Abstract
Accredited pharmacy programs in Australia provide a high standard of pharmacy education, attracting quality students. The principal pharmacy degree remains the 4-year bachelor of pharmacy degree; however, some universities offer graduate-entry master of pharmacy degrees taught in 6 semesters over a 2-year period. Curricula include enabling and applied pharmaceutical science, pharmacy practice, and clinical and experiential teaching, guided by competency standards and an indicative curriculum (a list of topics that are required to be included in a pharmacy degree curriculum before the program must be accredited by the Australian Pharmacy Council). Graduate numbers have increased approximately 250% with a dramatic increase from 6 pharmacy degree programs in 1997 to 21 such programs in 2008. Graduates must complete approximately 12 months of internship in a practice setting after graduation and prior to the competency-based registration examinations. An overview of pharmacy education in Australia is provided in the context of the healthcare system, a national system for subsidizing the cost of prescription medicines, the Australian National Medicines Policy and the practice of pharmacy. Furthermore, the innovations in practice and technology that will influence education in the future are discussed.
Keywords: pharmacy education, Australia, curriculum, international
INTRODUCTION
Australia has been educating pharmacists with formal courses for more than 125 years. Originally, pharmacists were educated through an apprenticeship system; however, this has evolved into high standard university programs producing broadly educated pharmaceutical scientists with advanced clinical skills who are eligible for registration as pharmacists after a period of supervised experiential practice.
With a population of approximately 21 million people, the Australian continent is roughly the same size as the continental United States and is comprised of 6 states (New South Wales, Queensland, South Australia, Tasmania, Victoria, and Western Australia) and several territories (the Northern Territory, the Australian Capital Territory, and others). It has a government-funded universal healthcare system, called Medicare, which provides Australian citizens and permanent residents with affordable, accessible, and high-quality health care. Medicare provides access to free treatment as a public (Medicare) patient in a public hospital and free or subsidized treatment by all medical practitioners, and for specified services through participating optometrists and dentists.1
The Pharmaceutical Benefits Scheme (PBS)2 is a national system for subsidizing the cost of most prescription medicines. The aim of the PBS, which commenced in 1948, is to provide reliable and affordable access to a wide range of necessary medicines. A Pharmaceutical Benefit item is a medication listed in the current pharmaceutical benefits schedule and is only available on presentation of a duly written prescription from a medical practitioner, dental practitioner, or optometrist. The medications included on the list are determined by the Commonwealth Minister for Health and Ageing on the advice of the Pharmaceutical Benefits Advisory Committee (PBAC).
A person obtaining a dispensed prescription under the PBS pays a patient copayment (currently A$30.30 for general patients). Concession Card holders, those covered by government entitlements (low income earners, welfare recipients, pensioners, HealthCare Card Holders, ex-military service personnel, and their families), have a reduced copayment (currently A$5.00). Additionally, there are safety net provisions for a reduction in the patient copayment contribution once a family has exceeded a certain dollar amount on PBS-subsidized medications in a calendar year. When a family on General Benefits has accumulated PBS prescription expenditure of A$1141.80, the copayment for a prescription item for the rest of the calendar year is A$5.00, and when Concessional Card holders reach an expenditure level of A$290.00, they subsequently receive their prescriptions free of charge for the rest of the calendar year. On January 1 of the following year all copayment totals begin again at zero and patients must commence paying toward their maximum for that year.3
PHARMACY EDUCATION IN AUSTRALIA
Types of Programs
The principal pharmacy degree offered by Australian universities to enter the profession is a 4-year bachelor of pharmacy degree. From 2003, some universities began offering graduate master of pharmacy degree programs, which consist of 6 semesters taught over a 2-year period. Following successful completion of one of these university-based bachelor's or master's degree programs, graduates must complete approximately 12 months of internship (previously referred to as preregistration training) in a practice setting (typically hospital or community pharmacy) under the supervision of a Pharmacy Board-approved pharmacist. The internship, which involves supervised practice and a program of coursework, is under the control of the relevant state or territory registering body (known as the Pharmacy Board) which undertakes assessment of the interns to ascertain their fitness for practice. Thus, for those who undertake a 4-year bachelor's degree, which is the most common pathway to registration, the overall program from entry to registration is 5 years.
