Abstract
BACKGROUND:
Unsedated transnasal gastroscopy is a technique with unverified clinical advantages.
OBJECTIVE:
To evaluate the efficacy and procedure times with transnasal gastroscopy by physicians with no previous experience in transnasal endoscopy.
METHODS:
Unsedated transnasal gastroscopy using 4.9 mm ultrathin transnasal gastroscopes with randomization to two different biopsy forceps was prospectively evaluated during a single day in January 2008. The outcomes included patient tolerance (scale: 1, no discomfort; 10, severe discomfort), physician technical assessment (1, excellent; 10, very poor), gastric biopsy quality, adverse events and procedure times.
RESULTS:
Twenty patients underwent transnasal gastroscopy. Nineteen patients (95%) successfully completed transnasal gastroscopy. The patient-reported mean (± SD) overall discomfort level during the procedure was 4.0±1.9 compared with a physician-estimated level of 3.2±1.7 (P=0.04). Only 10% (n=2) reported they would have preferred sedated over unsedated gastroscopy. Mean total encounter time from anesthesia to discharge was 33.5±9.3 min. The time from anesthesia to insertion was 7.0±5.3 min and from room exit to discharge 6.2±2.9 min. No patients who had gastric biopsies taken (zero of 14) had any of unacceptable quality. The only adverse event was distressing sensations (dyspnea, dizziness) in one patient that started during pre-endoscopy anesthetic application, persisting postendoscopy, but without any abnormalities in vital signs.
CONCLUSION:
Assuming the adverse event was a rare reaction, early experience with unsedated ultrathin transnasal gastroscopy was an efficient, effective and well-tolerated procedure for evaluation of the upper gastrointestinal tract.
Keywords: Endoscopy, Transnasal, Ultrathin, Unsedated
Abstract
HISTORIQUE :
La gastroscopie transnasale sans sédation est une technique aux avantages cliniques non vérifiés.
OBJECTIF :
Évaluer l’efficacité et le temps d’intervention de la gastroscopie transnasale par des médecins sans expérience de l’endoscopie transnasale.
MÉTHODOLOGIE :
La gastroscopie transnasale sans sédation au moyen de gastroscopes ultraminces de 4,9 mm avec deux forceps de biopsie utilisés de manière aléatoire a fait l’objet d’une évaluation prospective au cours d’une même journée en janvier 2008. Les issues incluaient la tolérance du patient (échelle : 1, aucun malaise et 10, malaise important), l’évaluation technique par le médecin, (1 : excellente, 10 : très faible), la qualité de la biopsie gastrique, les événements indésirables et la durée de l’intervention.
RÉSULTATS :
Vingt patients ont subi une gastroscopie transnasale. Dixneuf (95 %) l’ont terminée avec succès. Le taux de malaise global moyen (±ÉT) déclaré par les patients pendant l’intervention correspondait à 4,0±1,9 par rapport au taux estimé par les médecins de 3,2±1,7 (P=0,04). Seulement 10 % (n=2) ont déclaré qu’ils auraient préféré la gastroscopie sous sédation à celle sans sédation. La période moyenne entre l’anesthésie et le congé était de 33,5±9,3 min, entre l’anesthésie et l’insertion, de 7,0±5,3 min, et entre le départ de la chambre et le congé, de 6,2±2,9 min. Les patients ayant subi une biopsie gastrique n’ont obtenu aucune biopsie de mauvaise qualité (zéro sur 14). Le seul événement indésirable était des sensations pénibles (dyspnée, étourdissements) chez un patient, lesquelles ont commencé pendant l’application de l’anesthésie avant l’endoscopie et se sont poursuivies après l’endoscopie, sans anomalie des signes vitaux.
CONCLUSION :
Si on postule que l’événement indésirable constitue une réaction rare, l’expérience précoce de la gastroscopie transnasale ultramince sans sédation était une intervention efficiente, efficace et bien tolérée pour évaluer les voies gastro-intestinales supérieures.
