Abstract
INTRODUCTION:
There are currently few studies describing the use of high-fidelity (hi-fi) simulation in teaching neonatal resuscitation. Traditionally, residents are certified in the neonatal resuscitation program (NRP) after successful completion of a multiple-choice written examination and demonstration of skills during a hands-on ‘mega-code’. In the present study, the use of a hi-fi simulation mannequin was compared with a standard plastic mannequin when teaching the megacode portion of the NRP.
METHODS:
In the present pilot study, 15 first-year residents were randomly assigned to demonstrate neonatal resuscitation knowledge, with either the hi-fi mannequin (SimBaby, Laerdal Medical Corporation, USA) or a traditional plastic mannequin (ALS Baby, Laerdal Medical Corporation, USA). A written evaluation was conducted before and after the intervention. Each pair of residents experienced the two scenarios. Video performance was then assessed and compared.
RESULTS:
Residents randomly assigned to the hi-fi mannequin rated the experience higher (31±3.3 versus 27±3.5; P=0.026), and required less redirection from instructors during the megacode (scenario 1: 4.5±1.7 versus 15±6.9; P=0.015 and scenario 2: 1.8±1.3 versus 9.3±2.5; P=0.0009) than those who were randomly assigned to the plastic mannequin. Residents randomly assigned to the hi-fi mannequin did not have improved written scores or improved intubation times.
CONCLUSIONS:
The present pilot study demonstrated that a hi-fi mannequin can be used as part of an educational program, such as the NRP. The use of this technology in neonatal resuscitation training is well-received by learners and may provide a more realistic model for training. Further work is required to clarify its role in task performance and team training.
Keywords: High-fidelity simulation, Neonate, Resuscitation
Abstract
INTRODUCTION :
Peu d’études décrivent l’utilisation de la simulation haute fidélité dans l’enseignement de la réanimation néonatale. D’ordinaire, les résidents reçoivent l’agrément du Programme de réanimation néonatale (PRN) après avoir réussi un examen à choix multiples et démontré leurs compétences dans le cadre d’un « mégacode » pratique. Les auteurs ont comparé l’utilisation d’un mannequin de simulation haute fidélité à un mannequin de plastique ordinaire pendant l’enseignement du mégacode du PRN.
MÉTHODOLOGIE :
Dans le cadre de la présente étude pilote, 15 résidents de première année ont été répartis de manière aléatoire entre un mannequin haute fidélité (SimBaby, Laerdal Medical Corporation, États-Unis) et un mannequin de plastique ordinaire (ALS Baby, Laerdal Medical Corporation, États-Unis) pour démontrer leurs connaissances en réanimation néonatale. Les résidents ont subi une évaluation écrite avant et après l’intervention. Chaque paire de résidents a vécu les deux scénarios. Les auteurs ont ensuite évalué et comparé l’exécution par vidéo.
RÉSULTATS :
Les résidents attribués de manière aléatoire au mannequin haute fidélité ont mieux évalué leur expérience (31±3,3 par rapport à 27±3,5; P=0,026) et ont demandé moins de réorientations aux évaluateurs pendant le mégacode (scénario 1 : 4,5±1,7 par rapport à 15±6,9; P=0,015, et scénario 2 : 1,8±1,3 par rapport à 9,3±2,5; P=0,0009) que ceux qui étaient attribués de manière aléatoire au mannequin de plastique. Les résidents attribués de manière aléatoire au mannequin haute fidélité n’obtenaient pas de meilleurs résultats écrits et n’effectuaient pas l’intubation plus rapidement.
CONCLUSIONS :
Le présent projet pilote démontre que le mannequin haute fidélité peut être utilisé dans le cadre d’un programme de formation comme le PRN. Le recours à cette technologie pendant la formation en réanimation néonatale est appréciée par les stagiaires et peut fournir un modèle de formation plus réaliste. Il faudra poursuivre les travaux pour clarifier le rôle de ce mannequin dans l’exécution des tâches et la formation en équipe.
Although neonatal intensive care curriculums require teaching newborn resuscitation, the efficacy of current program may be suboptimal (1,2). The neonatal resuscitation program (NRP) is widely used in Canada and the United States to provide learners with the basic steps in neonatal resuscitation; it has recently been updated (3).
