ALTHOUGH all of the first attempts at orthotopic liver transplantation in man resulted in the early death of the recipient, after 23 days or less, the experience gained since the summer of 1967 has established the fact that this procedure can prolong life in patients dying of hepatic disease (10, 12, 13). Nevertheless, the operation has proved to be an exceptionally hazardous one, not only because of technical difficulties in its performance but also because of a number of complications which have been seen later. In this article, attention will be directed to these unsatisfactory aspects of orthotopic liver transplantation, to a consideration of how improvements might be made, and to a description of the histologic features of hepatic homografts, studied from a few hours to more than a year postoperatively.
CLINICAL OBSERVATIONS
Survival Statistics
Since 23 July 1967, 14 patients have undergone orthotopic liver transplantation. Five of the recipients are still alive after eight and one-half, seven, six, five, and three months. The other recipients died one-half, one, four, 35, 60, 105, 133, 186, and 400 days postoperatively.
Recurrent Carcinoma
The four patients in whom the indication for transplantation was hepatoma all survived operation and had at least a brief period of untroubled convalescence. The tumor was thought, in advance, to be confined to the liver in each instance. One of the recipients, a 24 year old woman, died 35 days postoperatively of pneumonitis caused by Pseudomonas aeruginosa. At autopsy, metastases were not detectable.
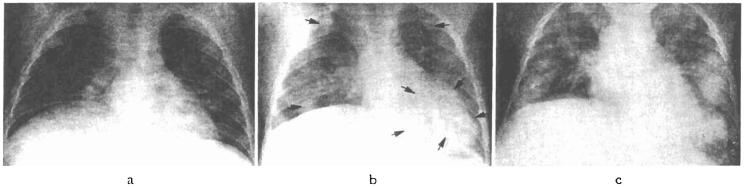
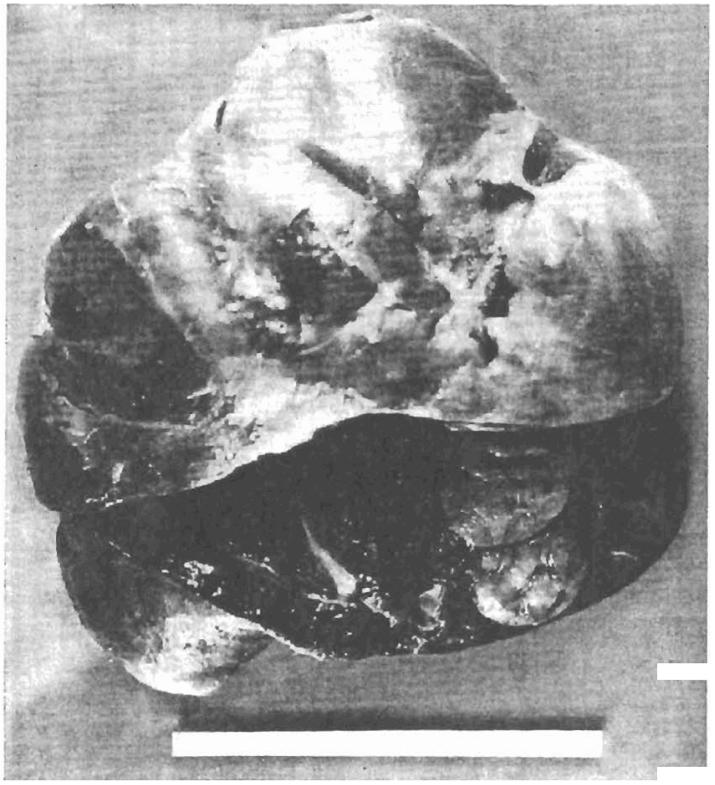
The other three patients lived for a long enough period to permit meaningful observations on the behavior of the malignant lesions. The longest surviving recipient in the series was a 19 month old female, in whom the diagnosis of hepatoma was made six months before transplantation. At operation, there was no evidence of extrahepatic metastasis, although gross tumor was present in the larger hepatic veins. However, three months later, multiple nodules appeared in both lungs (Fig. 1a and b). These rapidly progressed in size (Fig. 1c), despite chemotherapy with vincristine sulfate (Oncovin®). A short time later, bulky metastases developed in the abdomen, which caused bilateral ureteral obstruction, obstruction of the sigmoid colon, and compression of the cholecystoduodenostomy used for homograft biliary drainage. Multiple decompressing procedures were performed for palliation during the last ten months of life. Ultimately, intracranial metastases were responsible for seizures and, finally, coma. She died 400 days postoperatively. At autopsy, it was found that the carcinomatosis involved even the homograft. Two large nodules were found in close relation to portal vein radicles within the transplanted liver (Fig. 2).
Fig. 1.
Roentgenograms of the chest of a 19 month old child, who was treated with orthotopic liver transplantation for the indication of hepatoma. a, Preoperative study. Elevation of the right side of the diaphragm was caused by the marked hepatomegaly. b, Multiple pulmonary metastases as seen seven months after transplantation. Evidence of the spread had first been detected in the third postoperative month. c, Massive pulmonary metastases at one year. The child died of carcinonatosis 400 days after trasplantation.
Fig. 2.
Liver homograft obtained at autopsy, 400 days after transplantation. Note the two large metastatic nodules in the superior portion of the right lobe.
