Abstract
Objectives. We assessed the relative contribution of Hispanic ethnicity, country of origin, and nativity to lifetime prevalence of asthma among mothers and children enrolled in the Project on Human Development in Chicago Neighborhoods.
Methods. We used multilevel models to analyze data from wave 3 of the Project on Human Development in Chicago Neighborhoods study (2000 to 2001). Mothers reported physician-diagnosed asthma for themselves and their children. Maternal race, ethnicity, country of origin, and nativity were the predictors of interest.
Results. We found substantial heterogeneity in lifetime asthma within Hispanic subgroups for mothers and children. Hispanics of non-Mexican origin had greater odds of having asthma than did non-Hispanic Whites; respondents of Mexican origin did not differ from non-Hispanic Whites. Odds of experiencing asthma were more strongly related to nativity than to race, Hispanic ethnicity, or country of origin. Only immigrant Mexicans reported asthma prevalence lower than that of native non-Hispanic Whites.
Conclusions. Nativity is a strong predictor of lifetime asthma prevalence, suggesting the importance of potential interactions between genetic susceptibilities and environmental factors in both the native and the host countries.
The Hispanic health paradox—the relatively better health of this subgroup of the US population, despite their low socioeconomic status—has received considerable attention.1–4 Evidence for this paradox has been most consistently observed among Mexicans, suggesting that there may be a Mexican paradox or a nativity paradox.2,5–7
Asthma is one of the health conditions for which a Hispanic paradox has been observed. According to the most recent data, 20 million children and adults in the United States suffer from asthma, with a current prevalence of 7.2%8 and with substantial heterogeneity by race/ethnicity. Non-Hispanic Whites and Blacks have a prevalence of 6.9% and 9.2%, respectively, and Hispanics have the lowest prevalence (5.4%).8 However, the heterogeneity in current asthma prevalence within subgroups of Hispanics is greater than that between Hispanics and non-Hispanics: Hispanics of Puerto Rican origin have the highest prevalence among all racial/ethnic groups (14.5%), and Hispanics of Mexican origin have the lowest (3.9%).8 This pattern has been found among children as well as adults.8
This substantial heterogeneity among Hispanics from different backgrounds9 challenges the notion of a blanket Hispanic health paradox. Asthma prevalence among Hispanics appears to be affected by maternal nativity or country of origin. Although the issue of nativity is beginning to be considered more systematically in health research,10–15 studying this heterogeneity more explicitly in epidemiological research about asthma is still needed, and the results may have implications for understanding and reducing asthma disparities.9 Our aim, therefore, was to discover whether a Hispanic health advantage in reported asthma exists and to examine the relative importance of Hispanic ethnicity, country of origin, and nativity in determining asthma prevalence.
METHODS
Our data came from the Project on Human Development in Chicago Neighborhoods, a multilevel, multimethod longitudinal study of the role of contextual factors on individual development.16–18 The study had an accelerated cohort design, with 7 different age cohorts, from prenatal to young adult (0, 3, 6, 9, 12, 15, and 18 years). Participants were enrolled in 1995 and followed up in 3 waves of data collection. All members of households in the study who were within 6 months of 1 of the 7 cohort ages at the time of enumeration were eligible to participate. Data on asthma outcomes and individual-level predictors were ascertained during the third wave of follow-up, conducted from 2000 to 2001. A survey that included asthma outcomes was administered to respondents from the age cohorts who were 0 to 9 years at enrollment and to their mothers or primary caregivers. Our analyses included children and their caregivers from those cohorts who responded to the asthma questionnaire at wave 3. The response rate for this group was 78%. The sample included 3188 children; after excluding participants with missing information on the outcome and ethnicity, we had an analytic sample of 3178 children (Table 1). The adult sample included 2560 mothers or primary caregivers. We restricted our analysis to biological mothers and excluded participants who had missing data on the outcome variable and other covariates, for a final analytic sample of 2209 (Table 1).
TABLE 1.
