Abstract
Background & Objectives
Nicotine dependence (ND) is a pervasive public health concern and a leading cause of preventable mortality. Stressful life events (SLEs), which severely disrupt the lives of individuals experiencing such events, have been posited as correlates of persisting ND. While both ND and SLEs have been studied extensively in relation to other variables, there are few instances in which they have been investigated in concert.
Methods
In this study, we use data on 18,013 smokers from the 2001-2002 data set of the National Epidemiological Survey of Alcohol and Related Conditions (NESARC, N=43,093) to examine whether experiencing a SLE in the past 12 months was associated with meeting criteria for ND in the same past 12 months. Logistic regression analyses were conducted while accounting for a variety of covariates.
Results
A majority of the SLEs were associated with past 12 month ND, even after controlling for poverty, psychiatric and substance use disorders and a prior history of ND (odds-ratios 1.35-2.20). The rates of past 12 month ND were considerably greater in those experiencing more than one SLE.
Conclusions
While these data do not allow us to make causal interpretations, our results suggest an association between SLE and ND. Potentially, individuals experiencing SLEs may find it difficult to quit smoking; alternatively, directly or via correlated risks (e.g. living in a high risk neighborhood), smoking may increase the likelihood of exposure to SLEs.
1. INTRODUCTION
1.1 Nicotine Dependence (ND) as a risk factor for persistent smoking
Persistent cigarette smoking is the single most prevalent preventable cause of premature death in the United States (1) and the majority of other countries. Smoking has been linked to an ever increasing slew of health risks and illnesses including heart disease, respiratory disease, cancer, and stroke (2-3). Smoking cessation alleviates the risk of these and other smoking related health problems (2), however, one of the leading barriers to effective smoking cessation is ND. Difficulty quitting despite repeated attempts is a criterion of DSM-based ND (4). Furthermore, individuals who meet criteria for DSM-IV ND are 2.2 times less likely to remain smoke-free (5).
1.2 Stress and nicotine dependence
Stress has frequently been reported as a correlate of smoking persistence and relapse (6-11). A review investigating the effect of work environment on a variety of smoking-related variables found that several work stressors such as workload, role ambiguity, high responsibility for the work of others, and long hours predicted relapse from smoking cessation (12). An Australian study that investigated financial stress and its relationship with smoking cessation and relapse concluded that those in higher socioeconomic brackets were more likely to quit smoking and far less likely to relapse than those experiencing financial stress such as being unable to pay bills on time (13). A similar study found that current smokers (71%) were more likely to experience financial stress than ex-smokers (49.6%) (14).
1.3 Goals
Using data on 18,013 U.S. adults who had reported a lifetime history of smoking a 100 or more cigarettes in the first wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (2001-2002) we examined the association between self-reported experiences of 14 SLE and DSM-IV ND, both in the past 12 months.
2.0 METHODS
2.1 The NESARC sample
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (15), the first wave of which was collected between 2001 and 2002, is a representative sample of United States non-institutionalized inhabitants. Data collection and protocol were supervised by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). The study includes data on a total of 43, 093 individuals (43% males), 18 and older (median age 46 years, range 18-99 years), interviewed using face-to-face computerized personal interviews. Data on tobacco use, nicotine dependence, stress life events, alcohol use, illicit drug use and substance use disorders and psychopathology, as well as a host of other factors, were collected using the AUDADIS-IV (16). The NESARC overall survey response rate at wave 1 was 81% (15). Details regarding the NESARC and the AUDADIS are available in related publications (17).
2.2 Measures
Our primary hypothesis was to examine the association between past 12 month SLE and DSM-IV ND (4).
2.2.1 Nicotine Dependence (ND)
We defined ND based on DSM-IV criteria. An individual met criteria for DSM-IV ND if they endorsed 3 or more DSM-IV criteria which clustered in the past 12 months;
2.2.2 Stressful Life Events (SLE)
The 12 SLEs (18) listed in the NESARC assessed a variety of occupational, familial, financial, and legal issues. Participants were asked if they had experienced each event in the past 12 months. They included items assessing death or illness/injury of family, friends or a loved one, moving or having someone move in, being fired or laid off, unemployment while looking for a job for over a month, trouble with a boss or coworker, change in job/responsibilities/work hours, separation/divorce/serious breakup, problems with a neighbor/friend/relative, financial crisis and the participant or their relative being in trouble with the law. In addition to these, we incorporated two additional items (from Section 1 of the Background Information), that queried the participants about the number of times, in the past 12 months, that they had been hospitalized or personally been the victim of a crime - these items were coded dichotomously.
