Abstract
Objectives. We examined the cost-effectiveness of contraceptive methods dispensed in 2003 to 955 000 women in Family PACT (Planning, Access, Care and Treatment), California's publicly funded family planning program.
Methods. We estimated the number of pregnancies averted by each contraceptive method and compared the cost of providing each method with the savings from averted pregnancies.
Results. More than half of the 178 000 averted pregnancies were attributable to oral contraceptives, one fifth to injectable methods, and one tenth each to the patch and barrier methods. The implant and intrauterine contraceptives were the most cost-effective, with cost savings of more than $7.00 for every $1.00 spent in services and supplies. Per $1.00 spent, injectable contraceptives yielded savings of $5.60; oral contraceptives, $4.07; the patch, $2.99; the vaginal ring, $2.55; barrier methods, $1.34; and emergency contraceptives, $1.43.
Conclusions. All contraceptive methods were cost-effective—they saved more in public expenditures for unintended pregnancies than they cost to provide. Because no single method is clinically recommended to every woman, it is medically and fiscally advisable for public health programs to offer all contraceptive methods.
Unintended pregnancies occur increasingly and disproportionately to women with limited resources.1 Cost–benefit analyses have repeatedly shown substantial savings to the public in pregnancy-related medical expenses from the provision of contraceptive services to low-income women.2–4 However, these analyses have not been conducted for specific types of contraceptive methods, with the exception of a 1995 study by Trussell et al. comparing the costs of using 15 different methods of contraception, including the costs of providing the method and the costs of unintended pregnancies.5 Trussell et al. showed the theoretical cost-effectiveness of 5 years' use of contraceptive methods, not taking into account the costs of providing other method-related services or the likelihood of method discontinuation. Although Trussell et al. show that all methods can be cost-effective, it is not known what the relative cost-effectiveness of specific methods is when cost data are derived from an actual public health program and the tendency of a significant proportion of women to switch and discontinue methods is taken into account.
California's family planning program, Family PACT (Planning, Access, Care and Treatment), provides contraception and reproductive health services to women and men of reproductive age whose incomes do not exceed 200% of the federal poverty level and who have no other reproductive health care coverage. More than 2000 private and nonprofit providers across the state deliver family planning services and are reimbursed by the Family PACT program on a fee-for-service basis.6 The program was launched in 1997 and grew rapidly, serving 750 000 clients during its first full year of operation and more than 1.6 million per year in recent years.7 The size of the program and the detailed data kept by the program on contraceptive methods dispensed permit an analysis of the cost-effectiveness of specific methods of contraception.
Family PACT covers all contraceptive methods approved by the Food and Drug Administration at no cost to the client. Methods available since the program's inception include oral contraceptives, injectable contraceptives, intrauterine contraceptives, sterilization, and barrier methods. Dedicated emergency contraceptive pills became available in 1999, and the new contraceptive patch and vaginal ring were added to the formulary in 2002. With the introduction of new contraceptive methods, the pattern of methods dispensed through Family PACT has changed: by 2005, nearly 20% of women served each year received at least 1 pack of emergency contraceptives, 15% received a contraceptive patch, and 2% received a contraceptive ring, whereas the percentage of women receiving oral and injectable contraceptives has slightly declined. The percentage of women receiving barrier methods with or without another contraceptive has remained steady at around 45%.7
Given their limited time on the market and a lack of large-scale data on contraceptive method dispensing, little is known about the women using the new methods and the effect of these methods on unintended pregnancy. There has been some criticism of the high cost of the contraceptive patch and ring.8 However, given the absence of data on use of these methods and the cost of providing them, there has been no way to assess the validity of these criticisms. We assessed the cost-effectiveness of covering new contraceptive methods for women aged 13 to 44 years and evaluated the relative contribution of all methods to the fertility effect of the Family PACT Program. We compared the costs of providing contraceptives through Family PACT with the costs of unintended pregnancies to government programs.
METHODS
We employed the same methodology to estimate pregnancies averted that we used to estimate the fertility effect of the Family PACT Program in fiscal years 1997–1998 and 2002.9,10 For this study, we analyzed the fertility effect of each method of contraception separately. We estimated the number of pregnancies averted through the use of specific contraceptive methods to be the difference between the number of pregnancies expected in the absence of that method and the number expected given the provision of that method through Family PACT.