Distribution of Predictor Variables and Prevalence of Self-Reported Lifetime Asthma Among Mothers and Children: Project on Human Development in Chicago Neighborhoods, 2000–2001
| Mothers |
Children |
|||
| Total, Mean (SD) | Lifetime Asthma, Mean (SD) | Total, Mean (SD) | Lifetime Asthma, Mean (SD) | |
| Maternal age at wave 1 (range: 14–53 y) | 30.2 (6.98) | 30.0 (6.64) | ||
| Child's age at wave 3 (range: 2–15 y) | 8.88 (3.3) | 9.14 (3.3) | ||
| Gender | ||||
| Boys | 1629 (51.3) | 345 (60.7) | ||
| Girls | 1549 (48.7) | 223 (39.3) | ||
| Maternal smoking status | ||||
| Nonsmoker | 1680 (76.1) | 212 (68.2) | 2409 (75.8) | 409 (72.0) |
| Current smoker | 529 (24.0) | 99 (31.8) | 739 (23.3) | 152 (26.8) |
| Data missing | 30 (0.9) | 7 (1.2) | ||
| Maternal marital status | ||||
| Married | 1210 (54.8) | 135 (43.4) | 1775 (55.9) | 277 (48.8) |
| Single | 689 (31.2) | 128 (41.2) | 933 (29.4) | 204 (35.9) |
| With partner | 310 (14.0) | 48 (15.4) | 438 (13.8) | 79 (13.9) |
| Data missing | 32 (1.0) | 8 (1.4) | ||
| Race/ethnicity | ||||
| Non-Hispanic White | 423 (19.2) | 51 (16.4) | 505 (15.9) | 82 (14.4) |
| Non-Hispanic Black | 677 (30.7) | 114 (36.7) | 1058 (33.3) | 256 (45.1) |
| Mexican | 722 (32.7) | 59 (19.0) | 1002 (31.5) | 106 (18.7) |
| Other Hispanic | 275 (12.5) | 70 (22.5) | 485 (15.3) | 98 (17.3) |
| Non-Hispanic other | 97 (4.4) | 11 (3.5) | 128 (4.0) | 26 (4.6) |
| Data missing | 15 (0.7) | 6 (1.9) | ||
| Maternal nativitya | ||||
| Foreign born | 870 (39.4) | 70 (22.5) | 1227 (38.6) | 133 (23.4) |
| US born | 1324 (59.9) | 239 (76.8) | 1889 (59.4) | 421 (74.1) |
| Data missing | 15 (0.7) | 2 (0.6) | 62 (2.0) | 14 (2.5) |
| Maternal education | ||||
| < High school | 339 (15.4) | 39 (12.5) | 83 (2.6) | 65 (11.4) |
| Some high school | 494 (22.4) | 77 (24.8) | 512 (16.1) | 133 (23.4) |
| High school graduate | 296 (13.4) | 40 (12.9) | 730 (23.0) | 59 (10.4) |
| Some college | 789 (35.7) | 118 (37.9) | 416 (13.1) | 237 (41.7) |
| College graduate | 263 (11.9) | 34 (10.9) | 1082 (34.1) | 61 (10.7) |
| Data missing | 28 (1.3) | 3 (1.0) | 355 (11.2) | 13 (2.3) |
| Equivalized income, $ | ||||
| 0–15 000 | 1383 (62.6) | 202 (65.0) | 1984 (62.4) | 346 (60.9) |
| 15 000–20 000 | 180 (8.2) | 21 (6.8) | 251 (7.9) | 39 (6.9) |
| 20 000–30 000 | 296 (13.4) | 40 (12.9) | 419 (13.2) | 71 (12.5) |
| ≥ 30 000 | 221 (10.0) | 27 (8.7) | 281 (8.8) | 59 (10.4) |
| Data missing | 129 (5.8) | 21 (6.8) | 243 (7.7) | 53 (9.3) |
| Maternal nativity and race/ethnicity | ||||
| US-born non-Hispanic White | 356 (16.1) | 47 (15.1) | 417 (13.1) | 72 (2.5) |
| Immigrant non-Hispanic White | 64 (2.9) | 4 (1.3) | 80 (2.5) | 7 (12.7) |
| Non-Hispanic Blackb | 674 (30.5) | 114 (36.7) | 1035 (32.6) | 252 (1.2) |
| Mexican American | 135 (6.1) | 23 (7.4) | 189 (6.0) | 27 (44.4) |
| Immigrant Mexican | 585 (26.5) | 36 (11.6) | 808 (25.4) | 78 (4.8) |
| US-born other Hispanic | 122 (5.5) | 43 (13.8) | 226 (7.1) | 61 (13.7) |
| Immigrant other Hispanic | 150 (6.8) | 26 (8.4) | 241 (7.6) | 33 (10.7) |
| US-born other non-Hispanic | 46 (2.1) | 7 (2.3) | 54 (1.7) | 11 (5.8) |
| Immigrant other non-Hispanic | 50 (2.3) | 4 (1.3) | 66 (2.1) | 13 (1.9) |
| Data missing | 27 (1.2) | 7 (2.3) | 62 (2.0) | 14 (2.3) |
| Maternal length of stay in US | ||||
| US born | 1324 (59.9) | 239 (76.9) | 1889 (59.4) | 421 (74.1) |
| 0–4 y | 160 (7.2) | 6 (1.9) | 210 (6.6) | 20 (3.5) |
| 5–9 y | 241 (10.9) | 17 (5.5) | 324 (10.2) | 33 (5.8) |
| 10–14 y | 132 (6.0) | 11 (3.5) | 183 (5.8) | 19 (3.4) |
| ≥ 15 y | 291 (13.2) | 32 (10.3) | 427 (13.4) | 58 (10.2) |
| Data missing | 61 (2.8) | 6 (1.9) | 145 (4.6) | 17 (3.0) |
| Breastfeeding | ||||
| No | 1578 (49.7) | 302 (53.2) | ||
| Yes | 1557 (49.0) | 260 (45.8) | ||
| Data missing | 43 (1.4) | 6 (1.1) | ||
| Maternal asthma | ||||
| No | 2678 (84.3) | 388 (68.3) | ||
| Ever had asthma | 432 (13.6) | 168 (29.6) | ||
| Data missing | 68 (2.1) | 12 (2.1) | ||
Note. Among mothers, n = 2209, with 311 reporting lifetime asthma. Among children, n = 3178, with 568 reporting lifetime asthma.
Place of birth.
Includes both US- and foreign-born non-Hispanic Blacks.
