Abstract
The anti-rheumatoid agent aurothiomalate (ATM) is a potent inhibitor of oncogenic PKCι ATM inhibits non-small lung cancer (NSCLC) growth by binding PKCι and blocking activation of a PKCι-Par6-Rac1-Pak-Mek 1,2-Erk 1,2 signaling pathway. Here, we assessed the growth inhibitory activity of ATM in a panel of human cell lines representing major lung cancer subtypes. ATM inhibited anchorage-independent growth in all lines tested with IC50s ranging from ~300 nM – >100 µM. ATM sensitivity correlates positively with expression of PKCι and Par6, but not with the PKCι binding protein p62, or the proposed targets of ATM in rheumatoid arthritis (RA), thioredoxin reductase 1 or 2 (TrxR1 and TrxR2). PKCι expression profiling revealed that a significant subset of primary NSCLC tumors express PKCι at or above the level associated with ATM sensitivity. ATM sensitivity is not associated with general sensitivity to the cytotoxic agents cis-platin, placitaxel and gemcitabine. ATM inhibits tumorigenicity of both sensitive and insensitive lung cell tumors in vivo at plasma drug concentrations achieved in RA patients undergoing ATM therapy. ATM inhibits Mek/Erk signaling and decreases proliferative index without effecting tumor apoptosis or vascularization in vivo. We conclude that ATM exhibits potent anti-tumor activity against major lung cancer subtypes, particularly tumor cells that express high levels of the ATM target PKCι and Par6. Our results indicate that PKCι expression profiling will be useful in identifying lung cancer patients most likely to respond to ATM therapy in an ongoing clinical trial.
Keywords: mechanism-based therapy, anchorage-independent growth, tumorigenicity, small cell lung cancer, non-small cell lung cancer
INTRODUCTION
Lung cancer is the leading cause of cancer death in the United States exceeding mortality from breast, prostate and colorectal cancers combined 1. Despite advances in surgery, chemotherapy and radiotherapy, long term survival rates of lung cancer patients remain poor. Recent advances in treatment have come from novel mechanism-based therapeutics that target oncogenic signaling pathways activated in specific subsets of lung cancers. Small molecule inhibitors of the epidermal growth factor receptor (EGFR) tyrosine kinase (TKIs) exhibit potent anti-tumor activity in lung cancers that possess specific molecular characteristics that confer sensitivity to the drugs [reviewed in 2]. The presence of mutations in EGFR, and to a lesser extent, the presence of EGFR amplification and elevated EGFR expression, correlate positively with therapeutic response to the TKIs gefitinib and erlotinib 3. TKI-sensitizing EGFR mutations are more common in never-smokers, women, Asians, and patients with adenocarcinoma 2. These molecular and clinical characteristics have been used successfully to guide TKI therapy to patients most likely to respond. Clearly, there exists a need to identify effective mechanism-based therapeutics that target prevalent molecular characteristics in lung cancer patients who are not responsive to currently available therapy.
We recently identified atypical PKCι as an oncogene and therapeutic target for lung cancer therapy 4, 5. PKCι expression is elevated in a significant subset of NSCLC cell lines and primary NSCLC tumors. The PKCι gene, PRKCI, is a critical target of frequent, tumor-specific amplification, particularly in lung squamous cell carcinomas 4, and PRKCI amplification drives PKCι mRNA and protein expression in these tumors 4.
PKCι is required for anchorage-independent growth of NSCLC cells in vitro and tumorigenicity in vivo 6. PKCι drives anchorage-independent growth of NSCLC cells by activating a Rac1-Pak-Mek1,2-Erk1,2 signaling pathway 6. PKCι regulates Rac1 through a conserved Phox and Bem1p (PB1) protein interaction domain within the regulatory region of PKCι 6. PKCι binds via PB1-PB1 domain interactions to the polarity protein Par6 to form a complex that regulates Rac1 and drives anchorage-independent growth 6. Given the importance of the PKCι-Par6 interaction in NSCLC cell transformation, we screened a library of chemical compounds approved for human use to identify inhibitors of this interaction 5. From this screen, we identified two anti-rheumatoid gold compounds aurothioglucose (ATG) and aurothiomalate (ATM) that inhibit PKCι binding to Par6 in vitro 5. These compounds block transformation of NSCLC cells in vitro and tumorigenicity in vivo by disrupting PKCι-mediated activation of Rac1 5, 7. Based on our pre-clinical data, a phase I clinical trial of ATM in advanced stage NSCLC patients is currently ongoing to establish a maximum tolerated dose and to evaluate patients for therapeutic response to ATM.
A critical step in the clinical development of ATM is to determine the spectrum of ATM activity against major lung cancer subtypes, assess whether ATM exhibits anti-tumor activity in relevant pre-clinical lung cancer models in vivo at serum drug concentrations achievable in humans, and identify specific molecular characteristics of lung tumor cells that correlate with ATM response. Here we report that ATM exhibits broad anti-tumor activity against major forms of lung cancer in vitro, and that expression of PKCι and Par6 correlates with ATM response. PKCι expression profiling revealed a significant subset of primary NSCLC tumors that over-express PKCι to levels that correlate with ATM sensitivity in lung cancer cell lines. ATM inhibits tumor cell proliferation at serum drug concentrations routinely achieved in RA patients treated with ATM. Our results indicate that lung tumor PKCι expression profiling can be used to identify lung cancer patients most likely to benefit from ATM therapy in ongoing clinical trials.
MATERIALS AND METHODS
Reagents and Cell Culture
Antibodies were from the following sources: PKCι, BD PharMingen (San Diego, CA), FLAG, Sigma (St. Louis, MO); BrdU, DakoCytomation (Carpinteria, CA); β-actin, p44/42 extracellular signal-regulated kinase (Erk), and phospho-p44/ 42 Erk (Thr202/Tyr204), Cell Signaling Technology, Inc. (Danvers, MA); Pecam-1 (sc-1506) and c-IAP2 (sc-7944), Santa Cruz Biotechnology, Inc. (Santa Cruz, CA). Terminal deoxynucleotidyl transferase-mediated incorporation of biotinylated nucleotide at the 3’-OH ends of fragmented DNA of apoptotic cells was detected using the DeadEnd Colorimetric TUNEL System from Promega (Madison, WI). Aurothiomalate (ATM; Myochrysine, Taylor Pharmaceuticals, Decatur, IL), Cisplatin (Bedford Laboratories, Bedford, OH) and Gemcitabine HCl (Gemzar; Eli Lilly and Company, Indianapolis, IN) were diluted in phosphate-buffered saline (PBS). Paclitaxel (IVAX Pharmaceuticals, Inc., Miami, FL) was diluted in Me2SO. Cells were treated with concentrations of these agents as indicated and control cells were treated with either an equivalent volume of PBS or Me2SO equal to a final concentration of 0.1% v/v. Human A549, H1437, H2170, H460, H510, H187, H1703 and A427 lung cancer cell lines were obtained from the American Type Culture Collection (Manassas, VA) and maintained as suggested by the supplier in a humidified tissue culture incubator at 37°C in 5% CO2.
Anchorage-independent Growth Assays
Anchorage-independent growth was assessed by the ability to grow as colonies in soft agar in the presence of chemotherapeutic agents at the concentrations indicated in the figures as described previously 6. Soft agar colonies were visualized and quantified after four weeks in culture. The concentration of chemotherapeutic agent resulting in 50% growth inhibition (IC50) was calculated using SigmaPlot for Windows10.0 (San Jose, CA).
