Abstract
Use of prescription opioids for non-cancer pain has increased significantly in recent years, but it is not known if trends differ among the most common non-cancer pain conditions. We examined trends in opioid prescribing for the years 2000 through 2005 for individuals with arthritis/joint pain, back pain, neck pain, and headaches by type and number of pain diagnoses, using data from claims records from two health insurers: HealthCore commercially insured members (N=3,768,223) and Arkansas Medicaid (N=127,866). Rates of headache, back pain, and neck pain diagnoses increased significantly in Arkansas Medicaid enrollees, but more modestly among HealthCore enrollees. Rates of opioid use increased in both groups, with long term use (>90 days supply per year) increasing at twice the rate of any use. Rates of opioid use did not differ widely between non-cancer pain conditions, but long-term opioid use rates doubled with each additional pain diagnosis. Mean days supply and cumulative yearly dose increased between 2000 and 2005 for all pain types and with increasing number of pain diagnoses, but dose per day supply remained relatively stable. The greatest increases in dose among all the pain conditions were seen in short-acting DEA Schedule II opioids.
PERSPECTIVE
This study demonstrates increased use of opioids, particularly long-term use, in non-cancer pain over a six-year period among those with multiple pain types. These results appear to reflect a general increase in use of prescription opioids for non-cancer pain rather than a condition-specific change in prescribing practices.
Keywords: pain, opioids, pharmacoepidemiology
INTRODUCTION
One in five primary care patients endorse chronic non-cancer pain,14 and chronic non-cancer pain is associated with significant functional impairment and disability.6, 16, 29, 37 The use of prescription opioids for non-cancer pain is becoming an increasingly more common treatment strategy, and rates of use have increased significantly in the past two decades. Prescribing rates increased from 8 to 16% of all outpatient visits for musculoskeletal pain between 1980 and 2000,7 and the prevalence of primary care physician visits in which opioids were prescribed increased from 41 per 1000 total visits in 1992-1993 to 59 per 1000 in 2000-2001.22 Between 1998 and 2003, Medicaid prescriptions for opioids nearly doubled, representing approximately four percent of all Medicaid prescription drugs by 2003.5 The marked rate of increase in use of opioids for non-cancer pain, however, is controversial due to evidence of increasing nonmedical use of prescription opioids9, 28 and questions about the efficacy and safety of long-term opioid use.19, 35
Support for the use of long-term opioids differs by pain condition. A recent meta-analysis of randomized trials documented the efficacy of opioid treatment for non-cancer pain compared to placebo, but the mean length of these trials was five weeks and the longest trial was 16 weeks.13 While back pain has been the most frequent non-cancer pain diagnosis reported among those receiving prescription opioids in prior studies of clinical populations,1, 15, 22, 24 results from two recent systematic reviews question their benefit in long-term treatment.10, 19 Recommendations for neck pain generally follow those for back pain. Guidelines on the management of osteoarthritis have traditionally recommended reserving opioids for those patients in whom other first-line treatments, such as NSAIDS, are contraindicated, ineffective or not tolerated.27 An American Heart Association panel, however, has suggested that opioids may be preferred as a first-line treatment over NSAIDS for those with cardiovascular disease.3 The role of opioids in the treatment of chronic or recurrent headache is controversial due to their potential to cause medication overuse headache.17, 25, 39 If clinical use of opioids followed randomized trial evidence, we would expect to see stable to declining rates of use in back and neck pain and headache, with some increasing use in arthritis and joint pain.
Given the different recommendations regarding use of opioids for specific pain conditions and limited efficacy and safety data available to guide clinical decision-making, information on trends in opioid use among subgroups of pain patients is valuable to help direct the focus of future research studies. Prior analyses of trends in use of prescription opioids for non-cancer pain have used national survey data and have not examined whether trends differ by pain condition7, 22. The TROUP (Trends and Risks of Opioid Use for Pain) study was designed to assess trends in and risks of opioid therapy for non-cancer pain (NCP) in contrasting pain populations. In the initial analysis of data from this study, we examined general trends in prescription opioid use in two health insurers, HealthCore commercially insured members plans and Arkansas Medicaid, and found increases in the proportion of enrollees receiving NCP diagnoses, proportion of enrollees with NCP receiving opioids, and the cumulative yearly dose received per patient with NCP in both health insurers, between 2000 and 200530. This present analysis examines trends by type and number of NCP diagnoses, and addresses the following questions: 1) Are increases in use of opioids limited to particular NCP conditions? 2) How do patterns of use differ between the NCP conditions and among those with multiple NCP conditions?
MATERIALS AND METHODS
Study Design
Data were obtained from claims records from January 2000 through December 2005 from two sources: HealthCore (N=3,768,223), the country’s largest private health network, and Arkansas Medicaid (N=127,866). The HealthCore data included plans from five states in the West, Mid West, and South East regions of the United States. The two populations were chosen to allow for private-public payer comparisons, and specifically to describe the range of opioid use in different populations. We anticipated rates of opioid use would differ due to inherent differences in sociodemographic characteristics and disease burden. In addition, the Arkansas Medicaid population is a disadvantaged population situated in the highest opioid use area of the country, and thus makes an ideal population in which to study risks for opioid use and abuse in the treatment of chronic pain.
The study sample consisted of enrollees in the two health insurers during the years from 2000 to 2005. Due to the large number of persons included and retrospective nature of the study, a waiver of the requirements for informed consent was granted from the Human Subject’s Review Committees at the participating institutions. Inclusion criteria included one or more non-cancer pain conditions (NCP) identified by ICD-9-CM codes: back pain, neck pain, arthritis/joint pain, headache/migraine, and HIV/AIDS. These categories are not mutually exclusive, and therefore patients may be counted in more than one category if they receive more than one NCP diagnosis in a given calendar year. HIV/AIDS was included in initial study design because of special concerns about pain management for this condition. Management of this condition, however, targets issues other than pain and has changed significantly over the past ten years with the introduction of highly-active anti-retroviral therapies. Hence, this group is quite different from the other non-cancer pain conditions, and therefore trends will be presented in a separate paper. Total number of types of chronic pain coded within a calendar year was recorded. Individuals with a cancer diagnosis at any time 2000-5 (other than non-melanoma skin cancer), residents of nursing homes, those receiving hospice benefits, and anyone with less than nine months of eligibility in the calendar year were excluded. There were 894,310 enrollees in HealthCore and 43,342 in Arkansas Medicaid in 2005 who met inclusion criteria and were thus classified as having a NCP diagnosis.