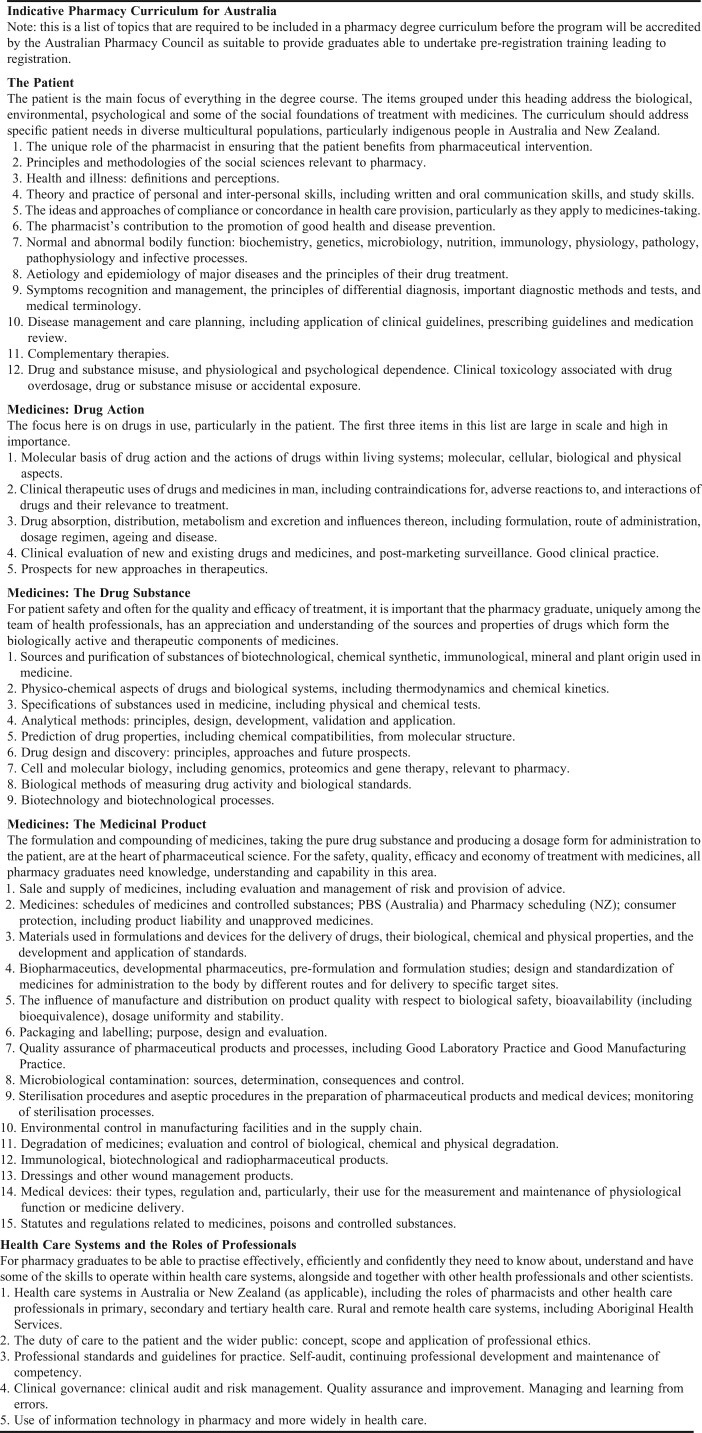
The graduate-entry master of pharmacy degree programs that have recently become available are similar to the bachelor's degree programs offered. The curriculum for the master's degree is based on the same indicative curriculum as the bachelor's degree, and the master's degree offers no advantage in terms of career opportunities. The indicative curriculum (Appendix 1) is a list of topics that must be included in any pharmacy degree program. Graduate entry programs are simply an accelerated pathway to completion of a pharmacy degree for those students who already hold at least a bachelor's degree in a related or other discipline, as the degree can be completed in 2 years rather than the usual 4 years. No pharmacy school in Australia currently offers a doctor of pharmacy (PharmD) degree as the entry point for registration; however, many offer a range of postgraduate degrees such as a master of clinical pharmacy, doctor of clinical pharmacy, graduate diploma, or graduate certificate award, in addition to research degrees such as research master's and PhD degrees. Curricula for these postgraduate coursework degrees vary in their emphasis but generally include components of therapeutics and, at the master's level and beyond, completion of a practice-based research project.
Selection Process
The majority of students enter a pharmacy program directly from secondary school, although some students transfer from other tertiary (ie, university) programs. Generally, many more qualified applicants apply each year for entry into pharmacy programs than can be accommodated. For example, in 2008 at Monash University, 1,558 applicants competed for approximately 200 first-year bachelor of pharmacy places. The number of students accepted into pharmacy programs varies from institution to institution as do the number of students who apply. Some of the larger, more established schools accept 200-250 students into their program, whereas other schools, especially the newer, less well-established schools and graduate programs, have much smaller enrolments.
For students applying for entry to a bachelor of pharmacy degree program following completion of their secondary education, the results of the final years of secondary school are a key criterion for entry. In each Australian state, all students undertake the same program of study for each year-12 secondary school unit of study and complete centrally administered assessment tasks (assignments and examinations). Grades are calculated by the central examinations council in each state. In the State of Victoria this is the Victorian Curriculum and Assessment Authority. All students undertaking year-12 units of study are ranked against one another based on their grades in each unit they have completed, using a complicated system to maintain equity. The International Baccalaureate is also recognized in Australia and grades are converted to create a score that enables students to be ranked against all other students. These rankings (the Equivalent National Tertiary Entrance Rank or ENTER) are used to select students who have applied for entry into tertiary programs of study.
Students usually apply for all university programs through a central agency (in the State of Victoria, the Victorian Tertiary Admissions Centre) and nominate up to 8 programs of study at any tertiary institution for which they wish to be considered. This list is finalized by the student in mid-December when final year-12 results are available. Faculties within each university then have until mid-January to select the required number of students from those who have applied for the programs offered within that faculty (the academic year in Australian schools and universities is approximately February to November). Due to the number of students who apply for entry into pharmacy and the short time available for selection, the decision is made predominantly on the basis of students' ENTER score. Their performance in the Undergraduate Medicine and Allied Health Admission Test (UMAT)4 or similar general test such as the Special Tertiary Admissions Test (STAT),5 may also be considered for entry into some schools. The UMAT is designed to assess the level of skills in the areas of logical reasoning and problem solving, understanding people and non-verbal reasoning and is used specifically to assist the selection of students into undergraduate medicine and some health science degree programs, such as pharmacy.4 The STAT is a series of related tests designed to assess a range of competencies commonly considered important for success in tertiary study. STAT assesses the student's ability to understand the material presented and to think critically about issues rather than the student's knowledge of a curriculum or a specific academic subject.5 Other admission requirements range from interviews to submission of a personal data file.