Asthma outcomes were ascertained through the International Study of Asthma and Allergies in Childhood survey.19 For children, we used maternal report of physician-diagnosed asthma during the child's life (lifetime asthma). Mothers who reported a diagnosis of asthma by a physician were categorized as having a positive lifetime asthma status. We also used alternative measures of asthma (i.e., current asthma, unconfirmed possible asthma) in sensitivity analyses to address concerns about underdiagnosis of asthma attributable to racial/ethnic disparities. Current asthma was defined as both a report of having been diagnosed with asthma by a health care professional and having current asthma symptoms (i.e., wheezing or using prescription medication for wheezing). Unconfirmed possible asthma was defined as never having received a diagnosis of asthma by a health care professional but reporting symptoms or medication use suggestive of asthma (i.e., wheezing or using prescription medication for wheezing).20,21
We considered 3 predictor variables. Maternal race/ethnicity was specified as non-Hispanic White, non-Hispanic Black, non-Hispanic other, or Hispanic. Respondents who failed to report race/ethnicity were considered to be a missing group and included as a separate category. We divided the Hispanic subgroup into persons of Mexican origin (referred to as Mexican) and other Hispanics. Maternal nativity was categorized as foreign born or US born. Most (95.4%) of the children were born in the United States, so we categorized them by their mother's nativity status.
We also tested for an interaction between race, Hispanic ethnicity and country of origin, and nativity. For ease of interpretation we included these as 1 variable with the following categories derived from combinations of mother's race, Hispanic ethnicity and country of origin, and nativity: non-Hispanic White American, non-Hispanic White immigrant, Mexican American, immigrant Mexican, Hispanic American, immigrant Hispanic, other non-Hispanic American, other non-Hispanic immigrant, and missing. The term American was used to represent participants who were born in the United States, and immigrants were defined as those who were born elsewhere. Non-Hispanic Blacks were not disaggregated into US and foreign born because few Black respondents were foreign born.
Hispanic and Latino are generic categories that are often used interchangeably. Although the term Latino is preferred among many Latino investigators, it clashes with the standard term for White or Anglo American, which is non-Hispanic White. Accordingly, we used Hispanic. We should note that the non-Mexican Hispanics (i.e., other Hispanics) in our study were primarily Puerto Ricans, who are US citizens. Consequently, the American or immigrant distinction for this group is more precisely a mainland or island distinction.
We analyzed age, marital status, education, equivalized income categories, and smoking status as covariates in the maternal sample. Equivalized income is a household income figure that takes account of the number of people in the household. We adopted the equivalization procedure used in the Luxembourg Income Study, which divides the household income by the square root of the number of household members.22 For the analysis of the child sample, we also included maternal history of asthma, child's gender and age, and whether the child had been breastfed. Information on sociodemographic characteristics and ethnic identification were obtained at wave 1 (baseline); data on maternal smoking and breastfeeding history were collected at wave 3, when asthma outcomes were ascertained.
Our data had a multilevel structure, with individuals at level 1 nested within 81 neighborhood clusters at level 2. To account for potential neighborhood variation in asthma, we adopted a multilevel logistic regression modeling approach.23,24 The principles and relevance of multilevel modeling for analyzing clustered data have been well described.25–27 The generic model was specified as a binary response y (diagnosed for asthma or not), for individual i living in neighborhood cluster j with a logit-link function:
 |
The equation consisted of a fixed part β0 + β(x) and random effects attributable to neighborhood clusters (u0j). The parameter β0 estimated the log odds for reporting asthma for the reference group, and β represented a vector of regression parameters associated with a vector of different independent variables (x). Assuming an independent and identical distribution, the random effects (u0j) associated with the neighborhood cluster were summarized as σu2, which quantified the neighborhood variance in the asthma. We used predictive quasi-likelihood procedures with first-order Taylor linearization, implemented with MLwiN.28,29
The following models were estimated. First, we modeled the log odds of asthma as a function of mother's race/ethnicity and nativity (separately as well as with mutual adjustment), adjusted for individual covariates and conditional on the random effect for neighborhoods. In this formulation, Hispanic ethnicity was not distinguished by country of origin. This model allowed an assessment of the relative importance of race/ethnicity and nativity. Second, we reestimated the first model by disaggregating Hispanic ethnicity by mother's country of origin (Mexican or not). This formulation estimated the relative importance of Hispanic ethnicity and country of origin on one hand and nativity on the other. Finally, we modeled the log odds of reported asthma by considering combinations of race, Hispanic ethnicity and country of origin, and nativity to assess the potential interaction between them. Together, these models tested our hypothesis that Hispanic subgroups would show heterogeneity in asthma prevalence and that odds of experiencing asthma would be affected by nativity.
RESULTS
Table 1 shows the attributes for the cohort. Approximately one third of the respondents were Mexicans, another one third were non-Hispanic Blacks, and 18% were non-Hispanic Whites. Other Hispanics composed about 12% of the maternal sample and 15% of the child sample. Overall, 11% of mothers and 18% of children reported lifetime asthma, with substantial heterogeneity between racial/ethnic groups. Mexican mothers and children had the lowest prevalence of asthma, with 6% and 11%, respectively, followed by non-Hispanic Whites (mothers, 9%; children, 16%). Non-Hispanic Blacks and other Hispanics had substantially higher prevalence of asthma among mothers (13% and 19%, respectively) as well as children (24% and 20%, respectively). Mothers born outside of the United States (40% of the sample) had a substantially lower lifetime prevalence of asthma (5%) than did those born in the United States (14%). We also observed this pattern in children: those whose mothers were not born in the United States had a lifetime asthma prevalence of 11%; the children of US-born mothers had a prevalence of 22%.
