Abstract
The authors here describe manual small incision cataract surgery (MSICS) by using topical anesthesia with intracameral 0.5% lignocaine, which eliminates the hazards of local anesthesia, cuts down cost and time taken for the administration of local anesthesia.
Aims
To evaluate the patients' and surgeons' experience in MSICS using topical anesthesia with intracameral lignocaine in terms of pain, surgical complications, and outcome.
Settings and Design
Prospective interventional case series.
Materials and Methods
Ninety-six patients of senile cataract were operated by MSICS under topical anesthesia with intracameral lignocaine using “fish hook technique.” The patients and the single operating surgeon were given a questionnaire to evaluate their experience in terms of pain, surgical experience, and complications.
Statistical Analysis Used
Statistical analysis software “Analyseit.”
Results
There were 96 patients enrolled in the study. The mean pain score was 0.7 (SD ± 0.97, range 0–5, median 0.0, and mode 0.0). Fifty-one patients (53%) had pain score of zero, that is, no pain. Ninety-one patients (˜95%) had a score of less than 3, that is, mild pain to none. All the surgeries were complication-free except one and the surgeon's experience was favorable in terms of patient's cooperation, anterior chamber stability, difficulty, and complications. The ocular movements were not affected, and hence, the eye patch could be removed immediately following the surgery.
Conclusions
MSICS can be performed under topical anesthesia with intracameral lignocaine, which makes the surgery patient friendly, without compromising the outcome.
Keywords: Anesthesia, intracameral lignocaine, pain evaluation, manual small incision cataract surgery, topical
Cataract is the main and biggest cause of curable blindness in India and worldwide. It has been estimated that there is a backlog created as 3.8 million people develop blinding cataract every year in India as against 2.7 million cataract surgeries done every year.[1,2] Cataract extractions is one of the most cost-effective of all surgical interventions[3,4] in terms of quality of life restored. The only treatment option for cataract is the surgical removal of the opaque lens and the implantation of an artificial lens. The state-of-the-art technique is phacoemulsification with the insertion of a foldable intraocular lens (IOL) through a self-sealing incision. The cost considerations and the steep learning curve associated with the phacoemulsification procedure make it an unsuitable procedure for high-volume surgery needed in developing countries. However, the manual small incision cataract surgery (MSICS) is the surgery of choice in such circumstances.[5]
The MSICS has been conventionally performed under peribulbar, retrobulbar anesthesia. Now there are some reports of the procedure being performed under subtenon and subconjunctival anesthesia too.[6] However, the difference between topical and these techniques remains palpable to the surgeon and the patients.
We here describe a topical anesthesia approach for performing MSICS. We have performed a pain evaluation survey on patients who underwent this procedure. This technique of MSICS under topical anesthesia with intracameral 0.5% lignocaine has not been described in literature yet.
Materials and Methods
The patients with significant cataract causing impairment of visual functions not correctable by glasses or with unacceptable glare, polyopia, or reduced quality of vision attributable to cataract and willing for cataract surgery were included in the study. Only contraindication was inability to understand verbal commands. Sensitivity to lignocaine was also an absolute contraindication to topical anesthesia.
Sample size was calculated by using confidence level of 95%, confidence interval of 10 and population size as 2000 (the total number of cataract surgeries at the hospital). This gave us a sample size of 92.
Ninety six patients were included in the study after performing tests and investigations for fitness for cataract surgery under local anesthesia. Cataract was classified according to the morphology, and the nuclear density was graded according to the slit lamp examination and standard photographs.
At the start of the surgery, the patients were instructed to hold the hand of the paramedical staff and to squeeze the hand whenever they felt pain, which was recorded together with the surgical step during which they felt pain.
Lignocaine 2% drops were instilled in the conjunctival sac 5 minutes before the surgery. The lids and periocular area were painted with povidone iodine 5% solution twice and the patient draped. Once fully draped, the eye speculum was inserted, and then, the 2% lignocaine viscous was generously poured on the exposed ocular surface. The patients usually reported a stinging sensation, but if instructed and advised to look towards the operating microscope light, brought the eye back in straight gaze. After waiting for about 1 minute, the surgery was started. No superior rectus suture was taken. Once the sclera was exposed, by making a fornix-based conjunctival flap, the blood vessels were cauterized, and a corneoscleral tunnel was designed. The incision length varied from 6 to 8 mm depending on the surgeon's assessment of the nucleus size. The entry into the anterior chamber was followed by intracameral injection of diluted 2% lignocaine (xylocaine, ASTRA IDL Ltd., India) solution, either commercially available preservative-free or regular 2% lignocaine injection diluted to 0.5% with Ringer's lactate solution. This concentration is safe for the corneal endothelium and provides adequate anesthesia to uveal tissue for pain-free surgery.[7–10] In our pain evaluation survey, we gave intracameral lignocaine to all the patients.