Immunoblot Analysis
Cell lysates were subjected to immunoblot analysis for PKCι abundance as described previously 6. Protein concentrations were determined using the Pierce bicinchoninic acid (BCA) Protein Assay Kit (Pierce Biotechnology, Rockford, IL) using bovine serum albumin (BSA) as a standard. Antigen-antibody complexes were detected using Amersham ECL-Plus (GE Healthcare, Buckinghamshire, UK). Images were developed on Kodak BioMax MR film and captured using the Kodak Gel Logic 100 Imaging System. Antigens were quantified using Kodak Molecular Imaging Software v4.0.5.
RNA Isolation and Quantitative PCR
Total RNA was extracted using RNAqueous (Ambion, Austin, TX), according to the manufacturer's protocols. RNA quality and integrity were measured using an Agilent 2100 Bioanalyzer (Agilent Technologies, Santa Clara, CA) and the Agilent RNA 6000 nano kit using Agilent 2100 Expert software following the manufacturer's protocols. Reagents for quantitative real time PCR (QPCR) analysis of human PKCι, Par6α, Par6β, Par6γ, p62, TrxR1 and TrxR2 mRNA abundance were purchased from Applied Biosystems (Foster City, CA). To assess for possible associations between Par6 and PKCι expression or ATM sensitivity, total Par6 abundance was calculated by summing the abundance of the three human Par6 isoforms Par6α, Par6β and Par6γ. Analysis was carried out using 10 ng of cDNA on an Applied Biosystems 7900 thermal cycler, and data were analyzed using the SDS 2.3 software package. All data were normalized to expression of 18S RNA using 2 ng of cDNA, and data were expressed as 2−(CT(target)−CT(18s)).
Quantitative PCR Analysis for PRKCI Gene Amplification
Genomic DNA from each cell line was analyzed for PRKCI gene amplification using Taqman technology on an Applied Biosystems 7900HT sequence detection system. The human RNaseP1 gene was used as a DNA template control and for normalization of results to total DNA. The primer/probe set for the human PRKCI gene was forward primer, 5'-GGCTGCATTCTTGCTTTCAGA-3'; reverse primer, 5'-CCAAAAATATGAAGCCCAGTAATCA-3'; and probe, 5'-CAATCTTACCTGCTTTCT-3'. The primer/probe set for the RNaseP1 gene was designed and provided by ABI Assay on Demand. A tumor cell line was scored positive for PRKCI gene amplification when analysis revealed a minimum of one extra copy of the PRKCI allele.
Mutational Analysis
Genomic DNA was obtained from lung cancer cell lines using the QIAamp® DNA Mini Kit (Qiagen, Valencia, CA) according to the manufacturer’s protocol. Genomic DNA was obtained from primary NSCLC tumors using phenol/chloroform extractions. PRKCI and KRAS exon-specific primers were designed and DNA was subjected to PCR amplification using the GeneAmp® High Fidelity PCR System (Applied Biosystems). Portions of the PCR reactions were run on a 2% agarose gel to verify proper PCR amplification and amplification products were purified using MultiScreen PCR96 Filter Plates (Millipore). Samples were sequenced on both strands by Mayo Clinic’s DNA Sequencing Core Facility using Applied Biosystems BigDye® terminator v1.1 cycle sequencing chemistry and analyzed on Applied Biosystems 3730XL DNA Analyzer. The data were analyzed using Vector NTI Advance 10 ContigExpress Software (Invitrogen). Chromatograms for exon sequences were viewed individually to ensure accuracy and aligned with the consensus sequence from public databases.
Tumorigenicity in Nude Mice
The growth of A427 and H460 human lung cancer cells as subcutaneous tumors in the presence and absence of ATM was assayed in athymic nude mice (Harlan-Sprague-Dawley, Indianapolis, IN) maintained in a defined, pathogen-free environment as described previously 6. Briefly, A427 and H460 cells in logarithmic growth phase were harvested and resuspended in serum-containing growth medium. 4–6-week-old female nude mice were injected subcutaneously into the flank with either 1 × 107 A427 or 5 × 106 H460 cells in 100 µl of growth medium. Once palpable tumors were established, mice were randomly divided into five treatment groups that received daily intramuscular injections of ATM at 2, 6, 20 or 60 mg/kg body weight or with an equal volume of diluent (sterile PBS). Tumor dimensions were measured using calipers and tumor volume (mm3) was calculated as described previously 6. The experiment was terminated when tumors in control mice reached ~2,000 mm3. Mice were injected intraperitoneally with 100 µg/g 5-bromo-2-deoxyuridine (BrdU) 1 h prior to sacrifice. Tumors were excised and samples obtained for combined protein and RNA extraction, and for fixation in 10% buffered formalin, embedding in paraffin and sectioning (5 µm). Sections were subjected to immunohistochemical analysis using antibodies to expression of BrdU, TUNEL and PECAM1 as described previously 6. Total tumor extracts were prepared using the PARIS (Protein and RNA Isolation System) Kit (Ambion) and equal amounts of protein were subjected to immunoblot analysis as described above.
Serum Gold Determinations
Serum was collected from mice treated with ATM at 0, 2, 6, 20 and 60 mg/kg daily for 14 days. Mice were anesthetized by CO2 inhalation and the caudal (inferior) vena cava was identified and dissected free of surrounding connective tissue. A 23G needle attached to a 5-mL syringe was carefully introduced into the inferior vena cava and gentle suction was applied with the syringe. Drawn blood was allowed to clot for 30 minutes and then centrifuged at 3,000 rpm for 10 min. Serum was collected and stored at −20°C. All materials were certified metal-free and clinical serum gold analysis was conducted by Mayo Medical Laboratories.
Statistical Analysis
The t-test, rank sum test and one way analysis of variance (ANOVA) were used to evaluate the statistical significance of the results. Pearson Product Moment Correlation was used to evaluate the strength of the association between pairs of variables. Statistical analyses were performed using SigmaStat for Windows 3.5 (San Jose, CA) and p-values ≤ 0.05 were considered statistically significant.