In models that mutually adjusted for race/ethnicity and nativity, as well as adjusting for sociodemographic and other risk factors, the odds ratio (OR) for reported asthma among Hispanic mothers was 2.05 (95% confidence interval [CI] = 1.32, 3.18) compared with non-Hispanic Whites (Table 2). Immigrant mothers, regardless of race/ethnicity, had a substantially lower risk of reported asthma (OR = 0.26; 95% CI = 0.17, 0.39) than did those born in the United States. Hispanic ethnicity increased the odds of reporting asthma among children, but this finding was not statistically significant. Children born to immigrant mothers had a substantially lower risk of asthma (OR = 0.50; 95% CI = 0.37, 0.68) than did children born to American mothers.
TABLE 2.
Mutually Adjusted Odds Ratios (ORs) for Lifetime Reported Asthma Among Mothers and Children, by Race/Ethnicity and Nativity: Project on Human Development in Chicago Neighborhoods, 2000–2001
| Model 1a |
Model 2b |
|||
| OR (95% CI) | P | OR (95% CI) | P | |
| Mothers | ||||
| Race/ethnicity | ||||
| Non-Hispanic White (Ref) | 1.00 | 1.00 | ||
| Non-Hispanic Black | 1.16 (0.76, 1.79) | .49 | 1.13 (0.74, 1.74) | .57 |
| Hispanic | 1.20 (0.79, 1.82) | .39 | 2.05 (1.32, 3.18) | .002 |
| Non-Hispanic other | 0.90 (0.44, 1.84) | .77 | 1.26 (0.60, 2.63) | .54 |
| Nativityc | ||||
| US born (Ref) | 1.00 | 1.00 | ||
| Foreign born | 0.36 (0.25, 0.52) | <.001 | 0.26 (0.17, 0.39) | <.001 |
| Data missing | 0.71 (0.15, 3.31) | .66 | 0.46 (0.09, 2.37) | .36 |
| Children | ||||
| Race/ethnicity | ||||
| Non-Hispanic White (Ref) | 1.00 | 1.00 | ||
| Non-Hispanic Black | 1.60 (1.15, 2.23) | .006 | 1.54 (1.10, 2.13) | .01 |
| Hispanic | 0.97 (0.69, 1.35) | .84 | 1.23 (0.87, 1.74) | .25 |
| Non-Hispanic other | 1.47 (0.88, 2.46) | .15 | 1.78 (1.05, 3.03) | .03 |
| Maternal nativityc | ||||
| US born (Ref) | 1.00 | 1.00 | ||
| Foreign born | 0.48 (0.37, 0.63) | <.001 | 0.50 (0.37, 0.68) | <.001 |
| Data missing | 1.09 (0.44, 2.72) | .86 | 1.08 (0.43, 2.71) | .87 |
Note. CI = confidence interval.
Adjusted for age (centered by mean age), marital status, maternal education, household equivalized income, maternal smoking status. For children, the model also adjusted for child's gender, breastfeeding, and maternal history of asthma.
Adjusted for the covariates in model 1 and mutually adjusted for race/ethnicity and nativity.
Place of birth.
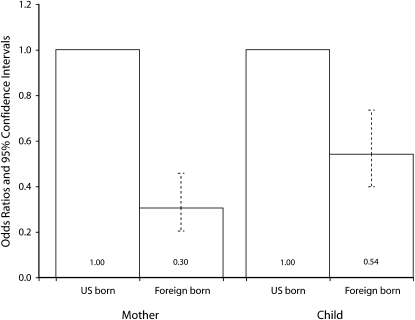
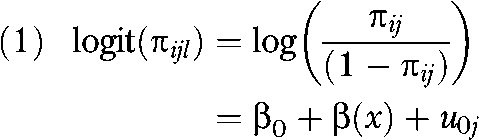
Disaggregating the Hispanic effect by country of origin revealed substantial heterogeneity in the odds of reported asthma (Figure 1). The odds ratios for reported asthma were not significantly different between non-Hispanic White adults and Mexican adults (P = .728). Non-Mexican Hispanics had a substantially increased risk of reporting asthma (OR = 3.47; 95% CI = 2.17, 5.53) compared with non-Hispanic White adults. A similar pattern was observed in the relationship between maternal Hispanic ethnicity and country of origin and the odds of reported asthma among children. Children of non-Mexican Hispanic mothers had a higher risk of experiencing asthma than did other children of non-Hispanic White mothers (OR = 1.52; 95% CI = 1.05, 2.21). Even after controlling for the nativity effect for Mexican origin, reported asthma was substantially lower among immigrant mothers (OR = 0.30; 95% CI = 0.20, 0.46) and children born to immigrant mothers (OR = 0.54; 95% CI = 0.40, 0.73) than among American mothers and their children (Figure 2).
FIGURE 1.
Odds ratios and 95% confidence intervals for lifetime reported asthma among mothers and children, by race/ethnicity: Project on Human Development in Chicago Neighborhoods, 2000–2001.
Note. The results reflect adjustment for age (centered by mean age), marital status, mother's education, household equivalized income, mother's smoking status, and place of birth. Models predicting child's asthma were further adjusted for gender, maternal history of asthma, and breastfeeding.
FIGURE 2.
Odds ratios and 95% confidence intervals for lifetime reported asthma among mothers and children, by nativity: Project on Human Development in Chicago Neighborhoods, 2000–2001.