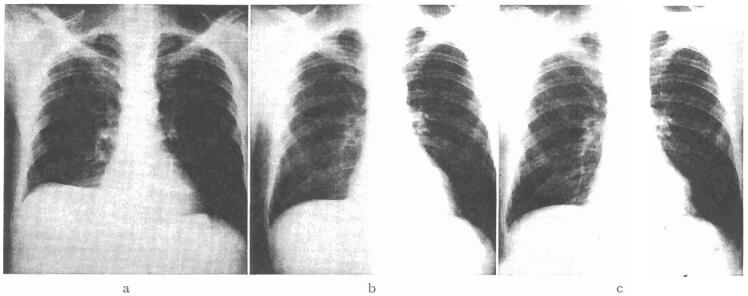
Two patients are still alive after liver replacement for hepatoma. In both, gross tumor was found in the major hepatic veins of the diseased organs at transplantation. One of the recipients, a 42 year old man, has perfect liver function six months postoperatively, but roentgenographically bilateral pulmonary metastases are evident (Fig. 3). The other patient, a 16 year old girl, does not as yet have a demonstrable recurrence of cancer, after seven months.
Fig. 3.
Roentgenograms of the chest of a 42 year old man who received an orthotopic liver transplantation on 14 April 1968. The indication for operation was hepatoma. a, Ten days postoperatively. b, Eighty days postoperatively. A tiny nodule, arrow, was detected in the right lung. c, Two months later, the nodule had perceptibly increased in size and other fine metastatic deposits appeared in both lungs.
Vascular Catastrophes
After clinical renal transplantation, the incidence of thrombosis of the major vessels or their branches has been extremely low. In contrast, in seven of the last 14 recipients of orthotopic liver homografts occlusive clots have developed in part of the homograft blood supply, and in another recipient, a nonthrombotic arterial obstruction developed.
Lobar arterial thrombosis
In earlier publications (12, 13), the distinctive complication of right hepatic arterial thrombosis was described in four of the first six patients in this series. The recipients, all children, became acutely febrile two to 100 days after transplantation, had high increases in the serum transaminase values, suffered from gram-negative septicemia as the necrotic tissue was invaded by enteric microorganisms, and were shown, by liver scans, to have areas of decreased radioisotope uptake in the central or right lobar portions of the homografts. Two of the four children died within a few days; the other two were temporarily saved by débridement procedures but ultimately died within from four to six months. Evidence was later obtained that distortion of the right hepatic artery could be caused by the kind of downward and medial rotation of the right lobe, which occurred if the suspensory ligaments of the liver were not re-attached (13). The falciform and triangular ligaments of the homograft were sutured to the companion structures in subsequent recipients. Regional hepatic gangrene was not seen again.
Total arterial thrombosis
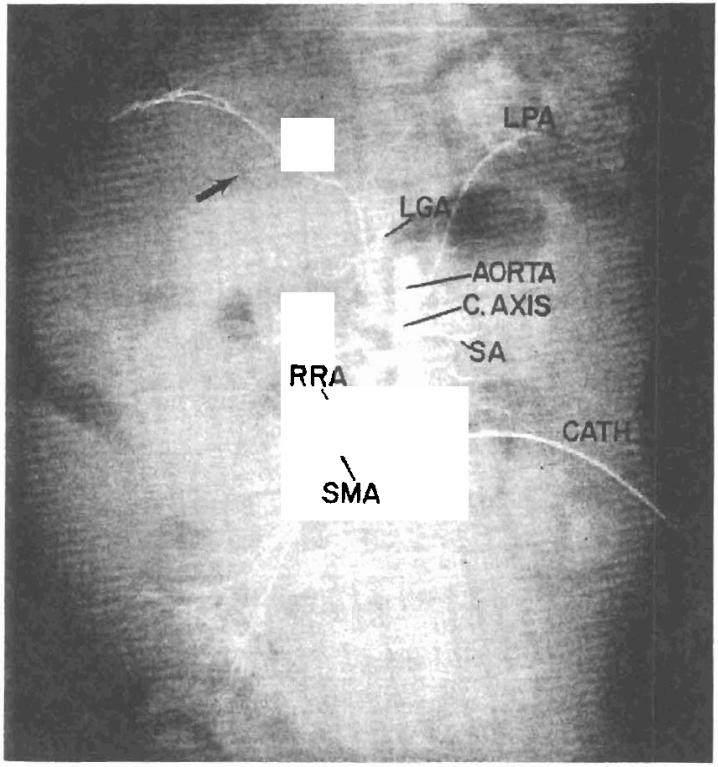
A fifth patient, among the first six, apparently also had a thrombosis of the right hepatic artery but survived for more than a year, only to eventually die of widespread metastases from the hepatoma for which she was originally treated. Atautopsy, 400 days postoperatively, an angiogram showed that the left hepatic arterial branch had also closed, probably at a later time. The celiac axis was patent to the origin of the splenic artery, but the common and proper hepatic arteries were absent (Fig. 4). The only demonstrable arterial supply to the homograft came from the right phrenic artery. It is of interest that a patient of Birtch and Moore also survived for more than a month after complete dearterialization of an orthotopic liver homograft, with little or no deterioration of hepatic function.
Fig. 4.
Postmortem aortogram obtained 400 days after orthotopic liver transplantation. Note that no hepatic arterial supply is demonstrable. C. AXIS, celiac axis: LGA, left gastric artery; LPA, left phrenic artery; RPA, right phrenic artery; RRA, right renal artery; SA, splenic artery; SMA, superior mesenteric artery.
