Many readers of HEPATOLOGY will recall January 1st, 2000 as a New Year’s day that was mildly surprisingly much like any other. The old millennium had ended with a fizzle. In addition to a tedious debate about whether 1999 was the technical end of the millennium, the months leading up to January 1st, 2000 were remarkable for the variably apocalyptic predictions of the impact of the Millenium (or Y2K) Bug. The Millenium Bug arose from a spectacularly penurious quirk of early computer program design that had resulted in software that, in an attempt to save memory, identified years by two digits rather than four (presumably the same individuals who abbreviated June to JUN). The year 2000 would thus be represented by 00 and might be interpreted by software as the year 1900. It is hard to overstate the dire nature of some of the projected consequences of Y2K, which included nuclear Armageddon. The United States Deputy Secretary of Defense, John Harme, chillingly predicted that Y2K would result in “nasty surprises around the globe,” while reassuring the public that 93% of “mission critical” defense systems were Y2K compliant (Looking at the Y2K bug, portal on CNN.com). Genetically a skeptic, I took out an extra $100 from the bank and pocketed two aspirin but otherwise made no special arrangements for January 1st, 2000. We all know the outcome. A sprinkling of innocuous software failures and a Global pandemic of simultaneous schadenfreude and relief was all the world had to show for the billions that had been spent on Y2K preparedness. Is the clinical impact of non-alcoholic fatty liver disease the Y2K of our specialty? Have we fashioned a mountain from a molehill of end-stage liver disease? The answer merits some consideration.
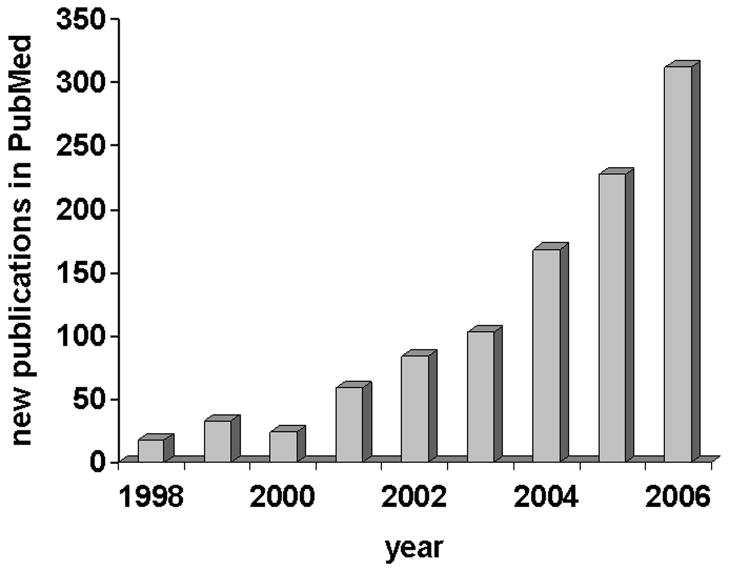
There is no important debate regarding the prevalence of NAFLD and NASH. Ian Wanless’s landmark autopsy-based cross-sectional study reported convincingly that the overall prevalence of NASH in adults in North America is 18.5% in obese and 2.7% in non-obese individuals.(1) Of obese individuals found to have NASH at autopsy, about one in seven had bridging fibrosis or cirrhosis. Based on current prevalences of obesity and type 2 diabetes, nonalcoholic fatty liver disease can conservatively be estimated to affect over 30 million people in the United States.(2–8) NAFLD has thus come to be regarded as a potentially important public health issue. The scale of the problem may be worsening in parallel with the relentless increases in the prevalence and severity of obesity in the United States and globally. Our communal interest in NAFLD is reflected in the number of publications that have appeared in the medical literature (Figure). A simple query of PubMed using the subject search terms NAFLD or NASH reveals a logarithmic increase in the number of NAFLD-related articles in the last ten years. State-of-the-Art NAFLD presentations have become a staple at annual meetings for the American Association for the Study of Liver Diseases and the American Gastroenterology Association, each offering up a Eureka! insight into the pathophysiology of this condition, from macrophage dysfunction to lipotoxicity, that have gradually increased our understanding of the biology of this condition. Yet despite the overwhelming evidence regarding the prevalence of NAFLD and NASH and a clutch of reports describing end-stage liver disease in NAFLD,(9, 10) there is an emerging sense that we may have oversold the clinical importance of NAFLD. A January 1st, 2000 post-Y2K feeling. Intense scientific interest and a flurry of publications do not always equate to