2.2.3 Covariates
In addition to sex (males=1), age (defined as a dummy variable reflecting being 40 years or younger) and self-reported Caucasian ethnicity, we adjusted for socio-economic status and for several substance-related and psychiatric correlates.
Living below the poverty line, was defined based on the thresholds established by the U.S. Census Bureau in 2002.
In addition to meeting criteria for DSM-IV ND prior to the past 12 months, we also controlled for a host of psychiatric correlates, including a lifetime history of DSM-IV conduct disorder, major depressive disorder, panic disorder, social phobia, specific phobia, and generalized anxiety disorder as well as a lifetime history of DSM-IV alcohol abuse/dependence.
2.3 Statistical Analysis
Analyses were restricted to those 18,013 individuals who reported a lifetime history of smoking 100 or more cigarettes. This allowed us to control for the potential confound of earlier stages of smoking behavior. Univariate and multivariate logistic regression estimating the association between smoking cessation and each stressful life event was conducted using survey logistic regression (19) to produce adjusted and unadjusted odds ratios. A multinomial logistic regression was used examine the association between the number of SLEs experienced (0,1,2,3,4 or more) and ND. Weights and other sampling design effects (sampling units and strata) were incorporated into the model.
3.0 RESULTS
3.1 Sample Characteristics
Of the 43,093 participants, 18,013 (50.4% men, 80.2% Caucasian, 35.1% aged 40 or younger and 15.2% living below the poverty line) reported having smoked 100 or more cigarettes. Of these smokers, 26.7% (N=4,811) met criteria for DSM-IV ND in the past 12 months - 91.4% of these past 12 month nicotine dependent individuals also reported a prior history of ND. The rates of psychiatric diagnoses and alcohol dependence in this sample of nicotine dependent individuals was somewhat higher than those reported in the full sample (conduct disorder: 6.9%; major depressive disorder: 22.5%; social phobia: 5.7%, panic disorder: 7.6%; specific phobias: 11.4%; generalized anxiety disorder: 5.8%; alcohol abuse/dependence: 42.1%).
3.2 SLEs
The prevalence of each of the 14 SLE in smokers is presented in Table 1. The most commonly reported life event in the past 12 months was illness/injury to a friend or family member (38.5%) while the least commonly reported life event was being the victim of a crime (4.8%).
Table 1.
Prevalence of stressful life events experienced in the past 12 months and their association (odds-ratios, O.R.) with past 12 month DSM-IV nicotine dependence in 18,013 individuals who reported smoking 100+ cigarettes during their lifetime
| In those who smoked 100+ cigarettes (%) (N=18,013) | In those with past 12 months DSM-IV nicotine dependence (%) (N=4692) | Univariate O.R. [95% C.I.] | Multivariate O.R. [95% C.I.]* | |
|---|---|---|---|---|
| Stressful Life Event | ||||
| Personally been hospitalized | 12.76 | 12.44 | 0.96 [0.85 - 1.08] |
1.03 [ 0.84 - 1.27] |
| Personally the victim of crime | 4.84 | 7.46 | 1.95 [1.62 - 2.33] |
1.27 [0.88 - 1.32] |
| Death of family member/friend | 35.02 | 36.45 | 1.09 [1.01 - 1.19] |
1.11 [0.98 - 1.25] |
| Illness/injury of friend/family | 38.49 | 43.32 | 1.32 [1.23 - 1.43] |
1.02 [0.90 - 1.15] |
| Move or new boarder | 16.02 | 24.9 | 2.35 [2.11 - 2.63] |
1.48 [1.24 - 1.78] |
| Fired or laid off | 12.12 | 7.4 | 2.39 [2.06 - 2.78] |
1.86 [1.47 - 2.36] |
| Unemployed and looking for a job > month | 10.26 | 17.2 | 2.46 [2.18 - 2.79] |
1.95 [1.57 - 2.43] |
| Trouble with boss/coworker | 9.21 | 15.89 | 2.51 [2.20 - 2.89] |
1.20 [0.96 - 1.52] |
| Change jobs, job responsibilities, or work hours | 22.52 | 35.43 | 2.48 [2.24 - 2.74] |
1.35 [1.16 - 1.57] |
| Separated/divorced or break off steady relationship | 7.72 | 13.91 | 2.97 [2.56 - 3.44] |
2.20 [1.72 - 2.81] |
| Serious problems with a neighbor, friend, or relative | 7.22 | 12.36 | 2.75 [2.35 - 3.21] |
1.44 [1.16 - 1.77] |
| Financial crisis, bankruptcy, unable to pay bills on time | 15.05 | 27.3 | 3.30 [2.95 - 3.69] |
1.72 [1.45 - 2.05] |
| Family member trouble with police, get arrested, or jailed | 7.32 | 12.41 | 2.50 [2.317- 2.87] |
1.57 [1.28 - 1.91] |
| You or family victim of crime | 7.73 | 11.87 | 1.98 [1.75 - 2.26] |
1.08 [0.88 - 1.33] |
Covariates: DSM-IV Nicotine Dependence prior to past 12 months, Sex, Age, Race, Poverty, Major Depression, Panic Disorder, Social Phobia, Specific Phobia, General Anxiety Disorder, Alcohol Dependence; those in bold were significant (p < 0.05)
3.3 Univariate association between SLEs and ND
A sizable portion of the 14 SLEs considered for this study correlated with a significantly increased likelihood of ND in the past 12 months. As shown in Table 1, with the exception of hospitalization, experiencing a stressful life event was associated with DSM-IV ND [Odds-ratios ranging from 1.09-3.30].