Note. The results reflect adjustment for age (centered by mean age), marital status, mother's education, household equivalized income, mother's smoking status, and place of birth. Models predicting child's asthma were further adjusted for gender, maternal history of asthma, and breastfeeding.
Table 3 presents adjusted results for the effect of various combinations of race, Hispanic ethnicity and country of origin, and nativity on the odds of reported asthma among mothers and children. Compared with non-Hispanic White American mothers, immigrant Mexican mothers were considerably less likely to report asthma (OR = 0.33; 95% CI = 0.18, 0.60), but Mexican Americans were more likely to report asthma, although this differential did not achieve statistical significance (P = .37). American Hispanic mothers of non-Mexican origin were more than 3 times as likely as American non-Hispanic White mothers to report asthma (OR =3.36; 95% CI = 1.97, 5.73).
TABLE 3.
Adjusted Odds Ratios (AORs) for Lifetime Reported Asthma Prevalence Among Mothers and Children, by Race/Ethnicity and Maternal Nativity: Project on Human Development in Chicago Neighborhoods, 2000–2001
| AOR (95% CI) | P | |
| Mothers | ||
| Nativity and race/ethnicity | ||
| US-born non-Hispanic White (Ref) | 1.00 | |
| Immigrant non-Hispanic White | 0.48 (0.16, 1.39) | .178 |
| Non-Hispanic Blacka | 1.17 (0.76, 1.81) | .483 |
| Mexican American | 1.31 (0.73, 2.37) | .365 |
| Immigrant Mexican | 0.33 (0.18, 0.60) | <.001 |
| US-born other Hispanic | 3.36 (1.97, 5.73) | <.001 |
| Immigrant other Hispanic | 1.20 (0.68, 2.13) | .536 |
| US-born other non-Hispanic | 1.02 (0.42, 2.47) | .965 |
| Immigrant other non-Hispanic | 0.65 (0.22, 1.93) | .439 |
| Data missing | 2.15 (0.82. 5.64) | .124 |
| Children | ||
| Maternal nativity and race/ethnicity | ||
| US-born non-Hispanic White (Ref) | 1.00 | |
| Immigrant non-Hispanic White | 0.52 (0.22, 1.19) | .115 |
| Non-Hispanic Black (US- and foreign-born) | 1.54 (1.09, 2.20) | .354 |
| Mexican American | 0.83 (0.49, 1.40) | .149 |
| Immigrant Mexican | 0.54 (0.34, 0.85) | <.001 |
| US-born other Hispanic | 1.74 (1.13, 2.68) | .040 |
| Immigrant other Hispanic | 0.73 (0.45, 1.20) | .030 |
| US-born other non-Hispanic | 1.17 (0.56, 2.45) | .742 |
| Immigrant other non-Hispanic | 1.42 (0.72, 2.83) | .538 |
| Data missing | 1.44 (0.56, 3.73) | .573 |
Note. CI = confidence interval. Adjusted for age (centered by mean age), marital status, maternal education, household equivalized income, and maternal smoking status. For children, models were also adjusted for child's gender, breastfeeding, and maternal history of asthma.
Includes both US- and foreign-born non-Hispanic Blacks.
Compared with children born to non-Hispanic White American mothers, children born to immigrant Mexican mothers had an odds ratio of 0.54 (95% CI = 0.34, 0.85) for reporting asthma (Table 3). Children born to American mothers belonging to other Hispanic groups had higher odds of reporting asthma (OR = 1.74; 95% CI= 1.13, 2.68) compared with children born to non-Hispanic White American mothers. Immigrant groups appeared to have a lower risk of reporting asthma (for mothers and children), although results in the remaining groups did not reach statistical significance (Table 3).
We also conducted sensitivity analyses to reduce the likelihood that these findings were confounded by differential access to health care. Ethnic-minority populations have been shown to have differential access to quality health care because of many factors (e.g., language preference, cultural beliefs and practices, health care–seeking behaviors, trust). It is therefore possible that our results for asthma prevalence, derived from reports of asthma diagnoses, may have been underestimated for ethnic minorities in this sample.20,21 Furthermore, asthma prevalence could have been underestimated among respondents who did not currently have symptoms, because asthma may be perceived as an intermittent rather than a chronic disease. To address these possibilities, we conducted sensitivity analyses with alternative definitions of asthma. Data were available on possible symptoms of asthma for children (i.e., report of wheezing or taking medicine for wheezy breathing without having received a physician's diagnosis), which we used to assess the extent to which our findings could be influenced by access to health care. We found no significant differences attributable to race/ethnicity and nativity in the prevalence of undiagnosed possible asthma (data available as a supplement to the online article at http://www.ajph.org). If access to health care were affecting the results, we would expect to see an even higher prevalence of unconfirmed possible asthma associated with our variables, so health care access probably did not have a major influence on our findings.
To address whether participants viewed asthma as a chronic disease, we reran the analysis predicting current asthma (defined as ever being diagnosed with asthma and having symptoms in the past 12 months); these results were qualitatively similar to our findings for lifetime prevalence of physician-diagnosed asthma, suggesting that a lack of current symptoms did not significantly affect our results.