Opioids were categorized into three major groups: short-acting DEA Schedule II opioids; long-acting DEA Schedule II opioids; and short-acting DEA Schedule III-IV opioids. Total morphine equivalents for a single prescription were calculated by multiplying the quantity of each prescription by the strength of the prescription (milligrams of opioid per unit dispensed), and multiplying this total by a conversion factor 31. Total morphine equivalents per patient per calendar year (cumulative yearly dose) were calculated by adding the morphine equivalents for each prescription filled during the year. Number of days opioids supplied in the calendar year (as calculated by the dispensing pharmacist) were categorized as 1-30, 31-90, 91-180, and 181+ days. The study was approved by the institutional review board at the University of Washington.
Statistical Analyses
The descriptive statistics (e.g. means, standard deviations, and percentages) of all variables measured were provided separately for each calendar year and both health insurers. The percent change for each variable was computed as the ratio of the change of the means (or percentages) between year 2000 and 2005 over the mean (or percentage) in year 2000. Because all the numbers were rounded to simplify presentation after the calculation was completed, minor rounding errors might be found between the means (or percentages) and percent change, especially for the means (or percentages) with smaller values. Two-sample t tests were used to calculate p values for the change in mean opioid dose and days supply between 2000 and 2005 for each of the pain diagnosis types and number. Odds ratios adjusted for age and gender were calculated using logistic regression to describe the likelihood of receiving >90 days supply of opioids in 2005 in the presence of each NCP diagnosis, relative to those without the NCP diagnosis of interest, or number of pain diagnoses, relative to no NCP diagnosis. Odds ratios were calculated using the total HealthCore and Arkansas Medicaid populations, including those without a NCP diagnosis. The percent with opioid dose greater than 120mg morphine equivalents per day was also calculated for each pain diagnosis type and number. We chose this dose because it is the threshold above which consultation with a pain specialist is recommended in the recent Washington State Opioid Dosing Guidelines38, and is a dose which is unlikely in those with only short-term or intermittent use. All the analyses were performed using SAS 9.1 (SAS Institute Inc., Cary, NC). Additional details of the study design and methods can be found elsewhere30.
RESULTS
Demographic and Clinical Characteristics
Table 1 describes the demographic characteristics and prevalence of pain types and number for HealthCore and Arkansas Medicaid enrollees with non-cancer pain diagnoses in 2000 and 2005. The percent change refers to the change in proportion of NCP enrollees with the specific characteristic. Rates of NCP diagnosis increased in both health insurers. Overall, the percent with one or more of the four NCP diagnoses increased from 17.8% to 23.7% in Healthcore, and from 31.1% to 33.9% in Arkansas Medicaid between 2000 and 2005 (data not shown). Among enrollees with NCP, most (59-70%) had only one NCP diagnosis. However, rates of multiple diagnoses increased in both plans between 2000 and 2005. Arthritis/joint pain was the most common NCP diagnosis in both plans, and was present in over three quarters of enrollees with a NCP diagnosis. In HealthCore, the percent with arthritis/joint pain, back pain, or headache increased, while neck pain decreased slightly between 2000 and 2005. In Arkansas Medicaid, the percent with back pain, neck pain or headache increased while arthritis/joint pain remained relatively stable between 2000 and 2005. The mean (standard deviation) number of pain diagnoses among HealthCore enrollees in 2005 was 1.5 (0.7) for those with arthritis/joint pain, 1.9 (0.8) for those with back pain, 2.3 (0.8) for those with neck pain, and 1.9 (1.0) for those with headaches. The mean number of pain diagnoses among Arkansas Medicaid enrollees in 2005 was 1.6 (0.8) for those with arthritis/joint pain, 2.0 (0.8) for those with back pain, 2.6 (0.8) for those with neck pain, and 2.4 (1.0) for those with headaches (data not shown).
Table 1. Demographic and Clinical Characteristics of HealthCore and Arkansas Medicaid Enrollees with Non-Cancer Pain (NCP) Diagnoses, 2000 and 2005.
| HealthCore | Arkansas Medicaid | ||||||
|---|---|---|---|---|---|---|---|
| Variables | Category | 2000 (N=483,759) | 2005 (N=894,310) | % change 00∼05 | 2000 (N=36,100) | 2005 (N=43,342) | % change 00∼05 |
| Age | Mean(SD) | 45.1 (13.9) | 45.8 (13.9) | 1.5% | 54.9 (20.8) | 50.8 (19.8) | -7.5% |
| Female | N (%) | 277,521 (57.4%) | 513,082 (57.4%) | 0.01% | 27,556 (76.4%) | 32,146 (74.2%) | -2.9% |
| Number of types of pain diagnoses | 1 | 339,600 (70.2%) | 588,825 (65.8%) | -6.21% | 24,588 (68.1%) | 25,870 (59.7%) | -12.4% |