significance (witness TT-virus and hepatitis G). The missing piece here is a well-conducted, large natural history cohort study of NAFLD. Given the need for histology to characterize NAFLD and the risk and expense associated with liver biopsies, such a study is unlikely to ever occur. Other potential sources of clues to the clinical impact of NAFLD might include the United Network for Organ Sharing (UNOS) and the National Health and Nutrition Education Survey (NHANES). While UNOS can provide accurate nodal data concerning transplant recipients (alive or dead, retransplanted etc.), other aspects of recipient information are plagued by unreliability and incompleteness. When entering diagnoses for liver transplant recipients at the time of listing, for example, only primary diagnosis is recorded and, until recently, NASH or NAFLD was not among the seventy available choices. Curiously, there has been room on the UNOS drop down list for several primary diagnoses that I have never seen among patients as an indication for transplantation. There are no less than four subgroups for PSC. The situation may be worse for cryptogenic cirrhosis, a likely alternative primary diagnosis for patients with cirrhosis due to NAFLD. Nurse coordinators or administrative assistants who enter this data would have to select “cirrhosis cryptogenic” rather than four other similar choices: “choles liver disease other”, “cirrhosis chronic active hepatitis etiology unknown”, “cirrhosis other specify” and “other specify”. Good luck! NASH now appears on the drop down list of primary diagnoses as “cirrhosis fatty liver (NASH)”. Even when this primary diagnosis is selected there are no criteria required for doing so, making the accuracy of the diagnosis unknowable. With those caveats in mind, it would seem to be hardly worth asking UNOS for data regarding the frequency of NAFLD as a primary diagnosis. Yet a report of such a query was published in Liver Transplantation, yielding some intriguing observations.(11) One of the most striking was that there had been a 35-fold(!) increase in the frequency of NAFLD as a primary diagnosis between 2001 and 2005. Most or all of that increase, however, is likely to have been attributable to the addition of NAFLD/NASH as a choice on the list of primary diagnoses in 2004, when the spike in NAFLD/NASH as a primary diagnosis occurred (from an n of 26 to 128). A more reliable index is probably the combined frequency of cryptogenic cirrhosis and NAFLD/NASH. This combination of primary diagnoses has increased from 3.6 to 6.9% in the five years between 2001 and 2005. Even this is likely to be an underestimate as patients with a hepatocellular carcinoma occurring on a background of cryptogenic cirrhosis or NAFLD will not be included as only the primary diagnosis (HCC in these cases) is recorded by UNOS at the time of listing for liver transplantation. A reasonable estimate would be that NAFLD is currently the underlying cause of liver disease in between 5–10% (n=~325–650 recipients, based on 2006 liver transplant volume (http://www.ustransplant.org/)). A notable number but not a catastrophic one. The rate of increase in liver transplantation is in keeping with earlier projections that may well see NAFLD overtake HCV as the most common primary diagnosis of liver failure in liver transplant recipients by 2020. The frequency of HCV as an indication for liver transplantation peaked in 2002 at 28% in the USA and has declined every year since with most recent frequency of 23% (http://www.ustransplant.org/).
Figure 1.
Number of original publications per year, using the search terms NAFLD and NASH, is shown.