The skill set taught by the NRP often forms the basis of acute care training for paediatric residents and staff paediatricians working in hospitals with neonates. Additionally, the NRP is mandated for staff working on maternity floors. Assessment of the NRP has been infrequent, although there are reports that approximately 30% of the NRP steps are not performed or are performed incorrectly (4). Furthermore, it has been reported that residents are successful less than 50% of the time when attempting intubation, despite recent certification in the NRP (1,2,5). Several studies (6,7) have demonstrated that residents have relatively few opportunities to lead resuscitations, even by the end of their training. This precludes the consolidation of learned skill sets and the development of competence through experience.
These reports are disconcerting and may be due to a number of factors, including methods used in teaching the neonatal resuscitation skill set. Different approaches to teaching neonatal resuscitation may facilitate learning, and may hopefully lead to improved patient outcomes.
The use of simulation-based training in neonatal resuscitation has been described previously and has recently been reviewed (8,9). It has been generally well-received by health care members who are experienced in neonatal resuscitation (8), and is recommended by many national and international organizations including the International Liaison Committee on Resuscitation (9–11). To the authors’ knowledge, there have been no previous reports in neonatal resuscitation directly comparing the use of a high-fidelity (hi-fi) simulator with a traditional mannequin.
Although simulation-based training is becoming increasingly popular, its effectiveness compared with traditional forms of teaching has been infrequently studied (12). The purpose of the present pilot study was to determine whether medical simulation using a hi-fi infant mannequin improves the educational experience and/or performance of learners during the NRP training.
METHODS
All first-year family medicine residents at St Michael’s Hospital (Toronto, Ontario) were invited to participate in the present pilot study as part of their NRP training. In Canada, the NRP is traditionally taught by having trainees review material by the American Academy of Pediatrics, write a multiple-choice examination and then manage one or more megacode scenarios using low-fidelity plastic mannequins. Approval from St Michael’s Hospital research ethics board was obtained for the present study, and written consent was received for each resident before the training session.
In the present pilot study, 15 first-year family medicine residents were available to participate. All were instructed to review the NRP manual and CD-ROM before the day of instruction, and all received the same 1 h didactic training session at the start of the day. This is the standard didactic training that accompanies the NRP manual. None of the participants had previously taken the NRP or the paediatric advanced life support course. The NRP written evaluation was conducted before and after the megacode. All the residents were taught how to operate the resuscitation equipment, how to provide assisted bag-and-mask ventilation and how to intubate. They were given 30 min of practice time with the traditional mannequin before the megacode scenarios.
The residents were randomly assigned to work with either the hi-fi mannequin (SimBaby, Laerdal Medical Corporation, USA) or the standard plastic mannequin (ALS Baby, Laerdal Medical Corporation, USA) using a computer-generated randomization program. The hi-fi mannequin was a sophisticated interactive patient model which could breathe, cry and mimic seizure activity. Vital signs, cardiac and respiratory status, pulse oximeter readings and cyanosis could be adjusted in real time via a remote laptop computer in response to learner actions, and were displayed for learners on a standard neonatal monitor with appropriate alarms. Visual cues from the hi-fi mannequin included perioral cyanosis, absence of chest and abdominal wall movement, seizure activity and feedback from the monitors (ie, apnea, bradycardia, low O2 saturation and blood pres-sure [BP]). Auditory cues included high and low alarm settings for O2 saturation and the cardiorespiratory and BP monitors, as well as the baby’s cry.
Residents were paired within each track (hi-fi and standard) for two different megacode scenarios. Each student took a turn leading one resuscitation and then assisting with the second. The two megacode scenarios were identical for the hi-fi and low-fidelity mannequin, each providing preparatory time for set up, as if in a resuscitation room. In St Michael’s Hospital, use of both O2 saturation and cardio-respiratory and BP monitoring are available for known, high-risk situations and are considered standards of care. Oximeter probes are increasingly being used in all neonatal resuscitation scenarios, in accordance with recent American Heart Association and International Liaison Committee on Resuscitation guidelines, which recommend avoiding hyperoxemia in the immediate newborn period (3,13).
Students were instructed to manage each case to the best of their ability. If students were unable to proceed, they were redirected by the instructors. Redirection did not include tips on how to manage the clinical scenarios. Both scenarios were adapted from the NRP textbook in use at that time (14) and were modified by the authors (DMC, TB and MF) who were experienced in neonatal resuscitation. These scenarios were presented according to a script lasting approximately 10 min. Students were given an introductory stem and then 30 s to prepare the equipment. The first megacode involved resuscitation of a full-term infant with meconium aspiration, and the second scenario involved a full-term infant with respiratory depression born to a mother with a history of chronic narcotic ingestion. Both scenarios described apneic newborns with persistent cyanosis and bradycardia requiring the learners to intubate, provide chest compressions and administer epinephrine via the endotracheal tube or a simulated intravenous line. Learners were not expected to demonstrate umbilical venous catheter insertion.