RESULTS
ATM inhibits anchorage-independent growth of lung cancer cell lines
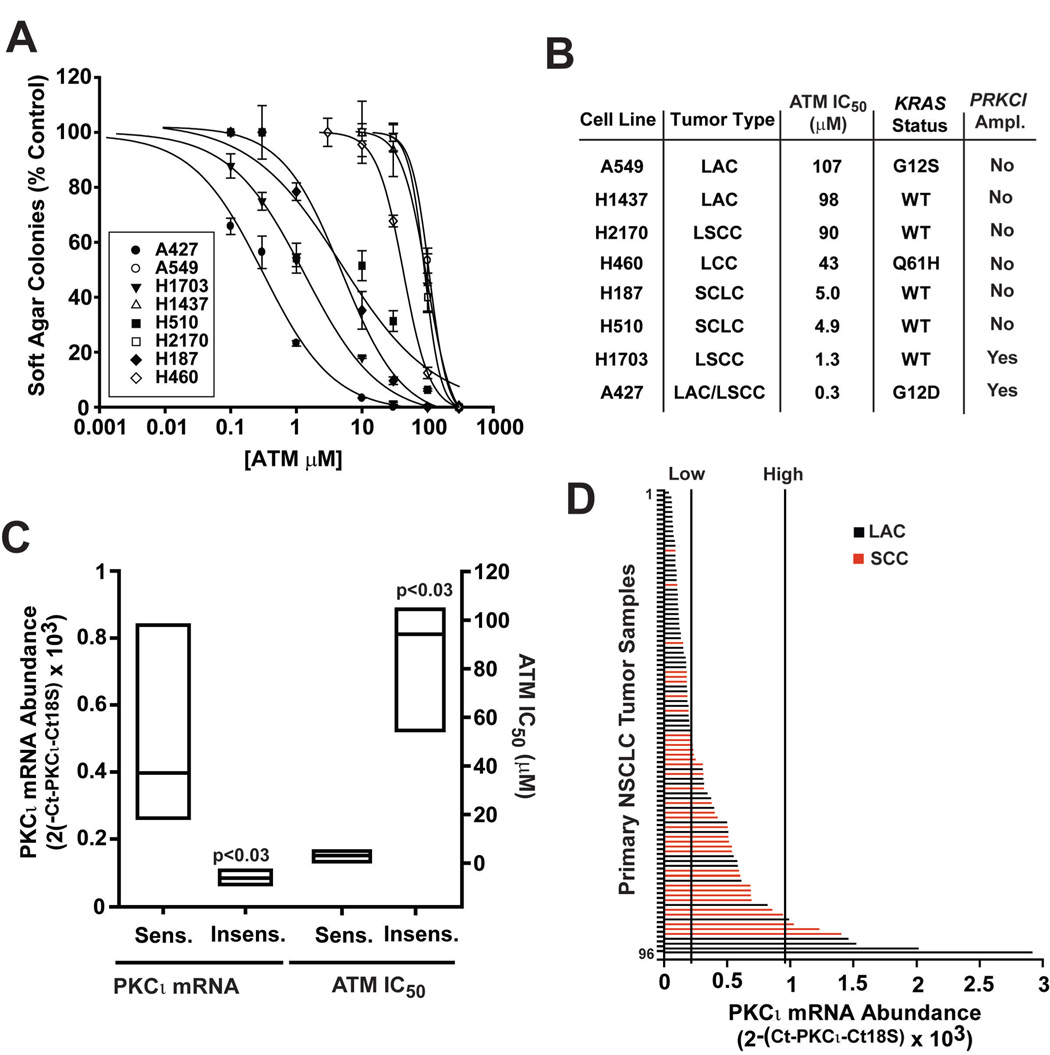
ATM is currently in a phase I dose escalation clinical trial for NSCLC. To facilitate the clinical development of ATM we assessed the ability of ATM to inhibit anchorage-independent growth of a panel of 8 human lung cancer cell lines that represent major forms of lung cancer, lung adenocarcinoma (LAC), lung squamous cell carcinoma (LSCC), large cell carcinoma (LCC) and small cell lung carcinoma (SCLC) (Figure 1). ATM induced dose-dependent inhibition of anchorage-independent growth in all cell lines tested (Figure 1A). Interestingly, the cell lines clustered into two distinct groups; ATM sensitive cell lines (IC50 ≤ 5 µM) and ATM insensitive cell lines (>40 µM). Figure 1B lists the 8 cell lines tested, their histopathological class and the calculated IC50 for ATM inhibition. No correlation between histopathological class and ATM sensitivity emerged, however LSCC and SCLC cells tended to be more sensitive and LACs less sensitive to ATM.
Figure 1. ATM inhibits anchorage-independent growth of human lung cancer cell lines.
A. Dose response curves of eight human lung cancer cell lines to the growth inhibitory effects of ATM. Cells were plated in soft agar in the presence of the indicated concentration of ATM and anchorage-independent growth was assessed by counting soft agar colonies 30 days after plating. Results are expressed as soft agar colonies as a percent of control in the absence of ATM. Values represent the mean +/−SEM; n=3. B. Cell line name, ATM sensitivity (IC50), tumor type, KRAS mutational status and PRKCI gene amplification status of the panel of 8 human lung cancer cell lines analyzed in this study. LAC=lung adenocarcinoma; LSCC= lung squamous cell carcinoma, LCC=large cell carcinoma; SCLC=small cell lung carcinoma; LAC/LSCC=lung adenocarcinoma with squamous cell characteristics. C. PKCι mRNA abundance correlates positively with ATM sensitivity. Box plots were used to analyse PKCι mRNA abundance (left bars) and ATM IC50 in sensitive (Sens.) and insensitive (Insens.) cell lines. The middle line in each box represents the median of values and the box indicates the upper and lower quartiles. P-values indicate a statistical difference exists between the sensitive and insensitive cell lines for both parameters. D. A significant subset of primary NSCLC tumors express PKCι at levels that correlate with ATM sensitivity. 96 primary NSCLC tumors (60 LAC and 36 LSCC) were analyzed for PKCι mRNA abundance by QPCR. Bars represent individual tumors and the length of the bar along the x-axis indicates PKCι mRNA abundance. Red denotes LSCC, Black denotes LAC. The vertical lines indicate the range of PKCι mRNA abundance values measured for the sensitive lung cancer cell line.
Endogenous PKCι and Par6 expression correlate with ATM sensitivity in lung cancer cell lines
PKCι is a critical downstream effector of oncogenic K-Ras and genetic disruption of PKCι blocks K-ras-mediated transformation 8. Given the prevalence of KRAS mutations in NSCLC, we assessed whether tumor cells harboring activating KRAS mutations exhibit enhanced sensitivity to ATM. Three of the eight cell lines analyzed contained a KRAS mutation. However, KRAS mutation status did not correlate with ATM sensitivity since mutations were present in both sensitive and insensitive cell lines (Figure 1B).
We previously demonstrated that PRKCI is a target for frequent tumor-specific amplification in NSCLC tumors, particularly LSCCs 4. Interestingly, PRKCI amplification was observed in the two most ATM-sensitive cell lines in our panel, H1703 and A427 cells, both tumors with squamous cell characteristics (Figure 1B). However, the H510 and H187 SCLC lines showed similar sensitivities to ATM but do not harbor PRKCI amplification. Thus, whereas PRKCI amplification is associated with ATM sensitivity in LSCC cells, it does not appear to be required for ATM sensitivity.
PRKCI amplification drives PKCι mRNA and protein expression in LSCC cell lines and primary LSCC tumors 4. Therefore, we assessed whether PKCι expression is associated with ATM sensitivity. QPCR analysis revealed that the four ATM sensitive cell lines express significantly higher PKCι levels than the four insensitive lines (Figure 1C; see also Supplemental Figure 1). As expected, ATM IC50 values were significantly different in sensitive and insensitive lines (Figure 1C). Rank sum analysis revealed a statistically significant correlation between PKCι mRNA abundance and sensitivity to ATM (log IC50 to ATM) (Table 1) with high PKCι mRNA levels correlating with ATM sensitivity (low ATM IC50). We previously demonstrated a strong correlation between PKCι mRNA abundance and PKCι protein expression in primary NSCLC tumors 4. Immunoblot analysis of PKCι protein expression (see Supplemental Figure 1) revealed a statistically significant correlation between PKCι protein and PKCι mRNA abundance and between PKCι protein abundance and ATM sensitivity (Table 1). Thus, both PKCι mRNA abundance and PKCι protein expression correlate with ATM sensitivity.
Table 1.