Contraceptive Coverage
For this study we relied on 3 full calendar years of Family PACT claims data. We used contraceptive method dispensing claims data from 2003. We also examined claims in 2002 to identify methods previously dispensed to clients who received methods in 2003 and claims in 2004 to predict contraceptive continuation, including intrauterine device and implant removals.
We estimated the number of months of contraceptive coverage provided under Family PACT on the basis of paid claims data on the quantity and type of contraceptives dispensed. The coverage for long-term methods (tubal ligations, intrauterine devices, and implants) was calculated as the number of months between the provision date and December 2004, unless the claims data showed an implant or intrauterine device removal before December 2004. We imposed this 2-year cap to avoid predicting pregnancies far into the future.
Because clients may not use all of the contraceptives they receive, we adjusted the number of months of contraceptive coverage for short-term methods, such as condoms and oral contraceptives, to account for method discontinuation. For oral contraceptives, we assumed that a woman who did not return for refills used half of the pills dispensed to her. We assumed that women who received 1 packet of emergency contraceptive pills used it; however, for women who were given more than 1 packet (provision in advance), we assumed that 50% used the second packet. We assumed a month of protection for every 12 condoms dispensed by pharmacies. For condoms and other barrier methods dispensed by clinics, the exact quantity of supplies dispensed was not available, and we assumed, given findings from the Family PACT medical records review, that each dispensing provided 2 months of contraceptive coverage. Each injection was assumed to provide 3 months of contraceptive coverage. In our sensitivity analysis, we examined the effect of adjusting for method discontinuation on our estimates of method-specific pregnancies averted.9
Estimating the Number of Pregnancies Averted
We estimated the probability of pregnancy in the absence of each method of contraception as follows. For each woman who received a new contraceptive method in 2003, we looked at the previously used method and calculated her probability of pregnancy in the absence of the new method. For example, to estimate the fertility rate in the absence of the contraceptive patch, we looked at the last methods dispensed to patch users prior to their 2003 patch visit. For women who had no previous Family PACT visits or who had not received contraceptives from Family PACT in the previous year, we used a programwide fertility rate estimated from clients' self-reports of contraceptive use prior to enrollment. These self-reports were taken from a review of medical records for dates of service in fiscal year 2000–2001 of 868 new Family PACT female clients who were not pregnant and not seeking pregnancy.
To estimate the number of pregnancies among clients, we modeled the month-by-month experience of each woman who received a contraceptive method, beginning with the month when the contraceptive was dispensed and ending with the last month of contraceptive coverage. For each month, we used a Markov model to calculate the probability that the woman would become pregnant on the basis of the failure rate of the method used (i.e., the proportion of users who experience a pregnancy in a year), age-specific fecundity, and the estimated probability of pregnancy in the months before the contraceptive was dispensed. Modeling pregnancies averted by month allowed us to use specific contraceptive dispensing data for months of coverage, rather than assuming a year of coverage for each client. It also allowed for repeat pregnancies within a year, a common outcome among women who use low-efficacy methods and terminate pregnancies by abortion.9
For this analysis, we made the same assumptions about contraceptive failure rates and pregnancy outcomes as in our study of the fertility effect of the entire Family PACT Program.9,10 The monthly probability of pregnancy by method was derived from typical-use annual probability of pregnancy by method from Hatcher et al.11 The contraceptive patch and ring were assumed to have the same probability of failure as oral contraceptives. We assumed that 40% of pregnancies end in induced abortion, 10% end in spontaneous abortion, 1% are ectopic, and the remaining 49% are carried to term.12,13
We expected that in the absence of each method of contraception, some women would use less effective methods and some would use more effective methods. We assumed that a woman who adopted a method of contraception at her first Family PACT visit would in the absence of the Family PACT program, return to using the method she used prior to enrollment. In the absence of individual-level data on methods used prior to enrollment, we used data from women new to Family PACT for whom contraceptive method use prior to enrollment was abstracted as part of a medical record review. Therefore, we anticipated that a method dispensed during a client's first visit would have an associated pregnancy rate in the absence of that method equal to that of the absence of the program.
