-fail criteria ratified by a suitably qualified person such as the pharmacist supervising the clinical placement. Most schools of pharmacy also employ some form of objective structured clinical examination (OSCE) in which students rotate through a series of stations where they are presented with tasks or scenarios that have to be completed within a time limit (5-10 minutes). Often schools employ actors/general public to role play patients. These OSCEs are essentially assessed on a competency basis (pass-fail), although a numerical grade is assigned in order to allow the assessment to contribute to the final award classification. Completion of the logbook is not graded, but satisfactory completion is necessary for progression to the next stage of the program or graduation.
In comparison to other European pharmacy programs, the UK programs stand out in that they provide the underlying scientific, and theoretical knowledge, alongside experimental and clinical expertise. Therefore, at the end of the 4-year program, the graduate is fully equipped to enter the clinical/practice arena. This differs from some other European programs where the university component of the education concentrates purely on the scientific aspects before the students graduate and enter the pharmacy practice training arena. The UK programs, at 4 years, are the shortest university programs in Europe (elsewhere in Europe, pharmacy programs are 5-6 years).
PHARMACY PRACTICE
Approximately 2000 pharmacy graduate enter preregistration each year. With the advent of new schools of pharmacy, and increased enrollments at established schools, this number is set to rise significantly. Students are selected by their preregistration employers on the basis of predicted grades, interviews, and references. There are more than enough preregistration placement providers to cover the increased student output; however, because not all registered providers offer placements each year, it is becoming more and more difficult for students to obtain placements of their choice. It is envisaged that in the near future there will be a degree of “unemployment” of new graduates at the preregistration stage, and some—probably weaker graduates—will be unable to secure a preregistration placement. To some extent, this is seen as beneficial to the profession (survival of the strongest), but in other respects it will inevitably have an impact on applications to schools of pharmacy when the promise of guaranteed career and employment fades. Ironically, employers already report difficulty in attracting suitable qualified pharmacists. Thus, the situation is developing into one of a shortage of preregistration places in the market, exacerbated by an excess of graduates looking to embark on their careers (ie, supply of graduates exceeding demand for them). Already, one university that had taken the first steps on development of an MPharm program has withdrawn due to market forces and the future demand for places on pharmacy programs.
By far the majority of pharmacy graduates enter the community/retail arm of the profession, followed by hospital, industry, and academia.4 Industry has reduced its demand for pharmacy graduates in light of the increase in the number of programs providing graduates in pharmaceutical sciences. Academia, however, is still in need of registered pharmacists, but finds itself unable to attract suitably qualified applicants; this situation has not changed significantly over the last 20 years. The reason is twofold: first, academic salaries do not compete with salaries within the other sectors of the profession; and second, there are only a limited number of practicing pharmacists that fulfill the research output criteria currently expected by universities. A new issue has had a further impact on academic pharmacy; annual registration fees for pharmacists have increased threefold in the last few years to £400 per year (approximately $800), while average salaries for pharmacists are £40,000 (approximately $80,000). Many academic pharmacists are therefore questioning the need to remain on the register if they have no clinical commitment. The universities and RPSGB are eager to encourage them to re-register, but the debate continues. Other career destinations for pharmacists, again which do not require continuedregistration, would be finance, law, and journalism.
PHARMACIST PRESCRIBING
The major development in the practice of pharmacy has been the introduction of supplementary prescribing and independent prescribing carried out by pharmacists. Supplementary prescribing is prescribing of repeat or modified prescriptions following diagnosis by a qualified clinician, whereas independent prescribing involves an element of diagnosis and choice of medicines. It is the professional responsibility of pharmacists not to prescribe outside their area of expertise. Qualification as a supplementary or independent prescriber currently requires practicing pharmacists to undertake additional accredited training subsequent to them becoming recognized as proficient in a particular pharmaceutical specialty, eg, gerontology, oncology, or renal medicine. Proficiency is determined by a pharmacist's depth of experience in a particular setting and is ascribed by the pharmacist's employer. In future years, all MPharm graduates will have covered the necessary supplementary and independent prescribing syllabus as part of their undergraduate program; hence, progression to accredited prescriber status will not require additional training. The addition of material pertaining to supplementary and independent prescribing to the undergraduate syllabus has greatly increased the emphasis on therapeutics and prescribing practice.
The final consideration for future pharmacy programs is the “skills escalator.”5 Pharmacy technicians are now required to possess recognized national qualifications and be registered with the pharmaceutical society. Government bodies would like to see the situation whereby qualified, registered pharmacy technicians should be able to progress to registration as a pharmacist without the need for undertaking the full 4-year program and 1-year preregistration training. MPharm Program development teams are therefore considering the variety of mechanisms for provision of accelerated entry and/or part-time study modes of pharmacy education.
EDUCATIONAL CHALLENGES
A common issue in student assessment that has been of increasing note over the last 10 years is academic dishonesty in general and plagiarism in particular.6 The main reason for this is the availability of source material on the Internet, and even web sites which offer assessment material for download at an appropriate price. There is clearly a conflict between the dishonesty involved in plagiarism and the spotless honesty and attention to procedure, ethics, and rules required of the professional pharmacist. Most schools of pharmacy have set procedures designed to detect such dishonesty such as Turnitin software (iParadigms, LLC, Oakland, CA) which requires students to submit their assignments electronically.7 The software then compares the submitted assignments with all others submitted at the time and those submitted prior to that time and instantly detects unoriginal material.