PKCι and Par6 Expression Correlate with ATM Senitivitiy
| Correlation | Correlation Coefficient | p-value |
|---|---|---|
| PKCι RNA vs. log ATM IC50 | −0.90 | 0.003 |
| PKCι RNA vs. PKCι protein | 0.96 | <0.001 |
| PKCι protein vs. log ATM IC50 | −0.79 | 0.020 |
| Par6 RNA vs. PKCι RNA | 0.77 | 0.024 |
| Par6 RNA vs. log ATM IC50 | −0.72 | 0.042 |
| p62 RNA vs. log ATM IC50 | −0.21 | 0.61 |
| TrxR1 RNA vs. log ATM IC50 | −0.18 | 0.68 |
| TrxR2 RNA vs. log ATM IC50 | 0.31 | 0.45 |
ATM was identified through a high-throughput drug screen for its ability to inhibit PKCι-Par6 binding in vitro 5, 7. PKCι-mediated transformation requires activation of the downstream effector molecule, Rac1 6. PKCι regulates Rac1 through interaction with Par6 6. Since ATM targets the PKCι-Par6 interaction, we reasoned that Par6 expression might also correlate with ATM sensitivity. Quantitative PCR analysis revealed a significant correlation between Par6 mRNA and PKCι mRNA abundance and between Par6 mRNA and ATM sensitivity in our panel of 8 lung cancer cell lines (Table 1). ATM also inhibits binding of PKCι to p62, another PB1 domain binding partner of PKCι 7. However, analysis revealed no correation between p62 mRNA abundance and ATM sensitivity (Table 1).
ATM is a clinically approved treatment for RA. ATM has been reported to bind and inhibit the activity of thioredoxin reductase 1 and 2 (TrxR1 and TrxR2) 9, and inhibition of these enzymes may contribute to the anti-rheumatoid activity of ATM. TrxRs are over-expressed in some human tumor cells and may play a role in tumor cell proliferation 10. However, we observed no correlation between TrxR1 or TrxR2 expression and ATM sensitivity in our lung cancer cell lines (Table 1). Thus, ATM sensitivity in lung cancer cells correlates specifically with expression of PKCι and Par6, the therapeutic target of ATM in lung cancer cells 5, 7.
Our data are reminiscent of the observed correlation between EGFR over-expression and/or EGFR mutation and sensitivity of NSCLC cells to TKI therapy 2, 3. We therefore assessed whether PRKCI mutations might likewise confer sensitivity to ATM. For this purpose, we sequenced exon 2 of PRKCI from genomic DNA prepared from our panel of cell lines. We focused on exon 2 of PRKCI because it encodes the PB1 domain of PKCι, including Cys69, the specific amino acid residue within PKCι targeted by ATM 7. However, no mutations were found (data not shown). We also sequenced the entire coding region of PRKCI from 40 primary NSCLC tumors and found no mutations that altered amino acid sequence (data not shown). We conclude that PRKCI mutations are either not present or very rare in NSCLC tumors and lung cancer cell lines. Our data do not support the hypothesis that ATM sensitivity is caused by somatic PRKCI mutations.
NSCLC tumors that express PKCι to levels similar to those observed in ATM sensitive cell lines might represent a subset of lung cancer patients likely to respond to ATM therapy. In order to assess whether NSCLC patients with this molecular characteristic exist, we analyzed 96 cases of primary NSCLC (60 LAC and 36 LSCC cases) for PKCι mRNA abundance by QPCR (Figure 1D). A significant subset of tumors (41/96 or 43%) exhibited PKCι expression at or above the level of expression seen in ATM sensitive cell lines (vertical lines indicate the lower and upper range of ATM sensitive lines). A higher percentage of SCC cases (23/36 or 64%) than LAC cases (18/60 or 30%) expressed high PKCι, however there exists a relatively small subset of LAC cases (5/60 or 8%) with extremely high PKCι expression (above the range observed in ATM sensitive cell lines). Thus, a significant subset of primary LSCC and LAC tumors express PKCι levels that in lung cancer cell lines correlate with ATM sensitivity.