3.4 Multivariate association between SLEs and ND
Even after controlling for the effect of covariates, moving or having someone move in with the individual, unemployment and job searching for over a month, a change of jobs, job responsibilities, or work hours, separation, divorce, or break up from a steady relationship, financial crisis, bankruptcy, or insolvency and imprisonment/ trouble with the law of a family member were associated with an increased likelihood of meeting criteria for DSM-IV ND in those past 12 months. In addition to SLEs, a prior (prior to past 12 months) history of DSM-IV ND (O.R. 65.1) and a lifetime history of panic disorder (O.R. 1.27) was also associated with ND in the past 12 months.
3.5 Interactions between SLEs and sex, age and race
With rare exception, after accounting for the main effects of each SLE and sex, age and race, interactions between SLE and these covariates were not significantly associated with ND. The only significant interactions associated with ND were between moving/new boarder and age (O.R.: 0.81 [0.68 - 0.95]), trouble with the law and sex (O.R.: 1.29 [1.02 - 1.62]) as well as age (O.R.: 0.69 [0.54 - 0.86]), and between financial crisis and race (O.R.: 1.43 [1.17 - 1.73]). This implies that the association between moving/new boarder or experiencing trouble with the law and ND are stronger in older individuals, and for the latter SLE, in men, while the association between ND and experiencing a financial crisis was stronger in Caucasians.
3.6 Number of SLEs and ND
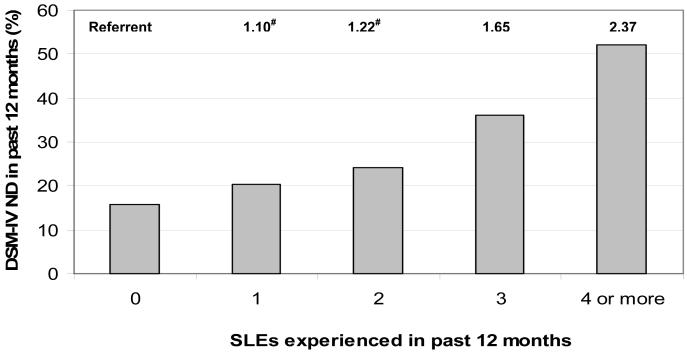
Figure 1 shows the prevalence of ND according to the number of SLEs experienced in the past 12 months. Multinomial logistic regressions revealed that individuals who experiencing 3 or more SLEs were significantly more likely to also report ND in the past 12 months, when compared with those who had experienced 1 or 2 SLEs (Figure 1).
Figure 1.
Prevalence of, and relative risk ratios (RRR, shown along the top of the panel, above the bars) between past 12 months DSM-IV nicotine dependence (ND) by number of stressful life events (SLEs) experienced during the same period in 18,013 individuals who reported smoking 100 or more cigarettes during their lifetime.
Legend: RRR are adjusted for covariates: DSM-IV Nicotine Dependence prior to past 12 months, Sex, Age, Race, Poverty, Major Depression, Panic Disorder, Social Phobia, Specific Phobia, General Anxiety Disorder, Alcohol Dependence; #RRR are statistically equal
4.0 DISCUSSION
4.1 Main finding
Using data on 18,013 smokers, our study found that even after controlling for a prior history of DSM-IV ND and for the effects of psychiatric diagnoses and alcohol abuse/dependence, SLEs were associated with DSM-IV ND in the same past 12 months.