| 2 | 110,603 (22.9%) | 224,404 (25.1%) | 9.75% | 8,879 (24.6%) | 12,435 (28.7%) | 16.7% | |
| 3 | 31,283 (6.5%) | 74,940 (8.4%) | 29.6% | 2,351 (6.5%) | 4,423 (10.2%) | 56.7% | |
| 4 | 2,273 (0.5%) | 6,141 (0.7%) | 46.1% | 282 (0.8%) | 614 (1.4%) | 81.4% | |
| Pain Diagnoses | |||||||
| Arthritis or joint pain | 348,059 (72.0%) | 690,376 (77.2%) | 7.3% | 29,790 (82.5%) | 35,972 (83.0%) | 0.6% | |
| Back pain | 186,921 (38.6%) | 354,979 (39.7%) | 2.7% | 13,479 (37.3%) | 19,328 (44.6%) | 19.4% | |
| Neck pain | 97,442 (20.1%) | 177,038 (19.8%) | -1.7% | 4,722 (13.1%) | 7,162 (16.5%) | 26.3% | |
| Headache | 31,325 (6.5%) | 64,624 (7.2%) | 11.6% | 2,536 (7.0%) | 4,003 (9.2%) | 31.5% | |
Opioid Use
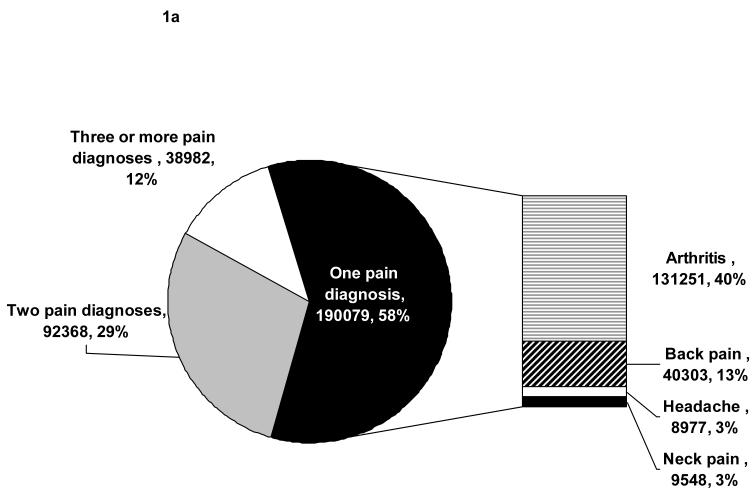
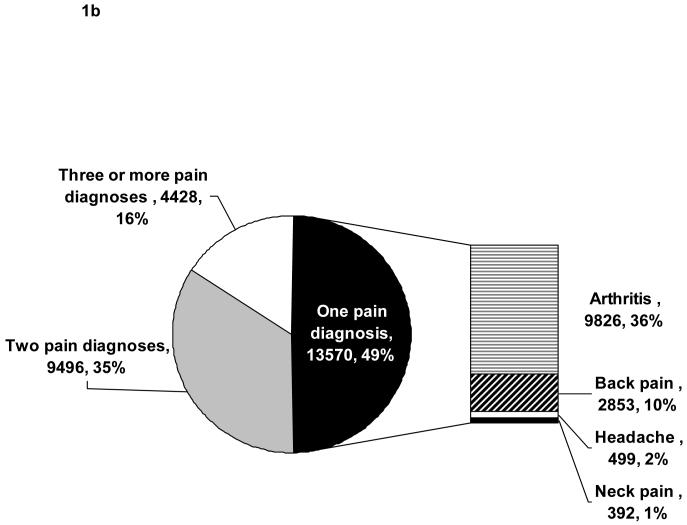
Figures 1a and 1b present the frequencies of specific pain types and number of diagnoses among all those with opioid use and at least one pain diagnosis in 2005. Over half of HealthCore and nearly half of Arkansas Medicaid enrollees on opioids had only one pain diagnosis, most commonly arthritis/joint pain. Among those with multiple pain diagnoses, most had arthritis/joint pain (HealthCore 90.4%, AR Medicaid 93.5%) and/or back pain (HealthCore 81.0%, AR Medicaid 86.3%), and less than half had neck pain (HealthCore 46.1%, AR Medicaid 37.9%) and/or headaches (HealthCore 14.5%, AR Medicaid 18.7%; data not shown). Between 2000 and 2005, there was a decrease in the proportion with only one pain diagnosis from 64% to 59% in HealthCore, and from 57% to 49% in Arkansas Medicaid (data not shown).
Figure 1.
a: Number and Type of Chronic Non-Cancer Pain Diagnoses among HealthCore Enrollees Receiving Opioids in 2005
b: Number and Type of Chronic Non-Cancer Pain Diagnoses among Arkansas Medicaid Enrollees Receiving Opioids in 2005
Table 2 lists the percent of HealthCore and Arkansas Medicaid enrollees with non-cancer pain who had any opioid use, and the percent with greater than a 90-day supply of opioids dispensed in the calendar years 2000 and 2005, by pain type and number of diagnoses.
Table 2. Opioid Use among HealthCore and Arkansas Medicaid Enrollees with Non-Cancer Pain by Pain Diagnosis Number and Type, 2000 and 2005.
| HealthCore N (% of all with pain number or type) | Arkansas Medicaid N (% of all with pain number or type) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pain Diagnosis | Opioid Use | Overall N (2005) | 2000 | 2005 | % change 00∼05 | Overall N (2005) | 2000 | 2005 | % change 00∼05 |
| Arthritis or joint pain | 690,376 | 35,972 | |||||||
| Any Use | 107,760 (31%) | 249949 (36%) | 16.9% | 15752 (53%) | 22849 (64%) | 20.1% | |||
| >90 days | 12737 (4%) | 34597 (5%) | 36.9% | 4665 (16%) | 8708 (24%) | 54.6% | |||
| Back pain | 354,979 | 19,328 | |||||||
| Any Use | 63340 (34%) | 146641 (41%) | 21.9% | 9190 (68%) | 14867 (77%) | 12.8% | |||
| >90 days | 9659 (5%) | 27232 (8%) | 48.5% | 3085 (23%) | 6693 (35%) | 51.3% | |||
| Neck pain | 177,038 | 7,162 | |||||||
| Any Use | 31374 (32%) | 70151 (40%) | 23.1% | 3211 (68%) | 5663 (79%) | 16.3% | |||
| >90 days | 4437 (5%) | 12665 (7%) | 57.1% | 1055 (22%) | 2576 (36%) | 61.0% | |||
| Headache | 64,624 | 4,003 | |||||||
| Any Use | 12382 (40%) | 28051 (43%) | 9.8% | 1805 (71%) | 3098 (77%) | 8.7% | |||
| >90 days | 2569 (8%) | 5790 (9%) | 9.3% | 536 (21%) | 1185 (30%) | 40.1% | |||
| Number of pain diagnoses | |||||||||
| 1 | 339,600 | 25,870 | |||||||
| Any Use | 92960 (27%) | 190536 (32%) | 18.2% | 11056 (45%) | 13627 (53%) | 17.2% | |||
| >90 days* | 7756 (2%) | 17154 (3%) | 27.6% | 2463 (10%) | 3555 (14%) | 37.2% | |||
| 2 | 110,603 | 12,435 | |||||||
| Any Use | 39030 (35%) | 92181 (41%) | 16.4% | 6132 (69%) | 9496 (76%) | 10.6% | |||
| >90 days | 5803 (5%) | 16023 (7%) | 36.1% | 2005 (23%) | 3988 (32%) | 42.0% | |||
| 3 | 31,283 | 4,423 | |||||||
| Any Use | 12924 (41%) | 34954 (47%) | 12.9% | 1886 (80%) | 3854 (87%) | 8.6% | |||
| >90 days | 2700 (9%) | 8492 (11%) | 31.3% | 800 (34%) | 2065 (47%) | 37.2% | |||
| 4 | 2,273 | 614 | |||||||
| Any Use | 1266 (56%) | 3758 (61%) | 9.9% | 245 (87%) | 574 (93%) | 7.6% | |||
| >90 days | 485 (21%) | 1402 (23%) | 7.0% | 117 (41%) | 359 (58%) | 40.9% | |||
The percent of Arkansas Medicaid enrollees by NCP diagnosis type receiving opioids was nearly twice that of HealthCore enrollees for any use, and nearly four times higher for >90 days supply. The percent with any opioid use by pain type ranged from 36% (arthritis/joint pain) to 43% (headache) in HealthCore and from 64% (arthritis/joint pain) to 79% (neck pain) in Arkansas Medicaid in 2005. The percent with any opioid use increased with increasing number of pain diagnoses (one to four), from 32% to 61% in HealthCore and from 53% to 93% in Arkansas Medicaid in 2005. The percent with >90 days supply increased markedly with each additional pain diagnosis, from 3 to 23% in HealthCore, and from 14 to 58% in Arkansas Medicaid.