Acute hepatic arterial insufficiency cannot usually be expected to have such benign consequences, and this was illustrated by the early death of two other children, who have been previously described (10). In one, the common hepatic artery thrombosed within a few hours after operation, and in the other, the same vessel was apparently compressed by the caudate lobe of the homograft, which had been obtained from an excessively large donor. Arterial insufficiency developed in the homograft, even though the vessel did not clot.
Portal vein thrombosis
Another eight year old child died less than a day after orthotopic transplantation as the result of complete clotting of the portal venous anastomosis. The vascular reconstruction had been complicated by a size disparity of the homograft and host portal veins as well as by an anomaly of the host arterial system. The technical details have been discussed previously (10).
The influence of size
The eight foregoing vascular accidents occurred in 11 pediatric patients. The ages of those who suffered right lobar dearterialization ranged from 13 to 21 months. Those in whom the total arterial or portal venous supply became obstructed were one to eight years of age. In contrast, the three adults, who were 16 to 42 years of age, did not have any similar complications.
A second association was also noted. Of the 14 patients, there were six in whom the sizes of the donor and recipient were approximately equal, one in whom the donor was only two-thirds the weight of the recipient, and seven in whom the donor weighed from 1.5 to 2.3 times as much as the recipient. All of the patients in the first two categories lived for at least five weeks postoperatively. Three of the seven in the third group had an early death from total occlusion of the hepatic artery or portal vein. The significance of these findings was obscured by the fact that anomalies of the recipient hepatic arteries complicated the operations, as has been reported elsewhere (10), in two of the three technically unsuccessful operations.
Late Rejection
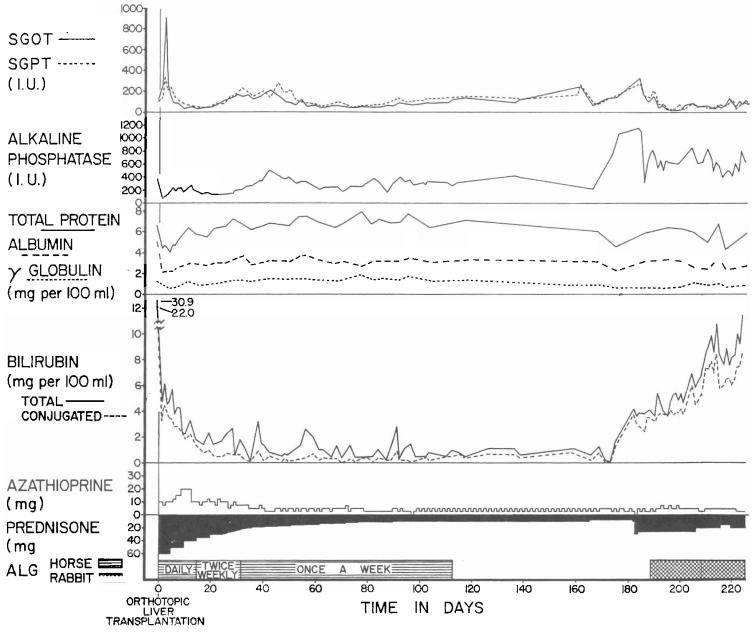
Immunosuppressive therapy, in all of these patients, was with azathioprine, prednisone, and horse antilymphocyte globulin. The first two agents were administered indefinitely in variable doses. Treatment with horse globulin was ultimately discontinued in all but two of the long-surviving patients, either because the end of the arbitrary four month period of administration had been reached (Fig. 5) or because there was serologic or clinical evidence of increasing sensitization to the injected foreign protein.
Fig. 5.
Course of a two year old child who received the liver of a 33 month old cadaveric donor. Liver function was excellent and stable for many postoperative months. About two months after horse antilymphocyte globulin, ALG, was discontinued, an indolent late rejection began. The changes in serum enzymes were partially reversed by intensification of immunosuppressive therapy, but the bilirubin has remained high. SGOT, serum glutamic oxalacetic transaminase; SGPT, serum glutamic pyruvic transaminase; I.U., international unit.
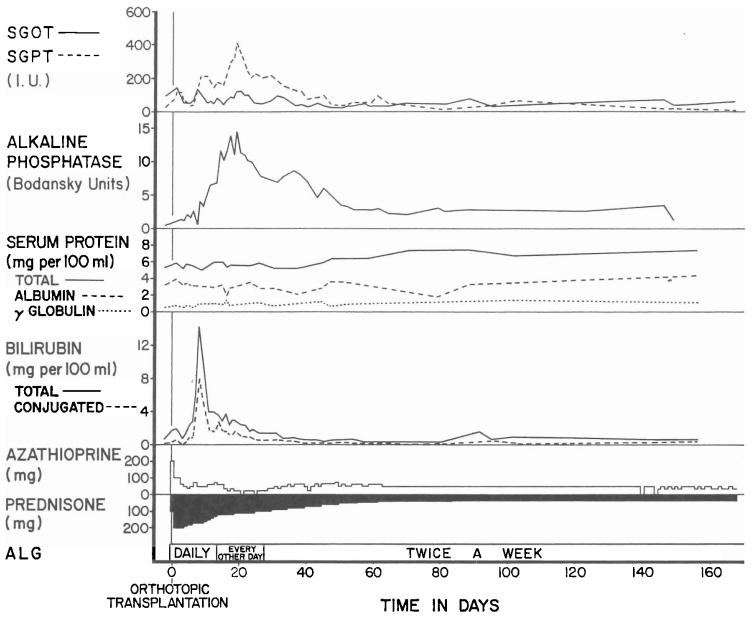
Eleven recipients did not die of vascular accidents in the immediate postoperative period, and they were studied for a minimum interval of at least five weeks. Ten of these patients passed through an early rejection crisis. However, the process was invariably controllable during the time of triple drug therapy. Three of the patients died after 35, 60, and 105 days, but not from liver failure. Two more of these recipients are alive with completely normal hepatic function six (Fig. 6) and three months after transplantation; they are still being treated with all three agents.
