Abstract
Manual chopping of the nucleus forms the backbone of nucleus reduction in manual small-incision cataract surgery (MSICS). The technique (“prechopping”) described by Akahoshi has been modified so that it is safe, predictable, and easy to use in MSICS.
Keywords: Akahoshi, Bhatti, low astigmatism, manual small incision cataract surgery, nucleus reduction, prechop
Despite the widespread adoption of phacoemulsification, there is still a pressing need for manual small incision cataract surgery (MSICS) that can deliver comparable results with quicker and cheaper methods. The purpose of this report is to describe prechopping technique of Akahoshi[1] modified by the author for MSICS.
Technique
A corneal tunnel of about 5–6 mm is made either nasally in the left eye or temporally in the right eye, and the anterior chamber (AC) is entered along its entire width, after making a continuous curvilinear capsulorrhexis. With hydrodissection and/or hydrodelineation, the nucleus is prolapsed into the AC. After the injection of methylcellulose in the AC to cushion the nucleus from the capsule and endothelium, the nucleus is then tilted so that the part near the 5–6 mm corneal tunnel is towards the endothelium, and the part away from the tunnel still rests in the capsular bag. The prechopper is then introduced from the right (the tunnel has been made nasally or temporally so that it is always on the right) through the corneal tunnel and the AC into the posterior part of the tilted nucleus, while the nucleus is supported and pressed mildly away from the endothelium by a dialer introduced through a small sideport in the upper left part of the limbus. It must be ensured that the sharp prechopper blades have burrowed into the nucleus and are not merely in the epinucleus, before the cross-action prechopper is squeezed to separate the blades and cleanly chop the nucleus into two halves along natural cleavage planes. The two halves can then be further distracted by pushing apart with the closed blades of the prechopper on one hand and the dialer on the other. These two halves are removed from the AC by vectis removal aided by methylcellulose in the AC. Various steps of the surgery are depicted in Figs. 1–6.
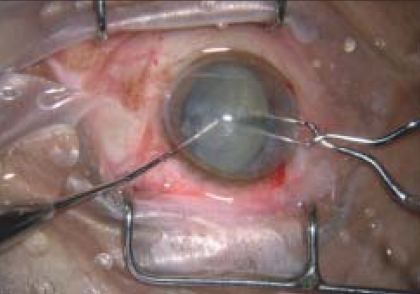
Figure 1.
The nucleus is dislocated into the anterior chamber
Figure 6.
The second nuclear fragment is removed by a vectis
Figure 2.
The prechopper buries into the nucleus from behind (on the right) while the dialer stabilizes the nucleus from above (on the left)
Figure 3.
The prechopper handle is squeezed to separate the blades and chop the nucleus
Figure 4.
The cleft in the nucleus is widened by distracting the 2 instruments
Figure 5.
The first nuclear fragment is removed by a vectis
Discussion
In the original Akahoshi technique,[1,2] Akahoshi has described the prechopping of the nucleus into four quadrants with a single-handed technique using a cross-action forceps with pointed tips and flat blades. After a 3-mm corneal tunnel incision, the Akahoshi chopper forceps is inserted, in the closed position, into the nucleus while it rests in the bag (after loosening by hydrodissection). The forceps is then opened cleaving the nucleus. The cleavage can then be extended till the entire nucleus is prechopped by the repeated insertion and opening of the forceps blades. The nucleus is then rotated, and the process is repeated at 90° to the original prechop to split the nucleus into four pieces.
This technique works well in the hands of Akahoshi, but the pressing of the prechopper into the nucleus leads to the risk of tearing the posterior capsule or dialyzing the zonules unless the surgeon has a very fine judgment of the amount of pressure that can be safely exerted. In this modification of the technique, the nucleus is first dislocated into the AC and then chopped from behind forward. Therefore, there is no pressure on the zonules. To prevent endothelial damage, a dialer or similar instrument is pressed into the nucleus from above, thus stabilizing it for the chop. Another semantic difference is that the Akahoshi technique is a prelude to phacoemulsification, so it is called a “prechop.” This technique is the core of the method itself, so it is better described as a “mechanical chop.” However, the terms coined by Akahoshi are used in this technique in deference to his earlier description of the basic method. Other surgeons have introduced minor variations of the technique.[3,4]
The technique is ideally suited for lateral incisions, both nasal and temporal. As most patients are old and already have some degree of against-the-rule astigmatism, the wound relaxation that invariably occurs with any incision in any technique here has the advantage of neutralizing the against-the-rule astigmatism, or in some cases, actually inducing a with-the-rule astigmatism.