ATM sensitivity is not due to general sensitivity to cytotoxic therapeutic agents
ATM sensitivity could be associated with a general sensitivity to chemotherapeutic agents. To assess this possibility, two ATM-sensitive cell lines (A427 and H1703) and two insensitive cell lines (H460 and A549), were evaluated for response to the conventional cytotoxic agents commonly used in lung cancer treatment, cis-platin, placitaxel and gemcitabine. Each line was assessed for anchorage-independent growth in the presence of the cytotoxic drugs and IC50 values calculated (Table 2). Whereas the four cell lines exhibit dramatically different sensitivities to ATM (ranging from 0.3 µM to > 100 µM), their sensitivity to cytotoxic agents did not vary widely; and the relatively small differences observed did not correlate with ATM sensitivity. These data indicate that ATM sensitivity is not a result of general drug sensitivity in ATM responsive cells.
Table 2.
ATM Sensitivity does not Correlate with Response to Cytotoxic Therpeutics
| IC50 for Inhibition of Anchorage Independent Growth | ||||
|---|---|---|---|---|
| Cell Line | ATM (µM) | Cisplatin(µM) | Taxol(nM) | Gemcitabine (nM) |
| A427 | 0.3 | 1.2 | 1.4 | 1.1 |
| H1703 | 1.3 | 0.5 | 0.8 | 1.4 |
| H460 | 43 | 0.2 | 1.3 | n.d. |
| A549 | 107 | 1.9 | 1.4 | 4.1 |
ATM sensitivity in vitro predicts responsiveness to ATM therapy in vivo
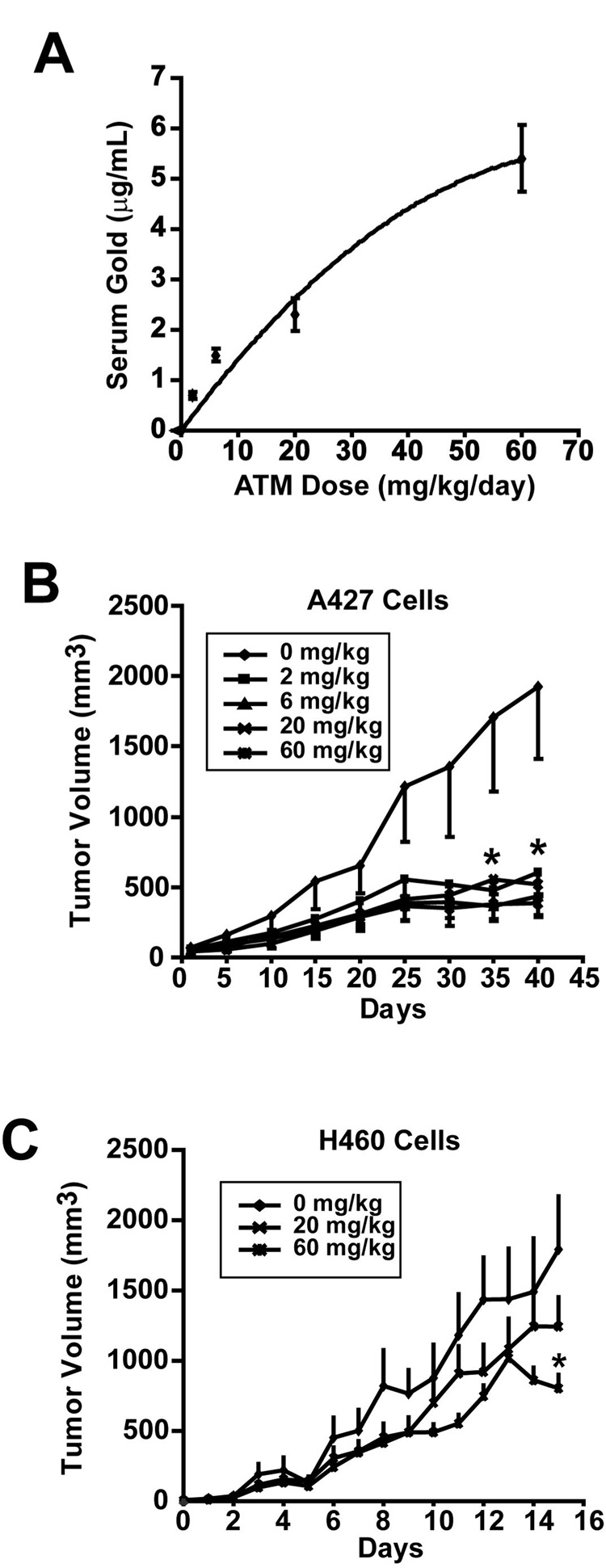
We next assessed the effect of ATM on lung cancer cell tumorigenicity in vivo. A427 and H460 cell lines were chosen for analysis because they differ significantly in ATM sensitivity and grow efficiently as subcutaneous tumors in nude mice. To establish appropriate dosing regimens for ATM we administered ATM by intraperitoneal injection at doses of 0, 2, 6, 20 and 60 mg/kg body weight daily for two weeks, at which time mice were sacrificed, blood drawn and serum gold levels determined by a clinically-approved serum gold assay (Figure 2A). No signs of toxicity were observed in these mice. Serum gold levels exhibited a linear relationship over this dose range and drug levels achieved were consistent with the range of serum gold (3–5 µg/mL) typically observed in RA patients undergoing ATM therapy 11. Serum gold levels of 3–5 µg/mL correspond to ATM concentrations of 15.4–25.6 µM, well within the range of ATM concentrations exhibiting inhibitory effects on anchorage-independent growth of NSCLC cell lines in vitro. We next assessed the ability of ATM to inhibit lung cancer cell tumorigenicity at these dose levels. Subcutaneous A427 or H460 cell tumors were established in nude mice and then treated with ATM or diluent (PBS) daily at the indicated doses. A427 cell tumors were highly responsive to ATM, exhibiting statistically significant inhibition of tumor growth at all concentrations tested (Figure 2B). These data indicate an apparent in vivo IC50 below 2.5 µM in A427 cells consistent with the in vitro IC50 of 0.3 µM. H460 tumors were less responsive to ATM, showing a statistically significant response (~50% reduction in tumor size) only at the 60 mg/kg dose (Figure 2C). These data suggest an approximate IC50 for ATM in H460 cells of ~25.6 mM, in line with the in vitro IC50 of 46 µM. Thus, ATM exhibits significant anti-tumor activity in two independent in vivo models of lung cancer at clinically relevant serum drug concentrations. Furthermore, the relative sensitivity of A427 and H460 cells to ATM in vitro was reflected in their response to ATM in vivo.
Figure 2. ATM inhibits lung tumor growth in vivo.