Transnasal gastroscopy is a recently developed technique for evaluating the upper gastrointestinal tract with an ultrathin endoscope. Passage of a transnasal endoscope from the anesthetized nasal cavity to the nasopharynx provides for subsequent direct and straight insertion of the endoscope into the esophagus. The avoidance of the larger traditional gastroscope (9 mm to 10 mm in diameter) and the absence of pressure to the posterior pharynx may minimize gagging and the discomfort associated with transoral gastroscopy (1). The potential benefits of unsedated transnasal gastroscopy include avoiding the risks, costs, and recovery time resources associated with sedated endoscopy (2,3). Additionally, patients may tolerate and prefer transnasal over transoral gastroscopy. Endoscope diameter is an important factor for transnasal tolerance (4). Recently, the Olympus GIF-N180 (Olympus, Japan) was developed as the thinnest transnasal endoscope on the market being the first to break the 5 mm barrier at 4.9 mm diameter, but had yet to be investigated relative to its tolerability by endoscopists naïve to transnasal endoscopy.
The Canadian North Helicobacter pylori (CANHelp) working group is a team of researchers whose initial project aims to investigate H pylori infection in the rural community of Aklavik, Northwest Territories. The use of unsedated transnasal gastroscopy was being considered for use in the Aklavik H pylori study but required evaluation. The objectives of the present study were to evaluate the efficacy, efficiency, tolerance and gastric biopsy quality of ultrathin (4.9 mm) unsedated transnasal endoscopy by physicians with no previous experience with the procedure.
METHODS
Study subjects
Subjects were volunteers or adult outpatients in Edmonton, Alberta, with an indication for gastroscopy (Table 1). All subjects provided informed consent for unsedated transnasal gastroscopy. Patients attended a single-day transnasal endoscopy session at the Royal Alexandra Hospital in Edmonton in January 2008.
TABLE 1.
Patient characteristics (n=20)
| Age, years (mean ± SD) | 57 ± 17 |
| Female, n (%) | 10 (50) |
| Indication, n | |
| Volunteers | 5 |
| Dyspepsia | 5 |
| Reflux | 4 |
| Varices screening | 4 |
| Gastric pathology follow-up | 2 |
Endoscopy procedure
Six physicians skilled in transoral gastroscopy, with no previous transnasal endoscopy experience, underwent a group training session the same day before beginning the procedures. Four physicians had at least 15 years of transoral gastroscopy experience. Two physicians had just completed their gastroenterology training in the past six months. The training session included a demonstration of the technical features of the transnasal endoscope by an Olympus representative. Subsequently, the nurses and physicians watched an Olympus training video of the transnasal procedure performed on two patients.
Patients received preprocedural topical nasopharyngeal anesthesia in a station outside the door of each endoscopy room. The anesthesia regimen was a combination of 4% xylocaine solution sniff (5 mL) and gargle (10 mL) separately, and 2% xylocaine gel (5 mL) cotton tip application to the full depth of the nasal cavity. Patients subsequently underwent unsedated transnasal gastroscopy with an Olympus GIF-N180 endoscope. The instrument is a 4.9 mm diameter endoscope with a working length of 110 cm and a 2.0 mm single instrument channel. The procedure was considered complete after reaching the descending duodenum. From volunteers or a subgroup of subjects with indication for gastric biopsies, one antral, one incisura and two body biopsies were taken for histology. In addition, four biopsies were taken for H pylori culture. The biopsy protocol was developed as part of the Aklavik H pylori study. Biopsy forceps type was randomized by coin toss to one of two different 2 mm diameter biopsy forceps (Olympus FB-241K standard smooth oval (5 mm cup) with needle or FB-221K alligator jaw step (5 mm cup) with needle.
Outcome assessment
Patient tolerance was assessed with a questionnaire administered immediately after they were ready for discharge (Table 2). Question responses were based on a scale of one to 10, with 1 = no discomfort, 5 = moderate discomfort and 10 = severe discomfort. Physicians were surveyed on technical factors after each procedure. Technical question responses were based on a scale of one to 10, with 1= excellent, 5 = moderate, 10 = very poor. Questionnaires were adapted from previous studies on transnasal endoscopy (1,5). Patient encounter times were recorded in predefined intervals from the time of anesthesia to the time of discharge (Table 3). A gastrointestinal pathologist evaluated the quantity and quality of all the biopsies taken for histology based on a three-point scale: acceptable (diagnostic material), borderline or unacceptable (nondiagnostic material).
TABLE 2.