No randomized, double-blinded study has been conducted by us, as the selection of cases, in clinical practice, itself negates the randomization process. However, we retrospectively looked at 20 consecutive cases each of phacoemulsification and MSICS, (unpublished data), and it was observed that the final astigmatism (not the induced astigmatism) was almost the same in both techniques. The final astigmatism averaged 0.46 diopter (D) for the cases treated by phacoemulsification and 0.45 D for the MSICS. The induced astigmatism is higher with this MSICS prechopping technique, but that can be turned to advantage when higher astigmatism preexists, giving a lower final astigmatism than that in phacoemulsification, in that case, by appropriately positioning the incision. Normally when data are presented, an effort is made to see that the data is randomized and free from bias. In the data we allude to, the purpose of the data is not research. It is to show how a skilful and willful clinical bias in case selection can yield excellent and similar results with two different techniques, by capitalizing on the properties of the different techniques. In these data, the fact that MSICS gives a higher induced cylinder was used to advantage by choosing it for those cases in which there was a higher preoperative cylinder, and positioning the incision to reduce the cylinder. The choice of technique in the clinical series from which our illustrative data were culled was thus not randomized but highly optimized (biased) to reduce the final astigmatism. The data do however give an idea of how effective this technique can be when appropriately tweaked. In a sense these data do not compare the astigmatism inducing properties of phacoemulsification and MSICS, but how appropriate clinical bias can be used to make them render equivalent results.
Please note that this is a MSICS (meaning that the incision size is about 5.5 to 6 mm). It is not ideally a sutureless technique, and the best results are obtained by taking one 10-0 suture to prevent wound slippage. The wound may be secure enough from the anatomical point of view even without a suture, but best astigmatic results mandate a suture. In the initial phase, when this technique was tried several years ago, about 10 cases were done without suture. None of them had the wound grossly opening out, but all except one had to have the corneal tunnel reopened and resutured after 2 weeks because of a high astigmatism (3-6 D). The average surgically induced astigmatism in this technique with one suture is about 0.75–1 D. In those cases with significant preexisting against-the-rule astigmatism, the technique may therefore give results superior to phacoemulsification with a foldable lens because of the possibility of neutralizing the preexisting astigmatism, by appropriately positioning the incision. In cases with no preexisting astigmatism, phacoemulsification with a foldable intraocular (IOL) would be superior, because of its lesser surgically induced astigmatism. As compared with phacoemulsifcation with a poly methyl metha acrylate (PMMA) lens, it seems logical to assume that if the incision size is similar (5.5 mm) to phacoemulsification with a PMMA lens, and execution is faster and has no incision location limitations, this technique may be considered superior. In fact, a right-handed surgeon can sit at the head end and make superior incisions, or nasal incisions (for the left eye), and temporal incisions(for the right eye), with equal facility.
In conclusion, this technique is a safe and effective way for atraumatic MSICS, with low postoperative astigmatism.
Footnotes
Nil
None declared.
References
- 1.Akahoshi T. The Karate Prechop technique. Cataract Refract Surg Today. 2002;2:63–4. [Google Scholar]
- 2.Akahoshi T. Phaco prechop: Manual nucleofracture prior to phacoemulsification. Op Tech Cataract Ref Surg. 1998;1:69–91. [Google Scholar]
- 3.Arleo RJ. Using Aqualase with Salvitti Akahoshi Prechop. Suppl Cataract Refract Surg Today. 2005:7–8. [Google Scholar]
- 4.Virgilio G, Alejandro T, Luis JE, Victor R, Angelica CM. Phaco Prechopping as an Option in High-Volume Cataract Services. Tech Ophthalmol. 2007;5:1–7. [Google Scholar]