Costs of Providing Services
To calculate the costs of providing contraceptive services by method, we assigned a primary method to each client, on the basis of what was dispensed at each visit, and all subsequent expenses for that client were attributed to that method until she was given a different method. In assigning the primary method, for clients who were dispensed more than 1 method, we used the following rank-ordered list: tubal ligation, intrauterine contraceptive, implant, injectable, vaginal ring, patch, oral contraceptives, barrier method, emergency contraceptive pill. A client who received an implant and a ring was assigned the implant as her primary method, because implant comes before ring in the list. In addition to the cost of the contraceptive supplies themselves, the costs of all subsequent clinician visits, laboratory work, and pharmacy claims, including services related to pregnancy testing or sexually transmitted infections, for a client were attributed to her primary method. For clinician visits, laboratory work, or pharmacy visits that did not involve the dispensing of contraceptives, costs were assigned to the primary method of the client's last clinician visit.
In 2003, Family PACT spent $385 million on female clients. Of that amount, $47 million (12%) was spent on clients who were not given a contraceptive method by the program in 2003, $28 million was spent on clients before their first dispensing visit of 2003, and $8 million was spent on clients outside the age range of our study. The remaining $302 million we attributed to particular primary methods of contraception for the purposes of our study.
Costs of Unintended Pregnancies
As part of a separate cost–benefit study,2 we estimated the cost to the public of an unintended pregnancy for 2 years after the birth. In 2002, each pregnancy averted by contraception provided by Family PACT that would have ended in abortion saved the public sector $372. Each birth averted would have cost the public $3228 from the time of conception to the time of delivery and $11 545 in medical, welfare, and other social service costs for a woman and child from the time of conception until 2 years after the birth.2 We adjusted the costs for pregnancies leading to birth to factor in the estimated 38% of adolescent pregnancies and 50% of adult pregnancies that were merely delayed, rather than prevented, by contraceptive use and that would still result in costs to the public when they occurred at a later date.2
Sensitivity Analyses
Our model of the cost savings from preventing unintended pregnancies with specific methods of contraception made some assumptions that might have affected the relative cost-effectiveness we found for particular methods. We conducted 3 sensitivity analyses to investigate the results' dependence on the probability estimates chosen. First, in our base model we adjusted the months of protection from short-term methods of contraception to account for method discontinuation. As a sensitivity analysis, we present our findings without this adjustment, assuming that clients used all the supplies they were given. Second, our use of estimated method-specific pregnancy rates in the absence of each method of contraception, which took into account the previous methods used, made some methods appear to be relatively more effective at reducing pregnancies, particularly those adopted by women who, in the absence of Family PACT, would use no method. In our second sensitivity analysis, all methods had the same probability of pregnancy in the absence of their use. Third, we examined the short-term financial returns of contraceptive provision, examining the medical savings only from the time of conception to the time of delivery or termination.
RESULTS
Contraceptives Dispensed to Women in 2003
Nearly 1 million female clients—217 000 aged 13 to 19 years and 738 000 aged 20 to 44 years—received contraceptive methods through Family PACT in 2003. Payments were made for oral contraceptives for about 449 000 clients, condoms and other barrier methods as a primary method for 405 000 clients, injectables for 162 000 clients, and long-term methods for 22 000 clients. Emergency contraceptives were dispensed without any other method to 37 000 clients. About 129 000 women received the new contraceptive patch, and 11 000 received the vaginal contraceptive ring.
The claims paid for women during 2003 provided each client with an average of 6.6 months of primary-method contraceptive coverage. Oral contraceptives accounted for half (50%) of the woman-months of protection dispensed, followed by injectables (17%), barrier methods (14%), and the patch (11%). Users of long-term methods (tubal ligation, intrauterine devices, and implants) received the greatest number of months of protection. Among reversible, short-term methods of contraception, oral contraceptives provided the greatest number of months of protection (7.1 months), followed by injectables (6.4 months) and the patch (5.5 months). Barrier methods provided 2.2 months of protection and emergency contraceptives used as the primary method provided 1.3 months, although clients who used these methods may have received other primary methods over the course of the year (Table 1).
TABLE 1.