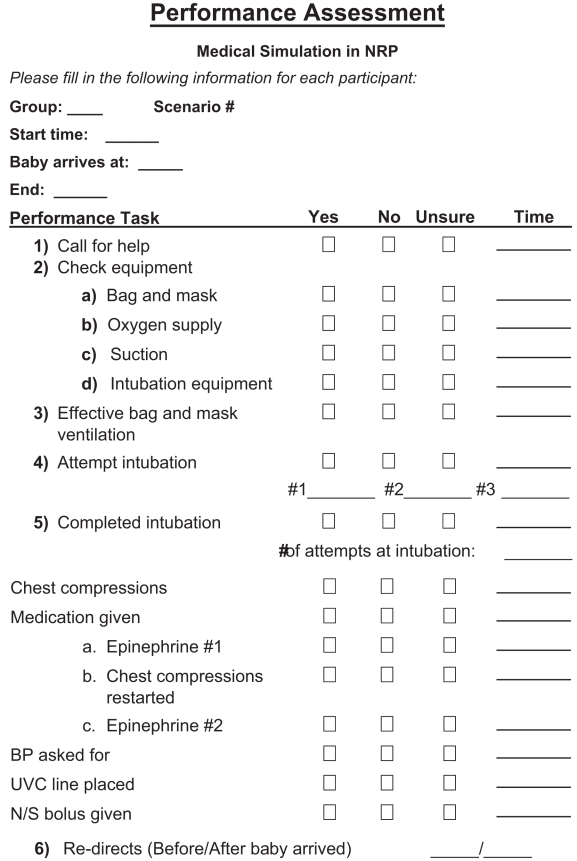
Videos of the megacodes were digitally recorded onto DVDs. Performance was assessed using a predeveloped checklist that was circulated among the authors and another paediatrician, who was experienced in neonatal resuscitation, for content validity (Appendix 1). The standardized checklist consisted of management items that were scored as yes, no, or unsure, and if yes, the time at which it occurred was recorded. A recently validated performance checklist was not available at the time of the present study (15). Video performance was then reviewed by the authors (DMC and TB). Time to complete each performance task was calculated on review of the video using running digital time. The arrival time of the mannequin onto the warmer was used as 0 s. The start of intubation was recorded and taken as proxy for the time at which the intubation was performed (Appendix 1).
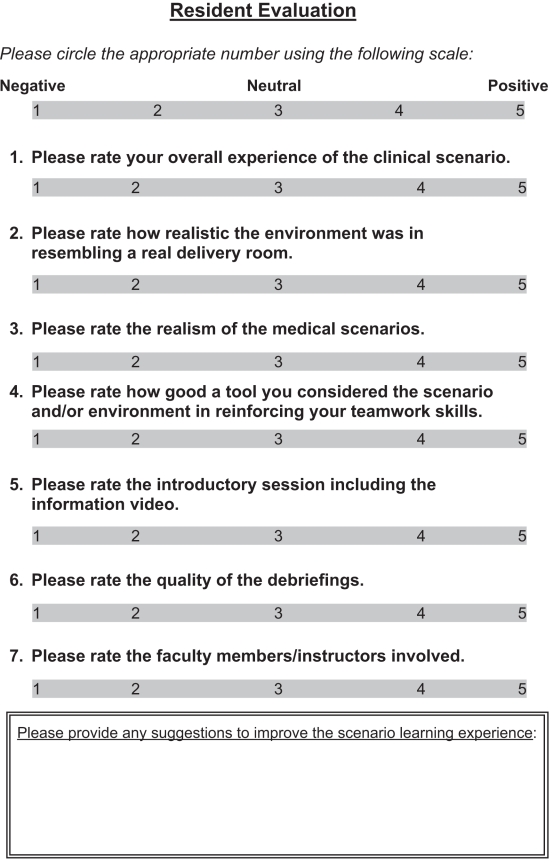
Residents were asked to complete evaluation forms using a previously developed questionnaire assessing resident satisfaction (Appendix 2) (16). The evaluation form consisted of four questions evaluating the simulated scenario, and three questions evaluating other aspects of the educational experience. Each question was scored by the resident using a Likert scale response of 1 to 5. Satisfaction scores from each resident were totalled; means and SDs were computed and compared using the Student’s t test.