Then, 2% hydroxy propyl methyl cellulose was injected into the anterior chamber and capsulorrhexis was done. Hydrodissection was performed to separate the cortex from the capsule. Nucleus was prolapsed out of the capsular bag after making sure that the capsulorrhexis was large enough with respect to the nucleus size, otherwise a relaxing incision with a cystitome was made. With nucleus in the anterior chamber the chamber was inflated with 2% hydroxy propyl methyl cellulose, and the nucleus was extracted with the fish hook technique.[11] In case of a very soft nucleus, irrigating vectis was used. The nucleus was brought out of the tunnel with the support of a forceps holding the anterior lip of the tunnel to prevent the upward rotation of the globe. The cortex was aspirated using Simcoe cannula, and then, with the chamber filled with 2% hydroxy propyl methyl cellulose, an IOL was implanted in the bag. The gel was washed out and the tunnel was inspected for integrity by looking for any leakage. At the end of the surgery, a subconjunctival injection of dexamethasone and gentamycin was given (0.25 ml each). There was no need to suture the conjunctiva or to cauterize it to bring it back, as the ballooning caused by the subconjunctival injection made it to come anterior and drape the exposed sclera. The eye was patched for about 20–30 minutes, and then, the dressing was removed, eye was examined, and topical medications were started.
Before opening the dressing, a pain survey questionnaire having visual analog scale for pain evaluation or Wong scale for simplified version of pain evaluation was given to the patients depending on their ability to comprehend. The surgeon also evaluated his experience in terms of surgical ease or difficulty, complications with regards to the topical anesthesia at the end of the surgeries. The surgeon's evaluation was based on four parameters. Patient's cooperation, difficulty due to ocular movements, and anterior chamber stability were graded on a scale of 1–3, thus giving a cumulative range of 3–9 points. The questionnaire was designed to provide results in a manner that the lower values represent favorable experience. The fourth parameter was complications or adverse events, which were mentioned as and when they happened.
Results
There were 96 patients enrolled in the study according to the inclusion and exclusion criteria. Forty-six (47.9%) patients were male. Patients' age ranged from 38 to 78 years (mean age 64.2 years). Forty-one were the right eye and 55 left eye.
Type of cataract according to the morphology was nuclear in 36 patients (37.5%), nuclear and subcapsular in 42 patients (43.7%), and subcapsular in rest. Nuclear density ranged from grade I–V and correlated with age.
The pain experience during the surgical procedure was recorded as the patient's response by squeezing the hand of the operation theater assistant during the surgery. The patients felt pain when the viscoelastic was being injected before capsulorrhexis (3 patients), during the stretching of the wound while delivering the nucleus (4 patients), and during the irrigation aspiration procedure (4 patients).
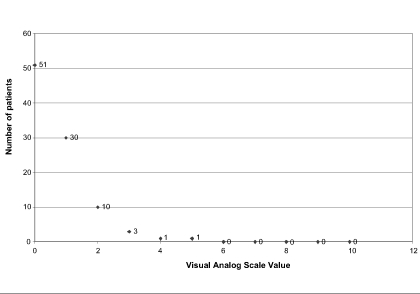
The visual analog scale or the Wong scale was used to evaluate the mean pain score. The mean pain score was 0.70 (SD ±0.97, range 0-5). Only five patients (˜5%) out of the whole series experienced pain who rated more than three on the visual analog scale of 10. The pain scores more than three has been accepted to represent moderate pain.[12,13] Thus, rest of the patients can be assumed to have mild pain. There were 91 patients (˜95%) who had a mean pain score of two or less. Fifty-one patients (53%) had pain score of zero that is no pain [Fig. 1].
Figure 1.
Frequency distribution of visual analog scale response of patients undergoing cataract surgery under topical anesthesia
The surgeon's evaluation of the technique in terms of surgical ease and complications was favorable. On a cumulative scale ranging from 3 to 9 (lower value indicating favorable result), the average score was 3.4 (SD ±0.85). Table 1 for frequency distribution of individual parameters taken into account.
Table 1.
Frequency distribution of surgeon's score for surgical experience during MSICS under topical anesthesia (n = 96)
| Surgeon's score | Patient cooperation | Unwanted ocular movements | Anterior chamber stability |
|---|---|---|---|
| 1 | 84 | 80 | 92 |
| 2 | 10 | 13 | 0 |
| 3 | 2 | 3 | 4 |
Lower score indicates favorable experience
Only one patient had a small zonular dehiscence, which did not relate to the anesthesia technique, but it was because of small capsulorrhexis during the insertion of the IOL.