Similar to other Australian schools of pharmacy, selection for entry into the bachelor of pharmacy program at the Faculty of Pharmacy and Pharmaceutical Sciences, Monash University, is based on high levels of achievement in the prerequisite areas of chemistry, mathematics, and English in year-12 of secondary school (year-12 level in these subjects is approximately equivalent to college level in the United States). Applicants who are offered a place at Monash University are generally in the top 2%-3% of all Victorian students (ENTER 97-98). Applicants are also required to achieve high scores (usually in the top 20%) on the UMAT. The selection criteria for other schools may vary considerably from this and a lower ENTER score cut off may apply. While the majority of students (approximately 75%) enter a bachelor of pharmacy program following their final secondary school examinations, other modes of entry also exist.6 A significant number of international students are admitted following secondary education in their country of origin and other students may already hold a previous degree or transfer from a partially completed degree in another discipline, such as science.
Students who have completed a relevant undergraduate degree are also able to apply to a postgraduate pharmacy program (master of pharmacy) which will meet the educational requirements for pharmacist training. These graduate-entry programs are open to suitable graduates who have successfully completed prerequisite subjects such as human biology, chemistry, biochemistry, microbiology, anatomy, and physiology within the previous 10 years, with a record of high academic performance. Additional requirements may include a 500-word statement/letter of application and referee reports from suitable individuals who can attest to the applicant's communication skills and application of ethical principles as required for the role of a health professional. An interview may also occur. Applications are ranked and entry is competitive.
Pharmacy Curriculum
A detailed indicative curriculum as outlined by the Australian Pharmacy Council (APC) for Accreditation of Pharmacy courses in Australia7 provides a checklist for curriculum developers and evaluators of the items which should appear in a curriculum if it is to achieve the expected educational outcomes (Appendix 1). While the curriculum items are grouped to give prominence to the patient and avoid traditional categorizations, this organization is not intended to be imposed on schools' curricula. This indicative curriculum applies to both the traditional 4-year BPharm course and the postgraduate MPharm and is used by Australian pharmacy schools as a guide for designing an appropriate course of study.
In general, for undergraduate courses, the early years of the course provide a foundation in the enabling physical, chemical, biological, and social sciences, and include pharmacy practice subjects from first year. The course then leads to more applied and discipline-specific topics, with a strong focus on clinical education. All pharmacy programs in Australia include experiential components. Indeed, this is a requirement set down by the APC as a key element for the accreditation of pharmacy curricula.
The pharmacy curricula in Australia are generally guided by the set of comprehensive competency standards published by the Pharmaceutical Society of Australia8 and accepted by the profession. This document outlines the knowledge, skills, and attitudes required by a practicing pharmacist and is underpinned by the Quality Use of Medicines Framework of the Australian National Medicines Policy.9 While they were primarily designed for professional practice, they also provide useful principles for educational purposes. The Competency Standards describe 8 functional areas (Table 1), each of which is subdivided into elements that describe activities expected in each functional area and performance criteria and evidence guides that can be used to determine competency.8
Table 1.
Each of these functional areas is further subdivided into numerous elements and competency statements
Program Highlights and Innovations
One of the strong components of pharmacy education in Australia is the balance between, and integration of, the enabling sciences, applied pharmaceutical sciences, social sciences, and clinical education. Research-informed teaching is essential to the provision of high quality and contemporary education for pharmacists during their initial degree leading to qualification and registration, and subsequently, as part of continuing education and professional development. The research intensive universities have established research and training programs of excellence, working in partnership with the clinical, hospital, and community pharmacy sectors, which has undoubtedly contributed to the high standard of healthcare provided by community and hospital pharmacists as well as to the quality of pharmacy education. In terms of pharmaceutical science, these universities are very well linked and integrated with national and international biotechnology and industry partners via collaborative research programs and joint initiatives. These broad-based, strong, and established research relationships with the pharmacy and pharmaceutical sectors are essential in supporting ongoing curriculum development and the ability to attract the best and brightest staff into academic pharmacy.
Pharmacy schools in Australia generally communicate with their students and provide information via Web-based programs such as Blackboard/WebCT (Blackboard, Inc, Washington DC). This is not only an effective and efficient means of providing information but also enables the use of advanced teaching methodologies such as discussion groups and assignment submission facilities. Students are generally provided with downloadable lecture notes in advance of lectures to provide the opportunity for preparation and to enable students to concentrate on the actual lecture presentation rather than on note taking.
Schools utilize a variety of technological resources to suit their needs, such as the use of automated lecture capture and delivery systems, which enable students and staff members to access lecture material online, within hours of the lecture. For example, the Lectopia program (Anystream Apreso, East Perth, Australia) originally developed at the University of Western Australia to automatically record designated lectures has been introduced at Monash University to enhance student learning, providing teaching content clarification and assistance with revision. This can be recorded as audio only, or simultaneous recording of the audio and any image that was transmitted through the data projector during the lecture.