There is a further issue of graduate employability. Currently, a pharmacy degree almost guarantees employment. With the increased number of schools of pharmacy opening in the UK, and therefore, an increased number of graduates, this may change. This will have several effects: first there could be unemployed graduates, which would hopefully improve the quality of the profession by keeping poorer practitioners unemployed. The longer-term outcome, however, is that fewer students will apply for pharmacy programs as they will cease to guarantee employment after graduation; hence, the number and quality of applicants could fall.
A further challenge lies in the issue of competency. There is no universally accepted competency framework or performance standard at the point of graduation or post-registration for pharmacists in the same way as there is for dentists, doctors, and opticians, whose professions each have a method to ensure uniformity of competency-based skills.8 The national registration examination is based on theory rather than practice; thus, in the case of pharmacists, fixed criteria tend to be knowledge-based rather than competency-based, and programs are not required to have a competency-based assessment. They are required to enable the student to demonstrate a knowledge of dispensing and a mere ability to dispense, rather than taking the holistic approach of demonstrating competence to achieve all the required outcomes of dispensing, such as counseling, limited diagnosis, and so forth. Moreover, there is much discussion about the effectiveness of assessing competency. For example, a student might fail an OSCE for not washing his hands when all other aspects of his performance was satisfactory. But how does one grade the “handwashing competency” of the student who does wash his hands (ie, can one wash one's hands particularly well?), or must this type of competency-based assessment become a mere pass/fail exercise?
CHANGES IN PRACTICE IMPACTING ON EDUCATION
The main change that is currently affecting practice is the introduction of supplementary and independent prescribing for pharmacists. After receiving appropriate training, pharmacists may write modified prescriptions following diagnosis by a qualified clinician. Independent prescribing involved an element of diagnosis and choice of medicines; for the latter situation there is a limitation that the prescription must be within the prescriber's area of expertise. Undergraduate programs will now include the additional training required for prescribing responsibilities. Probably the biggest challenge is the science versus practice debate. Do UK pharmacists need the science skills currently taught in order to practice effectively? In the UK there is a mixture of practical and theoretical science in years 1-4, interspaced with clinical professional practice. The European model normally has years 1-3 focussing on pure science, with years 4-5 concentrating on the clinical aspects. In the UK model, if the students do not need the science skills taught, when the curriculum changes, how will universities handle the relative underemployment of their science professors and the underuse of the science laboratories? To what extent is science taught because that is what has always been taught and that is what we know? This last question is occupying much of the discourse in the UK currently and may be the prelude to wider change in years to come.
SUMMARY
Challenges for UK pharmacy education over the coming years are the prevention of easy access to MPharm programs by graduates of other subjects; the possibility of a shortage of employment opportunities for pharmacy graduates; the potential for accelerated progression of pharmacy technicians to pharmacy graduates and the possibility of providing part-time courses in pharmacy. In addition, the requirement to introduce more therapeutics into the courses to cater for the new roles of supplementary and independent prescriber must be faced, at the same time debating the relative weighting of science and practice within the course.
REFERENCES
- 1.Chamberlain J. Reports: Bologna Agreement. Pharm J. 2005;275:667–8. [Google Scholar]
- 2.Wilson K, Jesson J, Langley C, Clarke L, Hatfield K. MPharm programmes: where are we now? Royal Pharmaceutical Society of Great Britain Available at: http://www.rpsgb.org/informationresources/downloadsocietypublications/. Accessed November 20, 2008.
- 3.Willis S, Shann P, Hassell K. University of Manchester: Centre for Pharmacy Workforce Studies; 2006. Studying pharmacy: who, when, how, why? what next? A longitudinal cohort study of pharmacy careers. [Google Scholar]
- 4.Jesson K, Langley J, Clarke L and Hatfield K. Pharmacy undergraduate students: career choices & expectations across a four-year degree programme. A report for Royal Pharmaceutical Society of Great Britain.
- 5.Making pharmacy education fit for the future, Report of the Pharmacy Education R&D Reference Group, Royal Pharmaceutical Society of Great Britain. Available at: http://www.rpsgb.org/pdfs/maphedfitforfuture.pdf. Accessed November 7, 2008.
- 6.Bates IP, Davies JG, Murphy C, Bone A. A multi-faculty exploration of academic dishonesty. Pharm Educ. 2005;5:69–76. [Google Scholar]
- 7.Turnitin Homepage. http://turnitin.com/static/index.html. Accessed November 7, 2008.
- 8.Duggan C. Reforming educational career development for practitioners in the UK, presented at Trends in Pharmacy Education, European Association of Faculties of Pharmacy Meeting, September 20-22, 2007.
- 9.Sosabowski MH, Ingram MJ. 21st century issues in pharmacy education in the United Kingdom. Am J Pharm Educ. 2003;67 doi: 10.5688/aj7206130. Article 122. [DOI] [PMC free article] [PubMed] [Google Scholar]