DISCUSSION
Our study had 3 salient findings. First, it corroborated the substantial Hispanic heterogeneity in asthma.9 Indeed, the heterogeneity in lifetime asthma among Hispanic subgroups was considerably greater than the difference between Hispanic and non-Hispanic groups. Second, the association between nativity and reported asthma was significantly stronger than the association between asthma and Hispanic ethnicity and country of origin. Not only was birth in another country associated with lower asthma prevalence, but nativity also accounted for much of the Hispanic heterogeneity in lifetime reported asthma. Finally, our data demonstrated the remarkable specificity in the reputed Hispanic health paradox: risk of lifetime asthma was lower only for immigrant Mexicans. Results for the remaining combinations of Hispanic ethnicity and country of origin (i.e., Mexican Americans, other immigrant Hispanics, or other Hispanic Americans) did not suggest any lowered asthma risk. Importantly, immigrant non-Mexican Hispanics and non-Mexican Hispanic Americans had the highest rates of asthma.
These findings were consistent across alternative outcomes (e.g., current asthma or undiagnosed possible asthma) and were not sensitive to inclusion of various demographic, socioeconomic, and known asthma risk factors. Our results suggest the overwhelming importance of nativity on reported asthma. They are largely consistent with the limited evidence that shows a protective effect of nativity for Mexicans,30 although a wider and more systematic investigation into the effects of nativity across other racial/ethnic groups is warranted.
Because a nativity effect has been demonstrated, it is important to understand why immigrants to the United States (and in our study, immigrant Mexicans) have a considerable health advantage over US natives of equivalent socioeconomic status.
One interpretation of the nativity effect is that it simply reflects a healthy migrant effect: those who are healthy or have relatively lower levels of morbidity are more likely to migrate. In other words, the nativity advantage we observed was attributable to the selective migration of individuals with lower asthma morbidity. This interpretation is compelling and intuitive, but the existing evidence is sparse and mixed. For example, infant mortality among Puerto Ricans was found to be lower among recent migrants to the United States than among nonmigrant families in Puerto Rico.39 However, a recent analysis of nationally representative longitudinal data from the Mexican Family Life Survey found that although health significantly predicted subsequent migration, the associations were weak and only a few health indicators were statistically significant.40
Although it is likely that individuals who migrate to the United States are generally healthier than their compatriots, it is equally possible (and especially in the case of asthma) that the health of immigrants reflects the general environmental and socioeconomic conditions of their native countries. In other words, Mexican citizens may be exposed to protective environmental factors that have not yet been discovered. This may be especially important for the mothers in our study who lived in Mexico during childhood. Epidemiological studies have underscored the importance of the early childhood environment in asthma risk.41
One mechanism through which nativity may influence asthma may pertain to the hygiene hypothesis. Early-life exposure to agricultural environments (especially to livestock) has been shown to be protective against the development of asthma and allergies.42–44 Indeed, asthma rates tend to be higher in industrialized and urbanized countries.45–47 Although our data did not specify whether respondents came from rural or urban environments, it is clear that a substantial majority of Mexican immigrants in the United States came from rural areas in Mexico.48,49
A nativity effect on asthma rates within an ethnic group underscores the importance of both environment and genetic susceptibility in the development and persistence of asthma symptoms. The synergistic importance of genes and the environment in explaining ethnicity differences in asthma is an active area of investigation. Hispanic subgroups may differ from one another in their environmental exposures, culture, and social indicators, as well as in their heredity. Hispanics represent a heterogeneous mix of American Indian, European, and African ancestries, and the complexities of the underlying genetic determinants across Hispanic groups are only beginning to be explored.50 Variable genetic vulnerability across Hispanic groups may confer ethnic-specific gene-by-environment interactions that contribute to asthma expression. Only a few studies have examined genetic risk among different Hispanic ethnic groups in the context of relevant environmental factors, although this has become a research priority in pediatrics.51
Limitations
Our measure of asthma prevalence was derived from self-reports. However, we used the standardized International Study of Asthma and Allergies in Childhood survey to ascertain asthma morbidity; this instrument has been validated in Mexican and other Latin American populations.31–33 It is also possible that the observed differences in asthma between Hispanics (and specifically immigrant Mexicans) and non-Hispanics could be attributable to diagnostic bias arising out of language differences in administering the questionnaire. We believe this was unlikely because studies from Mexico (conducted with internationally comparable assessments) report comparably lower rates of asthma and wheezing.34,35 It is still possible that immigrant Mexicans might have underestimated the presence of asthma morbidity and symptoms, given lower health expectations and less access to health care services. However, if less access to health services resulted in an underreporting of asthma morbidity, we would expect similar underreporting by respondents from other Hispanic groups (mainly Puerto Ricans in this study). We did not observe such an effect.
Our study was restricted to the city of Chicago, which may limit generalization to other populations. However, because of the large proportion of Mexicans in its Hispanic community (and therefore in our sample), Chicago may have been an ideal place to test the existence of a Hispanic paradox. Finally, our estimates of nativity effects among children were based on the mother's rather than the child's nativity, because of the small sample size of children born outside of the United States.
Much of the literature on the Hispanic health paradox has focused on documenting how acculturation36,37 erodes the initial health advantage that immigrants have.37 These studies commonly measure acculturation by nativity or length of stay in the United States.37,38 This is problematic because it conflates important distinctions. Our finding of an independent and strong nativity effect in asthma suggests the overwhelming importance of conditions in the native country. This emphasis is often lost, or considerably diluted, when nativity effects are considered only in the context of acculturation.