The majority of assessment for units within Australian pharmacy programs is by written, practical, and oral examinations, assignments, exercises, essays, practical work, or a combination of these. At Monash University, a simple but innovative program has been developed to provide each student in the third and fourth year with an individual patient profile to be used for allocation of clinical scenarios for assessment of clinical knowledge and patient care.10,11
Experiential Education
The nature of clinical training and its location within a given curriculum varies among pharmacy schools. Some schools have introductory experiential placements (externships) within the first years of the program; such placements are not usually highly clinically focused and are intended to introduce the student to the range of professional activities undertaken by pharmacists. In contrast, all schools have clinical placements incorporated into the final years of the university program after the students have acquired the appropriate level of knowledge in relevant areas such as communication, law, ethics, and therapeutics. In many pharmacy schools, these clinical placements occur predominantly in community pharmacy, with less hospital pharmacy exposure. In some schools, however, the exposure to community and hospital practice is more balanced due to greater access to hospital placement sites. For example, the clinical training within the pharmacy curriculum at Monash University occurs across years 3 and 4 of the pharmacy course. At this university, there are four 3-week rotations whereby each student undertakes 2 hospital placements (the second being at a more advanced level), a community pharmacy placement (within metropolitan Melbourne), and a rural pharmacy placement (most associated with community pharmacy, but some within a rural hospital or across both areas of practice). All 4 of the placement types within the pharmacy curriculum at Monash University are highly structured and each setting offers clear program objectives and a range of resources to support both the student and the preceptor. These placements are compulsory and arranged by the pharmacy school. One of the goals/motivations for creating the rural rotation site was to expose students to pharmacy practice in a rural environment in the hope that it would alert them to the professional (and lifestyle) benefits of living and working in a rural area. When it was introduced there was a shortage of pharmacists in rural and remote regions within Australia (the shortage continues, possibly to a reduced extent). The anecdotal evidence thus far is that many pharmacy students who have undertaken the rural placement are more inclined to contemplate, or actually enter into, a pharmacy career in rural Australia; thus, the rural placement program may prove to be an effective means to assist in addressing the shortage of pharmacists in rural parts of Australia.
To qualify for registration as a pharmacist, a person must have completed a bachelor or graduate-entry master of pharmacy degree recognized by a state or territory pharmacy board as a registrable qualification, and a period of preregistration training and supervised practice (an internship of approximately 12 months).12 Because pharmacy practice is currently not subject to specialization in Australia, a registered pharmacist must be competent to practice in the full range of practice settings. The necessary competencies, as mentioned previously, are set out in the Pharmaceutical Society of Australia's Competency Standards for Pharmacists in Australia (Table 1).8
The internship year is generally undertaken in a hospital or community setting; a small number undertake their training in an industry setting. There are required components of the internship including completion of an accredited education program (such as that provided by the Pharmaceutical Society of Australia, Monash University, and others) and registration is contingent on passing the competency-based pharmacy board examinations. The internship coursework program at Monash University can also be completed as part of a graduate certificate in pharmacy practice.
The structure of the pharmacy board examination varies somewhat between states but is generally in the form of an oral examination at the end of the internship and may involve an Objective Structured Clinical Examination (OSCE). Students are also required to pass a separate Law and Ethics examination, a calculations examination, and the Australian Pharmacists Competency Assessment Test (APCAT).13 The APCAT written examination is offered 6 times per year for Australian preregistration pharmacists. Candidates in any Australian state or territory may attempt the oral examination after at least 75% of the supervised practice hours (internship) have been completed. In order to be eligible for registration, interns must demonstrate that they satisfy the comprehensive set of professional competency standards.8
Accreditation
Pharmacy school and registrable degree program activities in Australia are accredited by the New Zealand and Australian Pharmacy Schools Accreditation Committee (NAPSAC) on behalf of the APC.7 NAPSAC accreditation aims to “provide assurance to the registering authorities, the profession and the public that standards for pharmacy degree education are being rigorously evaluated against comparable standards across Australia and New Zealand.”12 The process has been well formulated and there are clear guidelines for both the accreditation process and relevant criteria. The ongoing development of the process and review systems ensures consistent levels of structure and quality within the various curricula. It aims to ensure that there is an appropriate research base and level of scholarly research activity in all programs to provide for a contemporary educational experience.
In preparation for the accreditation process the school prepares a comprehensive set of documentation addressing the key criteria for accreditation. This is considered by an independent panel of people (representing pharmacy academia, the student body and professional associations) who also undertake a visit to the school over several days to inspect facilities and interview university staff, students, and stakeholders from the profession and other relevant areas. Following the visit the pharmacy school receives a report that may contain points that must be addressed before accreditation is granted. The school is then given time to prepare a response to these points prior to the NAPSAC making a final decision. Full accreditation is for a period of 5 years. Accreditation of a new pharmacy school involves 3 stages12:
Preliminary Approval.
Preliminary approval is granted to a new school to offer a registrable pharmacy degree program after successful initial evaluation of the school and program against the accreditation criteria. Preliminary approval is normally granted prior to, or commensurate with, the entry of the school's first cohort into the program.
Provisional Accreditation.
Provisional accreditation of a new school and its registrable pharmacy degree program is granted after successful review of the performance of the school in terms of its ability to satisfy the accreditation criteria, usually after its first year of teaching. Provisional accreditation continues until a school is able to achieve full accreditation or, in the event of major shortcomings, until accreditation is revoked. Graduates from provisionally accredited schools have a registrable qualification.
Full Accreditation.
Full accreditation may be granted for a period of up to 5 years to a school and course already having provisional accreditation after it has successfully demonstrated through appropriate evaluative procedures that it has satisfied the full accreditation criteria. A school is eligible for full accreditation after its first cohort of graduates has at least 12 months of practice experience following their period of preregistration training.