In general, the percent of enrollees with any opioid use and >90 days supply increased between 2000 and 2005 in both plans for all pain types and regardless of number of pain diagnoses. Increases in opioid use were most marked in those with multiple pain diagnoses and those with >90 days supply. With the exception of arthritis/joint pain, the percent increase in any opioid use between 2000 and 2005 was greater in HealthCore than Arkansas Medicaid enrollees. The percent increase in use with >90 days supply of opioids, however, was greater in Arkansas Medicaid than in HealthCore. In contrast to trends observed for percent with >90 days supply, the percent with opioid dose >120mg morphine equivalents per day ranged from 4-8% and did not vary significantly by pain diagnosis type, number of pain types, health insurer, or year (data not shown).
Table 3 displays odds ratios and 95% confidence intervals, adjusted for age and gender, representing the likelihood of receiving >90 days supply of opioids in 2005 for each of the pain diagnoses and number of pain diagnoses. Odds ratios were statistically significant for each of the pain types except for arthritis or joint pain in HealthCore. In HealthCore, back pain and headache conferred the highest risks of receiving >90 days supply of opioids. In Arkansas Medicaid, back pain and neck pain conferred the highest risks. Having only one pain diagnosis was associated with a decreased likelihood of receiving >90 days supply of opioids in HealthCore, and only mildly increased the odds in AR Medicaid. Odds ratios nearly doubled for each increase in number of pain diagnoses in both insurers.
Table 3.
Age and Gender-Adjusted Odds of Receiving >90 Day Supply of Opioids in 2005 by Pain Type and Number among All HealthCore and Arkansas Medicaid Enrollees
| HealthCore (N=3,768,223) | Arkansas Medicaid (N= 127,866) | |||
|---|---|---|---|---|
| Pain Diagnosis* | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Arthritis or joint pain | 0.99 | 0.97-1.00 | 1.91 | 1.81-2.01 |
| Back pain | 2.33 | 2.29-2.37 | 3.86 | 3.69-4.04 |
| Neck pain | 1.80 | 1.76-1.83 | 2.69 | 2.55-2.84 |
| Headache | 2.45 | 2.38-2.52 | 2.08 | 1.93-2.24 |
| Number of pain diagnoses† | ||||
| 1 | 0.58 | 0.57-0.59 | 1.13 | 1.05-1.21 |
| 2 | 1.47 | 1.44-1.51 | 3.56 | 3.31-3.84 |
| 3 | 2.53 | 2.46-2.60 | 7.21 | 6.61-7.86 |
| 4 | 6.42 | 6.02-6.83 | 12.73 | 10.70-15.14 |
Reference=all enrollees without the pain diagnosis of interest
Reference=no pain diagnosis
Opioid Dose and Days Supply by Pain Type
Table 4 lists the mean days supply and cumulative dose (total, short-acting schedule II, long-acting schedule II and schedule III-IV in mg morphine equivalents) per calendar year among enrollees with non-cancer pain diagnoses and any opioid use in 2000 and 2005 by pain diagnosis type. In general, the mean days supply and cumulative opioid dose was greater in Arkansas Medicaid enrollees compared to HealthCore enrollees, regardless of pain type.
Table 4. Mean Opioid Days Supply and Cumulative Yearly Dose among HealthCore and Arkansas Medicaid Enrollees Receiving Opioids by Non-Cancer Pain Diagnosis Type, 2000 and 2005.
| HealthCore | Arkansas Medicaid | |||||
|---|---|---|---|---|---|---|
| Opioid Use | 2000 (N=146,180) | 2005 (N=321,429) | % change 00∼05 | 2000 (N=19,319) | 2005 (N=27,551) | % change 00∼05 |
| Arthritis or joint pain | ||||||
| Days Supply of Opioids Per Year [mean (SD)] | 44.0 (102.1) | 54.4 (126.7) | 23.6% | 90.9 (130.3) | 122.2 (156.6) | 34.3% |
| Cumulative Yearly Opioid Dose, mg morphine equivalents [mean (SD)] | ||||||
| Total | 2546.1 (12779.2) | 3537.6 (20981.4) | 38.9% | 5,322.3 (13347.1) | 7371.0 (18966.0) | 38.5% |
| Short-acting Schedule II | 1275.0 (9556.5) | 2666.4 (22260.7) | 109.1% | 1510.6 (4361.4) | 4568.6 (11587.4) | 202.4% |
| Long-acting Schedule II | 20272.3 (42718.7) | 28689.2 (53846.7) | 41.5% | 23556.2 (36640.8) | 29761.7 (41665.0) | 26.3% |
| Schedule III-IV | 1555.6 (3839.2) | 1561.1 (3688.2) | 0.4% | 3631.6 (6089.8) | 3847.5 (5776.0) | 5.9% |
| Back pain | ||||||
| Days Supply of Opioids Per Year [mean (SD)] | 55.4 (118.0) | 72.5 (150.6) | 30.8% | 106.6 (147.2) | 145.0 (168.2) | 36.0% |