Indeed, the notion of acculturation invokes a different question: what conditions in the host environment tend to dissipate the nativity advantage? It is important to examine the effect of acculturation on the health outcomes of immigrants, but considering nativity or length of residence in the host country in the context of acculturation conflates distinctive questions and provides little understanding of either.
Conclusions
Our study provides further evidence to contest the widespread use of the term health paradox in explaining asthma prevalence among Hispanics. Repeated use of this term misleadingly discounts the substantial heterogeneity within Hispanic subgroups. Indeed, Hispanics who are not of Mexican origin have the highest burden of asthma. Moreover, Mexicans (regardless of their nativity) do not have lower asthma prevalence than do non-Hispanic Whites. To the extent there might be a health paradox, it is clearly based on nativity and not ethnicity. Our results comprehensively demonstrate this to be so among immigrant Mexicans, but a more systematic examination of the effects of nativity on asthma among other ethnic groups would likely shed more light on the nature of the racial/ethnic distribution of asthma in the United States.
Acknowledgments
S. V. Subramanian is supported by a National Institutes of Health Career Development Award (NHLBI K25 HL081275).
We are grateful to Dolores Acevedo Garcia for her extremely helpful comments on our article, as well as to 4 anonymous reviewers for constructive comments.
Human Participant Protection
The study was approved by the institutional review board of the Harvard School of Public Health.
References
- 1.Vega WA, Amaro H. Latino outlook: good health, uncertain prognosis. Annu Rev Public Health 1994;15:39–67 [DOI] [PubMed] [Google Scholar]
- 2.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis 2001;11(3):496–518 [PubMed] [Google Scholar]
- 3.Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann N Y Acad Sci 2001;954:140–174 [DOI] [PubMed] [Google Scholar]
- 4.Scribner R. Paradox as paradigm–the health outcomes of Mexican Americans. Am J Public Health 1996;86(3):303–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao Y, Cooper RS, Cao G, et al. Mortality patterns among adult Hispanics: findings from the NHIS, 1986 to 1990. Am J Public Health 1998;88(2):227–232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health 1999;89(10):1543–1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guendelman S. Mexican women in the United States. Lancet 1994;344(8919):352. [DOI] [PubMed] [Google Scholar]
- 8.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma–United States, 1980–2004. MMWR Surveill Summ 2007;56(8):1–54 [PubMed] [Google Scholar]
- 9.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics 2006;117(1):43–53 [DOI] [PubMed] [Google Scholar]
- 10.Hajat A, Lucas JB, Kington R. Health outcomes among Hispanic subgroups: data from the National Health Interview Survey, 1992-95. Adv Data 2000 Feb 25. (310):1–14 [PubMed] [Google Scholar]
- 11.Hummer RA, Rogers RG, Nam CB, LeClere FB. Race/ethnicity, nativity, and US adult mortality. Soc Sci Q 1999;80(1):136–153 [Google Scholar]
- 12.Dey AN, Lucas JW. Physical and mental health characteristics of US- and foreign-born adults: United States, 1998–2003. Adv Data 2006 Mar 1. (369):1–19 [PubMed] [Google Scholar]
- 13.Acevedo-Garcia D, Bates LM. Latino health paradoxes: empirical evidence, explanations, future research, and implications. In: Rodriguez H, Saenz R, Menjivar C, eds Latino/as in the United States: Changing the Face of America. New York, NY: Springer; 2007:101–113 [Google Scholar]
- 14.Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics 2005;115(1):e20–e30 [DOI] [PubMed] [Google Scholar]
- 15.Acevedo-Garcia D, Soobader MJ, Berkman LF. Low birthweight among US Hispanic/Latino subgroups: the effect of maternal foreign-born status and education. Soc Sci Med 2007;65(12):2503–2516 [DOI] [PubMed] [Google Scholar]
- 16.Earls F, Buka SL. Project on Human Development in Chicago Neighborhoods. Technical report. Rockville, MD: National Institute of Justice; 1997 [Google Scholar]
- 17.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science 1997;277:918–924 [DOI] [PubMed] [Google Scholar]
- 18.Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proc Natl Acad Sci U S A 2008;105(3):845–852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asher MI, Keil U, Anderson HR, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995;8(3):483–491 [DOI] [PubMed] [Google Scholar]
- 20.Pearson WS, Ahluwalia IB, Ford ES, Mokdad AH. Language preference as a predictor of access to and use of healthcare services among Hispanics in the United States. Ethn Dis 2008;18(1):93–97 [PubMed] [Google Scholar]
- 21.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and the use of services in US children. Pediatrics 2008;121(2):e286–e298 Epub 2008 Jan 14 [DOI] [PubMed] [Google Scholar]
- 22.Buhmann B, Rainwater L, Schmaus G, Smeeding TM. Equivalence scales, well-being, inequality, and poverty: sensitivity estimates across ten countries using the Luxembourg Income Study (LIS) database. Rev Income Wealth 1988;34(2):115–142 [Google Scholar]
- 23.Goldstein H. Multilevel Statistical Models. 3rd ed London, England: Arnold; 2003 [Google Scholar]