PHARMACY EDUCATION AND PHARMACY WORKFORCE
Pharmacy education in Australia has undergone major structural change over the past 10 years due to the significant increase in the number of schools offering pharmacy degrees and the number of graduates entering the workforce. In 1997, prior to national accreditation of pharmacy curricula in Australia, there were 6 university programs offering 6 bachelor of pharmacy degrees, with approximately 485 graduates annually. In 2002, this increased to 9 universities offering 9 bachelor of pharmacy degrees producing 720 graduates, and in 2008, there are 16 universities offering 21 pharmacy degrees (14 bachelor and 7 graduate-entry master of pharmacy degrees) producing 1250 graduates.14 The increase in the number of pharmacy programs offered may be due in part to a large shortfall in the number of pharmacists available to meet demand predicted in pharmacy workforce surveys, especially in rural and regional areas throughout Australia.15,16
One mechanism proposed to address the workforce shortage was an increase in the number of pharmacy graduates, although it was also recommended that this should not require significant infrastructure investment.15 The workforce assessment, calculated on projected enrolments at 9 universities (and not the 16 that now offer pharmacy programs) was that by 2007 the predicted number of pharmacy graduates would be 759,15 whereas the actual number for 2007 was 1250. In addition, there are approximately 80-100 overseas trained pharmacists annually who satisfy the requirements of the APC and become registered in Australia. It appears that the provision of new programs for educating pharmacists may have resulted in an over correction and that careful consideration needs to be given to the appropriate “steady state” supply of pharmacists entering the profession. Consequently, there is a developing concern over the medium term viability of the smaller (and recent) pharmacy schools in light of these changes. A new pharmacy workforce survey has been commissioned and should be completed in late 2009.
Current Pharmacy Practice
There are approximately 5000 pharmacies in Australia, and in most states in Australia, ownership of pharmacies is available only to registered pharmacists.17 There are restrictions on the number of pharmacy premises that any one pharmacist can own, either individually or in partnership with other registered pharmacists. As a consequence, although there are a number of buying groups that provide branding identification of pharmacies for advertising purposes, there are no large company-owned chains of community pharmacies operating in Australia.
Most community pharmacies are relatively small businesses, often with the owner also serving as the manager of the business. This structure provides an opportunity for regular contact between the pharmacist for pharmaceutical care of people requiring medication, with mandatory medication counselling for all “prescription only medicines” and “pharmacist only medicines” and counselling strongly recommended for “pharmacy only medicines.”18 Activities of community pharmacists are largely concerned with primary care activities and dispensing medicines prescribed through the Pharmaceutical Benefits Scheme (PBS) with the PBS Regulations controlling both prescribing and dispensing practice. Pharmacists are reimbursed by the government for medicines dispensed under the PBS. Manufacturers of PBS listed medicines produce standard packages of medicines in quantities according to PBS requirements—generally 1 month's supply or one course of treatment.3 This has the benefit that pharmacists or technicians do not have to count tablets, thereby leaving more time for patient contact activities.
Medicines in Australia are classified into 8 schedules with varying controls over sale and supply. Two of these schedules, “pharmacy only medicines” and “pharmacist only medicines,” apply to groups of medicines that can only be supplied through a pharmacy, but do not require a doctor's prescription. Pharmacy only medicines are medicines that require advice from a pharmacist in order to ensure their safe use, and which should be available from a pharmacy; they must be kept in the professional service area of the pharmacy (where there is no public access) and must be under the direct supervision of a pharmacist. Pharmacist only medicines are medicines the safe use of which requires professional advice but which should be available to the public from a pharmacist without a prescription. These medicines can only be sold by the pharmacist personally and must be kept in a part of the pharmacy that is not accessible to consumers. Most of these medicines may not be advertised to consumers.19 Some examples of pharmacist only medicines include inhaled bronchodilators, the “morning after pill,” oral fluconazole, and orlistat. Prescription only medicines (the use and supply of which is restricted) are available only from a pharmacist on presentation of a prescription written by a duly qualified prescriber. This schedule contains a huge list of medicines similar to that of prescription-only medicines in the United States, Canada, United Kingdom, and Europe. In Australia, direct-to-consumer advertising of prescription only medicines is prohibited.15
Practice Opportunities
Once registered, pharmacists are eligible to practice in any setting. The main areas of practice are in community pharmacies (67%) and hospital pharmacy departments (30%).20 A small number of graduates may enter the pharmaceutical industry, return to university for higher degrees in research, undertake research in universities or research institutes, or work in other areas of practice. In community practice, the majority of work is in dispensing and primary health care, with a growing number of pharmacists obtaining credentials to enable them to conduct medication reviews. Pharmacists are also employed in a variety of other positions in academia, government, and within professional organizations.
There are a number of new practice opportunities for community pharmacists in Australia, particularly in the areas of Home Medication Review (HMR) and Residential Medication Management Review (RMMR), which are new pharmacy services funded by the national government. All residents of nursing homes, accommodation homes, or hostels in Australia are eligible for a RMMR. Also, any individual who needs a medication review is able to have an HMR with a General Medical Practitioner's (GP) approval. Only pharmacists accredited by either the Australian Association of Consultant Pharmacy (AACP)21 or the Society of Hospital Pharmacists of Australia (SHPA)22 are eligible to be reimbursed for providing these services.
Accreditation to conduct medication reviews via AACP is a 2-stage process: the preparatory stage consists of training in medication management and preparation of a portfolio of suitable experience, while the assessment stage requires successful completion of 50 multiple-choice questions and 4 hypothetical case studies. Accreditation by SHPA requires certification as a Geriatric Pharmacy Specialist by the Commission for Certification in Geriatric Pharmacy, or certification as a Pharmacotherapy Specialist by the US Board of Pharmaceutical Specialties.22 Re-accreditation is required every 3 years and requires demonstration of continuous professional development (CPD) and medication review activity, followed by a multiple-choice assessment.
Most pharmacists in hospital practice commence work as clinical pharmacists on a general ward, and gradually develop the knowledge and skills to practice in more specialized areas. Career progression requires demonstration of increased skills, acceptance of increased responsibility, and often, a higher qualification. Relevant postgraduate qualifications include those in areas such as clinical pharmacy, pharmacy practice, and public health, with more than 30% of hospital pharmacists having a postgraduate qualification.15,23 Hospital pharmacists with relevant postgraduate qualifications may be entitled to a salary increment reflective of their increased knowledge and skills, and are also more likely to move into more senior roles within the pharmacy department. The career structure for pharmacists in hospitals has, until recently, been focused on management progression. In recent years this has changed with the emergence of more senior clinical positions as clinical pharmacists develop expertise in areas such as intensive care, cardiology, infectious diseases, and oncology.
