Abstract
A patient presented with a unilateral dislocated condyle that was resistant to reduction by simple manual manipulation because of elevator muscle spasm and severe muscle and temporomandibular joint pain. A technique involving a masseteric nerve block and a temporal nerve block was used, allowing a quick, safe, and minimally painful reduction. The method used for delivering these nerve blocks is described here.
Keywords: Masseteric nerve block, Deep temporal, Temporomandibular joint dislocation, TMJ reduction, TMJ subluxation, Open lock
Introduction
Various procedures and maneuvers can cause a condylar dislocation. Yawning or opening widely is one causative factor, especially in patients with generalized joint hypermobility.1,2 Dislocation also can occur during bronchoscopy,3 laryngoscopy,4 or general anesthetic procedures.5,6 Treatment for acute mandibular condylar dislocation consists of manual reduction through a downward and posterior application of force to the mandible. The downward force clears the condyle of the articular eminence, and the posterior force re-seats the condyle within the glenoid fossa.7
Two major factors hamper this procedure: elevator muscular spasm with resistance of manual distraction of the head of the mandibular condyle from the articular eminence, and pain in and around the joint capsule.8 If the dislocation is prolonged, pain and spasticity of the elevator muscles will occur.9 Various methods have been used to counter the pain and/or spasm, but these are not without limitations. One commonly used method is asking the patient to open widely, or to open against resistance. Through reciprocal inhibition, the muscle tone of the elevator muscles is reduced, and manual reduction (described above) can be attempted concurrently.1 This method is often successful, although not always. Another approach is to use muscle relaxants to reduce spasm. However, the oral form takes up to 1 hour to begin reducing muscle tone, and the effect may be insufficient for a reduction procedure. In addition, swallowing a pill may be difficult for a patient with an open lock. The muscle relaxant can be given intravenously, but most general dentists do not have the necessary equipment for, nor are they familiar with, administering drugs through that route.7 Sedatives have also been used. Oral sedatives have limitations similar to those of muscle relaxants. IV sedation is effective but, as with IV muscle relaxants, requires a special setup with monitoring that is not found in most general dentists' offices. Local anesthetic around the joint capsule decreases joint pain, but it decreases neither muscle pain nor muscle spasm.
In refractory cases, the patient may be placed under general anesthesia to allow manual reduction. When this fails, temporal myotomy7 or midline mandibulotomy10 methods have been used.
The purpose of this report is to describe briefly a new method in which masseteric and deep temporal nerve blocks are used for the reduction of mandibular dislocation. These peripheral blocks are unique in that they reduce both masseter and temporalis muscle pain and spasms, and they do so quickly and efficiently. These blocks may improve the chance of successful reduction, thereby averting the need for consideration of general anesthesia and/or surgical correction. The longer the condyle remains dislocated, the more difficult reduction will be. As time goes on, pain and muscle spasms increase, and reduction is hampered.9 If the procedure is prolonged further, fibrosis begins, which adds to the difficulty of reduction.11 Therefore, it is very important that the provider use a quick and reliable method to reduce difficult dislocations.
Methods
An 84-year-old Chinese woman presented to the Emergency Department at the University of Medicine and Dentistry; she described severe pain on the right side of her face in the region of the temporomandibular joint (TMJ). She could neither close nor open her mouth normally without pain. Her present condition had started approximately 7 to 9 hours earlier, after she yawned. She reported a history of dislocations over the past 25 years, with the most recent event occurring 90 days earlier. At that time, she was able to reduce the luxation herself, but she presented to the Emergency Department because of associated pain. This time, however, she was able to reduce only the left mandibular condyle on her own; the right mandibular condyle, because of exquisite pain and spasm, remained luxated.
Visual examination of the patient revealed swelling in the right malar region. Clinical examination detected a bony protrusion on the right side under the zygomatic arch anterior to the TMJ, consistent with a dislocated condyle. Digital palpation of the protuberance and of the temporalis and masseter muscles elicited extremely painful withdrawal responses. A panoramic radiograph confirmed that the right mandibular condyle (Figure 1) was displaced to a position anterior and superior to the articular eminence.
Figure 1.
Section of panoramic radiograph showing dislocated right condyle.
The first attempt to manually reduce the right condyle failed because the process of applying intraoral downward and posterior pressure triggered intolerable pain. IV sedation was suggested but was not provided because of the patient's advanced age.
A second approach of reducing the right condyle by using peripheral nerve blocks of the masseteric and deep temporal nerves, as well as local infiltration over the lateral TMJ capsule, was suggested. A 30-gauge needle was used to inject approximately 0.6 mL of 2% lidocaine with 1:100,000 epinephrine lateral to the right TMJ capsule, to achieve anesthesia of the lateral joint capsular ligament. Epinephrine has a tendency to irritate muscle tissue; therefore, these injections all were placed around nerves, and not in muscle.
Another 0.6 mL of 2% lidocaine with 1:100,000 epinephrine was used for the masseteric nerve block, which will be described shortly.