Discussion
The use of topical anesthesia has been described with the supplemented subconjunctival anesthesia for standard extracapsular cataract extraction with the implantation of IOL by Smith way back in 1990.[14] The described use of topical anesthesia is presently limited to clear corneal phacoemulsification technique. The advantages are numerous, for the patients as well as for the surgeon. Topical anesthesia saves the patients from the risks of globe perforations, optic nerve injury, possibility of life-threatening respiratory arrest,[15] and above all, the pain and fear perceived because of the peribulbar or retrobulbar injections.
Topical anesthesia has additional benefits like not interfering with visual function, immediate visual recovery, absence of pain due to injection, unlimited ocular motility, and absence of an increase in orbital volume.[16] Various studies regarding the pain perception and patients' acceptability for anesthetic technique have been done and they concluded that the patients' satisfaction for anesthesia is comparable for topical versus other techniques.[17–20]
Besides the patients' subjective appreciation of pain during surgery, which may be limited by their tolerance and expression, there are studies which have investigated the various physiological and biochemical parameter changes during the surgery under topical anesthesia. Fichman has investigated the blood pressure, pulse rate, and respiration rate of patients during surgery under topical anesthesia and has found no major changes in these parameters.[21] There is no significant change in the plasma cortisol levels during surgery under topical anesthesia, indicating that the procedure is well tolerated and does not pose stress to the patient.[22] Thus, with all the advantages of topical anesthesia, it may be the preferred technique.[17–20]
Lignocaine gel has been previously shown to be an effective,[23,24] and possibly, a superior[25,26] substitute to lignocaine drops. There has been no unwanted effect of the gel preparation of the drug on extracapsular cataract surgery and phacoemulsification; both have been successfully performed using the 2% lignocaine jelly.
In this study, the mean pain score of 0.70 (SD ±0.97, range 0–5) is comparable to the studies done on topical anesthesia use for phacoemulsification. The mean pain score of 0.84 (SD ±1.30, range 0–7) against peribulbar anesthesia 0.73 (SD ±1.5, range 0–5) was seen in a study done by Philipp, using 2% lignocaine drops.[27] Similar results have been observed with the use of lignocaine 2% jelly for providing topical anesthesia for phacoemulsification for cataract removal in various other studies.[23–26] The mean pain score in the present study was similar to the mentioned studies for the topical group, except that none of the patients in our studies needed subtenon lignocaine supplementation as was required by some patients in all the mentioned studies.
Topical anesthesia is used to anesthetize conjunctiva and sclera for several procedures like scleral indentation, forced duction test, subconjunctival injections, pterygium surgery,[28] and cryoapplication for retinal cryopexy. Thus, topical anesthesia is effective and safe for manipulating conjunctiva and sclera as well. This fact has been utilized and demonstrated well in our study, where the pain experience of the patients has been comparable to that during phacoemulsification performed under topical anesthesia reported in other studies.
A pain evaluation study comparing the delivery of prechopped nucleus through a clear corneal incision and phacoemulsification through clear corneal incision using topical anesthesia has shown that the perioperative pain is significantly higher in the prechop method.[29] The authors had used benoxenate hydrochloride 0.5% drops. The pain experienced by the patients during cataract surgery under topical anesthesia is during the steps when there is stretching of the eye ball. Similar opinion has been expressed by Philipp et al., regarding the cause of pain in topical anaesthesia.[27]
The clear corneal approach for MSICS has the problem that an attempt to keep the incision size small, so that it is self-sealing will cause stretching of the wound during delivery of the nucleus and will cause pain leading to unacceptability by patients. In this study, we have used 2% lignocaine gel in place of drops, as the gel formulation is superior in providing anesthesia.[23,24] Second, as we have used sclerocorneal tunnel, the wound length could be increased to accommodate a larger nucleus, and hence, less stretching and less pain was experienced by the patient. The use of fish hook technique[11] could be preferable over irrigating vectis because the later technique tends to increase the intraocular pressure. Hence, the combination of lignocaine viscous, sclerocorneal tunnel, and use of fish hook is helpful in performing painless MSICS under topical anesthesia.
Surgeon's evaluation of the technique has been favorable as demonstrated by the fact that patients' cooperation was good in majority of cases (87.5%). In most of the patients, there were no unwanted eye movements (83%). With topical anesthesia, there is no rise in intraocular pressure as compared with peribulbar anesthesia. This is because the placement of 5 ml of anesthetic cocktail in the orbit increases the intraocular pressure. Thus, even without the use of ocular pressure, the anterior chamber stability is good in topical anesthesia.