Following demonstration of competency at initial registration, there was, until recently, no requirement to demonstrate ongoing competency. A number of pharmacy boards in Australia have introduced more stringent requirements for annual registration. In some states, including Victoria, this involves each pharmacist maintaining a record of all professional development activities undertaken and completing a self-assessment of their ability to provide a number of services. In order to maintain general registration, pharmacists must state their ability to provide the following key services: promote and contribute to optimal use of medicines, dispense medicines, prepare pharmaceutical products, provide primary health care, and provide medication and health information and education. The boards reserve the right to grant provisional registration, restricting the services that a pharmacist may provide until he/she demonstrates competence.24
There is momentum within the pharmacy profession (particularly the hospital sector) to improve the methods by which pharmacists demonstrate their competency. There are a number of documents available to assist in this process apart from the profession's competency standards.8 The Society of Hospital Pharmacists of Australia produces a number of Standards of Practice which include Standards of Practice for Clinical Pharmacy, Community Liaison, Provision of Consumer Medicines Information, as well as standards in a variety of specialty areas such as oncology, psychiatry, and critical care.25 The Pharmaceutical Society of Australia also has a variety of standards including Standards for the Provision of Pharmacy Only Medicines and Pharmacist Only Medicines in Community Pharmacy.18
There is also ongoing interest in formal tools to assess competence. The Safe Medication Practice Unit (SMPU) in Queensland Health has implemented a General Level Framework (GLF) for pharmacist activities, which is based on the GLF developed by the Competency Development and Evaluation Group in the United Kingdom (UK). 26 All hospital pharmacists in Queensland are evaluated for competency by a trained evaluator who accompanies them on a clinical visit and then provides feedback on their performance. Other states are investigating the option of introducing similar competency assessments and the universities will potentially have an important role in administering these assessments. There is also potential for competency assessment to contribute to a postgraduate award. This is already in place in the UK where the GLF is one component of a postgraduate diploma in general pharmacy practice.
EDUCATIONAL CHALLENGES AND THE FUTURE OF PRACTICE
Pharmacy education in Australia is facing some important challenges similar to those faced in many other developed countries.27-30 These relate to changes occurring in the profession of pharmacy that will have an impact on the education that needs to be provided for future generations of pharmacists and therefore for the schools of pharmacy providing this education.
The practice of pharmacy has been evolving, moving from a purely dispensing role into a medication management role—a trend which is likely to continue into the future. The practice of pharmacy now has much less emphasis on the dispensing process per se (especially compounding skills) and more emphasis on therapeutics. Pharmacists wish to strengthen their role as “medication experts” and to do so, they will need to improve and expand their advanced patient assessment skills in order to monitor and adjust therapy. Although widespread use of pharmacogenomics to individualize therapy is still in the future, pharmacists need to be able to contribute to these new forms of therapeutic intervention.
Pharmacy education curricula and pedagogical approaches have been changed to accommodate some of these new practice directions, with more focus on teaching patient care skills: communication, patient assessment, and disease state management. There is also increased emphasis on competency-based teaching and assessment to ensure that pharmacy graduates have the clinical skills required to deliver new cognitive pharmacy services. Some skills that pharmacists may need in the near future for provision of advanced services are currently not included in all Australian pharmacy curricula, eg, direct patient assessment or therapeutic monitoring or advanced consultation skills.
The introduction or increased emphasis on clinical areas has led to a reconsideration of the amount of basic science included in the pharmacy curriculum. While it is important that pharmacists have highly developed skills to enable them to be competent delivering patient care both now and into the future, it is equally important that these skills are underpinned by a strong education in the basic sciences. The level of science required to ensure that pharmacists of the future will be able to understand the chemistry and pharmacology of new drugs dictates that these aspects remain important components of pharmacy curricula. However, the science that is included must be relevant to the needs of the practicing pharmacist of the future and demonstrate its importance for maintaining competence to practice.
Currently, pharmacists in Australia are not legally permitted to prescribe prescription only medicines, but can prescribe from the range of pharmacist only medicines. Research is being undertaken to investigate the feasibility of pharmacist prescribing in Australia and to develop workable models of practice, competency standards, and educational programs.31 Pharmacist prescribing is already occurring in the UK and in some areas of North America and will no doubt occur in Australia in the near future. Pharmacist prescribing has the potential to lead to the development of new roles for pharmacists, both in hospital and community practice, increasing professional satisfaction.32,33 The expansion of professional roles will also impact pharmacy education as there will be a need for delivery of education programs to ensure that competent pharmacists are available to undertake these new responsibilities.
All pharmacists have the same level of registration at present and are able to practice in any area. Even now, however, there is some specialization within pharmacy that is likely to be extended in the future. It is unlikely that all pharmacists will have the expertise to provide advanced pharmacy services in the future or, indeed, have a desire to provide these services. Will this lead to overt specialization within the profession? Will there, or should there be, different levels of pharmacist registration? With some pharmacists accredited to provide a narrow range of services within their specialist expertise, as is now occurring for pharmacists accredited to provide medication review in Australia, do we have general pharmacy practitioners and specialist pharmacy practitioners, similar to the medical model? Schools of pharmacy may need to consider whether it is necessary to provide either a specialist postgraduate education program to credential pharmacists for advanced or specialist practice, or specialist pathways within the undergraduate degree program. Currently it is more usual for pharmacists to obtain additional specialist qualifications after their primary degree; however, these structures could be reconsidered in the light of changes to pharmacy practice and pressures on undergraduate curricula to include education in advanced areas, such as pharmacogenomics or patient physical examination techniques.