Patient survey postendoscopy (n=20)
| Question | Mean score | Median score | SD |
|---|---|---|---|
| 1. What was your anxiety level before the freezing? | 4.0 | 4.0 | 2.5 |
| 2. What was your anxiety level during the freezing? | 4.0 | 3.5 | 2.8 |
| 3. What was your pain level in your nose during the freezing? | 2.5 | 2.0 | 1.4 |
| 4. What was your pain level during initial insertion of the endoscope? | 5.3 | 6.0 | 2.7 |
| 5. What was your pain level during the remainder of the endoscopy? | 4.0 | 4.0 | 2.4 |
| 6. What was your level of gagging during the initial insertion of the endoscope? | 2.7 | 1.5 | 2.1 |
| 7. What was your level of gagging during the remainder of the endoscopy? | 2.3 | 1.0 | 1.6 |
| 8. What was your level of overall discomfort during the procedure? | 4.0 | 4.0 | 1.9 |
Based on a scale of 1 to 10, with 1 = no discomfort, 5 = moderate discomfort, 10 = severe discomfort
TABLE 3.
Encounter times for unsedated transnasal gastroscopy (n=20)
| Encounter interval | Mean time, min | SD |
|---|---|---|
| Local anesthesia to room entry | 7.1 | 5.3 |
| Room entry to nasal insertion | 5.3 | 4.2 |
| Nasal insertion to esophagus intubation | 2.7 | 3.8 |
| Esophagus to descending duodenum | 1.9 | 1.3 |
| Descending duodenum to endoscope withdrawal | 7.3 | 3.1 |
| Withdrawal to room exit | 3.0 | 1.9 |
| Room exit to discharge | 6.2 | 2.9 |
| Total | 33.5 | 9.2 |
Data include one patient of 20 who had unsedated transoral gastroscopy after transnasal insertion failed
Ethics approval
The study was reviewed and approved by the University of Alberta Heath Research Ethics Board.
Statistical analysis
Analyses were performed using Stata/IC-10 statistical software (Stata Corp, USA). Distributions of continuous variables are described by the mean (± SD) and the median. For comparisons, the difference in mean and 95% CI are presented; P values are from the nonparametric data, Wilcoxon’s signed rank test for continuous variables and Fisher’s exact test for categorical variables.
RESULTS
A total of 20 patients attended the transnasal gastroscopy session. The characteristics of the participants are shown in Table 1. The age of the patients was 57±17 years. Fifty per cent were female. Ninety- five per cent of patients successfully completed unsedated transnasal endoscopy (19 of 20) (Figure 1), including one who refused the local anesthetic. One case was unsuccessful because of the inability to pass the endoscope through a tight nasal cavity, but then successfully completed unsedated ultrathin transoral gastroscopy.
Figure 1).
The completion rate for unsedated transnasal gastroscopy (n=20)
Patient satisfaction
Postprocedural patient questionnaire results are summarized in Table 2. On the 10-point scale, the mean anxiety level before and during anesthesia was 4.0±2.5 and 4.1±2.8, respectively. The mean pain level during freezing was 2.5±1.4. The mean pain level was highest during the initial insertion of the endoscope, at 5.3±2.7 and lowered to 4.0±2.4 for the remainder of the endoscopic procedure. The mean level of gagging during the initial insertion and the remainder of the endoscopy was 2.7±2.1 and 2.3±1.6, respectively. The mean overall level of discomfort rated by the patients was 4.0±1.9. Overall, only two patients (10%) reported that they would have preferred sedated endoscopy over unsedated endoscopy (Figure 2). Of seven patients who reported having sedated transoral gastroscopy in the past, 86% (n=6) reported that they would prefer to have unsedated transnasal endoscopy if the test was needed in the future.
Figure 2).
Postendoscopy survey of patient preference of unsedated versus sedated gastroscopy (n=20)
Adverse events
There were no major adverse events. However, one patient felt distressing symptoms of shortness of breath during the administration of local anesthesia before the procedure and dizziness after the procedure with a spontaneous recovery within 9 min. However, the patient waited a further 30 min before feeling well enough to go home. The patient’s clinical status and vital signs were monitored throughout without any abnormalities detected; however, he reported feeling extreme cold for several hours after he went home, starting approximately 1 h after leaving the hospital. There were no events of epistaxis that required treatment or recovery for any of the patients.