Primary Contraceptive Methods Provided to Female Family PACT Clients and Estimated Pregnancy Rates in the Absence of the Method: California, 2003
| Clients Aged 13–19 y |
Clients Aged 20–44 y |
All Clients |
|||||||
| Contraceptive Method | No.a | Average Months of Protection per Client | Estimated Pregnancy Rate in Absence of Method, % | No.a | Average Months of Protection per Client | Estimated Pregnancy Rate in Absence of Method, % | No.a | Average Months of Protection per Client | Percentage of Total Months of Primary Contraceptive Protection Attributable to Method |
| Interval tubal ligationb | 0 | NA | NA | 4 006 | 18.3 | 38 | 4 006 | 18.3 | 1 |
| Implantb | 17 | 17.4 | 40 | 88 | 18 | 39 | 105 | 17.9 | 0 |
| Intrauterine deviceb | 1 077 | 16 | 39 | 16 674 | 16.2 | 39 | 17 751 | 16.1 | 5 |
| Injectable | 34 885 | 5.8 | 40 | 127 833 | 6.6 | 41 | 162 718 | 6.4 | 17 |
| Ring | 2 751 | 4.1 | 38 | 8 366 | 4.3 | 39 | 11 117 | 4.2 | 1 |
| Patch | 29 380 | 4.7 | 38 | 99 643 | 5.7 | 38 | 129 023 | 5.5 | 11 |
| Oral contraceptives | 100 990 | 6.9 | 41 | 348 392 | 7.1 | 41 | 449 382 | 7.1 | 50 |
| Barrier methods | 93 473 | 2.2 | 40 | 312 336 | 2.2 | 40 | 405 809 | 2.2 | 14 |
| Emergency contraceptives | 14 885 | 1.3 | 39 | 22 726 | 1.3 | 39 | 37 611 | 1.3 | 1 |
| All | 217 263 | 6 | 42 | 738 331 | 6.8 | 43 | 955 594 | 6.6 | 100 |
Note. PACT = Planning, Access, Care, and Treatment.
Numbers in this column add to more than the n for this group because some women made visits for more than 1 primary method over the course of the year.
Assumes a 2-year cap on duration of contraceptive protection.
Pregnancy Rates in the Absence of Family PACT or Specific Methods
Before enrolling in Family PACT, 27% of the women were using no method of contraception and 3% were using natural family planning methods such as periodic abstinence and withdrawal. Nearly 4 in 10 women (38%) were using condoms, and the remaining 32% were using hormonal methods or intrauterine devices. Girls and women aged 13 to 19 years were more likely than were women aged 20 to 44 years to be using condoms and less likely to be using hormonal or intrauterine contraceptives. We estimated that 43% of the women would have become pregnant over the course of a year in the absence of Family PACT. Our estimates of pregnancy rates in the absence of each method of contraception are shown in Table 1.
Pregnancies Averted by Specific Methods of Contraception in 2003
On the basis of the quantity and type of contraceptive methods dispensed, we estimated that because of method failure and noncompliance, Family PACT clients experienced 37 000 pregnancies during the time they were using contraceptives dispensed in 2003. If these women had been using the methods they used before adopting a primary method through Family PACT, or for women with no history of contraceptive use, the same method array as women new to the program, they would have experienced 216 000 pregnancies. The difference, 178 000 pregnancies, is an estimate of the number of pregnancies averted through the provision of specific contraceptive methods by Family PACT in 2003 (Table 2). This estimate is somewhat lower than the estimate of 205 000 pregnancies averted by the program in 200210 because in this analysis some women continue to use subsidized contraceptive services, they just would revert to methods they had previously used in the program.
TABLE 2.
Number of Pregnancies Averted and Cost Savings for Each Contraceptive Method Provided by Family PACT: California, 2003
| Contraceptive Method | Estimated No. of Pregnancies in Absence of Method | Estimated No. of Pregnancies With Method | No. of Pregnancies Averted | Costs Associated With Provision of Method, $ in Thousands | Cost Savings per Dollar Expenditure, $ |
| Interval tubal ligationa | 2 246 | 31 | 2 215 | 2 959 | 4.46 |
| Implanta | 59 | 0 | 59 | 22 | 15.90 |
| Intrauterine devicea | 9 077 | 191 | 8 886 | 7 309 | 7.24 |
| Injectable | 42 036 | 2 656 | 39 380 | 41 873 | 5.60 |
| Ring | 1 640 | 298 | 1 343 | 3 140 | 2.55 |
| Patch | 22 897 | 4 501 | 18 395 | 36 646 | 2.99 |
| Oral contraceptives | 110 515 | 19 978 | 90 537 | 132 674 | 4.07 |
| Barrier methods | 25 332 | 8 757 | 16 575 | 73 879 | 1.34 |
| Emergency contraceptives | 1 837 | 968 | 869 | 3 633 | 1.43 |
| All | 215 641 | 37 380 | 178 261 | 302 133 | 3.52 |
Note. PACT = Planning, Access, Care, and Treatment.