Thus, combining MSICS with topical anesthesia with intracameral 0.5% lignocaine makes cataract management better in every respect.
This study however has its own limitations. Being a noncomparative study, conclusive evidence of superiority of topical anesthesia over local anesthesia for MSICS is not available. The surgeries were done by a single surgeon; this arrangement might have omitted differences induced by variations in the surgical technique and skill. These limitations can be overcome by performing a prospective comparative study involving multiple centers and surgeons.
Conclusions
It is possible to perform MSICS under topical anesthesia with the use of 2%lignocaine jelly and 0.5% intracameral lignocaine. The anesthesia achieved is adequate for patient comfort and safe cataract surgery.
Surgeon's questionnaire for evaluating surgical experience during MSICS under topical anesthesia.
| Name: | Age | Sex | |||
| Surgery | Anesthesia | Date | |||
| Operating Surgeon | |||||
| 1 | 2 | 3 | |||
| Patient cooperation | Excellent | Good | Poor | ||
| Difficulty due to ocular movements | None | Some | Great diff. | ||
| Anterior chamber stability | Excellent | Good | Poor | ||
| Complications | None | yes (mention) |
Pain evaluation form for cataract surgery under topical anesthesia.
| Name: | Age | Sex |
| Surgery | Anesthesia | Date |
| Time | ||
| Delivered by |
Footnotes
Nil
None declared.
References
- 1.Minasian DC, Mehera V. 3.8 Milion blinded by cataract each year: Projections of the first epidemiological study of incidence of cataract blindness in India. Br J Ophthalmol. 1990;74:341–3. doi: 10.1136/bjo.74.6.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jose R. National programme for the control of blindness. Indian J Comm Health. 1997;3:5–9. [Google Scholar]
- 3.Marseille E. Cost-effectiveness of cataract surgery in a public health eye care program in Nepal. World Health Organ Bull OMS. 1996;74:319–24. [PMC free article] [PubMed] [Google Scholar]
- 4.Porter R. Global initiative: The economic case. Commun Eye Health. 1998;27:44–5. [PMC free article] [PubMed] [Google Scholar]
- 5.Chang DF. Tackling the greatest challenge in cataract surgery. Br J Ophthalmol. 2005;89:1073–7. doi: 10.1136/bjo.2005.068213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parkar T, Gogate P, Deshpande M, Adenwala A, Maske A, Verappa K. Comparison of subtenon anaesthesia with peribulbar anaesthesia for manual small incision cataract surgery. Indian J Ophthalmol. 2005;53:255–9. doi: 10.4103/0301-4738.18907. [DOI] [PubMed] [Google Scholar]
- 7.Shah AR, Diwan RP, Vasavada AR, Keng MQ. Corneal endothelial safety of intracameral preservative-free 1% xylocaine. Indian J Ophthalmol. 2004;52:133. [PubMed] [Google Scholar]
- 8.Heuermann T, Hartmann C, Anders N. Long-term endothelial cell loss after phacoemulsification: Peribulbar anesthesia versus intracameral lidocaine 1%. Prospective randomized clinical trial. J Cataract Refract Surg. 2002;28:639–43. doi: 10.1016/s0886-3350(01)01216-0. [DOI] [PubMed] [Google Scholar]
- 9.Pandey SK, Werner L, Apple DJ, Agarwal A, Agarwal A, Agarwal S. No-anesthesia clear corneal phacoemulsifi-cation versus topical and topical plus intracameral anesthesia: Randomized clinical trial. J Cataract Refract Surg. 2001;27:1643–50. doi: 10.1016/s0886-3350(01)00793-3. [DOI] [PubMed] [Google Scholar]
- 10.Karp CL, Cox TA, Wagoner MD, Ariyasu RG, Jacobs DS. Intracameral anesthesia: A report by the American Academy of Ophthalmology. Ophthalmology. 2001;108:1704–10. doi: 10.1016/s0161-6420(01)00793-x. [DOI] [PubMed] [Google Scholar]
- 11.Hennig A, Kumar J, Singh AK, Ansari A, Singh S, Gurung R, Foster A. World Sight Day and cataract blindness. Br J Ophthalmol. 2002;86:830–1. doi: 10.1136/bjo.86.7.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain. 1997;72:95–7. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Stiell I, Hobden E, Wells G. Clinically meaningful values of the visual analog scale of pain severity. Acad Emerg Med. 2000;7:550. [Google Scholar]