| Cumulative Yearly Opioid Dose, mg morphine equivalents [mean (SD)] | ||||||
| Total | 3434.5 (17112.6) | 5041.8 (26484.5) | 46.8% | 6458.8 (16860.5) | 8967.5 (20983.9) | 38.8% |
| Short-acting Schedule II | 1807.1 (12350.4) | 3995.4 (28842.3) | 121.1% | 1953.4 (6680.0) | 5538.5 (13030.1) | 183.5% |
| Long-acting Schedule II | 22138.5 (46773.4) | 30794.6 (55408.6) | 39.1% | 26245.7 (39962.7) | 29720.5 (39117.3) | 13.2% |
| Schedule III-IV | 1825.3 (4179.6) | 1888.8 (4105.0) | 3.5% | 3734.0 (5975.9) | 4155.1 (5681.9) | 11.3% |
| Neck pain | ||||||
| Days Supply of Opioids Per Year [mean (SD)] | 52.0 (114.2) | 70.6 (149.9) | 35.8% | 107.8 (153.3) | 151.6 (174.7) | 40.6% |
| Cumulative Yearly Opioid Dose, mg morphine equivalents [mean (SD)] | ||||||
| Total | 3106.3 (14864.7) | 4800.1 (24496.7) | 54.5% | 6386.8 (16141.5) | 9824.1 (22227.7) | 53.8% |
| Short-acting Schedule II | 1632.0 (8625.7) | 3969.8 (25105.6) | 143.3% | 1667.8 (4858.5) | 6410.8 (13426.7) | 284.4% |
| Long-acting Schedule II | 21758.0 (44909.0) | 29274.4 (51534.4) | 34.6% | 25386.9 (35915.5) | 28527.5 (38331.1) | 12.4% |
| Schedule III-IV | 1691.7 (4007.3) | 1833.6 (4038.8) | 8.4% | 3491.0 (5645.9) | 4091.9 (5410.7) | 17.2% |
| Headache | ||||||
| Days Supply of Opioids Per Year [mean (SD)] | 73.4 (141.6) | 78.8 (157.2) | 7.3% | 92.7 (135.4) | 121.6 (156.0) | 31.1% |
| Cumulative Yearly Opioid Dose, mg morphine equivalents [mean (SD)] | ||||||
| Total | 4150.9 (18842.7) | 5016.0 (25305.1) | 20.8% | 5045.8 (13978.9) | 6776.3 (15600.1) | 34.3% |
| Short-acting Schedule II | 2578.4 (19416.6) | 4032.3 (25111.6) | 56.4% | 1377.2 (3423.2) | 4197.3 (10541.1) | 204.8% |
| Long-acting Schedule II | 24513.6 (47615.8) | 30128.6 (56265.0) | 22.9% | 22001.4 (37780.3) | 21399.2 (30506.5) | -2.7% |
| Schedule III-IV | 2220.8 (4667.7) | 2077.8 (4489.9) | -6.4% | 3112.8 (5175.6) | 3722.1 (5594.3) | 19.6% |
Among Arkansas Medicaid enrollees in 2005, mean days supply per calendar year by pain type ranged from 121.6 (headache) to 151.6 (neck pain), and mean cumulative opioid dose ranged from 6776.3 (headache) to 9824.1 (neck pain) mg morphine equivalents (Table 4). Among HealthCore enrollees in 2005, mean days supply by pain type ranged from 54.4 (arthritis/joint pain) to 78.8 (headaches), and mean cumulative opioid dose ranged from 3537.6 (arthritis/joint pain) to 5041.8 (back pain) mg morphine equivalents. The greatest percent increase in mean days supply and total dose between 2000 and 2005 in both plans occurred among those with neck pain.
The mean cumulative yearly dose of short-acting schedule II agents was higher and increased more markedly between 2000 among 2005 for all pain types in Arkansas Medicaid relative to Healthcore. The mean cumulative yearly dose of long-acting schedule II agents also increased between 2000 and 2005, but much less than that of short-acting agents, and the increase was greater for Healthcore enrollees than for Arkansas Medicaid enrollees. While schedule III-IV opioids were the most commonly prescribed opioid type in both health insurers30, the mean cumulative yearly dose remained relatively stable between 2000 and 2005 in HealthCore, and increased only slightly in Arkansas Medicaid, for all pain types. The median values for yearly cumulative dose and days supply were smaller than the means for all pain types and number, and the distributions shifted to the right between 2000 and 2005 (data not shown). All differences between 2000 and 2005 values noted in Table 4 were statistically significant by two-sample t test at p<0.001 except for mean cumulative yearly dose of long-acting schedule II opioids in Arkansas Medicaid for back pain (p=0.028), neck pain (p=0.185), and headache (p=0.854).
Opioid Dose and Days Supply by Number of Pain Diagnoses
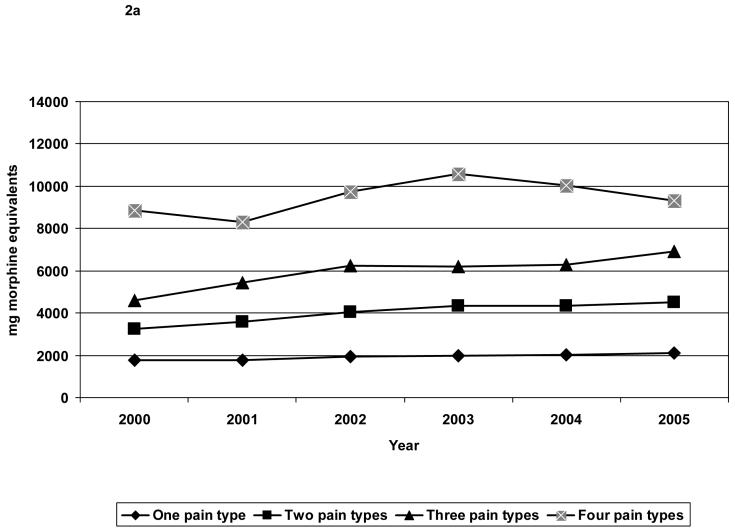
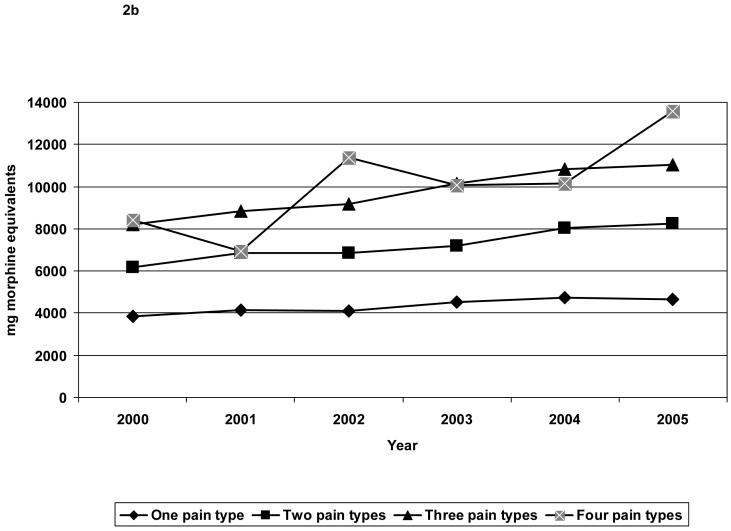
Figures 2a and 2b depict trends in mean cumulative yearly dose of opioids by number of pain diagnoses. In general, the mean days supply (data not shown) and cumulative opioid dose was greater in Arkansas Medicaid enrollees compared to HealthCore enrollees, regardless of number of pain diagnoses.