The time at which performance items were initiated was recorded for each scenario. Means and SDs were calculated for the trainees in both groups. Means were compared using the Student’s t test. P<0.05 was considered significant. Changes in the written evaluation test scores were also compared between each group. The number of times the scenario required redirection from the instructor was recorded and used as a surrogate for realism.
RESULTS
Eight residents were randomly assigned to resuscitation scenarios using the hi-fi mannequin. Seven residents were allocated to resuscitation scenarios using the standard plastic mannequin. The seventh resident in this group was paired with a paediatric resident at a similar level of training, who assisted with the resuscitation only.
Residents in the hi-fi group rated the experience higher than those randomly assigned to the standard teaching (overall 31±3.3 versus 27±3.5; P=0.026, megacode experience only) (Table 1). There were no differences observed in responses to the questions pertaining to the introduction session, debriefing and instructors (Appendix 2, questions 5 to 7). Differences in pre- and postwritten evaluation scores tended to be higher in the hi-fi group but were not significantly different (hi-fi versus standard +5.1±5.3 versus +2±2.7; P=0.26) (Table 1).
Table 1.
Resident rating of educational experience
| Hi-fi(n=8) | Standard (n=7) | P | |
|---|---|---|---|
| Overall rating (×/35) | 31±3.3 | 27±3.5 | 0.026 |
| Megacode rating (×/20) | 18±2.2 | 15±2.7 | 0.023 |
| Change in test scores | +5.1±5.3 | +2.0±2.7 | 0.26 |
High-fidelity (hi-fi) represents those residents assigned to the hi-fi simulation mannequin, while standard represents those randomly assigned to the standard mannequin. All values are expressed as means ± SDs, unless otherwise stated
Residents in the hi-fi group required less redirection from instructors during the megacode (scenario 1: 4.5±1.7 versus 15±6.9; P=0.015 and scenario 2: 1.8±1.3 versus 9.3±2.5; P=0.0009) (Table 2).
Table 2.
Resident performance
| Hi-fi(n=8) | Standard (n=7) | P | |
|---|---|---|---|
| Time to intubation (s) | |||
| Scenario 1 | 268±108 | 297±60 | 0.32 |
| Scenario 2 | 179±34 | 198±95 | 0.36 |
| Number of redirects | |||
| Scenario 1 | 4.5±1.7 | 15±6.9 | 0.015 |
| Scenario 2 | 1.8±1.3 | 9.3±2.5 | 0.0009 |
High-fidelity (hi-fi) represents those residents assigned to the hi-fi simulation mannequin, while standard represents those randomly assigned to the standard mannequin. All values are expressed as means ± SDs, unless otherwise stated
Performance task times were similar between groups and seemed to improve after the first scenario (Table 2). Residents in the hi-fi group tended to intubate sooner compared with those using the standard mannequin (scenario 1: 268±108 s versus 297±60 s; P=0.32, and scenario 2: 179±34 s versus 198±95 s; P=0.36), but this did not reach statistical difference (Table 2). There was no difference in the time it took for residents to intubate, nor was there any difference in the time it took for the other tasks to be completed (time to bag-and-mask ventilation, time to chest compressions and time to administration of epinephrine).
DISCUSSION
To our knowledge, this is the first report of the use of hi-fi simulation as an educational tool in teaching the NRP. Hi-fi simulation has already been demonstrated to increase individual learner skills, such as intubation of the adult patient, and to improve aspects of team performance in adult medicine (16–21). However, there is currently a paucity of research involving paediatric hi-fi simulation, with most reports (20–22) being descriptive in nature. Simulation has been objectively studied previously in neonatal resuscitation (8), but to date there has not been a comparison of hi-fi simulation with standard teaching tools.
Our pilot study demonstrated the usefulness of hi-fi interactive medical simulation technology in teaching neonatal resuscitation. As demonstrated in a previous study (8) using a computerized simulator, the hi-fi mannequin was well-received by learners. In addition, our hi-fi simulation provided a more realistic model for training students, engaging the trainees more than a standard mannequin. The significant differences in the number of redirects required by learners (posthoc analysis α=0.05, power of 90% power) suggests that the computerized auditory and visual cues provided by the hi-fi mannequin improved learner-response time and seemed to promote independent decision-making during both megacode scenarios.