- 14.Smith R. Cataract extraction without retrobulbar anesthetic injection. Br J Ophthalmol. 1990;74:205–7. doi: 10.1136/bjo.74.4.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eke , Tom , Thompson , John R. Serious complications of local anaesthesia for cataract surgery: A 1 year national survey in the United Kingdom. Br J Ophthalmol. 2007;91:470–5. doi: 10.1136/bjo.2006.106005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nielsen PJ. Immediate visual capability after cataract surgery: Topical versus retrobulbar anesthesia. J Cataract Refract Surg. 1995;21:302–4. doi: 10.1016/s0886-3350(13)80137-x. [DOI] [PubMed] [Google Scholar]
- 17.Nielsen PJ. A prospective evaluation of anxiety and pain with topical anesthesia or retrobulbar anesthesia for small incision cataract surgery. Eur J Implant Ref Surg. 1995;7:6–10. [Google Scholar]
- 18.Maclean H, Burton T, Murray A. Patient comfort during cataract surgery with modified topical and peribulbar anesthesia. J Cataract Refract Surg. 1997;23:277–83. doi: 10.1016/s0886-3350(97)80354-9. [DOI] [PubMed] [Google Scholar]
- 19.Zehetmayer M, Radax U, Skorpik C, Menapace R, Schemper M, Weghaupt H, et al. Topical versus peribulbar anesthesia in clear corneal cataract surgery. J Cataract Refract Surg. 1996;22:480–4. doi: 10.1016/s0886-3350(96)80046-0. [DOI] [PubMed] [Google Scholar]
- 20.Johnston RL, Whitefield LA, Giralt J, Harrun S, Akerele T, Bryan SJ, et al. Topical versus peribulbar anesthesia, without sedation, for clear corneal phacoemulsification. J Cataract Refract Surg. 1998;24:407–10. doi: 10.1016/s0886-3350(98)80332-5. [DOI] [PubMed] [Google Scholar]
- 21.Fichman RA. Use of topical anesthesia alone in cataract surgery. J Cataract Refract Surg. 1996;22:612–4. doi: 10.1016/s0886-3350(96)80019-8. [DOI] [PubMed] [Google Scholar]
- 22.Gozum N, Altan-Yaycioglu R, Gucukoglu A, Arslan O. Does topical anesthesia increase patient's serum cortisol level? Int J Ophthalmol Visual Sci. 2003;2:2. [Google Scholar]
- 23.Barequet IS, Soriano ES, Green WR, O'Brien TP. Provision of anaesthesia with single application of lidocaine 2% gel. J Cataract Refract Surg. 1999;25:626–31. doi: 10.1016/s0886-3350(99)00004-8. [DOI] [PubMed] [Google Scholar]
- 24.Assia EI, Pras E, Yehezkel M, Rotenstreich Y, Jager-Roshu S. Topical anesthesia using lidocaine gel for cataract surgery. J Cataract Refract Surg. 1999;25:635–9. doi: 10.1016/s0886-3350(99)00026-7. [DOI] [PubMed] [Google Scholar]
- 25.Bardocci A, Lofoco G, Perdicaro S, Ciucci F, Manna L. Lidocaine 2% gel versus lidocaine 4% unpreserved drops for topical anesthesia in cataract surgery: A randomized controlled trial. Ophthalmology. 2003;110:144–9. doi: 10.1016/s0161-6420(02)01562-2. [DOI] [PubMed] [Google Scholar]
- 26.Soliman MM, Macky TA, Samir MK. Comparative clinical trial of topical anesthetic agents in cataract surgery: Lidocaine 2% gel, bupivacaine 0.5% drops, and benoxinate 0.4% drops. J Cataract Refract Surg. 2004;30:1716–20. doi: 10.1016/j.jcrs.2003.12.034. [DOI] [PubMed] [Google Scholar]
- 27.Jacobi PC, Dietlein TS, Jacobi FK. A comparative study of topical vs. Retrobulbar anaesthesia in complicated cataract surgery. Arch Ophthalmol. 2000;118:1037–43. doi: 10.1001/archopht.118.8.1037. [DOI] [PubMed] [Google Scholar]
- 28.Oksuz H, Tamer C. Efficacy of lidocaine 2% gel in pterygium surgery. Acta Ophthalmol Scand. 2005;83:206–9. doi: 10.1111/j.1600-0420.2005.00404.x. [DOI] [PubMed] [Google Scholar]
- 29.Kongsap P, Wiriyaluppa C. A comparison of patient pain during cataract surgery with topical anesthesia in prechop manual phacofragmentation versus phacoemulsification. J Med Assoc Thai. 2006;89:959–66. [PubMed] [Google Scholar]