4.2 SLEs and smoking
Our results are congruent with those from other studies. For instance, Wewers (20) found that nicotine abstinent subjects reported fewer work-related stressful events than relapsed subjects. Furthermore, work-related stress was influential in the formation of smoking behavior during the postcessational period (21). Another study investigating sex differences and the effects of SLEs in relation to smoking status similarly found that SLE related to health and finances had the greatest effect on smoking status, particularly in reference to women (22).
4.3 Possible hypotheses
As we do not have information on the timing of the SLE relative to ND, we cannot ascribe a causal relationship between SLE and ND (23). Therefore, while it is likely that experiencing an SLE increases risk for continued or new onsets of ND, it is also plausible that prior ND contributes to SLEs or that a third unmeasured factor jointly influences risk for experience SLEs and sustained ND.
4.3.1. SLEs increase risk for ND
While theories surrounding mechanisms of self-medication are complex, some studies have posited that individuals experiencing SLEs may self-medicate with nicotine (24-26). Particularly in women, smoking may be used to cope with negative affect (7, 27-28)., although we did not observe significant gender differences in our study A potential mechanism to consider here is that alteration of the hypothalamic-pituatary-adrenal (HPA) axis in habitual smokers may mediate the link between stress-responsivity and inability to quit smoking (see reviews 29 & 30 for details on this and other potential mechanisms). In our study, participants were not asked whether the life event was subjectively stressful to them or not, hence we cannot be certain that the relationship observed in our analysis represents stress responsivity.
4.3.2 ND increases risk of exposure to SLEs
While there is relatively less known about the effects of ND on SLEs, Koenen et al (31) have reported that a history of ND increased the odds (1.2) of trauma exposure and of Post Traumatic Stress Disorder (PTSD, O.R. 1.9) in Vietnam Era Male Twins. The HPA-axis which is dysregulated by chronic smoking has been implicated in the relationship between ND and PTSD but mechanisms linking ND to trauma exposure are less well understood (32). Sustained smoking is expensive and may contribute to financial loss - several studies conducted in New York City after the implementation of a steep tax increase found that heavy smokers were resistant to economical sanctions (33-36). In the current climate of increased awareness of the deleterious health effects and the low tolerance for smoking in public places, nicotine dependent individuals may also experiencing stressful interpersonal situations due to pressure from family and friends to quit.
4.3.3. The influence of unmeasured correlates on both SLEs and ND
Dwelling in high risk neighborhoods or delinquent peer affiliations (37-41) may mediate the relationship between SLEs and ND. Individuals who engage in risky behaviors (42), either due to their environment or due to their predisposition to conduct problems, or both, will be more likely to experience SLEs and continue smoking.
4.4 Strengths and limitations
The strengths of our study include the power afforded by a large representative sample and our ability to control for several potential covariates. We were, in our study, also able to control for earlier stages of smoking, such as a lifetime history of smoking 100+ cigarettes as well as for a prior history of ND - the ability to conduct analyses on ‘exposed’ smokers was afforded by the impressive sample size of the NESARC and allowed us to focus on ND without biases of earlier stages of smoking. The limitations of our study include our inability to attribute causality to our results, any biases introduced by retrospective recall and absence of data on environmental measures that may have increased risk for exposure to SLE (neighborhood adversity/peers).
4.5 Conclusion
Irrespective of the mechanism, individuals who experience SLE will also be less likely to successfully remit from ND. In some instances, these individuals may be socioeconomically disadvantaged (43-44) or in high-risk environments and therefore, may not have access to quality care, particularly therapeutic aids that are sensitive to the maladaptive effects of SLEs on smoking and particularly, nicotine dependence. In addition to increasing clinician awareness surrounding the potential role of SLEs in the persistence of smoking, legislation that increases accessibility of care to vulnerable populations is much needed.
Acknowledgements
This research was conducted by Ms. Balk as a Summer with NIDA intern (DA023668S1). We are also supported by DA023668 (AA), DA18267 and DA18660 (MTL).