Assumes a 2-year cap on duration of contraceptive protection.
When we estimated pregnancies averted by method, we found that slightly more than half (91 000) of the averted pregnancies were attributable to oral contraceptive use, 22% (39 000) were attributable to injectable contraceptive use, 10% (18 000) were attributable to the contraceptive patch, approximately 10% (17 000) were attributable to use of barrier methods, and 6% (11 000) were attributable to use of long-term methods (Table 2).
Cost Savings per Dollar Spent on Family PACT by Primary Contraceptive Method
All contraceptive methods were cost-effective in that they prevented unintended pregnancies, but the cost savings per dollar spent varied by method (Table 2). The contraceptive implant produced the highest savings; however, the small number of implant users may have skewed these data. The intrauterine device produced the second highest savings per dollar spent, despite the fact that we capped the duration of contraceptive protection it provided at 2 years. Among short-term methods, injectable contraceptives produced the highest savings, at $5.60 saved per $1.00 spent on services, followed by oral contraceptives ($4.07), the patch ($2.99), and the ring ($2.55). Barrier methods ($1.34) and emergency contraceptives ($1.43) produced lower savings per $1.00 spent on services.
Sensitivity of Results to Methodology and Inputs
In our first sensitivity analysis, we examined the number of pregnancies averted estimated without adjustment for discontinuation of barrier methods, the ring, the patch, and oral contraceptives. This adjustment reduced the months of protection provided by these methods and reduced the cost savings associated with their use. We examined whether adjustment for discontinuation of use disproportionately affected one short-term method more than others. As Table 3 shows, the cost savings associated with use of barrier methods is disproportionately reduced by this adjustment. However, even assuming that clients used all the supplies they received does not increase the savings for barrier methods to the level of savings for hormonal methods.
TABLE 3.
Sensitivity Analyses of Method-Specific Savings From Preventing Unintended Pregnancies
| Base Case Cost Savings per Dollar Expenditure, $ | Scenario 1: Women Use All Methods Dispensed |
Scenario 2: Constant Risk of Pregnancy Across Methods in Absence of Program |
Scenario 3: Medical Costs Through End of Pregnancy Only |
||||
| Contraceptive method | Cost Savings per Dollar Expenditure, $ | Percentage Change From Base Case | Cost Savings per Dollar Expenditure, $ | Percentage Change From Base Case | Cost Savings per Dollar Expenditure, $ | Percentage Change From Base Case | |
| Interval tubal ligation | 4.46 | 4.46 | 0 | 5.14 | 15 | 1.35 | −70 |
| Implant | 15.90 | 15.90 | 0 | 17.76 | 12 | 4.80 | −70 |
| Intrauterine device | 7.24 | 7.24 | 0 | 8.12 | 12 | 2.19 | −70 |
| Injectable | 5.60 | 5.60 | 0 | 5.77 | 3 | 1.69 | −70 |
| Ring | 2.55 | 2.68 | 5 | 2.99 | 17 | 0.77 | −70 |
| Patch | 2.99 | 3.13 | 5 | 3.81 | 27 | 0.90 | −70 |
| Oral contraceptives | 4.07 | 4.32 | 6 | 4.65 | 14 | 1.23 | −70 |
| Barrier methods | 1.34 | 1.83 | 37 | 2.32 | 74 | 0.40 | −70 |
| Emergency contraceptives | 1.43 | 1.43 | 0 | 1.87 | 31 | 0.43 | −70 |
| All | 3.52 | 3.77 | 7 | 4.17 | 19 | 1.06 | −70 |
In our second sensitivity analysis, we examined the effect of our method-specific failure rates for the absence of each contraceptive method. We compared the results we obtained by using method-specific failure rates with 1 programwide rate of unintended pregnancy in the absence of the program. The programwide rate of pregnancy was higher because fewer women used contraceptive methods in the absence of the family planning program. If all women adopted the methods that new Family PACT clients used prior to their enrollment, the savings for all contraceptive methods under Family PACT would be almost 19% higher.