A. Serum gold levels in mice. Nude mice were injected with ATM intramuscularly at the indicated concentration daily for 14 days, at which time, blood was drawn and serum analyzed for drug (gold) levels. Values represent the mean serum level +/−SEM; n=8. B. Effect of ATM on A427 tumor growth in vivo. Nude mice were injected subcutaneously with 1 × 107 A427 cells. Once palpable tumors were established, mice were randomly assigned to one of 5 treatment groups receiving ATM at 0, 2, 6, 20 or 60 mg/kg daily in sterile PBS (diluent). Tumors were measured and tumor volumes calculated as described in Materials and Methods. Values represent the mean tumor volume +/− SEM; n=6. *denotes a statistically significant difference in tumor volume at all ATM doses compared to diluent with P-values <0.05. C. Effect of ATM on H460 tumor growth in vivo. Nude mice were injected subcutaneously with 5 × 106 H460 cells. Once palpable tumors were established, mice were randomly assigned to three treatment groups receiving 0, 20 or 60 mg/kg ATM daily and analyzed as described in B. above. Values represent the mean tumor volume +/− SEM; n=6. * denotes statistically significant difference from diluent with P-value <0.05.
ATM treatment inhibits lung tumor cell proliferation
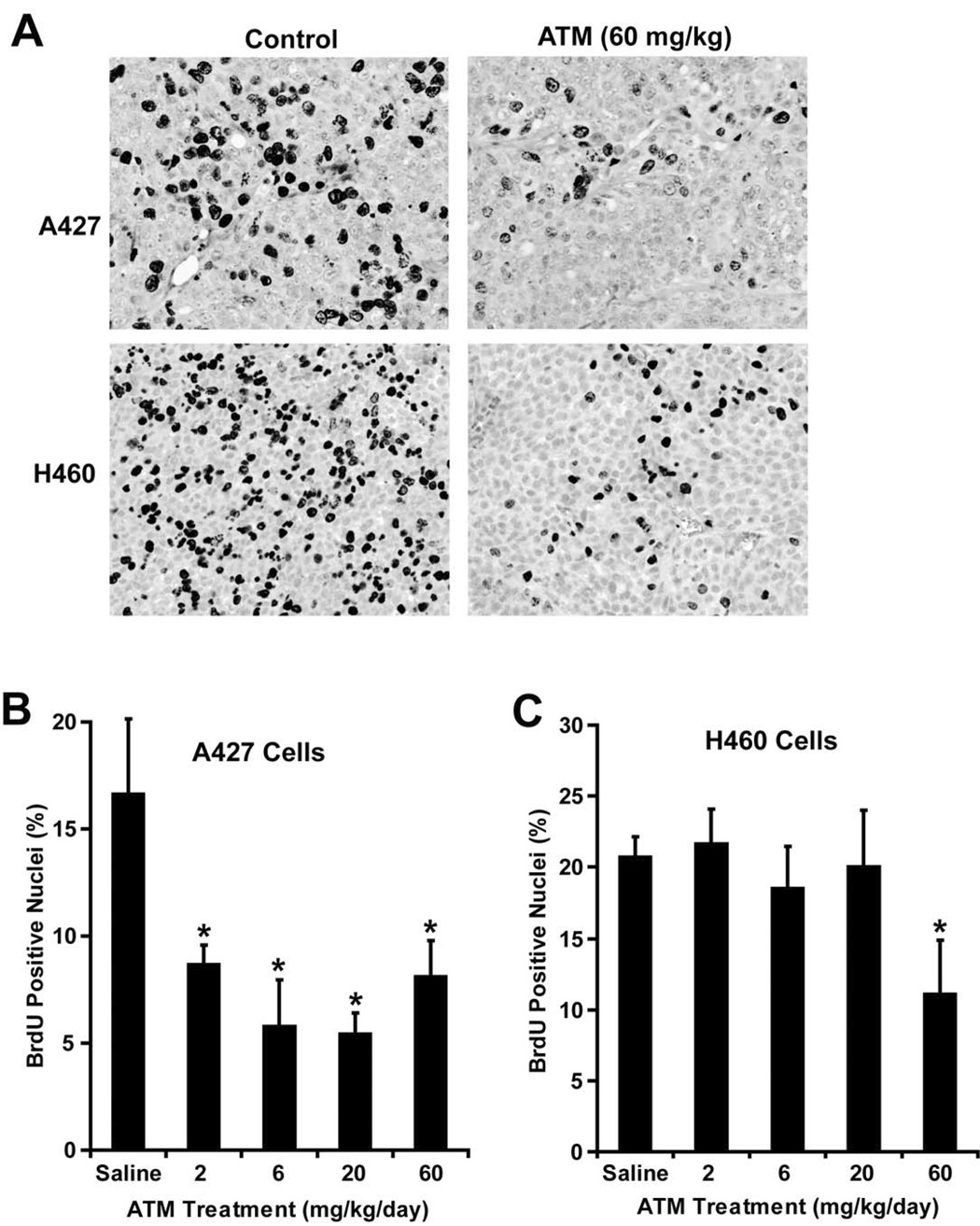
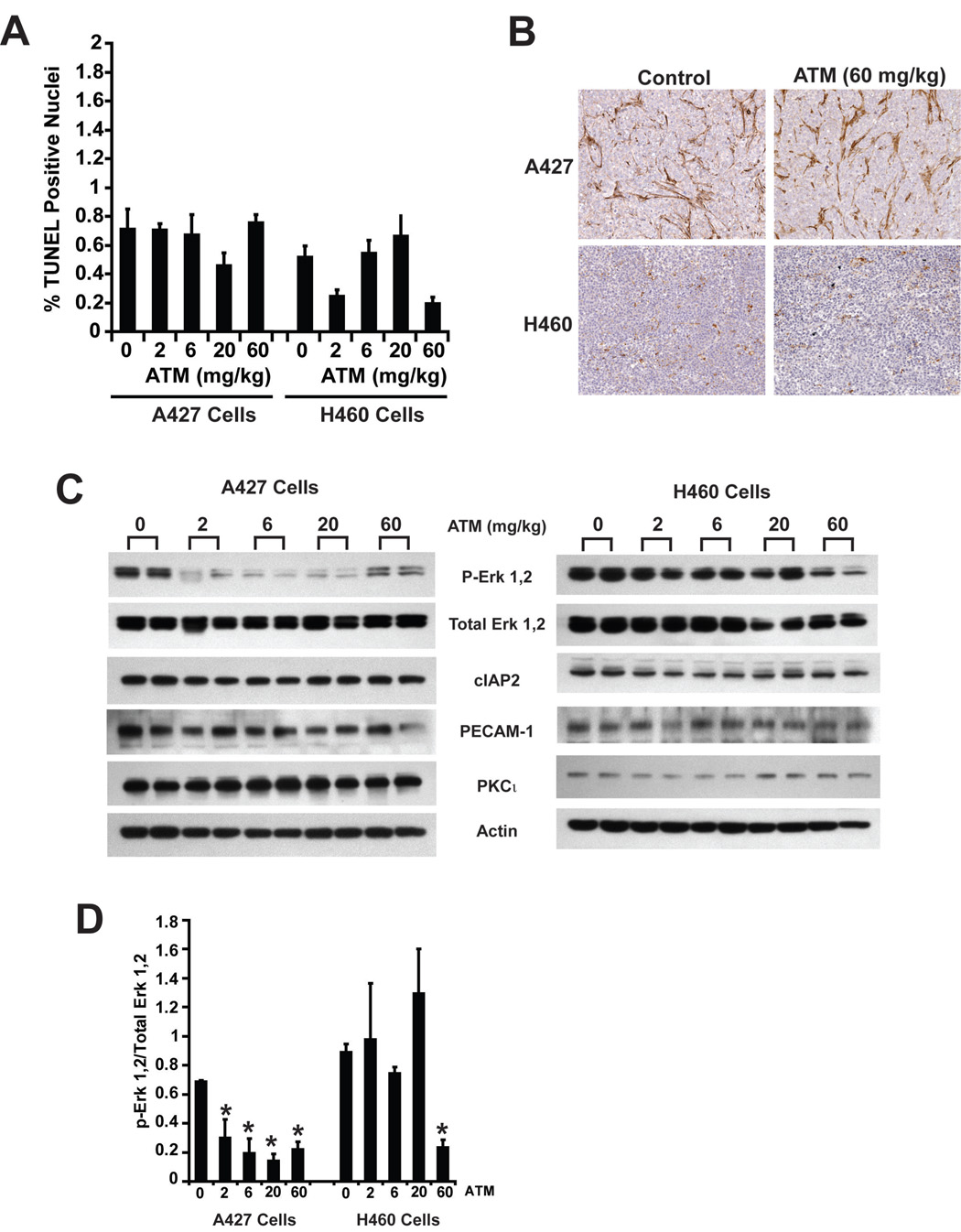
The inhibitory effect of ATM on tumor growth in vivo might result from either decreased cell proliferation, decreased cell survival or a combination of these mechanisms. Therefore, we assessed the effect of ATM on cellular proliferation by BrdU labeling, and apoptosis by TUNEL staining. Immunohistochemical analysis demonstrated a decrease in BrdU-positive staining nuclei in both A427 and H460 tumors cells after treatment with 60 mg/kg ATM (Figure 3A). Quantitative analysis of BrdU labeling demonstrated a statistically significant decrease in BrdU labeling in A427 tumors at all ATM doses, consistent with the observed inhibition of tumor growth (Figure 3B). In H460 tumors, a statistically significant decrease in BrdU-labeling was seen only at the 60 mg/kg dose, consistent with the observed effect of ATM on H460 cell tumor growth (Figure 3C). Quantitative analysis of TUNEL staining revealed that the apoptotic index (defined as TUNEL-positive cells/total cells) was very low (< 1%) in both A427 and H460 tumors and that ATM did not induce a significant increase in apoptotic index in either cell line (Figure 4A). Consistent with this finding, A427 and H460 tumor lysates showed no change in expression of cIAP2, an anti-apoptotic protein whose expression is commonly induced in tumor cells exposed to apoptotic stimuli (Figure 4C). These data indicate that the growth inhibitory effects of ATM are due predominantly to inhibition of cell proliferation without significant induction of tumor cell apoptosis.
Figure 3. ATM inhibits tumor cell proliferation in vivo.
Mice harboring A427 and H460 tumors treated with saline or ATM at the indicated doses were injected intraperitoneally with BrdU 60 minutes prior to sacrifice. Tumor tissues were excised and processed for immunoblot and immunohistochemical analysis as described in Materials and Methods. A. ATM inhibits BrdU incorporation into A427 and H460 tumors. Immunohistochemistry of representative sections of A427 and H460 tumors treated with saline (control) or 60 mg/kg ATM. B. and C. Quantitative analysis of BrdU labeling was performed on A427 (B) and H460 (C) tumors treated with saline or ATM at the indicated doses. Data represent BrdU-positive nuclei expressed as the percent of total nuclei. Values are given as mean +/− SEM; n=6. * denotes a statistically significant difference (P < 0.05) from saline-treated controls.
Figure 4. ATM inhibits tumor cell proliferation without affecting tumor cell apoptosis or tumor vascularity.