Fig. 6.
Course of a 42 year old man who received a liver homograft six months previously. There was a vigorous early rejection, but this reversed promptly without any changes in therapy. Liver function has been normal for many months. Therapy with horse antilymphocyte globulin, ALG, has never been discontinued. Unfortunately, pulmonary metastases from the hepatoma have developed. (Fig. 3). SGOT, serum glutamic oxalacetic transaminase; SGPT, serum glutamic pyruvic transarninase; I.U., international unit.
In contrast, the other six patients had therapy with antilymphocyte globulin stopped from 17 days to four months postoperatively. In five, jaundice recurred within one to nine weeks, drastic revisions in therapy being necessary. An example is shown in Figure 5. The indication for transplantation was congenital biliary atresia. After operation, the serum bilirubin value promptly fell from 31 milligrams per cent to nearly normal. The child remained in good health until the horse antilymphocyte globulin was discontinued four months postoperatively. About two months later, clinically evident jaundice had returned. The late rejection was treated by increasing the prednisone doses and by beginning a course of rabbit antilymphocyte globulin. The sharp increases in serum transaminase and alkaline phosphatase values were promptly reversed, but not the icterus.
None of the patients who experienced late rejection died as a direct consequence, although two had chronic liver failure when they died as a result of septic complications, four and one-half and more than six months postoperatively, and a third patient eventually required retransplantation, as will be mentioned.
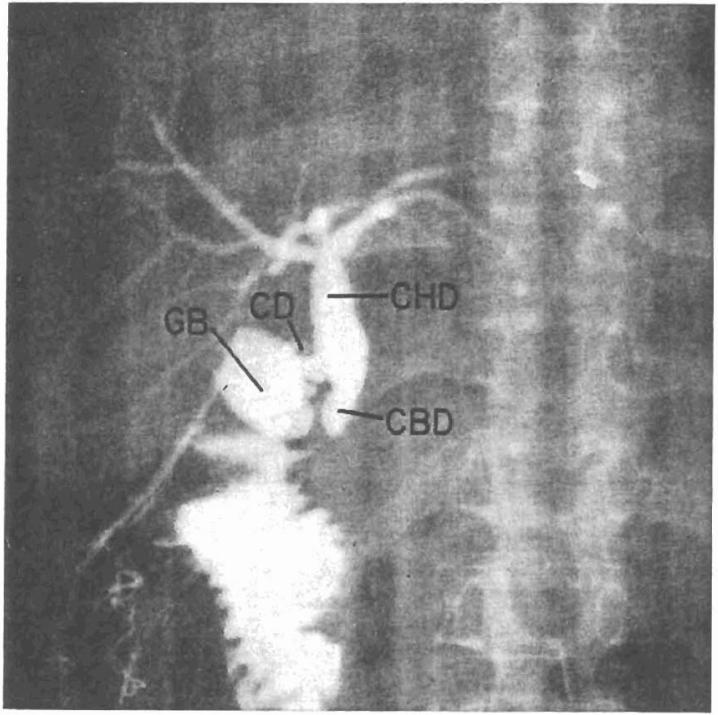
In the patients in whom late rejection developed, liver function was, at least, temporarily stabilized after intensification of the immunosuppressive therapy to the extent that protein and carbohydrate metabolism could be maintained at a satisfactory level. However, they were left with abnormalities, suggestive of extrahepatic biliary obstruction. One patient was reoperated upon. Operative cholangiography showed the patency of the biliary drainage system (Fig. 7). In no instance have the serum bilirubin and alkaline phosphatase values ever returned to the previous state after such a late rejection.
Fig. 7.
Operative cholangiogram of a 16 year old girl obtained ten weeks after orthotopic liver transplantation for the indication of hepatoma. Re-exploration was carried out because of persistent jaundice. The dye was injected after inserting a Foley catheter through the cholecystoduodenostomy into the gallbladder. Note that the biliary drainage from the homograft is not obstructed but that the fine ramifications of the intrahepatic ductal system are not seen. CBD, common bile duct; CD, cystic duct; CHD, common hepatic duct; GB, gallbladder.
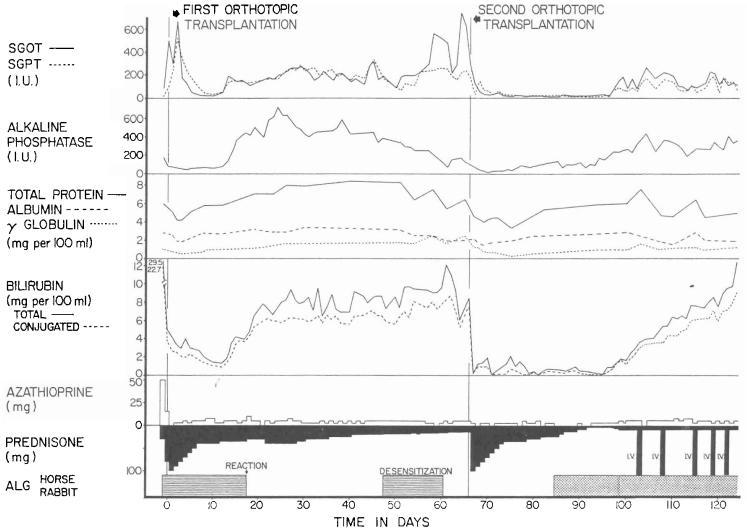
Retransplantation
In one patient, of special interest, it was necessary to discontinue horse antilymphocyte globulin 17 days after operation because of intense local reactions at the intramuscular injection sites. Uncontrollable rejection developed (Fig. 8) and ultimately lead to the decision to perform orthotopic retransplantation. At the second operation, the homograft was found to be enormously swollen and to have a mottled surface (Fig. 9). It weighed 880 grams, compared to an estimated 250 grams nine and one-half weeks previously.