Footnotes
Declaration of interest: Authors have no conflicts of interest to declare
References
- 1.Centers for Disease Control (CDC) Annual smoking-attributable mortality, years of potential life lost, and economic costs-United States. MMWR. 2002;51:300–303. [PubMed] [Google Scholar]
- 2.Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ. 2000;321:323–329. doi: 10.1136/bmj.321.7257.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smoking and Tobacco Control Program. National Cancer Institute . Monograph 8: Changes in Cigarette-Related Disease Risks and Their Implications for Prevention and Control. Bethesda, MD: 1997. [Google Scholar]
- 4.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th edition edn American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 5.Breslau N, Johnson EO, Hiripi E, Kessler R. Nicotine dependence in the United States: prevalence, trends, and smoking persistence. Arch Gen Psychiatry. 2001;58:810–816. doi: 10.1001/archpsyc.58.9.810. [DOI] [PubMed] [Google Scholar]
- 6.Kalman D. The subjective effects of nicotine: methodological issues, a review of experimental studies, and recommendations for future research. Nicotine Tob Res. 2002;4:25–70. doi: 10.1080/14622200110098437. [DOI] [PubMed] [Google Scholar]
- 7.Perkins KA, Donny E, Caggiula AR. Sex differences in nicotine effects and self-administration: review of human and animal evidence. Nicotine Tob Res. 1999;1:301–315. doi: 10.1080/14622299050011431. [DOI] [PubMed] [Google Scholar]
- 8.Pomerleau OF, Pomerleau CS. Research on stress and smoking: progress and problems. Br J Addict. 1991;86:599–603. doi: 10.1111/j.1360-0443.1991.tb01815.x. [DOI] [PubMed] [Google Scholar]
- 9.Shiffman S, Gnys M, Richards TJ, Paty JA, Hickcox M, Kassel JD. Temptations to smoke after quitting: a comparison of lapsers and maintainers. Health Psychol. 1996a;15:455–461. doi: 10.1037//0278-6133.15.6.455. [DOI] [PubMed] [Google Scholar]
- 10.Shiffman S, Hickcox M, Paty JA, Gnys M, Kassel JD, Richards TJ. Progression from a smoking lapse to relapse: prediction from abstinence violation effects, nicotine dependence, and lapse characteristics. J Consult Clin Psychol. 1996b;64:993–1002. doi: 10.1037//0022-006x.64.5.993. [DOI] [PubMed] [Google Scholar]
- 11.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob.Control. 1998;7:409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albertsen K, Borg V, Oldenburg B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev Med. 2006;43(4):291–305. doi: 10.1016/j.ypmed.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Siahpush M, Carlin JB. Financial stress, smoking cessation and relapse: results from a prospective study of an Australian national sample. Addiction. 2005;101(1):121–27. doi: 10.1111/j.1360-0443.2005.01292.x. [DOI] [PubMed] [Google Scholar]
- 14.Siahpush M, Spittal M, Singh GK. Association of smoking cessation with financial stress and material well-being: results from a prospective study of a population-based national survey. Am J Pub Health. 2007;97(12):2281–2287. doi: 10.2105/AJPH.2006.103580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001-2002 of the National Epidemiologic Survey on Alcohol and Related Conditions. National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003a. [Google Scholar]
- 16.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003b;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 17.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 18.Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol Alcohol. 2005;40:453–460. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- 19.Stata Corporation . STATA Statistical Software: Release 8.2. Stata Corp.; College Station, TX: 2005. [Google Scholar]
- 20.Wewers ME. The role of postcessation factors in tobacco abstinence: stressful events and coping responses. Addict Behav. 1998;13(3):297–302. doi: 10.1016/0306-4603(88)90057-3. [DOI] [PubMed] [Google Scholar]
- 21.Falba T, Teng HM, Sindelar JL, Gallo WT. The effect of involuntary job loss on smoking intensity and relapse. Addiction. 2005;100:1330–1339. doi: 10.1111/j.1360-0443.2005.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKee SA, Maciejewski PK, Falba T, Mazure CM. Sex differences in the effects of stressful life events on changes in smoking status. Addiction. 2003;98:847–855. doi: 10.1046/j.1360-0443.2003.00408.x. [DOI] [PubMed] [Google Scholar]