A. ATM does not induce apoptosis in lung cancer tumors. A427 and H460 tumors treated with the indicated doses of ATM were stained by TUNEL and apoptotic index (% TUNEL positive nuclei) was calculated. Values represent the mean +/− SEM; n=6. B. ATM does not affect tumor vascularity. Sections of fixed and paraffin-embedded A427 and H460 tumors from mice treated with either diluent (control) or 60 mg/kg ATM were subjected to immunohistochemical analysis for the endothelial cell marker PECAM1. Representative sections are shown. C A427 (top) and H460 (bottom) tumor extracts from animals treated with the indicated doses of ATM were subjected to immunoblot analysis using antibodies to phospho-Erk 1,2, Erk 1,2, cIAP2, PECAM1, PKCι and actin. and D. ATM inhibits phosphorylation of Erk 1,2 in vivo. y A427 and H460 tumor extracts from mice treated with the indicated doses of ATM were subjected to immunoblot analysis and phospho-Erk 1,2 and total Erk 1,2 levels quantitated by densitometry. Data are expressed as the ratio of phospho-Erk to total Erk and represent the mean +/− SD; n=3. * denotes a statistically significant difference (P < 0.04) from saline-treated controls.
It is possible that ATM decreases tumor cell proliferation indirectly by inhibiting tumor vascularization. To assess this possibility, A427 and H460 cell tumors were stained for the endothelial cell marker PECAM1 (Figure 4B). The pattern and intensity of PECAM1 staining in A427 and H460 tumors treated with 60 mg/kg ATM was indistinguishable from untreated control tumors. Immunoblot analysis of A427 and H460 cell tumors from ATM-treated and control tumors showed no significant change in tumor-associated PECAM1 expression (Figure 4C). We conclude that the anti-tumorigenic effects of ATM are mediated through direct inhibition of tumor cell proliferation in vivo and not tumor cell apoptosis or tumor vascularization.
ATM inhibits the Mek/Erk proliferative signaling axis in vivo
Genetic disruption of PKCι signaling inhibits anchorage-independent growth of A549 NSCLC cells in vitro by blocking activation of the PKCι-Par6-Rac1-Pak-Mek 1,2-Erk 1,2 proliferative signaling axis 6. ATM inhibits anchorage-independent growth by selectively targeting the PB1 domain of PKCι 7 and blocking oncogenic PKCι signaling to Rac1 5. To assess whether ATM inhibits the Mek/Erk pathway in A427 and H460 tumors in vivo, we determined phospho-Erk 1,2 and total Erk 1,2 levels in control and ATM-treated tumors by immunoblot analysis (Figure 4C). A427 and H460 cell tumors from ATM-treated mice exhibited reduced levels of phospho-Erk 1,2 when normalized to total Erk (phospho-Erk/total Erk) (Figure 4D). A statistically significant reduction in phospho-Erk 1,2 was seen in A427 tumors at all ATM doses, and in H460 cell tumors at the 60 mg/kg ATM dose, consistent with the growth inhibitory effects of ATM in these cells. These data are consistent with ATM-mediated inhibition of proliferative signaling through the PKCι-activated Mek/Erk signaling axis.
DISCUSSION
Lung cancer is the leading cause of cancer mortality in the United States 1. Lung cancer accounts for a third of all cancer deaths and claims over 160,000 lives annually. Despite best available treatments, prognosis for NSCLC patients is poor. This dismal clinical outlook has prompted a search for more effective strategies to treat NSCLC. The EGFR TKIs have emerged as a highly effective therapy in a small subset of NSCLC patients 3, 12. Molecular analysis revealed that TKIs are dramatically effective in the subset of lung cancers that harbor EGFR mutation, EGFR amplification and/or over-expression of EGFR 3. Patients with lung tumors exhibiting these molecular characteristics tend to be non-smokers, Asian and those diagnosed with lung adenocarcinoma 12. However, these characteristics define a relatively small subset of total lung cancer cases and there is a need to identify more effective therapeutic approaches to treat the substantial subset of lung cancers which are not responsive to TKI therapy.
We recently demonstrated that the atypical PKC isozyme, PKCι, is an oncogene that drives anchorage-independent growth of NSCLC cells through activation of a proliferative PKCι-Par6-Rac1-Pak-Mek-Erk signaling axis 4, 6. We also identified ATM as a potent inhibitor of oncogenic PKCι signaling, that inhibits anchorage-independent growth and tumorigenicity of NSCLC cells 5, 7. The current studies were conducted to determine the efficacy of ATM against major subtypes of lung cancer, identify molecular characteristics of lung cancer cells that correlate with ATM responsiveness, and determine whether ATM is an effective treatment in pre-clinical models of lung cancer in vivo at drug concentrations achievable in humans.
Our results demonstrate that ATM exhibits growth inhibitory activity in cell lines representing the major forms of lung cancer. LSCC and SCLC cell lines tended to be more sensitive to ATM than LAC and LCC cells. Our results provide proof of principle for targeting the oncogenic PKCι signaling pathway in a mechanism-based approach to the treatment of lung cancer. Of particular interest, both SCLC cell lines in our study exhibited high sensitivity to ATM. SCLC is difficult to treat and few therapeutic options exist for the substantial number of SCLC patients that fail standard therapy. Our results indicate that ATM should be explored as a new mechanism-based therapy for SCLC. Analysis of the prevalence of PKCι over-expression in SCLC and ATM sensitivity in an expanded collection of SCLC cell lines will be the subject of future investigation.
The overriding molecular characteristic correlating with ATM response in our studies is expression of PKCι and Par6, the therapeutic target of ATM. Tumor cells expressing high levels of these proteins are very sensitivity to ATM therapy in vitro and in vivo. PKCι and Par6 are coordinately over-expressed in lung cancer cells, indicating that the PKCι-Par6 interaction is a critical oncogenic signaling complex and relevant therapeutic target. It is likely that other molecular and biological characteristics of lung cancer cells can influence ATM response, however our data indicate that PKCι expression profiling could be useful in identifying likely responders to ATM therapy. Our previous studies demonstrated that PKCι is over-expressed in ~70% of primary NSCLC tumors 4. In LSCC tumors, PKCι expression is driven by tumor-specific PRKCI amplification. Our current results indicate that ATM may be particularly effective in lung tumors that harbor PRKCI amplification since the two most ATM responsive tumor cell lines in our study harbor PRKCI amplification. This finding has important implications for the clinical use of ATM since PRKCI amplification and PKCι over-expression is a frequent event in squamous carcinomas of the head and neck 13, esophagus 14, 15, ovary 16–18 and cervix 19. Thus, ATM may be an effective therapeutic approach in these tumors.
PKCι over-expression is not confined to tumor cells harboring PRKCI amplification. PKCι over-expression is prevalent in both LAC and LSCC despite the fact that PRKCI amplification is largely confined to LSCC tumors 4. Furthermore, the two SCLC cell lines analyzed here over-express PKCι and exhibit high ATM sensitivity but do not harbor PRKCI amplification. These data argue that PKCι over-expression, rather than PRKCI gene amplification per se, is an important characteristic of ATM response. Our analysis indicates that some 40% of primary NSCLC tumors express PKCι at or above the levels associated with ATM sensitivity. This observation suggests that a substantial subset of lung cancer patients may benefit from ATM therapy. Interestingly, when considered as a whole, LAC and LSCC tumors over-express PKCι to similar levels 4. However, PKCι expression profiling of individual LAC and LSCC tumors reveals a different pattern of PKCι over-expresssion in these tumor types. Whereas a majority of LSCC tumors over-express PKCι, two distinct populations of LAC tumors emerge; a majority of LAC cases that express relatively low PKCι and a small subset (accounting for about 8% of our patient cohort) that express extremely high PKCι. Based on our current findings, this latter subset of LAC may be particularly responsive to ATM. There are likely to be multiple factors that influence ATM sensitivity and response in vivo. However, our present results provide a compelling rationale for the clinical development of ATM for the treatment of lung cancer, and provide a molecular basis for patient stratification in ongoing clinical trials of ATM.