In our third sensitivity analysis, by limiting the cost associated with unintended pregnancies to just those medical expenditures that occur up to the time of delivery or termination, we obtained a conservative measure of the short-term returns of providing contraception. Within 9 months of conception, $1.00 spent on contraceptives provided through the program was associated with only $1.06 in savings. Only the ring, the patch, emergency contraceptives, and barrier methods were not associated with positive savings within 9 months of conception.
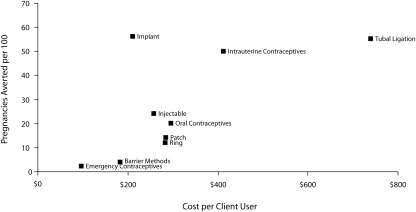
The cost-efficiency curve in Figure 1 shows the investment in contraceptive services per user along the x-axis and the effectiveness in pregnancies averted along the y-axis. At low levels of investment there were slim returns in effectiveness. Very high levels of investment per user yielded diminishing returns. Investments in intrauterine devices and implants yielded the highest returns.
FIGURE 1.
Cost-efficiency of contraceptive methods provided by California's Family PACT (Planning, Access, Care, Treatment) program, 2003.
DISCUSSION
Limitations
We made assumptions that had the effect of reducing the cost savings associated with very-long-term and very-short-term contraceptive methods. The conservative cap of 2 years on the effect of long-term methods resulted in an underestimation of the cost savings from these methods, which women may continue to use for many years. We may also have underestimated the duration of contraceptive coverage for barrier methods if clients' supplies lasted longer than 2 months or overestimated the duration of coverage if they ran out before 2 months.
We did not capture the cost savings associated with postpartum tubal ligations, because Family PACT covers only interval tubal ligations (procedures not done in conjunction with hospitalization for delivery). Postpartum tubal ligations are likely associated with higher cost savings than interval tubal ligations.
Our implant provision costs and use are for Norplant devices that were provided in 2003, when the product was no longer on the market, but doctors were still implanting supplies they had in stock. However, the latest implant device, Implanon, would likely have similar efficacy and continuation in the first 2 years of use. The cost of the Implanon device is about 20% higher than the cost of Norplant, which may translate into slightly lower cost-effectiveness than we estimated for Norplant.
Our study year, 2003, was the first full year in which the contraceptive patch and ring were available through Family PACT. As a result, many users were likely first-time users who may have been given a small supply on a trial basis. With the passage of time, clients may be given a larger quantity of these products, perhaps providing coverage equivalent to oral contraceptives, which would increase the cost savings associated with providing these new methods of contraception.
Conclusions
We found all contraceptive methods dispensed through Family PACT to be cost-effective. Long-term methods are very cost-effective. Barrier methods and emergency contraceptives tend to yield the lowest savings per dollar spent because of their relatively low efficacy and short duration of use. Higher costs and fewer months of contraceptive protection from the contraceptive patch and ring result in lower cost savings than for oral contraceptives; however, these easier-to-use methods offer enhanced convenience for clients. Highly user-dependent methods, such as oral contraceptives and barrier methods, are less effective because they are more likely to be used imperfectly. Missed oral contraceptive pills are quite common and contribute to unintended pregnancy.14–16 Recent research indicates that compliance rates are at least as high for the ring as for oral contraceptives and that patch compliance may be even higher, which may lead to lower failure rates and greater cost savings.17,18 This would be especially true if women who use the patch or the ring receive sufficient quantities to provide coverage equal to that provided by oral contraceptives.
Because all contraceptive methods are cost-effective, public health programs can offer a range of methods to increase the chances that their clients will find a method that suits their needs. Providers should be encouraged to dispense or prescribe more months of contraceptive protection per visit as appropriate, which would reduce the number of clinic visits and costs while increasing method continuation.