The two patients who reported that they would have preferred sedated endoscopy had atypical experiences. One had a history of nasal fractures and during the procedure a tight passage to the posterior pharynx was encountered. The patient felt moderate to severe discomfort throughout but insisted on completing the procedure. The other was the patient who developed shortness of breath and dizziness beginning with the administration of local anesthesia. This patient had undergone previous sedated endoscopy and although he preferred the sedated procedure, he attributed his discomfort to the local anesthetic. He indicated that the discomfort level from the endoscopy insertion was low enough that he would be willing to have the unsedated transnasal endoscopy with a lower dose of local anesthesia.
Duration of procedure
The mean patient encounter times are shown in Table 3. The mean total patient encounter time was 33.5±9.2 min. The mean time from local anesthesia to room entry (room entry proceeded after anesthesia was deemed adequate by cotton-tip applicator insertion to the posterior nasal cavity) was 7.1±5.3 min. The mean endoscopy time from nasal insertion to reaching the duodenum was 4.6±4.3 min. The longest mean procedural time interval was the time after reaching the duodenum to removal of the endoscope at 7.3±3.1 min (during which multiple gastric biopsies under protocol were taken from 14 patients). The mean time from room exit to discharge was 6.2±2.9 min.
Physician satisfaction
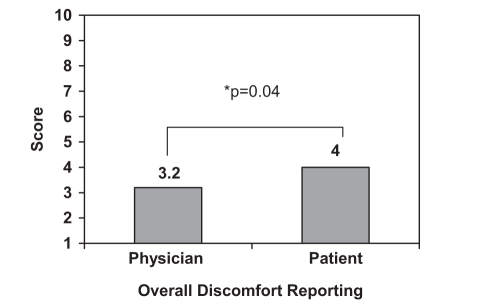
The physician endoscopy assessments, based on a scale of one to 10 are summarized in Table 4. The mean Difficulty with inserting the endoscope transnasally was 2.7±2.3. The mean level of the image quality of the endoscope was 2.2±1.5. The mean ease of handling the endoscope was 2.9±1.9. Physician estimation of patient discomfort was less than patient-reported values (3.2±1.8 versus 4.0±1.9; P=0.04) (Figure 3).
TABLE 4.
Physician technical assessments postendoscopy (n=20)
| Physician assessment | Mean score | Median score | SD |
|---|---|---|---|
| 1. What was the level of difficulty with transnasal insertion? | 2.7 | 2.0 | 2.3 |
| 2. What was the level of image quality (ie, clarity, resolution)*? | 2.7 | 2.0 | 1.5 |
| 3. What was the level of handling of the scope (ie, maneuverability)*? | 2.9 | 2.5 | 1.9 |
| 4. What was the level of overall discomfort experienced by the patient? | 3.2 | 3.0 | 1.7 |
Questions 2 and 3 are based on a scale of 1 to 10, with 1 = excellent, 5 = moderate and 10 = very poor
Figure 3).
Overall discomfort score during unsedated endoscopy reported by physician versus patient (n=20)
Adequacy of biopsy sample
The results of the biopsy assessments with the two different forceps are described in Table 5. A total of 14 patients had biopsies taken. Six patients had a total of 24 histological biopsies by alligator jaw forceps and eight patie nts had a total of 40 biopsies by smooth oval cup forceps (additional biopsies for pathology with the smooth cup forceps were taken from one patient with a gastric ulcer). An acceptable amount of gastric surface epithelium was present in 50% (12 of 24) of alligator jaw forceps biopsies and 85% (34 of 40) of smooth cup forceps biopsies (P=0.004). Gastric tissue orientation was acceptable in 54% (13 of 24) and 68% (27 of 40) of alligator jaw and smooth cup forceps, respectively (P=0.3). When assessed in sets of two samples based on location (two antral/incisura and two body), none of the sets contained an unacceptable quantity for assessment of gastritis. However, 83% of the alligator jaw biopsy sets compared with 65% of the smooth cup biopsy sets had at least one biopsy size of greater than 2 mm (P=0.4). There were no differences in biopsy quality or quantity among endoscopists.
TABLE 5.