Figure 2.
a: Trends in Mean Cumulative Yearly Opioid Dose by Number of Pain Types, HealthCore 2000-2005
b: Trends in Mean Cumulative Yearly Opioid Dose by Number of Pain Types, Arkansas Medicaid 2000-2005
Among Arkansas Medicaid enrollees in 2005, mean days supply of opioids per year increased from 83.0 for one pain diagnosis to 211.0 for four pain diagnoses, and the corresponding mean cumulative opioid dose increased from 4,640.4 to 13,578.3 mg morphine equivalents. Among HealthCore enrollees in 2005, mean days supply of opioids per year increased from 36.5 for one pain diagnosis to 142.1 for four pain diagnoses, and the corresponding mean cumulative opioid dose increased from 2,120.1 to 9,305.3 mg morphine equivalents. Mean days supply and cumulative opioid dose increased with increasing number of pain diagnoses in both insurers; however the greatest percent increase was observed between those with one versus two pain diagnoses. The greatest percent increase in mean days supply and cumulative yearly dose between 2000 and 2005 in both insurers occurred among those with three or four pain diagnoses. Similar to trends by pain type, the increase in cumulative yearly dose was most marked for short-acting schedule II agents relative to other opioid types, and among Arkansas Medicaid enrollees. The differences in mean days supply and cumulative yearly dose of opioids between 2000 and 2005 for each number of pain diagnoses were statistically significant by two-sample t test at p<0.001 except for HealthCore enrollees with four pain diagnoses (p=0.211 for change in mean days supply, p=0.613 for change in mean cumulative yearly opioid dose).
In contrast to the trends observed for mean days supply and cumulative opioid dose when examined alone, mean dose per days supply stayed relatively stable for each pain type and number between 2000 and 2005, and ranged from 47.8 to 54.5 (data not shown).
DISCUSSION
Results from this study demonstrate increases in mean cumulative yearly dose and days supply of opioids between 2000 and 2005 for each of the four common non-cancer pain types, and with increasing number of pain diagnoses. Increasing rates of use and days supplied were seen in all the NCP conditions tracked, and there was no evidence of differential rates of increase by pain type. Whereas rates of opioid use did not differ widely between non-cancer pain conditions, long-term opioid use rates doubled with each additional pain diagnosis. Dose increases were most marked for short-acting schedule II agents for all pain types and number. In contrast, mean cumulative yearly opioid dose of schedule III-IV opioids remained relatively stable between 2000 and 2005. This growth in use of the more potent Schedule II opioids, and for longer duration, likely reflects increased attention to the problem of inadequately treated pain in addition to changing clinical attitudes concerning the use of potent opioids for non-cancer pain.
While the majority of the population of NCP patients receiving opioids in both insurers had only one pain diagnosis (most commonly arthritis/joint pain), the percent with multiple pain diagnoses increased between 2000 and 2005. In addition, differences in opioid use varied more by number of pain diagnoses than by pain types. Hence, trends in opioid prescribing by pain type likely reflect the degree of comorbidity (i.e., number of pain diagnoses) within each pain type. The pain type with the lowest mean cumulative opioid dose and days supply (arthritis/joint pain) was also the pain type most likely to occur without additional comorbid pain diagnoses. Similarly, those with neck pain had the highest mean number of pain conditions, and also had the greatest increases in dose and percent with >90 days supply. The highest levels, and greatest percent increases, in mean cumulative opioid dose and days supply occurred for the most part among those with back or neck pain, and with three or four pain diagnoses. Mean opioid dose per day supply and percent with daily dose >120mg morphine equivalents, however, did not change much between 2000 and 2005. Hence, as with the overall trends previously reported30, increases in cumulative yearly dose were driven by an increase in days supply, not the amount prescribed per day. The percent of enrollees with NCP diagnoses and the percent with any opioid use increased between 2000 and 2005, but at a lower rate than the increases observed in long-term opioid use (>90 days supply) and mean days supply during the same years. This suggests that rates of opioid initiation are not increasing as fast as rates of opioid continuation within the group of NCP patients already on opioids.
The trends observed in this study suggest an increased tendency to prescribe long-term opioid therapy, especially to those patients with multiple pain conditions. It is not possible from these analyses to determine the exact reasons for the trends observed, but some speculations can be made based on prior research. The mean cumulative opioid dose and days supplied in both insurers increased with increasing number of pain diagnoses, possibly reflecting greater pain intensity or activity interference. Individuals with multiple pain site may be more likely to have an inadequate response to non-opioid pain treatments36. Multiple pain conditions have also been shown to be more strongly associated with psychopathology than single pain conditions,11 and the presence of a comorbid mental disorder may predict opioid use among individuals with chronic pain.33
The higher rates of opioid use, days supply and dose in the Arkansas Medicaid sample likely reflects the greater disability and disease burden of this population.33, 34 It is also possible that this disadvantaged population has less access to non-opioid rehabilitative therapies (e.g., physical therapy) for NCP compared to privately insured individuals.12 This observed difference between the two insurers appears to be general, and not specific, to certain pain types or number.
The higher rates of opioid use found in this study for enrollees with back pain compared to those with arthritis/joint pain are consistent with data from the population-based Healthcare for Communities Survey.32, 33 Treatment guidelines for low back pain recommend opioid analgesics for those who have severe, disabling pain that is not controlled with acetaminophen and NSAIDs.2, 8 None of the randomized trials evaluating the use of opioids for back pain, however, have examined long-term use.10, 19, 35 Continued pain relief with treatment longer than six months has been reported for some in open label, uncontrolled studies, but dropout rates have been high21, 23. The increases in mean days supply and percent with >90days observed in our study suggest that these opioids are being prescribed on an increasingly long-term basis. While the current research base on use of opioids for NCP is insufficient to recommend one opioid over another,10, 19 the use of longer-acting agents has been recommended for pain that is frequent or constant.4 Our data, however, show only a modest increase over time in mean cumulative yearly of long-acting agents compared to larger increases for short-acting agents.