Are there patients with NAFLD dying from liver-related causes that never make it to transplantation? Without doubt, although we can only guess how many. In lieu of a population based study, the best potential source of information regarding the frequency of NAFLD as a cause of end-stage liver disease may be the third National Health and Nutrition Survey (NHANES III). Three groups have studied the NHANES III regarding NAFLD.(8, 12, 13) The prevalence of unexplained elevations in ALT was 7% in individuals with the metabolic syndrome and 3.5% in those without the metabolic syndrome. As many patients with NAFLD have normal ALT, these frequencies almost certainly underestimate the actual frequency of NAFLD. And, more importantly, they tell us nothing about the frequency of liver related deaths. In a community population-based study, the absolute risk of death from NAFLD appeared to be low, with a reported standardized mortality ratio of 1.34 (95% CI, 1.003–1.76; P=0.03).(14) Extrapolating these numbers, of 100 patients diagnosed with NAFLD, five will develop cirrhosis, and three will develop liver-related complications (e.g. hepatocellular carcinoma) within 10 years. With a current projected prevalence of NAFLD in the USA of ~30 million, this would produce 90,000 patients per year with end-stage liver disease due to NAFLD. Many of these 90,000 patients/yr will have strong relative or absolute contraindications to liver transplantation due to other complications of the metabolic syndrome and obesity. The frequency of end-stage liver disease due to NAFLD thus may be less than we expected but still substantial. Of course, I’m just guessing, using the best data I can find. A plea for better data is, ultimately my reason for penning this article. If you have such data, HEPATOLOGY is eager to hear from you. We can assure you a fair and expeditious review. Otherwise, we will again be watching the clock for the New Year. In this case we will be waiting for 2020 to find out if NAFLD is the real Millenium Bug, King of the Indications for Liver Transplantation, depleter of organs and taker of life. Or not so much.
References
- 1.Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–1110. doi: 10.1002/hep.1840120505. [DOI] [PubMed] [Google Scholar]
- 2.Angulo P. Nonalcoholic fatty liver disease.[comment] [Review] [95 refs] 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 3.Charlton M. Nonalcoholic fatty liver disease: a review of current understanding and future impact. 2004 doi: 10.1016/s1542-3565(04)00440-9. [Review] [117 refs] [DOI] [PubMed] [Google Scholar]
- 4.Noel M, Hickner J, Ettenhofer T, Gauthier B. The high prevalence of obesity in Michigan primary care practices. An UPRNet study. Upper Peninsula Research Network. Journal of Family Practice. 1998;47:39–43. [PubMed] [Google Scholar]
- 5.Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little Rr, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988–1994 [see comments] Diabetes Care. 1998;21:518–524. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM. The obesity epidemic in children and adults: current evidence and research issues. 1999;31(Suppl–14) doi: 10.1097/00005768-199911001-00004. [Review] [47 refs] [DOI] [PubMed] [Google Scholar]
- 7.Popkin BM, Udry JR. Adolescent obesity increases significantly in second and third generation U.S. immigrants: the National Longitudinal Study of Adolescent Health. Journal of Nutrition. 1998;128:701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- 8.Fraser A, Longnecker MP, Lawlor DA. Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999–2004. Gastroenterology. 2007;133:1814–1820. doi: 10.1053/j.gastro.2007.08.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charlton M, Kasparova P, Weston S, Lindor K, Maor-Kendler Y, Wiesner RH, Rosen CB, et al. Frequency of nonalcoholic steatohepatitis as a cause of advanced liver disease. 2001;7:608–614. doi: 10.1053/jlts.2001.25453. [DOI] [PubMed] [Google Scholar]
- 10.Kim WR, Poterucha JJ, Porayko MK, Dickson ER, Steers JL, Wiesner RH. Recurrence of nonalcoholic steatohepatitis following liver transplantation. Transplantation. 1996;62:1802–1805. doi: 10.1097/00007890-199612270-00021. [DOI] [PubMed] [Google Scholar]
- 11.Angulo P. Nonalcoholic fatty liver disease and liver transplantation. 2006;12:523–534. doi: 10.1002/lt.20738. [Review] [97 refs] [DOI] [PubMed] [Google Scholar]
- 12.Liangpunsakul S, Chalasani N. Unexplained elevations in alanine aminotransferase in individuals with the metabolic syndrome: results from the third National Health and Nutrition Survey (NHANES III) Am J Med Sci. 2005;329:111–116. doi: 10.1097/00000441-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003;98:960–967. doi: 10.1111/j.1572-0241.2003.07486.x. [DOI] [PubMed] [Google Scholar]
- 14.Adams LA, Lymp JF, St S, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. [see comment] 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]