Gastric biopsy assessment by forceps type
| Assessment |
Forceps type |
P | |
|---|---|---|---|
| Smooth cup (n=8) | Alligator jaw (n=6) | ||
| Total biopsies, n | 40 | 24 | |
| Quantity of surface epithelium, n (%) | 0.004 | ||
| Acceptable | 34 (85) | 12 (50) | |
| Borderline | 6 (15) | 12 (50) | |
| Unacceptable | 0 | 0 | |
| Orientation of specimen, n (%) | 0.3 | ||
| Acceptable | 27 (67) | 13 (54) | |
| Borderline | 13 (33) | 11 (46) | |
| Unacceptable | 0 | 0 | |
DISCUSSION
Unsedated transnasal gastroscopy has potential clinical and resource utilization advantages. The current pilot study by the CANHelp working group was undertaken to determine the feasibility, efficacy and tolerance of unsedated transnasal gastroscopy by physicians naïve to transnasal endoscopy before use in the community-based Aklavik H pylori study.
Previous studies (4) have demonstrated that transnasal endoscopy is clinically effective and that endoscope diameter is an important factor in patient tolerance of the procedure. Previous studies on transnasal endoscopy have used 5.3 mm to 6.5 mm endoscopes (1,3,5,6). The present study investigated the efficacy of a 4.9 mm ultrathin transnasal gastroscope.
In the present study, unsedated transnasal endoscopy by physicians naïve to the procedure was technically successful with a 95% completion rate. Only one patient was unable to proceed with the procedure because of the inability to pass the endoscope by the nasal turbinates; however, the patient was subsequently able to complete unsedated transoral gastroscopy with the ultrathin endoscope. The high completion rate is consistent with other studies (3,7) using slightly larger calibre transnasal endoscopes in which over 90% of patients successfully completed transnasal endoscopy. Recently, a Canadian group of experienced transnasal endoscopists also reported a high completion rate of 98% (8).
Patient tolerance for unsedated transnasal gastroscopy in the present study was high, with 90% of the patients completing the procedure preferring unsedated over sedated gastroscopy. Cho et al (8) also demonstrated a similar preference rate of 88% for transnasal gastroscopy. Among patients in the present study who had sedated gastroscopy in the past, 85% preferred the unsedated technique. On average, patients rated the overall discomfort as less than moderate on the study scale. The overall patient discomfort in the present initial pilot study is similar to a recent larger study (9) of 140 patients undergoing 4.9 mm transnasal endoscopy by naïve physicians in which discomfort was midlevel between none to moderate. Physicians underestimated the patients’ average overall discomfort but this was a small clinical difference on the evaluation scale used in the present study. The most discomfort reported with the procedure was during the nasal insertion phase of the procedure which is consistent with another study (1). This highlights the importance of performing proper topical anesthesia before nasal endoscope insertion. There is no literature describing the optimal anesthesia technique for transnasal endoscopy. Regimens have included different concentrations, doses and formulations of xylocaine, topical vasoconstrictors and topical decongestants applied to the nasal cavity (10,11). Additional topical anesthesia to the pharynx is used variably in transnasal gastroscopy (1,7). For convenience, the topical anesthesia used in the present study was limited to xylocaine and was applied to both the nasal cavity and pharynx. Additionally, we believed that xylocaine gel applied to a cotton tip was an excellent way to confirm that the posterior nasal cavity was well-anesthetized before endoscopy. Adequate anesthesia takes several minutes to obtain a good effect; the xylocaine regimen used in the present study required 7 min. The level of gagging was minimal in the current study, which may be explained by the small-calibre endoscope, the transnasal technique and possibly to pharyngeal anesthesia as well.