While those with arthritis/joint pain had a lower absolute mean cumulative yearly opioid dose and days supply, dose and days supply still increased over time. Traditionally, opioids have been recommended as an alternative for osteoarthritis after acetaminophen, and if non-steriodal anti-inflammatory agents (NSAIDs; including COX-2 selective inhibitors) were contraindicated, ineffective or poorly tolerated.27 Acetaminophen and NSAIDs have similarly been recommended as first-line agents for treatment of back pain. Since 2004-2005, however, NSAID recommendations have been shifted towards short-term use due to cardiovascular and gastrointestinal safety concerns, making the use of opioids more accepted in these populations. Nevertheless, we observed increasing trends in opioid use long before this change in guidelines, suggesting there are other factors that account for the increase. The analyses in this study were limited to opioid use trends, and did not include information on other medications used to treat pain and treatment responsiveness. Hence, it is not possible to determine whether opioids were used as an alternative to NSAIDS in accord with guideline recommendations.
The percent of opioid users with headaches in this study was small, consistent with the range of 4-28% reported in prior studies.1, 24 Rates of use increased between 2000 and 2005, although less than for the other pain conditions. The majority of those with headaches and opioid use had multiple pain diagnoses, and thus it is likely that in some cases, opioids were targeted more towards other pain diagnoses. Headache is a very diverse diagnostic category, ranging from mild tension headache, to intermittent but severe migraine attacks, to chronic daily headache. Recommendations regarding the use of opioids for headache are generally limited to treatment of acute migraine attacks that do not respond to first-line agents.20 Daily scheduled opioids may provide some benefit for a small number of those with chronic daily headache,26 however in general, chronic use is controversial due to concerns about the risk of medication overuse headache with overuse of narcotic analgesics.18, 25, 39
There are several limitations to our study. The identification of pain types in our study was based on mention of diagnoses in administrative claims records, and lacks detail on frequency, severity or duration of symptoms. Some of those we identified as having a NCP diagnosis may have had pain that was relatively short-term (e.g., back pain following an acute injury with full recovery) or that is relatively infrequent or managed with prophylactic medication (e.g., migraine headaches). However, given that nearly three fourths of the samples from both insurers had arthritis/joint pain, and most of those with the other pain types had at least one other pain diagnosis, symptoms are likely to be chronic or recurrent for a large percentage of the enrollees identified as having NCP. We did not link the opioid prescriptions more directly to the diagnoses other than determining they were prescribed in the same year. Hence, it is possible some of the opioids were prescribed for conditions other than those examined here. The data presented in this analysis focused on descriptive data of trends over time, and did not include information on other variables that may influence opioid dosing or duration such as medical and psychiatric comorbidities and other concurrent pain treatments. In future TROUP analyses, we plan to examine the relationships between socio-demographic, medical and psychiatric factors and opioid use.
In summary, results from this study demonstrate increases between 2000 and 2005 in NCP diagnosis rates and percent with each diagnosis prescribed acute or chronic opioids. There were also increases observed in mean cumulative dose and day supply of opioids in both a private and publicly insured population, most notable for those with multiple pain diagnoses and/or neck pain. Further research is warranted to determine the long term benefits and risks to patients with multiple pain conditions associated with long-term opioid use.
Acknowledgements
This research was supported by a grant from the National Institute on Drug Abuse DA022560 to Mark D. Sullivan. Dr. Braden is supported by a Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant [T32 MH20021 (Katon)].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
None of the authors have any company holdings that would present a conflict of interest. We are grateful to Gary Moore for building the Arkansas Medicaid analytic dataset.
REFERENCES
- 1.Adams NJ, Plane MB, Fleming MF, Mundt MP, Saunders LA, Stauffacher EA. Opioids and the treatment of chronic pain in a primary care sample. J Pain Symptom Manage. 2001;22:791–796. doi: 10.1016/s0885-3924(01)00320-7. [DOI] [PubMed] [Google Scholar]
- 2.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of nonsteroidal antiinflammatory drugs: an update for clinicians: a scientific statement from the American Heart Association. Circulation. 2007;115:1634–1642. doi: 10.1161/CIRCULATIONAHA.106.181424. [DOI] [PubMed] [Google Scholar]
- 4.Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Med. 2003;349:1943–1953. doi: 10.1056/NEJMra025411. [DOI] [PubMed] [Google Scholar]
- 5.Brixner DI, Oderda GM, Roland CL, Rublee DA. Opioid expenditures and utilization in the Medicaid system. J Pain Palliat Care Pharmacother. 2006;20:5–13. [PubMed] [Google Scholar]
- 6.Buist-Bouwman M, de Graaf R, Vollebergh W. Comorbidity of physical and mental disorders and the effect on work-loss days. Acta Psychiatrica Scandinavica. 2005;111:436–443. doi: 10.1111/j.1600-0447.2005.00513.x. al e. [DOI] [PubMed] [Google Scholar]
- 7.Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs. 2000. Pain. 2004;109:514–519. doi: 10.1016/j.pain.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr., Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 9.Cicero TJ, Inciardi JA, Munoz A. Trends in abuse of Oxycontin and other opioid analgesics in the United States: 2002-2004. J Pain. 2005;6:662–672. doi: 10.1016/j.jpain.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Deshpande A, Furlan A, Mailis-Gagnon A, Atlas S, Turk D. Opioids for chronic low-back pain. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD004959.pub3. CD004959. [DOI] [PubMed] [Google Scholar]
- 11.Dworkin SF, Von Korff M, LeResche L. Multiple pains and psychiatric disturbance. An epidemiologic investigation. Arch Gen Psychiatry. 1990;47:239–244. doi: 10.1001/archpsyc.1990.01810150039007. [DOI] [PubMed] [Google Scholar]