Although there was a trend toward quicker task performance for learners using hi-fi simulation, and a suggestion of improved NRP written evaluation scores, these differences were not statistically significant. This may have been due to the overall design of the study and the small number of participants.
There are several limitations to our pilot study. The hi-fi infant simulator was used in our study because it was readily available. It differs from a true hi-fi neonatal simulator in terms of size and access to the umbilicus for control placement. We believed that this did not interfere with our study because residents were instructed that these were 4 kg term babies, and during the megacodes, umbilical access was not required. Second, the number of residents in each group was small and randomization may not have been adequate to demonstrate a difference. A post hoc power analysis using these values (assuming an error of 0.05 and power of 80%) would require more than 100 residents to demonstrate significant differences. Furthermore, the performance checklist has not been previously validated, although it is similar in content to a recently validated tool (15). Finally, when analyzing learner performance, the assessor was not blinded to the intervention. It would have also been preferable to have an independent observer who was skilled in resuscitation to review the video footage. Future studies investigating hi-fi simulation in neonatal resuscitation should include a larger number of trainees, the recently published validated tool and a hi-fi neonatal mannequin.
We also acknowledge that feasibility issues such as set-up costs, capital equipment, human resources requirements, and time and organizational constraints were neither explored nor compared with traditional teaching methods in the present study. In larger academic centres, in which resources are more likely to be available and ‘simulation programs’ are already in place (or being developed), these factors are less likely to be limitations. However, this may not be transferable to smaller nonacademic centres, where the NRP is often taught. Further evaluation of these types of barriers would need to be included to determine generalizability.
Hi-fi simulation also needs to be studied in terms of improving team performance. Improved communication and training of staff have been recently identified as key strategies in reducing perinatal and infant mortality (10). Traditional teaching methods in neonatal resuscitation (ie, low-fidelity mannequins or mannequins that have a defined clinical response to a given treatment plan) may not adequately provide health care workers with that training. Reproducing resuscitation scenarios that are complex, infrequent or emotionally charged are important and can be accomplished using this training tool. The use of hi-fi simulation in improving team performance in neonatal resuscitation was not assessed in the present study, but is of ongoing interest to us and several other investigators (10,16,23). Focusing on collaboration and improving team skills during newborn resuscitation should improve patient care (23–25).
CONCLUSION
The present pilot study demonstrates that a hi-fi mannequin can be used as part of an educational program, such as the NRP. The use of this technology in neonatal resuscitation training is well-received by learners and may provide a more realistic model for training. Further work is required to clarify its role in task performance and team training.
APPENDIX 1
APPENDIX 2
REFERENCES
- 1.Falck AJ, Escobedo MB, Baillargeon JG, Villard LG, Gunkel JH. Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics. 2003;112:1242–7. doi: 10.1542/peds.112.6.1242. [DOI] [PubMed] [Google Scholar]
- 2.Leone TA, Rich W, Finer NN. Neonatal intubation: Success of pediatric trainees. J Pediatr. 2005;146:638–41. doi: 10.1016/j.jpeds.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 3.Kattwinkel J. Textbook of Neonatal Resuscitation. 5th edn. Chicago: The American Academy of Pediatrics and the American Heart Association; 2006. [Google Scholar]
- 4.Thomas EJ, Sexton JB, Lasky RE, Helmreich RL, Crandell DS, Tyson J. Teamwork and quality during neonatal care in the delivery room. J Perinatol. 2006;6:163–9. doi: 10.1038/sj.jp.7211451. [DOI] [PubMed] [Google Scholar]
- 5.Walton DM, Edwards MC. Nationwide survey of pediatric residency training in newborn medicine: Preparation for primary care practice. Pediatrics. 2002;110:1081–7. doi: 10.1542/peds.110.6.1081. [DOI] [PubMed] [Google Scholar]
- 6.White JR, Shugerman R, Brownlee C, Quan Lu. Performance of advanced resuscitation skills by pediatric housestaff. Arch Pediatr Adolesc Med. 1998;152:1232–5. doi: 10.1001/archpedi.152.12.1232. [DOI] [PubMed] [Google Scholar]
- 7.Nadel FM, Lavelle JM, Fein JA, Giardino AP, Decker JM, Durbin DR. Assessing pediatric senior residents’ training in resuscitation: Fund of knowledge, technical skills, and perception of confidence. Pediatr Emerg Care. 2000;16:73–6. doi: 10.1097/00006565-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Halamek LP, Kaegi DM, Gaba DM, et al. Time for a new paradigm in pediatric medical education: Teaching neonatal resuscitation in a simulated delivery room environment. Pediatrics. 2000;106:e45–53. doi: 10.1542/peds.106.4.e45. < http://pediatrics.aappublications.org/cgi/reprint/106/4/e45> (Version current at October 7, 2008). [DOI] [PubMed]
- 9.Murphy AA, Halamek LP. Simulation-based training in neonatal resuscitation. Neoreviews. 2005;6:489–92. [Google Scholar]
- 10.Joint Commission on Accreditation of Healthcare Organizations Sentinel event alert. < http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_30.htm> (Version current at October 7, 2008).