Fig. 8.
Course of a 23 month old child who received two orthotopic liver homografts. When the first one rejected, the patient became febrile and progressively more toxic. The organ was eventually removed and replaced with a second liver. Although a difficult rejection is still in progress, affecting the final homograft, the patient is in good condition. SGOT, serum gIutamic oxalacetic transaminase; SGPT, serum glutamic pyruvic transaminase; I.U., international unit.
Fig. 9.
Appearance of the rejected liver which was removed (Fig. 8) and replaced with a second homograft. Note the huge size and uneven color of the organ.
The first homograft for the two year old recipient was obtained from a three year old cadaveric donor, but the second liver was from a seven year old child. The recipient had a stormy postoperative course after retransplantation, mainly, because the huge size of the new organ made breathing difficult and eating for the first ten postoperative days impossible. An emergency batch of rabbit antilymphocyte globulin was prepared and when this regimen was begun, the prednisone and azathioprine doses were drastically reduced. At present, the second homograft is undergoing an indolent, but persistent, rejection (Fig. 8), the outcome of which is not yet clear.
PATHOLOGIC OBSERVATIONS
Early Failure
Three of the homografts were obtained at autopsy, one-half, one, and four days after operation. In the first specimen, the hepatic arterial supply had apparently been compressed by the caudate lobe of the oversized homograft, although the vessel had not clotted. Some of the hepatocytes were necrotic, and moderately dense colIections of small lymphocytes were found around the tributaries of the portal vein in several of the smaller portal tracts. In the second and third specimens, respectively, the portal vein and hepatic arteries had thrombosed. The hepatic artery obstruction was associated with complete infarction of the homograft and the portal vein thrombosis with necrosis of the hepatocytes in the central and middle zones of the lobules. Cellular infiltration was absent in these two specimens.
Late Homografts
Tissue was also obtained from another eight homografts, either at autopsy, from biopsy, or at retransplantation. At the time of histologic examination, these livers had supported life from 35 days to more than 13 months. The findings in the ischemic right lobes of four of these hepatic grafts have been previously described (12, 13). In the present account, emphasis will be placed on changes thought to have resulted from immunologic damage.
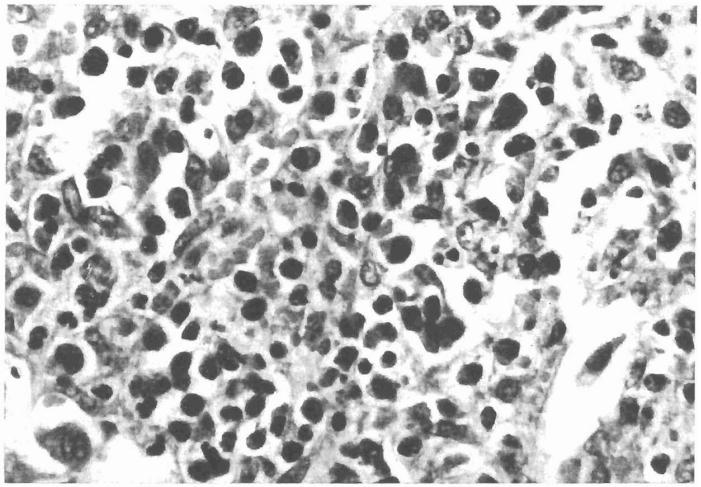
Cellular infiltration
Mononuclear cell infiltration, occasionally accompanied by a few eosinophilic polymorphonuclear leukocytes, was found in seven of the eight homografts (Fig. 10). The majority of the mononuclear cells had the ultrastructure of unmodified small lymphocytes. A variable proportion were larger lymphoid cells with pyroninophilic cytoplasm, containing many free ribosomes. Some were plasma cells with abundant, rough endoplasmic reticulum in their cytoplasm; a few were macrophages. The cells were commonest around the portal and central veins and beneath the endothelium of these vessels. Infiltrating cells were less frequent in the spaces of Disse. In only four of the tissue samples, obtained at eight, 28, 30, and 66 days after transplantation, was the infiltration dense, and these samples contained 10 to 40 per cent of pyroninophilic lymphoid cells. The 66 day sample came from the homograft previously mentioned under the heading of retransplantation, in which uncontrollable rejection followed the premature cessation of treatment with anti-lymphocyte globulin. The other three biopsies came from homografts which later lost their cellular infiltration, as shown in subsequent samples obtained at periods up to 400 days after transplantation.
Fig. 10.
Hepatic homograft removed 66 days after transplantation. Uncontrollable rejection followed early withdrawal of antilymphocyte globulin. Large numbers of infiltrating mononuclear cells with basophilic cytoplasm lie in a portal tract. Hematoxylin and eosin, ×417.