Overall, only two patients (10%) reported they would prefer sedated endoscopy in the future if endoscopy was required. Both of these patients had atypical experiences including the only adverse event encountered – dizziness and shortness of breath from the time of local anesthesia to the end of the procedure and a prolonged recovery time (although no changes in oxygenation or vital signs were detected). Toxicity from topical xylocaine is usually related to systemic toxicity (12) when serum levels exceed 5 μg/mL. In the current study, the maximum dose of topical xylocaine administered in the nasal cavity, where systemic absorption is possible, was 300 mg and is not associated with serum levels greater than 5 μg/mL (10,12). Additionally, xylocaine gel applied to the nasal cavity is associated with limited systemic absorption (12). The frequency of atypical nontoxicity related reactions to xylocaine is unknown. Epistaxis has been reported with the larger transnasal endoscopes in the past at a rate of approximately 5% (3–5). There was no epistaxis requiring active treatment postendoscopy in the present study. Although the present study population was limited only to 20 patients, a larger study with the 4.9 mm endoscope also reported a minimal epistaxis rate of 1% (9). Overall, patients with a history of nasal abnormalities or sensitivity to topical anesthetics may not be optimal patients for transnasal endoscopy.
The technical features of the ultrathin endoscope were rated highly by the physicians. The average nasal insertion difficulty and handling was rated between moderate and excellent. It should be kept in mind that the physicians had no previous familiarity with the transnasal procedure and these assessments occurred during a learning curve for skill and comfort with handling the longer, more flexible single-dial transnasal instrument.
In terms of the quality of the gastric biopsies, the sizes of the specimens appeared smaller than traditional gastroscopy specimens due to the smaller forceps needed for the 2 mm instrument channel. In the comparison between the alligator jaw and the smooth cup forceps, the latter appeared to obtain greater epithelium quantity. There are no previous published reports on biopsy quality with ultrathin endoscopes; thus, further studies are needed to evaluate this issue. However, there were no patients in the present study who had gastric biopsies of nondiagnostic quality to assess for gastritis and atrophy, although a few were of borderline quality, suggesting a need for an adequate sampling number to ensure optimal clinical assessment with transnasal endoscopy. We did not evaluate esophageal or small bowel biopsies, with orientation being an important detail for the latter.
The average total time from the start of nasal anesthesia to patient discharge in the present study was 33.5 min. There was no encounter time to factor in before anesthesia because this was the first step in the study protocol. The duration of endoscopy timed from transnasal insertion in the present study was 11.9 min compared with 8.5 min in a larger study by endoscopy-naïve physicians reported by Meffei et al (9). The endoscopy times described in the present study reflect the initial early experience of physicians with transnasal endoscopy because each physician performed fewer than six procedures while the study by Meffei et al (9) had four physicians who performed transnasal endoscopy on a total of 140 patients. The shorter time reported by Meffei et al (9) may reflect progression along the endoscopy learning curve after a larger number of procedures. Additionally, the longest time interval (7.3 min) was the time after reaching the duodenum to subsequent removal of the endoscope. This interval may be inflated because the protocol in the present study required taking eight biopsy samples from the stomach in 70% of the patients and manually orienting each biopsy sample for histology before endoscope removal. Although transnasal gastroscopy in-room procedure time has been comparable with the sedated transoral route in previous studies (2,6), the average recovery time has been shown to be shorter by up to 30 min (13). In the present study, the average recovery time was only 6.2 min, similar to average time of 7 min reported from another transnasal study (13).
CONCLUSION
Unsedated transnasal endoscopy is a safe, effective and efficient technique for outpatient upper gastrointestinal endoscopy when performed by physicians naïve to transnasal endoscopy. Gastric biopsy quality is adequate with the smaller diameter forceps. Satisfactory outcomes may be achieved after initial performance of a limited number of procedures. As a result of the present pilot study, the technique was deemed feasible for the CANHelp working group Aklavik H pylori study located in the remote Arctic where only a local health centre is available.
Acknowledgments
We wish to acknowledge the contributions of Olympus Canada personnel Peter Bresee, patient care managers Susan Derk and Brenda Holowaty; University of Alberta Hospital and Royal Alexandra Hospital (Edmonton, Alberta) endoscopy nurses Leanne Ellis, Jennifer Antonio, Sheila Berrisford, Kathy Korner, Cinnamon Landhauser, Paula Ledsham, Louise Steffan and service aides Austin Babb, Tamara Bangs, Tammy Church and Sharda Naidu.
Footnotes
DISCLOSURE: Dr Justin Cheung is a clinical research fellow supported by the Canadian Association of Gastroenterology, the Canadian Institute for Health Research, Ferring and the Alberta Heritage Foundation for Medical Research fellowships.