Pharmacy schools need to ensure that all graduates have literature evaluation skills and a thorough knowledge of evidence-based practice and medical informatics to ensure that they are well equipped for the wide availability and easy access to information and the variable quality of information that is and will become available. Patients are becoming increasingly aware of access to information regarding their diseases and the medication and other treatments available for their management. They are better informed but also in need of knowledgeable people to either help find the information or to make sense of the information they have retrieved. The pharmacist, arguably the most accessible health professional, is the logical person to fill this need. The further evolution of pharmacy within the information age means that pharmacy graduates will need to fully understand the information resources available and the use of technology both in practice and research.30
The advances in technology are also applicable to teaching. With increased numbers of students enrolled in pharmacy courses, academics are faced with an increased teaching workload. The preparation and delivery of e-learning content, the use of Web-interfaces, discussion groups, audience response technology, and digitized lectures improves the learning experience and outcomes; however, there is an associated increase in workload for teaching staff members. Although many assume that providing a variety of teaching methodology enables students to exercise their preferred learning style, there has been little formal assessment of whether outcomes are improved. Further research needs to be undertaken both to assess the effectiveness of e-learning technology on a broad scale, and to document the staff time involved.
The practice of pharmacy in the future will increasingly involve a team-based approach to patient care and the pharmacist's role in that team is yet to be fully defined. Interdisciplinary teaching and learning is in its infancy in most universities in Australia, and how this is achieved and in what context is still to be determined. The determination of appropriate learning outcomes and then embedding these into an already full curriculum are challenges that will need to be addressed in the future. There is at present a major research project at Monash University involving 11 faculties, departments, or groups of health sciences looking at the specific area of interdisciplinary education.
While workforce requirements in Australia appear to have been addressed, this area will need to be continually monitored to ensure that there is not an oversupply of pharmacists. The pharmacy workforce is also becoming increasingly female and the possible longer-term effects of this on the workforce are unknown.15,20
An important challenge facing schools of pharmacy in Australia, similar to the international situation, is the likelihood that there will be a shortage of appropriately qualified academic faculty members, particularly in the pharmacy practice and drug delivery disciplines.27,30,34 This situation is especially acute (and limiting) in the new pharmacy programs in Australia, considering the increase from 6 to 16 schools in a decade. The availability and financial attraction of pharmacy positions in community or hospital settings can make an academic career seem less attractive. The requirement for a postgraduate degree, preferably a PhD, means time is needed to undertake further and intense study. A solution to maintaining academic faculty levels will need to be found, and may include moving toward a model of clinical teachers similar to that used in medical teaching.
The challenge for schools of pharmacy will therefore be to provide education that will provide graduates with the knowledge, skills, and attitudes to move the profession forward, become leaders of change, maintain high standards of professional competence, and deliver pharmacy services that may be very different from those currently available. The curriculum offered must produce graduates who have sufficient basic skills in all areas—basic sciences, clinical sciences, and pharmacy practice—in order to be able to build on that fundamental knowledge over a lifetime of practice.
CONCLUSION
Australia has an advanced system of pharmacy practice that operates within a unique national healthcare framework that is underpinned by Medicare and the Pharmaceutical Benefits Scheme, which provide good quality and affordable medical and pharmaceutical services to all in the community; the Australian National Medicines Policy that sets the agenda for quality use of medicines; and the laws applying to medicinal substances that dictate that medicines are not regarded as ordinary items of commerce. This provides a wonderful opportunity for pharmacists to practice their profession at a very high level and contribute to improved health outcomes. The graduates produced by the schools of pharmacy in Australia are educated and trained to meet existing and future demands of a profession that is ever more patient oriented and focused on the quality use of medicines. Australian pharmacy education programs are graduating high-quality pharmacists with the requisite knowledge, skills, and attitudes to enable them to practice pharmacy at a high level in the current environment and the ability to adapt to future changes and lead the profession.
Appendix 1. Indicative Pharmacy Curriculum for Australia
REFERENCES
- 1.Australian Government, Medicare Australia. About Medicare Australia. 2008; Available at: http://www.medicareaustralia.gov.au/about/whatwedo/medicare.jsp. Accessed November 20, 2008.
- 2.Australian Government, Medicare Australia. Pharmaceutical benefits Scheme (PBS). Available at: http://www.medicareaustralia.gov.au/provider/pbs/index.jsp. Accessed November 20, 2008.
- 3.Department of Health and Ageing. Schedule of Pharmaceutical Benefits for Approved Pharmacists and Medical Practitioners. 2007; Available at: http://www.pbs.gov.au/html/healthpro/publication/view?date=20081101&type=FlashPaper&name=general-schedule. Accessed November 20, 2008.
- 4.Australian Council for Educational Research. Undergraduate Medical and Allied Health Admission test. Available at: www.uac.edu.au/uac/umat.html. Accessed November 20, 2008.
- 5.Australian Council for Educational Research. Special Tertiary Admissions Test. Available at: http://www.acer.edu.au/stat/. Accessed November 20, 2008.
- 6.Smith L, Saini B, Krass I, Chen T, Bosnic-Anticevich S, Sainsbury E. Pharmacy students' approaches to learning in an Australian University. Am J Pharm Educ. 2007;71(6) doi: 10.5688/aj7106120. article 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Australian Pharmacy Council. Accreditation of Pharmacy Degree Courses in Australia and New Zealand. Available at: http://www.pharmacycouncil.org.au/PDF/NAPSACAccredCriteria.pdf. Accessed November 20, 2008.