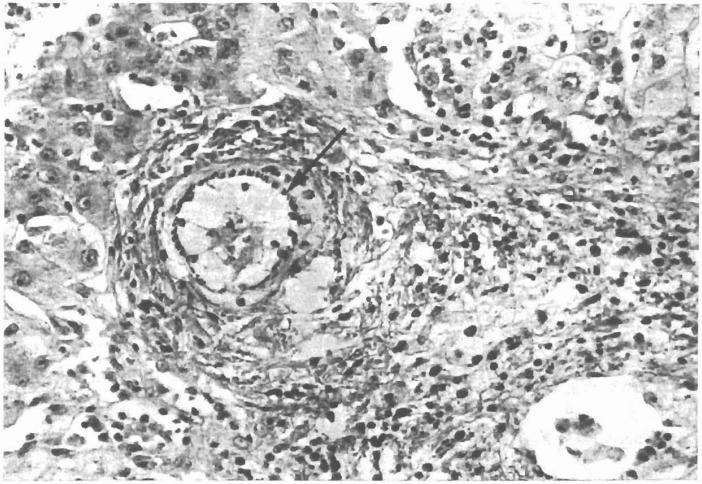
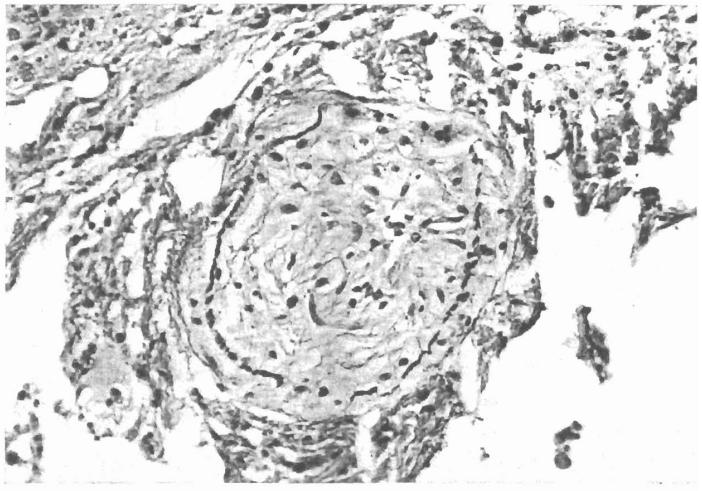
Arterial intimal thickening
There was thickening of the intima of the small branches of the hepatic arteries in four of the eight homografts (Figs. 11 and 12); this late change was first seen 66 days after transplantation of the graft, which was removed because of uncontrollable rejection. It was present in a widespread and particularly severe form and lead to a great narrowing or obstruction of the vessels in this latter graft as well as in the liver from the patient who died 186 days after transplantation. The thickened intima had many large cells with abundant cytoplasm, containing fine droplets of fat. Frequently, the internal elastic lamina was ruptured.
Fig. 11.
Same liver graft as seen in Figure 10. In the portal tract, a branch of the hepatic artery is greatly narrowed by large intimal cells with foamy cytoplasm. The internal elastic lamina of the vessel is indicated by the arrow. Elastic stain, ×208.
Fig. 12.
Same liver graft as seen in Figures 10 and 11 shows a branch of the hepatic artery in a portal tract. The vessel is completely occluded by intimal thickening, and the internal elastic lamina is ruptured. Elastic stain, ×208.
Hepatic fibrosis and cirrhosis
Increased amounts of reticulin and collagen in the portal tracts and, to a lesser extent, condensation of reticulin around the central veins, were found in seven of the eight homografts. In several livers, this was accompanied by the linking of portal tracts to each other by fibrous bands, but in only two instances had this progressed to portal cirrhosis with regeneration nodules and areas of hepatocyte necrosis. Proliferating small bile ductules were present in the portal areas of some livers. These changes were first found 54 days after transplantation.
Cholestasis
Bile thrombi were present in the centrilobular canaliculi in six of the eight homografts. All six were livers which also showed diffuse fibrosis. In one of the grafts, the major intrahepatic bile ducts were also dilated and filled with casts composed of inspissated bile surrounded by polymorphonuclear leukocytes.
Enlargement of Kupffer cells
The Kupffer cells were enlarged and prominent in four of the five longest surviving grafts. The cytoplasm contained material that ultrastructurally was finely granular and that by immunofluorescence stained for immunoglobulins G and M and for complement.
Necrosis and atrophy of the centrilobular hepatocytes
In those grafts that showed dense cellular infiltration, with or without fibrosis, there was usually evidence of atrophy or necrosis of the centrilobular hepatocytes.
DISCUSSION
In almost all the attempts at orthotopic liver transplantation, made before the summer of 1967, the indication was primary hepatic cancer. The early deaths of these patients made observations impossible regarding the effect of the procedure on the natural history of this disease. More recent experience is still too limited to permit a decisive conclusion about this question. However, the appearance of metastases in two of the more recently treated patients is a discouraging finding. As the studies of Berman as well as those of Spatt and Grayzel have shown, hepatomas ordinarily follow a highly unfavorable course and usually lead to death within a few weeks or months after diagnosis. Total hepatectomy extends the criteria of local resectability but does not ensure against tumor spread.