CANHelp working group: Edmonton, Alberta: Karen Goodman, Justin Cheung, Richard Fedorak, Sander Veldhuyzen van Zanten (University of Alberta); Mario Millan (Misericordia Hospital –Edmonton, Alberta); Robert Bailey (Capital Health Northern Health Services Network). Yellowknife, Northwest Territories: John Morse and Tom Guzowski (Stanton Territorial Health Authority).
REFERENCES
- 1.Preiss C, Charton J, Schumacher, et al. A randomized trial of unsedated transnasal small-calibre esophagogastroduodenoscopy (EGD) versus per oral small calibre EGD versus conventional EGD. Endoscopy. 2003;38:641–6. doi: 10.1055/s-2003-41513. [DOI] [PubMed] [Google Scholar]
- 2.Shaker R, Saeian K. Unsedated transnasal laryngoesophagogastroduodenoscopy: An alternative to conventional endoscopy. Am J Med. 2001;111(Suppl 8A):53S–6S. doi: 10.1016/s0002-9343(01)00852-x. [DOI] [PubMed] [Google Scholar]
- 3.Yagi J, Adachi K, Arima N, et al. A prospective randomized comparative study on the safety and tolerability of the transnasal esophagogastroduodenoscopy. Endoscopy. 2005;37:1226–31. doi: 10.1055/s-2005-921037. [DOI] [PubMed] [Google Scholar]
- 4.Craig A, Hanlon J, Dent J, et al. A comparison of transnasal and transoral endoscopy with small-diameter endoscopes in unsedated patients. Gastrointest Endosc. 1999;49:292–6. doi: 10.1016/s0016-5107(99)70003-9. [DOI] [PubMed] [Google Scholar]
- 5.Birkner B, Fritz, Schatke, et al. A prospective randomized comparison of unsedated ultrahin versus standard esophagogastroduodenoscopy in routine outpatient gastroenterology practice: Does it work better through the nose? Endoscopy. 2003;35:647–51. doi: 10.1055/s-2003-41523. [DOI] [PubMed] [Google Scholar]
- 6.Trevisani L, Cifala V, Sartori S, et al. Unsedated ultrathin upper endoscopy is better than conventional endoscopy in routing outpatient gastroenterology practice: A randomized trial. World J Gastroenterol. 2007;13:906–11. doi: 10.3748/wjg.v13.i6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murata A, Akahoshi K, Sumida Y, et al. Prospective randomized trial of transnasal versus per oral endoscopy using an ultrathin videoendoscope in unsedated patients. J Gastroenterol Hepatol. 2007;22:482–5. doi: 10.1111/j.1440-1746.2006.04730.x. [DOI] [PubMed] [Google Scholar]
- 8.Cho S, Arya N, Swan K, et al. Unsedated transnasal endoscopy: A Canadian experience in daily practice. Can J Gastroenterol. 2008;22:243–6. doi: 10.1155/2008/514297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maffei M, Dumortier J, Dumonceau JM. Self-training in unsedated transnasal EGD by endoscopists competent in standard peroral EGD: Prospective assessment of the learning curve. Gastrointest Endosc. 2008;67:410–8. doi: 10.1016/j.gie.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 10.Middleton R, Shah A, Kirkpatrick Topical nasal anesthesia for flexible bronchoscopy. A comparison of four methods in normal subjects and in patients undergoing transnasal bronchoscopy. Chest. 1991;99:1093–6. doi: 10.1378/chest.99.5.1093. [DOI] [PubMed] [Google Scholar]
- 11.Loukides S, Katsoulis K, Tsarpalis K, et al. Serum concentrations of lignocaine before, during and after fibreoptic bronchoscopy. Respiration. 2000;67:13–7. doi: 10.1159/000029456. [DOI] [PubMed] [Google Scholar]
- 12.VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel and the National Center for Patient Safety A guidance on the use of topical anesthetics for naso/oropharyngeal and laryngotracheal procedures. www.pbm.va.gov/criteria/benzocaine.pdf (version current at July 1, 2008).
- 13.Bampton P, Reid D, Johnson R, et al. A comparison of transnasal and transoral esophagogastroduodenoscopy. J Gastroenterol Hepatol. 1998;13:579–84. doi: 10.1111/j.1440-1746.1998.tb00693.x. [DOI] [PubMed] [Google Scholar]