- 12.Freburger JK, Holmes GM, Carey TS. Physician referrals to physical therapy for the treatment of musculoskeletal conditions. Arch Phys Med Rehabil. 2003;84:1839–1849. doi: 10.1016/s0003-9993(03)00375-7. [DOI] [PubMed] [Google Scholar]
- 13.Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. Cmaj. 2006;174:1589–1594. doi: 10.1503/cmaj.051528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization Study in Primary Care. JAMA. 1998;280:147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 15.Hariharan J, Lamb GC, Neuner JM. Long-term opioid contract use for chronic pain management in primary care practice. A five year experience. J Gen Intern Med. 2007;22:485–490. doi: 10.1007/s11606-006-0084-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Latham J, Davis B. The socioeconomic impact of chronic pain. Disability and Rehabilitation. 1994;16:39–44. doi: 10.3109/09638289409166435. [DOI] [PubMed] [Google Scholar]
- 17.Lipton RB, Bigal ME. Opioid therapy and headache: a cause and a cure. Neurology. 2004;62:1662–1663. doi: 10.1212/wnl.62.10.1662. [DOI] [PubMed] [Google Scholar]
- 18.Markley HG. Chronic headache: appropriate use of opiate analgesics. Neurology. 1994;44:S18–24. [PubMed] [Google Scholar]
- 19.Martell BA, O’Connor PG, Kerns RD, Becker WC, Morales KH, Kosten TR, Fiellin DA. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 20.Matchar DB, Young WB, Rosenberg JH, Piertrzak MP, Silberstein SD, Lipton RB, Ramadan NM. Evidence-based guidelines for migraine headache in the primary care setting: pharmacological management of acute attacks. American Academy of Neurology. 2000:1–58. [Google Scholar]
- 21.Noble M, Tregear SJ, Treadwell JR, Schoelles K. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35:214–228. doi: 10.1016/j.jpainsymman.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 22.Olsen Y, Daumit GL, Ford DE. Opioid prescriptions by U.S. primary care physicians from 1992 to 2001. J Pain. 2006;7:225–235. doi: 10.1016/j.jpain.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Portenoy RK, Farrar JT, Backonja MM, Cleeland CS, Yang K, Friedman M, Colucci SV, Richards P. Long-term use of controlled-release oxycodone for noncancer pain: results of a 3-year registry study. Clin J Pain. 2007;23:287–299. doi: 10.1097/AJP.0b013e31802b582f. [DOI] [PubMed] [Google Scholar]
- 24.Reid MC, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O’Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. J Gen Intern Med. 2002;17:173–179. doi: 10.1046/j.1525-1497.2002.10435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saper JR, Dodick D, Gladstone JP. Management of chronic daily headache: challenges in clinical practice. Headache. 2005;45(Suppl 1):S74–85. doi: 10.1111/j.1526-4610.2005.4501004.x. [DOI] [PubMed] [Google Scholar]
- 26.Saper JR, Lake AE, 3rd, Hamel RL, Lutz TE, Branca B, Sims DB, Kroll MM. Daily scheduled opioids for intractable head pain: long-term observations of a treatment program. Neurology. 2004;62:1687–1694. doi: 10.1212/01.wnl.0000125189.17830.02. [DOI] [PubMed] [Google Scholar]
- 27.Schnitzer TJ. Update on guidelines for the treatment of chronic musculoskeletal pain. Clin Rheumatol. 2006;25(Suppl 1):S22–29. doi: 10.1007/s10067-006-0203-8. [DOI] [PubMed] [Google Scholar]
- 28.Sees KL, Di Marino ME, Ruediger NK, Sweeney CT, Shiffman S. Non-medical use of OxyContin Tablets in the United States. J Pain Palliat Care Pharmacother. 2005;19:13–23. [PubMed] [Google Scholar]
- 29.Stang PE, Brandenburg NA, Lane MC, Merikangas KR, Von Korff MR, Kessler RC. Mental and physical comorbid conditions and days in role among persons with arthritis. Psychosom Med. 2006;68:152–158. doi: 10.1097/01.psy.0000195821.25811.b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan MD, Edlund MJ, Fan MY, DeVries A, Braden JB, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000-2005 in Medicaid and Blue Cross-Blue Shield insurance plans: the TROUP study. Pain. 2008 doi: 10.1016/j.pain.2008.04.027. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan MD, Edlund MJ, Fan MY, DeVries A, Braden JB, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000-2005 in Medicaid and Blue Cross-Blue Shield insurance plans: the TROUP study. Pain. 2008 doi: 10.1016/j.pain.2008.04.027. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan MD, Edlund MJ, Steffick D, Unutzer J. Regular use of prescribed opioids: association with common psychiatric disorders. Pain. 2005;119:95–103. doi: 10.1016/j.pain.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 33.Sullivan MD, Edlund MJ, Zhang L, Unutzer J, Wells KB. Association between mental health disorders, problem drug use, and regular prescription opioid use. Arch Intern Med. 2006;166:2087–2093. doi: 10.1001/archinte.166.19.2087. [DOI] [PubMed] [Google Scholar]
- 34.Sullivan MD, LaCroix AZ, Russo JE, Walker EA. Depression and self-reported physical health in patients with coronary disease: mediating and moderating factors. Psychosom Med. 2001;63:248–256. doi: 10.1097/00006842-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Trescot AM, Boswell MV, Atluri SL, Hansen HC, Deer TR, Abdi S, Jasper JF, Singh V, Jordan AE, Johnson BW, Cicala RS, Dunbar EE, Helm S, 2nd, Varley KG, Suchdev PK, Swicegood JR, Calodney AK, Ogoke BA, Minore WS, Manchikanti L. Opioid guidelines in the management of chronic non-cancer pain. Pain Physician. 2006;9:1–39. [PubMed] [Google Scholar]
- 36.Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007;127:276–286. doi: 10.1016/j.pain.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 37.Von Korff M, Crane P, Lane M, Miglioretti DL, Simon G, Saunders K, Stang P, Brandenburg N, Kessler R. Chronic spinal pain and physical-mental comorbidity in the United States: results from the national comorbidity survey replication. Pain. 2005;113:331–339. doi: 10.1016/j.pain.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 38.Washington State Agency Medical Directors’ Group [Accessed February 1, 2008];Interagency guideline on opioid dosing for chronic non-cancer pain: an educational pilot to improve care and safety with opioid treatment. 2007 Available at: http://www.agencymeddirectors.wa.gov/opioiddosing.asp.
- 39.Zwart JA, Dyb G, Hagen K, Svebak S, Holmen J. Analgesic use: a predictor of chronic pain and medication overuse headache: the Head-HUNT Study. Neurology. 2003;61:160–164. doi: 10.1212/01.wnl.0000069924.69078.8d. [DOI] [PubMed] [Google Scholar]