Women using family planning services should be given information about the relative effectiveness of different contraceptive methods so that they can make educated decisions. For new users of any contraceptive method, follow-up support should be available to ensure the user's compliance and understanding and to ascertain the method's acceptability. Users of barrier methods and emergency contraceptives should be encouraged to use additional, longer-term methods of contraception. Together, these measures will contribute to higher contraceptive compliance and continuation, lower failure rates, and fewer unintended pregnancies.
Acknowledgments
This research was funded by the State of California Office of Family Planning through a contract to the Bixby Center for Global Reproductive Health, University of California, San Francisco.
Human Participant Protection
This research was approved by the University of California, San Francisco Committee for Human Research (CHR H429-16233).
References
- 1.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health 2006;38:90–96 [DOI] [PubMed] [Google Scholar]
- 2.Amaral G, Foster DG, Biggs A, Jasik C, Judd S, Brindis C. Public savings from the prevention of unintended pregnancy: a cost analysis of family planning services in California. Health Serv Res 2007;42:1960–1980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forrest JD, Samara R. Impact of publicly funded contraceptive services on unintended pregnancies and implications for Medicaid expenditures. Fam Plann Perspect 1996;28:188–195 [PubMed] [Google Scholar]
- 4.Forrest JD, Singh S. The impact of public-sector expenditures for contraceptive services in California. Fam Plann Perspect 1990;22:161–168 [PubMed] [Google Scholar]
- 5.Trussell J, Leveque JA, Koenig JD, et al. The economic value of contraception: a comparison of 15 methods. Am J Public Health 1995;85:494–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Family PACT program report fiscal year 06/07. A report to the State of California Department of Public Health Office of Family Planning. Available at: http://www.familypact.org/Files/FamPACT_AnnualReport_2006-07.pdf. Accessed July 28, 2008.
- 7. Family PACT program report fiscal year 04/05. A report to the State of California Department of Health Services Office of Family Planning. Available at: http://www.familypact.org/_resources/documents/GraphicSummaryFY04-05.pdf. Accessed June 26, 2007.
- 8.Sonfield A. Summer price spike: a case study about publicly funded clinics and the cost of contraceptive supplies. Guttmacher Policy Rev 2006;9:2–5 [Google Scholar]
- 9.Foster DG, Klaisle CM, Blum M, Bradsberry ME, Brindis CD, Stewart FH. Expanded state-funded family planning services: estimating pregnancies averted by the Family PACT Program in California, 1997–1998. Am J Public Health 2004;94:1341–1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Foster DG, Biggs MA, Amaral G, et al. Estimates of pregnancies averted through California's family planning waiver program in 2002. Perspect Sex Reprod Health 2006;38:126–131 [DOI] [PubMed] [Google Scholar]
- 11.Hatcher RA, Trussell J, Nelson AL, et al. Contraceptive Technology. 18th ed.New York, NY: Ardent Media; 2004 [Google Scholar]
- 12.Henshaw SK. Unintended pregnancy in the United States. Fam Planning Perspect 1998;30:24–29 [PubMed] [Google Scholar]
- 13.Saraiya M, Berg CJ, Shulman H, Green CA, Atrash HK. Estimates of the annual number of clinically recognized pregnancies in the United States, 1981–1991. Am J Epidemiol 1999;149:1025–1029 [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg MJ, Waugh MS, Burnhill MS. Compliance, counseling and satisfaction with oral contraceptives: a prospective evaluation. Fam Plann Perspect 1998;30:89–92, 104 [PubMed] [Google Scholar]
- 15.Ornstein RM, Fisher MM. Hormonal contraception in adolescents: special considerations. Paediatric Drugs 2006;8:25–45 [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg MJ, Waugh MS, Long S. Unintended pregnancies and use, misuse and discontinuation of oral contraceptives. J Reprod Med 1995;40:355–360 [PubMed] [Google Scholar]
- 17.Archer DF, Cullins V, Creasy GW, Fisher AC. The impact of improved compliance with a weekly contraceptive transdermal system (Ortho Evra) on contraceptive efficacy. Contraception 2004;64:189–195 [DOI] [PubMed] [Google Scholar]
- 18.Oddsson K, Leifels-Fischer B, de Melo NR, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1-year randomized trial. Contraception 2004;71:176–182 [DOI] [PubMed] [Google Scholar]