Indeed, there is reason to be fearful that the immunosuppressive therapy necessary to prevent rejection of the homograft may itself be a factor which could accelerate the dissemination of residual neoplasm. According to the hypothesis of Burnet, the consequent immunologic crippling should result in at least a partial loss of the normal surveillance mechanism, by which mutant cells are identified as “nonself” and eliminated or presumably restricted in their growth potential. That this view may have some validity is attested to by the ease with which carcinoma has been accidentally transplanted from renal donors dying of cancer but whose kidneys were not grossly involved, and by the report of Penn and his associates of an increased incidence of malignant neoplasia arising de novo in recipients of renal homografts that had been obtained from normal donors. An observation even more relevant to the problem under discussion was recently made by Williams and his co-workers who performed renal homotransplantation in a child six months after excision of a Wilms' tumor. Sixteen months after transplantation, at which time cure of this kind of neoplasm would usually have been assured under normal conditions, metastases became apparent, and death resulted within a few weeks.
Even if it is found that a hepatoma can be cured with hepatic replacement, it is virtually certain that the greatest value of liver transplantation will be for the treatment of nonneoplastic liver disease. Before this objective can be met on a large scale, improvements of several kinds will be necessary. For example, a full explanation for the high incidence of vascular accidents is not as yet available. Mechanical factors may play an important role, as mentioned earlier, in connection with the lobar arterial thromboses. In addition, it is probably more than coincidental that all eight of the partial or complete vascular occlusions occurred in the 11 pediatric patients in whom the reconstructed vessels were all extremely small. There were no such examples in the three adults.
Another condition which may make liver replacement more hazardous than transplantation of other organs is the profound effect, as described by Groth and von Kaulla and their associates, which the procedure itself has on the coagulation mechanism of the recipient. A hemorrhagic diathesis often develops during operation. However, if an organ is provided which functions promptly and well, the clotting defect is rapidly corrected and may be succeeded by a hyper-coagulable state. At least in infant recipients, it may consequently be advisable in some instances to consider systemic heparinization in the early postoperative period. Even this may be insufficient, since the fatal portal vein thrombosis, described in one of our patients, developed in spite of anticoagulants.
Unfortunately, even those recipients who received technically perfect transplantation procedures and in whom thrombosis of their homograft blood supply or metastatic disease did not subsequently develop were not assured a trouble-free late course. It became apparent that most of the patients were dependent upon the combination drug therapy initially used for continuing stable function of the homografts. This was true whether or not a good histocompatibility match had been thought by Terasaki to be present. When the heterologous antilymphocyte globulin was discontinued, delayed rejection soon developed in almost every patient. Furthermore, it proved to be impossible to completely reverse the consequent deterioration in hepatic function.
The regularity with which this complication occurred has prompted suggestions for alternative regimens for adjuvant heterologous globulin therapy (11). The possibilities include the administration of the anti-lymphocyte globulin for much longer periods than the arbitrary four months used for most of these patients. If sensitization to the equine protein precludes this, it may be feasible to change to another species, such as the rabbit or goat, an expedient which has already been followed in two of our patients. Of potentially greater value might be the administration of the antilymphocyte globulin in much larger doses, in an effort to attain the kind of early and long-lasting tolerance that has been produced by Medawar as well as by Monaco and his associates with this general approach in rodents.
With the transplantation of the vital un-paired organs, improvement of existing methods of immunosuppression and tissue typing is much more urgent than is the case with the kidney. In the event of rejection of a renal homograft, the transplant can be removed and effective long term support provided with an artificial kidney. A comparable option is not available with either the liver or the heart, which must be replaced under these circumstances, if life is to continue.
It is of some importance to realize that this is a practical possibility, as was demonstrated by one of the patients in this series who received a second liver homograft in the orthotopic location. It has become evident from the follow-up of liver recipients, that homograft failure is apt to occur gradually enough in many patients to permit consideration of, and planning for, retransplantation. The same pertains after cardiac homotransplantation, since Lower and his associates have demonstrated that late rejection of the transplanted canine heart may require weeks, or even months, to be advanced enough to cause death.
The notion that if liver homografts are eventually rejected the process can be expected to be a gradual one is supported by the pathologic studies, reported herein which are the first that have become available from human beings in any quantity. The slow pace at which liver homografts deteriorate, if this occurs late, can be explained by the histologic findings. Initially, there may be a dense lymphoid cell infiltration of the portal and central areas. However, this seems to recede after the first month, except in those patients in whom adequate immunosuppression cannot be maintained. A period of repair follows in which there is a laying down of reticulin fibers and collagen in the portal areas. This is often accompanied by condensation of the centrilobular reticulin and centrilobular cholestasis. Occasionally, this diffuse fibrosis may later progress to cirrhosis. Severe arterial narrowing, due to intimal thickening, occurs in those patients in whom rejection is poorly controlled. With the exception of the arterial lesions, these changes closely follow those that have been described in liver homografts in dogs treated with immunosuppressive drugs.
SUMMARY
Fourteen orthotopic liver transplantations have been performed since July 1967 in patients with hepatoma or biliary atresia. Three deaths have occurred in the immediate postoperative period due to occlusion of either the common hepatic artery or portal vein. Five of the remaining 11 patients are still alive eight and one-half, seven, six, five, and three months later. One of the surviving patients has had a second orthotopic transplantation after the rejection of the originally placed homograft. The other six patients who survived the immediate postoperative period died 35, 60, 105, 133, 186, and 400 days postoperatively. Indirectly, or directly, the cause of death in four of the latter six patients was thrombosis of the right hepatic artery and subtotal hepatic gangrene. The other two patients died of pneumonitis and carcinomatosis, respectively.