- 24.Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. Thousand Oaks, CA: Sage Publications; 2002 [Google Scholar]
- 25.Blakely T, Subramanian SV Multilevel studies. In: Oakes JM, Kaufman JS, eds Methods in Social Epidemiology. San Francisco, CA: Jossey-Bass; 2006:316–340 [Google Scholar]
- 26.Subramanian SV. The relevance of multilevel statistical methods for identifying causal neighborhood effects. Soc Sci Med 2004;58(10):1961–1967 [DOI] [PubMed] [Google Scholar]
- 27.Subramanian SV, Jones K, Duncan C. Multilevel methods for public health research. In: Kawachi I, Berkman LF, eds Neighborhoods and Health. New York, NY: Oxford University Press; 2003:65–111 [Google Scholar]
- 28.Goldstein H, Rasbash J. Improved approximations for multilevel models with binary responses. J Royal Stat Soc A 1996;159:505–513 [Google Scholar]
- 29.Rasbash J, Steele F, Browne W, Prosser B. A User's Guide to MLwiN Version 2.0. London, England: Centre for Multilevel Modelling, Institute of Education; 2004 [Google Scholar]
- 30.Eldeirawi K, McConnell R, Freels S, Persky VW. Associations of place of birth with asthma and wheezing in Mexican American children. J Allergy Clin Immunol 2005;116(1):42–48 [DOI] [PubMed] [Google Scholar]
- 31.Del-Rio-Navarro B, Berber A, Blandon-Vijil V, et al. Identification of asthma risk factors in Mexico City in an International Study of Asthma and Allergy in Childhood survey. Allergy Asthma Proc 2006;27(4):325–333 [DOI] [PubMed] [Google Scholar]
- 32.Del-Rio-Navarro B, Del Rio-Chivardi JM, Berber A, Sienra-Monge JJ, Rosas-Vargas MA, Baeza-Bacab M. Asthma prevalence in children living in north Mexico City and a comparison with other Latin American cities and world regions. Allergy Asthma Proc 2006;27(4):334–340 [DOI] [PubMed] [Google Scholar]
- 33.Pearce N, Aït-Khaled N, Beasley R, et al. Worldwide trends in the prevalence of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2007;62:758–766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mallol J, Sole D, Asher I, Clayton T, Stein R, Soto-Quiroz M. Prevalence of asthma symptoms in Latin America: the International Study of Asthma and Allergies in Childhood (ISAAC). Pediatr Pulmonol 2000;30(6):439–444 [DOI] [PubMed] [Google Scholar]
- 35.Tatto-Cano MI, Sanin-Aguirre LH, Gonzalez V, Ruiz-Velasco S, Romieu I. Prevalencia de asma, rinitis y eczema en escolares de la ciudad de Cuernavaca, Morelos [Prevalence of asthma, rhinitis and eczema in school children in the city of Cuernavaca, Mexico] Salud Publica Mex 1997;39:497–506 [PubMed] [Google Scholar]
- 36.Gold DR, Acevedo-Garcia D. Immigration to the United States and acculturation as risk factors for asthma and allergy. J Allergy Clin Immunol 2005;116(1):38–41 [DOI] [PubMed] [Google Scholar]
- 37.Abraido-Lanza AF, Armbrister AN, Florez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health 2006;96(8):1342–1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amaro H, de la Torre A. Public health needs and scientific opportunities in research on Latinas. Am J Public Health 2002;92(4):525–529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Landale NS, Oropesa RS, Gorman BK. Migration and infant death: assimilation or selective migration among Puerto Ricans? Am Sociol Rev 2000;65:888–909 [Google Scholar]
- 40.Rubalcava LN, Teruel GM, Thomas D, Goldman N. The healthy migrant effect: new findings from the Mexican Family Life Survey. Am J Public Health 2008;98(1):78–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu AH, Szefler SJ. Advances in childhood asthma: hygiene hypothesis, natural history, and management. J Allergy Clin Immunol 2003;111(3 suppl):S785–S792 [DOI] [PubMed] [Google Scholar]
- 42.Braun-Fahrlander C, Riedler J, Herz U, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med 2002;347(12):869–877 [DOI] [PubMed] [Google Scholar]
- 43.Riedler J, Eder W, Oberfeld G, Schreuer M. Austrian children living on a farm have less hay fever, asthma and allergic sensitization. Clin Exp Allergy 2000;30(2):194–200 [DOI] [PubMed] [Google Scholar]
- 44.Kilpelainen M, Terho EO, Helenius H, Koskenvuo M. Farm environment in childhood prevents the development of allergies. Clin Exp Allergy 2000;30(2):201–208 [DOI] [PubMed] [Google Scholar]
- 45.Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet 1998;351:1225–1232 [DOI] [PubMed] [Google Scholar]
- 46.Beasley R, Crane J, Lai CK, Pearce N. Prevalence and etiology of asthma. J Allergy Clin Immunol 2000;105(2 pt 2):S466–S472 [DOI] [PubMed] [Google Scholar]
- 47.von Mutius E, Fritzsch C, Weiland SK, Roll G, Magnussen H. Prevalence of asthma and allergic disorders among children in united Germany: a descriptive comparison. BMJ 1992;305(6866):1395–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fussell E. Sources of Mexico's migration stream: rural, urban, and border migrants to the United States. Soc Forces 2004;82:937–967 [Google Scholar]
- 49.Fussell E, Massey DS. The limits to cumulative causation: international migration from Mexican urban areas. Demography 2004;41(1):151–171 [DOI] [PubMed] [Google Scholar]
- 50.Choudhry S, Seibold MA, Borrell LN, et al. Dissecting complex diseases in complex populations: asthma in Latino Americans. Proc Am Thorac Soc 2007;4(3):226–233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA 2002;288(1):82–90 [DOI] [PubMed] [Google Scholar]