- 8.Pharmaceutical Society of Australia. Competency Standards for Pharmacists in Australia. 2003; Available at: http://www.psa.org.au/site.php?id=643. Accessed November 20, 2008.
- 9.Australian Government Department of Health and Ageing. National Medicines Policy. 2000; Available at: http://www.health.gov.au/internet/main/publishing.nsf/Content/97C00068C0A2C772CA256F18004685DC/$File/nmp2000.pdf. Accessed November 20, 2008.
- 10.Marriott JL. Development and implementation of a computer-generated “virtual” patient program. Pharm Educ. 2007;7:335–40. [Google Scholar]
- 11.Marriott JL. Use and evaluation of “virtual” patients for assessment of clinical pharmacy undergraduates. Pharm Educ. 2007;7:341–9. [Google Scholar]
- 12.New Zealand and Australian Pharmacy Schools Accreditation Committee. Canberra, ACT: Accreditation Criteria; 2005. Accreditation of Pharmacy Degree Courses in Australia and New Zealand. [Google Scholar]
- 13.Australian Pharmacy Council Inc. Australian Pharmacy Competency Assessment Tool (APCAT) Candidate's Guide; 2007. Available at: http://www.pharmacycouncil.org.au/PDF/APCAT%20Guide%202007.09.01.pdf. Accessed November 20, 2008.
- 14.Australian Pharmacy Council. Canberra, Australia: Australian Pharmacy Council Inc; 2007. Annual Report July 2006-November 2007. [Google Scholar]
- 15.Gadiel D. Canberra: Health Care Intelligence Pty.Ltd; 2003. A study of the supply and demand of pharmacists, 2000–2010. [Google Scholar]
- 16.National Pharmacy Workforce Reference Group. Canberra: The Pharmacy Guild of Australia; 1999. Health Care Intelligence Pty Ltd. A study of the demand and supply of pharmacists, 1995–2010. [Google Scholar]
- 17.The Pharmacy Guild of Australia. About the Guild. Frequently Asked Questions. 2006; Available at: http://www.guild.org.au/content.asp?id=610. Accessed November 20, 2008.
- 18.Pharmaceutical Society of Australia. Standards for the Provision of Pharmacy Medicines and Pharmacists Only Medicines in Community Pharmacy. 2006 November, 2005; Available at: http://www.psa.org.au/site.php?id=1089. Accessed November 20, 2008.
- 19.Australian Government Department of Health and Ageing. Australian Government; 2007. Therapeutic Goods Act 1989. Therapeutic Goods Advertising Code 2007. [Google Scholar]
- 20.Graduate Careers Council of Australia. Pharmacy post-registration graduate destination survey April 2005: Committee of Heads of Pharmacy Schools in Australia and New Zealand; 2005.
- 21.Australian Association of Consultant Pharmacy. Available at: http://www.aacp.com.au/. Accessed November 20, 2008.
- 22.Society of Hospital Pharmacists Australia. Accreditation System for Medication Management Reviews. Fact Sheet 2001 March 2006; Available at: http://www.shpa.org.au/pdf/positionstatement/fact_accreditation.pdf. Accessed November 20, 2008.
- 23.O'Leary KM, Allinson YM. Snapshot of the Australian public hospital pharmacy workforce in 2003. JJ Pharm Pract Res. 2004;34:104–8. [Google Scholar]
- 24.Pharmacy Board of Victoria. Pharmacy services, general registration; 2007. Available at: http://www.pharmacybd.vic.gov.au/cmsdocs/pharmserv_intro.pdf. Accessed November 20, 2008.
- 25.Society of Hospital Pharmacists Australia. SHPA Practice Standards and Definitions. 2007; Available at: http://www.shpa.org.au/docs/practicestandards.html. Accessed November 20, 2008.
- 26.Competency Development and Evaluation Group. Safe Medication Practice Unit, Queensland Health. Available at: http://www.codeg.org/index.php?id=q_health. Accessed November 20, 2008.
- 27.Taylor KMG, Bates IP, Harding G. The Implications of Increasing Student Numbers for Pharmacy Education. Pharm Educ. 2004;4:33–9. [Google Scholar]
- 28.Roche VF. Challenges and Opportunities for schools and colleges of Pharmacy in the next decade. Paper presented at NABP/AACP Combined District 7 and 8 Meeting; Tucson, Arizona: American Association of Colleges of Pharmacy; 2000. [Google Scholar]
- 29.Angaran DM, Bonal J, Eide G, Koda-Kimble MA, Lake KD, Leufkens HGM. Clinical Pharmacy: looking 20 years back … looking 20 years forward. Pharmacotherapy 2000;20(10, Pt2):235S-42S. [DOI] [PubMed]
- 30.Raehl CL. Responding to the Academy's needs. Am J Pharm Educ. 2007;71(6) article 107. [Google Scholar]
- 31.Emmerton L, Marriott JL, Bessell T, Nissen L, Dean L. Pharmacists and Prescribing Rights: review of international developments. J Pharm Pharm Sci. 2005;8:217–25. [PubMed] [Google Scholar]
- 32.Emmerton L, Bessell T, Marriott J, Nissen L, Dean L. Reforming the Quality use of Medicines in Australian Aged Care Facilities: A New Pharmacy Practice Model. Int J Pharm Pract. 2007;15:331–7. [Google Scholar]
- 33.Sansom LN. Future Healthcare delivery- Where is Pharmacy? J Pharm Pract Res. 2007;37:6–7. [Google Scholar]
- 34.Beardsley R, Matzke GR, Rospond R, et al. Factors influencing Pharmacy Faculty Workforce. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720234. article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]