- 23.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 24.Abrams DB, Monti PM, Pinto RP, Elder JP, Brown RA, Jacobus SI. Psychosocial stress and coping in smokers who relapse or quit. Health Psychol. 1987;6:289–303. doi: 10.1037//0278-6133.6.4.289. [DOI] [PubMed] [Google Scholar]
- 25.Johnson EO, Breslau N. Is the association of smoking and depression a recent phenomenon? Nicotine Tob Res. 2006;8:257–262. doi: 10.1080/14622200600576644. [DOI] [PubMed] [Google Scholar]
- 26.Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am J Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- 27.Perkins KA, Gerlach D, Vender J, Grobe J, Meeker J, Hutchison S. Sex differences in the subjective and reinforcing effects of visual and olfactory cigarette smoke stimuli. Nicotine Tob Res. 2001;l3:141–150. doi: 10.1080/14622200110043059. [DOI] [PubMed] [Google Scholar]
- 28.Perkins KA, Jacobs L, Sanders M, Caggiula AR. Sex differences in the subjective and reinforcing effects of cigarette nicotine dose. Psychopharmacology (Berl) 2002;163:194–201. doi: 10.1007/s00213-002-1168-1. [DOI] [PubMed] [Google Scholar]
- 29.Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164:1149–1159. doi: 10.1176/appi.ajp.2007.05030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kreek MJ, Koob GF. Drug dependence: stress and dysregulation of brain reward pathways. Drug Alcohol Depend. 1998;51:23–47. doi: 10.1016/s0376-8716(98)00064-7. [DOI] [PubMed] [Google Scholar]
- 31.Koenen KC, Hitsman B, Lyons MJ, Niaura R, McCaffery J, Goldberg J, Eisen SA, True W, Tsuang M. A twin registry study of the relationship between posttraumatic stress disorder and nicotine dependence in men. Arch Gen Psychiatry. 2005;62:1258–1265. doi: 10.1001/archpsyc.62.11.1258. [DOI] [PubMed] [Google Scholar]
- 32.al’Absi M. Hypothalamic-pituitary-adrenocortical responses to psychological stress and risk for smoking relapse. Int J Psychophysiol. 2006;59:218–227. doi: 10.1016/j.ijpsycho.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 33.Cantreill J, Hung D, Fahs MC, Shelley D. Purchasing patterns and smoking behaviors after a large tobacco tax increase: a study of Chinese Americans living in New York City. Public Health Rep. 2008;123:135–146. doi: 10.1177/003335490812300206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002-2003. Am J Public Health. 2005;95:1016–1023. doi: 10.2105/AJPH.2004.058164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mostashari F, Kerker BD, Hajat A, Miller N, Frieden TR. Smoking practices in New York City: the use of a population-based survey to guide policy-making and programming. J Urban Health. 2005;82:58–70. doi: 10.1093/jurban/jti008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shelley D, Cantrell MJ, Moon-Howard J, Ramjohn DQ, VanDevanter N. The $5 man: the underground economic response to a large cigarette tax increase in New York City. Am J Public Health. 2007;97:1483–1488. doi: 10.2105/AJPH.2005.079921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Conrad KM, Flay BR, Hill D. Why children start smoking cigarettes: predictors of onset. Br J Addict. 1992;87:1711–1724. doi: 10.1111/j.1360-0443.1992.tb02684.x. [DOI] [PubMed] [Google Scholar]
- 38.Jones DN, Schroeder JR, Moolchan ET. Time spent with friends who smoke and quit attempts among teen smokers. Addict Behav. 2004;29:723–729. doi: 10.1016/j.addbeh.2004.02.026. [DOI] [PubMed] [Google Scholar]
- 39.Kobus K. Peers and adolescent smoking. Addiction. 2003;98(Suppl 1):37–55. doi: 10.1046/j.1360-0443.98.s1.4.x. 37-55. [DOI] [PubMed] [Google Scholar]
- 40.Vink JM, Willemsen G, Engels RC, Boomsma DI. Smoking status of parents, siblings and friends: predictors of regular smoking? Findings from a longitudinal twin-family study. Twin Res. 2003;6:209–217. doi: 10.1375/136905203765693861. [DOI] [PubMed] [Google Scholar]
- 41.van KI, van LJ, Droomers M, de HA. Residential environment and health: a review of methodological and conceptual issues. Rev Environ Health. 2004;19:381–401. [PubMed] [Google Scholar]
- 42.Duncan SC, Strycker LA, Duncan TE. Exploring associations in developmental trends of adolescent substance use and risky sexual behavior in a high-risk population. J Behav Med. 1999;22:21–34. doi: 10.1023/a:1018795417956. [DOI] [PubMed] [Google Scholar]
- 43.Flint AJ, Novotny TE. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983-1993: the independent risk of being poor. Tob Control. 1997;6:14–18. doi: 10.1136/tc.6.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Haustein KO. Smoking and poverty. Eur J Cardiovasc.Prev Rehabil. 2006;13:312–318. doi: 10.1097/01.hjr.0000199495.23838.58. [DOI] [PubMed] [Google Scholar]