Several recurrent late problems occurred in this series. Four of the recipients were operated upon because of hepatoma, and metastases developed in two, including the patient who lived for more than a year. There is a hypothetic possibility that the immunosuppressive therapy used to prevent homograft rejection may have caused acceleration of the growth of the recurrent tumor. A more definite limitation of the immunosuppressive regimen was encountered In six patients, the heterologous antilymphocyte globulin, which was used as an adjuvant to azathioprine and prednisone, was eventually stopped. Indolent late rejection then developed in five of six patients within one to eight weeks.
The liver homografts have been examined in 11 of the 14 patients. Of the eight long-surviving patients, seven livers became infiltrated by lymphoid cells. Repeat biopsies showed that the number of infiltrating cells decreased after the first month, except in the patient with uncontrollable rejection following premature withdrawal of antilymphocyte globulin. Cellular infiltration was accompanied by necrosis or atrophy of the centrilobular hepatocytes. Portal fibrosis developed in seven of the grafts, and in two, this condition progressed to cirrhosis. Centrilobular cholestasis and condensation of reticulin were present in six of the grafts. In four livers, thickening was present in the intima of the small branches of the hepatic arteries. These changes probably resulted from rejection.
Acknowledgments
Supported by U. S. Public Health Service Grants No. AM-06344, HE-07735, AM-07772, AI-04152, FR-00051, FR-00069, AM-12148, and AI-AM-08898; and by grants from the British Heart Foundation, Clark Memorial Fund, Medical Research Council, St. Mary's Hospital Research Fund, and the Wellcome Trust.
Footnotes
Presented at the Sessions on Papers of General Interest, Clinical Congress of American College of Surgeons, 18 October 1968.
REFERENCES
- 1.BERMAN C. Primary carcinoma of the liver. Bull. N. Y. Acad. Med. 1959;35:275. [PMC free article] [PubMed] [Google Scholar]
- 2.BIRTCH AG, MOORE FD. Personal communication. Aug 22, 1968.
- 3.BURNET FM. The new approach to immunology. New Eng. J. Med. 1961;264:24. doi: 10.1056/NEJM196101052640107. [DOI] [PubMed] [Google Scholar]
- 4.GROTH CG, PECHET L, STARZL TE. Coagulation during and after orthotopic transplantation of the human liver. Arch. Surg. 1968 doi: 10.1001/archsurg.1969.01340070049006. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LOWER RR, DONG E, SHUMWAY NE. Long-term survival of cardiac homografts. Surgery. 1965;58:110. [PubMed] [Google Scholar]
- 6.MEDAWAR PB. Biological effects of heterologous antilymphocyte sera. In: Rapaport FT, Dausset J, editors. Human Transplantation. Grune & Stratton, Inc.; New York: 1968. pp. 501–509. [Google Scholar]
- 7.MONACO AP, WOOD ML, RUSSELL PS. Studies on heterologous antilymphocyte serum in mice-III, immunologic tolerance and chimerism produced across the H-2 locus with adult thymectomy and anti-lymphocyte serum. Ann. N. Y. Acad. Sci. 1966;129:190. [Google Scholar]
- 8.PENN I, HAMMOND W, BRETTSCHNEIDER L, STARZL TE. Proceedings of the Transplantation Society. Grune & Stratton, Inc.; New York: 1968. Malignant lymphomas in transplantation patients. in press. [PMC free article] [PubMed] [Google Scholar]
- 9.SPATT SD, GRAYZEL DM. Primary carcinoma of the liver. Amer. J. Med. 1948;5:570. doi: 10.1016/0002-9343(48)90107-7. [DOI] [PubMed] [Google Scholar]
- 10.STARZL TE, BRETTSCHNEIDER L, PENN I, BELL P, GROTH CG, BLANCHARD H, KASHIWAGI N, PUTNAM CW. Proceedings of the Transplantation Society. Grune & Stratton, Inc.; New York: 1968. Orthotopic liver transplantation in man. in press. [PMC free article] [PubMed] [Google Scholar]
- 11.STARZL TE, BRETTSCHNEIDER L, PENN I, SCHMIDT RW, BELL P, KASHIWAGI N, TOWNSEND CM, PUTNAM CW. Proceedings of the Transplantation Society. Grune & Stratton, Inc.; New York: 1968. A trial with heterologous antilymphocyte globulin in man. in press. [PMC free article] [PubMed] [Google Scholar]
- 12.STARZL TE, GROTH CG, BRETTSCHNEIDER L, MOON JB, FULGINITI VA, COTTON EK, PORTER KA. Extended survival in 3 cases of orthotopic homotransplantation of the human liver. Surgery. 1968;63:549. [PMC free article] [PubMed] [Google Scholar]
- 13.STARZL TE, GROTH CG, BRETTSCHNEIDER L, PENN I, FULGINITI VA, MOON JB, BLANCHARD H, MARTIN AJ, PORTER KA. Orthotopic homotransplantation of the human liver. Ann. Surg. 1968;168:392. doi: 10.1097/00000658-196809000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.VON KAULLA KN, KAYE H, VON KAULLA E, MARCHIORO TL, STARZL TE. Changes in blood coagulation before and after hepatectomy or transplantation in dogs and man. Arch. Surg. 1966;92:71. doi: 10.1001/archsurg.1966.01320190073016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WILLIAMS G, LEE H, HUME D. Proceedings of the Transplantation Society. Grune & Stratton, Inc.; New York: 1968. Renal transplants in children. in press. [PubMed] [Google Scholar]