Finally, 0.6 mL of 2% lidocaine with 1:100,000 epinephrine was injected deep to the temporalis muscle, in the area of the anterior temporalis muscle; the injection site is located in the depression that represents the greater wing of the sphenoid bone. The needle was inserted through the temporalis muscle to contact bone. Anesthetic then was delivered to block the deep temporal nerve.
Aspiration was done during all injections to avoid intravenous placement of the anesthetic.
Approximately 2 minutes elapsed between the last injection and any attempted manipulation, to allow anesthesia and paralysis to take effect. Then, in a manner similar to that used by the Emergency Department dentist previously, pressure was applied to the mandible in a downward and posterior direction. Although the patient continued to experience increased pain during the procedure, pain intensity was markedly decreased. Muscular contraction also had diminished significantly, allowing a relatively quick reduction.
The patient was instructed to limit the use of her jaw. It is advised that the patient limit jaw use for at least 1 week, to allow repair of the capsule and ligaments, thereby preventing dislocation while they were still loose.7
Discussion
Methods used previously to reduce muscle spasm and joint pain have several limitations. Masseteric and deep temporal nerve blocks are relatively simple and safe injections that can aid in reducing pain and spasm in the masseter and temporalis muscles, caused by a dislocated mandibular condyle. Sensory and motor nerve branches are blocked. This aids reduction in 2 ways: it relaxes the spasm, and it lessens the pain. The very action of lessening the pain also reduces the force of the spasm, because pain causes reflexive muscle guarding.8
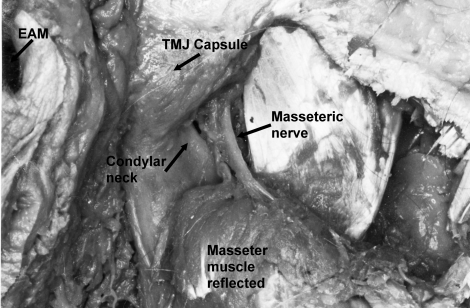
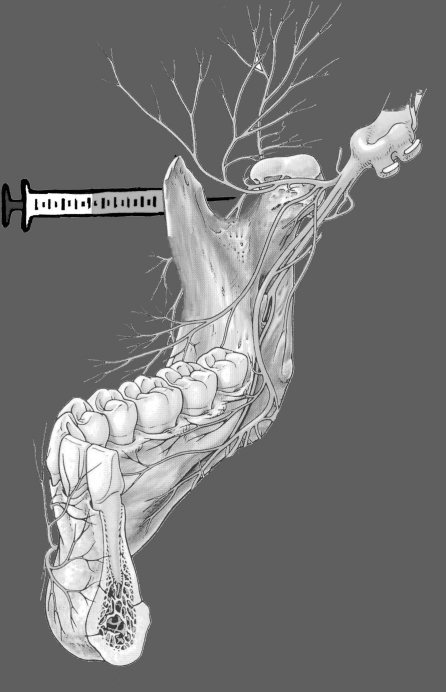
The masseteric nerve penetrates the masseter after it passes through the mandibular notch (Figure 2). Consequently, the mandibular notch is the ideal point at which the anesthetic can be delivered, to achieve maximum anesthetic effect on the masseter muscle.12 The technique used for this injection is as follows: The width of the ramus is visualized by grasping the anterior and posterior borders with the thumb and middle finger (Figure 3). The index finger from the same hand then locates the zygomatic arch at a point halfway between the thumb and the middle finger (Figure 4). The index finger then moves inferiorly until it reaches the mandibular notch (Figure 5). The needle is introduced posterior to the index finger, while the practitioner attempts to hit the neck of the condyle (Figures 6 and 7). For this patient, who has a petite build, the needle was advanced approximately 8 mm. The anesthetic was deposited at this point.
Figure 2.
Dissection of the right masseteric nerve. The masseteric nerve branches off from the mandibular division of the trigeminal nerve, then passes through the mandibular notch before penetrating the masseter.
Figure 3.
Visualization of the width of the ramus by grasping the anterior and posterior borders with the thumb and middle finger.
Figure 4.
The index finger locates the zygomatic arch at a point halfway between the thumb and the middle finger.
Figure 5.
The index finger moves inferiorly until it reaches the mandibular notch.
Figure 6.
The needle is introduced posterior to the index finger; hitting the neck of the condyle is attempted.
Figure 7.
Image of needle insertion, toward the neck of the condyle.
Deep temporal nerve block is achieved by first locating the anterior temporalis muscle. This muscle is palpated just above the zygomatic bone, where a depression can be felt. Deep to this portion of the temporalis muscle is the greater wing of the sphenoid bone. The anesthetic needle is directed into this area until it hits the sphenoid bone. Anesthetic is delivered without withdrawal of the needle, because the deep temporal nerves course along the surface close to the bone.
Johnson described a similar technique, which he used to reduce 17 patients.13 He entered the skin from a point superficial to the glenoid fossa, then moved the needle in an anterior direction until he contacted the posterior surface of the condylar neck.