- 11.Chamberlain DA, Hazinski MF. Education in resuscitation. Resuscitation. 2003;59:11–43. doi: 10.1016/j.resuscitation.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 12.Issenberg SB, McGaghie WC, Petrusa ER, Lee GD, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med Teach. 2005;27:10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 13.ECC Committee, Subcommittees and Task Forces of the American Heart Association 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 14.Kattwinkel J. Textbook of Neonatal Resuscitation. 4th edn. Chicago: The American Academy of Pediatrics and the American Heart Association; 2000. [Google Scholar]
- 15.Lockyer J, Singhal N, Fidler H, Weiner G, Aziz K, Curran V. The development and testing of a performance checklist to assess neonatal resuscitation megacode skill. Pediatrics. 2006;118:e1739–44. doi: 10.1542/peds.2006-0537. < http://pediatrics.aappublications.org/cgi/content/full/118/6/e1739> (Version current at October 7, 2008). [DOI] [PubMed]
- 16.Shapiro MJ, Morey JC, Small SD, et al. Simulation based teamwork training for emergency department staff: Does it improve clinical team performance when added to an existing didactic teamwork curriculum? Qual Saf Health Care. 2004;13:417–21. doi: 10.1136/qshc.2003.005447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steadman RH, Coates WC, Huang YM, et al. Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Crit Care Med. 2006;34:151–7. doi: 10.1097/01.ccm.0000190619.42013.94. [DOI] [PubMed] [Google Scholar]
- 18.Weller JM, Bloch M, Young S, et al. Evaluation of high fidelity patient simulator in assessment of performance of anaesthetists. Br J Anaesth. 2003;90:43–7. [PubMed] [Google Scholar]
- 19.Barsuk D, Ziv A, Lin G, et al. Using advanced simulation for recognition and correction of gaps in airway and breathing management skills in prehospital trauma care. Anesth Analg. 2005;100:803–9. doi: 10.1213/01.ANE.0000143390.11746.CF. [DOI] [PubMed] [Google Scholar]
- 20.Weinstock PH, Kappus LJ, Kleinman ME, Grenier B, Hickey P, Burns JP. Toward a new paradigm in hospital-based pediatric education: The development of an on-site simulator program. Pediatr Crit Care Med. 2005;6:635–41. doi: 10.1097/01.pcc.0000185489.07469.af. [DOI] [PubMed] [Google Scholar]
- 21.Fiedor ML. Pediatric simulation: A valuable tool for pediatric medical education. Crit Care Med. 2004;32:S72–4. doi: 10.1097/01.ccm.0000110732.68981.52. [DOI] [PubMed] [Google Scholar]
- 22.Cheng A, Duff J, Grant E, Kissoon N, Grant VJ. Simulation in paediatrics: An educational revolution. Paediatr Child Health. 2007;12:465–8. doi: 10.1093/pch/12.6.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas EJ, Taggart B, Crandell S, et al. Teaching teamwork during the Neonatal Resuscitation Program: A randomized trial. J Perinatol. 2007;27:409–14. doi: 10.1038/sj.jp.7211771. [DOI] [PubMed] [Google Scholar]
- 24.Zabari M, Suresh G, Tomlinson M, et al. Implementation and case-study results of potentially better practices for collaboration between obstetrics and neonatology to achieve improved perinatal outcomes. Pediatrics. 2006;118(Suppl 2):S153–8. doi: 10.1542/peds.2006-0913M. [DOI] [PubMed] [Google Scholar]
- 25.Ohlinger J, Kantak A, Lavin JP, et al. Evaluation and development of potentially better practices for perinatal and neonatal communication and collaboration. Pediatrics. 2006;118(Suppl 2):S147–52. doi: 10.1542/peds.2006-0913L. [DOI] [PubMed] [Google Scholar]