Supplementary Material
ATM Sensitivity, PKCι mRNA Abundance and PKCι Protein Expression in Lung Cancer Cell Lines Each of the eight lung cancer cell lines in our panel were assessed for PKCι mRNA abundance by QPCR and PKCι protein expression by immunoblot analysis. mRNA abundance is expressed as 2−Ct PKCι−Ct18S); PKCι protein expression is expressed in optical density units normalized to PKCι expression in A549 cells.
ACKNOWLEDGEMENTS
We gratefully acknowledge Capella Weems, Aaron Bungum, Dr. Eric Edell and Dr. Andras Khoor for assistance in acquisition, annotation, pathologic characterization, processing and analysis of human lung cancer tissue samples, Pam Kreinest and Brandy Edenfield for immunohistochemical analyses and members of the Fields laboratory for helpful comments and critical review of the manuscript. This work was supported in part by grants to A.P.F. from the National Institutes of Health (CA81436) and the American Lung Association/LUNGevity Lung Cancer Discovery Award. R.P.R. is recipient of a Ruth L. Kirschstein National Research Service Award (NRSA) from the National Cancer Institute.
REFERENCES
- 1.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.Sequist LV, Bell DW, Lynch TJ, Haber DA. Molecular predictors of response to epidermal growth factor receptor antagonists in non-small-cell lung cancer. J Clin Oncol. 2007;25:587–595. doi: 10.1200/JCO.2006.07.3585. [DOI] [PubMed] [Google Scholar]
- 3.Bell DW, Lynch TJ, Haserlat SM, et al. Epidermal growth factor receptor mutations and gene amplification in non-small-cell lung cancer: molecular analysis of the IDEAL/INTACT gefitinib trials. J Clin Oncol. 2005;23:8081–8092. doi: 10.1200/JCO.2005.02.7078. [DOI] [PubMed] [Google Scholar]
- 4.Regala RP, Weems C, Jamieson L, et al. Atypical protein kinase C iota is an oncogene in human non-small cell lung cancer. Cancer Res. 2005;65:8905–8911. doi: 10.1158/0008-5472.CAN-05-2372. [DOI] [PubMed] [Google Scholar]
- 5.Stallings-Mann M, Jamieson L, Regala RP, Weems C, Murray NR, Fields AP. A novel small-molecule inhibitor of protein kinase Ciota blocks transformed growth of non-small-cell lung cancer cells. Cancer Res. 2006;66:1767–1774. doi: 10.1158/0008-5472.CAN-05-3405. [DOI] [PubMed] [Google Scholar]
- 6.Regala RP, Weems C, Jamieson L, Copland JA, Thompson EA, Fields AP. A typical protein kinase Ciota plays a critical role in human lung cancer cell growth and tumorigenicity. J Biol Chem. 2005;280:31109–31115. doi: 10.1074/jbc.M505402200. [DOI] [PubMed] [Google Scholar]
- 7.Erdogan E, Lamark T, Stallings-Mann M, et al. Aurothiomalate inhibits transformed growth by targeting the PB1 domain of protein kinase Ciota. J Biol Chem. 2006;281:28450–28459. doi: 10.1074/jbc.M606054200. [DOI] [PubMed] [Google Scholar]
- 8.Murray NR, Jamieson L, Yu W, et al. Protein kinase Ciota is required for Ras transformation and colon carcinogenesis in vivo. J Cell Biol. 2004;164:797–802. doi: 10.1083/jcb.200311011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sakurai A, Yuasa K, Shoji Y, et al. Overexpression of thioredoxin reductase 1 regulates NF-kappa B activation. J Cell Physiol. 2004;198:22–30. doi: 10.1002/jcp.10377. [DOI] [PubMed] [Google Scholar]
- 10.Becker K, Gromer S, Schirmer RH, Muller S. Thioredoxin reductase as a pathophysiological factor and drug target. Eur J Biochem. 2000;267:6118–6125. doi: 10.1046/j.1432-1327.2000.01703.x. [DOI] [PubMed] [Google Scholar]
- 11.Blocka KL, Paulus HE, Furst DE. Clinical pharmacokinetics of oral and injectable gold compounds. Clin Pharmacokinet. 1986;11:133–143. doi: 10.2165/00003088-198611020-00003. [DOI] [PubMed] [Google Scholar]
- 12.Sequist LV, Joshi VA, Janne PA, et al. Response to treatment and survival of patients with non-small cell lung cancer undergoing somatic EGFR mutation testing. Oncologist. 2007;12:90–98. doi: 10.1634/theoncologist.12-1-90. [DOI] [PubMed] [Google Scholar]
- 13.Snaddon J, Parkinson EK, Craft JA, Bartholomew C, Fulton R. Detection of functional PTEN lipid phosphatase protein and enzyme activity in squamous cell carcinomas of the head and neck, despite loss of heterozygosity at this locus. Br J Cancer. 2001;84:1630–1634. doi: 10.1054/bjoc.2001.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Imoto I, Pimkhaokham A, Fukuda Y, et al. SNO is a probable target for gene amplification at 3q26 in squamous-cell carcinomas of the esophagus. Biochem Biophys Res Commun. 2001;286:559–565. doi: 10.1006/bbrc.2001.5428. [DOI] [PubMed] [Google Scholar]
- 15.Pimkhaokham A, Shimada Y, Fukuda Y, et al. Nonrandom chromosomal imbalances in esophageal squamous cell carcinoma cell lines: possible involvement of the ATF3 and CENPF genes in the 1q32 amplicon. Jpn J Cancer Res. 2000;91:1126–1133. doi: 10.1111/j.1349-7006.2000.tb00895.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang L, Huang J, Yang N, et al. Integrative genomic analysis of protein kinase C (PKC) family identifies PKCiota as a biomarker and potential oncogene in ovarian carcinoma. Cancer Res. 2006;66:4627–4635. doi: 10.1158/0008-5472.CAN-05-4527. [DOI] [PubMed] [Google Scholar]
- 17.Eder AM, Sui X, Rosen DG, et al. Atypical PKCiota contributes to poor prognosis through loss of apical-basal polarity and cyclin E overexpression in ovarian cancer. Proc Natl Acad Sci U S A. 2005;102:12519–12524. doi: 10.1073/pnas.0505641102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weichert W, Gekeler V, Denkert C, Dietel M, Hauptmann S. Protein kinase C isoform expression in ovarian carcinoma correlates with indicators of poor prognosis. Int J Oncol. 2003;23:633–639. [PubMed] [Google Scholar]
- 19.Sugita M, Tanaka N, Davidson S, et al. Molecular definition of a small amplification domain within 3q26 in tumors of cervix, ovary, and lung. Cancer Genet Cytogenet. 2000;117:9–18. doi: 10.1016/s0165-4608(99)00135-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ATM Sensitivity, PKCι mRNA Abundance and PKCι Protein Expression in Lung Cancer Cell Lines Each of the eight lung cancer cell lines in our panel were assessed for PKCι mRNA abundance by QPCR and PKCι protein expression by immunoblot analysis. mRNA abundance is expressed as 2−Ct PKCι−Ct18S); PKCι protein expression is expressed in optical density units normalized to PKCι expression in A549 cells.