TMJ hypermobility is a major risk factor for condylar dislocation. Patients with systemic joint hypermobility are likely to have hypermobility localized to the TMJ as well.2 Eighty-three percent of patients in a 100-person study had condyles at or anterior to the eminence at a normal opening range.14
If necessary, sedation may be used in addition to masseteric and deep temporal nerve blocks. Should this fail, general anesthesia with manual reduction, or the use of slow traction wires, is another option.7 More invasive procedures that may be considered after this include temporal myotomy7 and sagittal split mandibular osteotomy.15
If dislocation becomes recurrent, surgical treatments to prevent dislocation should be considered; these involve increasing the height of the articular eminence to prevent the condyle from passing to the anterior side of the eminence,16 or reducing the eminence to allow spontaneous reduction when the condyle passes anteriorly.17
We describe here a new approach in which masseteric nerve block, deep temporal nerve block, and lateral joint infiltration are used to reduce pain and spasms during manual reduction of a luxated mandible. This technique is quick, safe, and easy to implement. Continued treatment of dislocations through this approach will shed further light on the advantages and disadvantages of this method.
Footnotes
Address correspondence to Dr Andrew L Young, 110 Bergen Street, Reception Area 12, Room D-881, University Heights, Newark, New Jersey, e-mail: andrewyoungdds@yahoo.com
References
- Pertes R.A, Gross S.G. Clinical Management of Temporomandibular Disorders and Oroafacial Pain. Chicago: Quintessence; 1995. p. 266. [Google Scholar]
- Kavuncu V, Sahin S, Kamanli A, Karan A, Cihan A. The role of systemic hypermobility and condylar hypermobility in the temporomandibular joint dysfunction syndrome. Rheumatol Int. 2006;26:257–260. doi: 10.1007/s00296-005-0620-z. [DOI] [PubMed] [Google Scholar]
- Kim S.K, Kim K. Subluxation of the TM joint: unusual complications of transoral bronchoscopy. Chest. 1983;83:288–289. doi: 10.1378/chest.83.2.288b. [DOI] [PubMed] [Google Scholar]
- Schwartz A.J. Dislocation of the mandible: a case report. AANA J. 2000;68:507–513. [PubMed] [Google Scholar]
- Sosis M, Lazar S. Jaw dislocation during general anesthesia. Can J Anaesth. 1987;34:407–408. doi: 10.1007/BF03010145. [DOI] [PubMed] [Google Scholar]
- Lipp M, von Domarus H, Daublander M, Leyser K.H, Dick W. Effects of intubation anesthesia on the temporomandibular joint. Anesthetist. 1987;36:442–445. [PubMed] [Google Scholar]
- Laskin D.M, Greene C.S, Hylander W.L. TMDs: An Evidence-Based Approach to Diagnosis and Treatment. Chicago: Quintessence; 2006. p. 415. [Google Scholar]
- Littler B.O. The role of local anesthesia in reduction of long-standing dislocation of the temporomandibular joint. Br J Oral Surg. 1980;18:81–85. doi: 10.1016/0007-117x(80)90056-6. [DOI] [PubMed] [Google Scholar]
- Caminiti M.F, Weinberg S. Chronic mandibular dislocation: the role of non-surgical and surgical treatment. J Can Dent Assoc. 1998;64:484–491. [PubMed] [Google Scholar]
- Lee S.H, Son S.I, Park J.H, Park I.S, Nam J.H. Reduction of prolonged bilateral temporomandibular joint dislocation by midline mandibulotomy. Int J Oral Maxillofac Surg. 2006;35:1054–1056. doi: 10.1016/j.ijom.2006.03.023. [DOI] [PubMed] [Google Scholar]
- Hayward J.R. Prolonged dislocation of the mandible. J Oral Surg. 1965;23:585–594. [PubMed] [Google Scholar]
- Quek S.Y, Grunwerg B.S. The masseteric nerve block for masseter muscle pain—a clinical note. Quintessence Int. In press. [PubMed]
- Johnson W.B. New method for reduction of acute dislocation of the temporomandibular articulations. J Oral Surg. 1958;16:501–504. [PubMed] [Google Scholar]
- Sheppard I.M, Sheppard S.M. Range of condylar movement during mandibular opening. J Prosthet Dent. 1965;15:263–271. doi: 10.1016/0022-3913(65)90096-x. [DOI] [PubMed] [Google Scholar]
- Smith W.P, Johnson P.A. Sagittal split mandibular osteotomy for irreducible dislocation of the temporomandibular joint: a case report. J Oral Maxillofacial Surg. 1994;23:16–18. doi: 10.1016/s0901-5027(05)80319-4. [DOI] [PubMed] [Google Scholar]
- Dautrey J. Reflections sur la chirurgie de l/articulation temporomandibulaire. Acta Stom Belg. 1975;72:577–581. [PubMed] [Google Scholar]
- Myrhaug H. A new method of operation for habitual dislocation of the mandible. Acta Odont Scand. 1951;9:247–261. doi: 10.3109/00016355109012789. [DOI] [PubMed] [Google Scholar]