Abstract
Childhood-onset obsessive-compulsive disorder (OCD) affects 1%–2% of children and adolescents. It is characterized by recurrent obsessions and compulsions that create distress and interfere with daily life. The symptoms reported by children are similar to those seen among individuals who develop OCD in adulthood, and the two groups of patients are treated with similar symptom-relieving behavior therapies and medications. However, there are differences in sex ratios, patterns of comorbidity, and the results of neuroimaging studies that might be important. Here we review the diagnosis and treatment of childhood-onset OCD in light of pediatric and adult studies. We also discuss current knowledge of the pathophysiology of the disorder. Despite advances in this area, further research is needed to understand better the etiopathogenesis of the disorder and to develop new, more effective therapeutic options.
Introduction
The Diagnostic and Statistical Manual of Mental Disorders (4th edition) (DSM-IV) defines obsessive-compulsive disorder (OCD) in both adults and children as recurrent obsessions or compulsions that are time consuming or cause marked distress or significant impairment in daily functions (1). The DSM-IV further states that obsessions are recurrent and intrusive thoughts, ideas, images, or impulses that cause marked anxiety and distress (1). Common obsessions in children include preoccupations with contamination, harm to self or others, and symmetry, as well as fear that a bad outcome will occur if a ritual is not completed in just the right way (1). In addition, compulsions are defined as repetitive behaviors or mental acts that prevent or reduce anxiety caused by an obsession (1). Common compulsions in children include washing, checking, and ordering rituals (1). These are often repeated a set number of times but also may be tic-like behaviors that are repeated until the person feels “just right.” In 1997, Leckman and colleagues used the “just-right” characteristic and other behaviors to identify four phenomenological subtypes of childhood-onset OCD based on the child’s symptoms: obsessions and checking; symmetry and ordering; cleanliness and washing; and hoarding (2). The Yale-Brown obsessive-compulsive scale (Y-BOCS) and the children’s Y-BOCS (CY-BOCS) further categorize the symptoms of OCD in adults and children, respectively, by providing a specific measure of the severity of the symptoms that is not influenced by the type of obsessions or compulsions present (3). This measurement is used to determine baseline symptom severity and response to treatment (3). The Y-BOCS and CY-BOCS scales are very similar and differ only in the miscellaneous obsessions and compulsions categories, which in the CY-BOCS scale contain the same questions, but broken down into three categories: magical thoughts/superstitious obsessions, excessive game playing/superstitious behavior (i.e., stepping over certain spots on the floor to avoid something bad), and miscellaneous obsessions and compulsions (4).
The DSM-IV criteria allow the diagnosis of OCD to be made even for patients with poor insight into their condition, i.e., if they do not recognize that their obsessions or compulsions are excessive or unreasonable (1). This is especially relevant in the diagnosis of childhood-onset OCD, since young children often lack insight into the irrationality of their actions (5). Further, more than one-third of adults and about 40% of children diagnosed with OCD deny that their compulsions are driven by obsessive thoughts (6, 7). In 1998, Eisen and colleagues developed the Brown Assessment of Beliefs Scale (BABS), a clinician-administered scale designed to assess, for a range of psychiatric disorders, the insight patients have into their condition and found that 30% of adults with OCD had limited insight (8). This 30% of adults is thought to constitute a possible subgroup of individuals with adult-onset OCD, defined by a poorer prognosis and resistance to treatment (5). Findings from a recent study on pediatric OCD suggest that the prognosis of children with poor insight is worse than that of children with good insight (9). Lack of insight militates against the benefits of cognitive-behavioral therapy (CBT), as the patient is less willing to resist the urge to perform a compulsion (a crucial element of the therapy, as discussed later). Poor insight has also been reported among adults who initially present with OCD but go on to meet criteria for schizophrenia or other psychiatric disorders (10).
In this Review, we focus on childhood-onset OCD, discussing the characteristics, epidemiology, treatment, and pathophysiology of the disorder. Where knowledge is limited in this population, we draw from studies of patients with adult-onset OCD, which provide potential insight that can be further investigated in the pediatric population.
Childhood-onset OCD and associated comorbidities
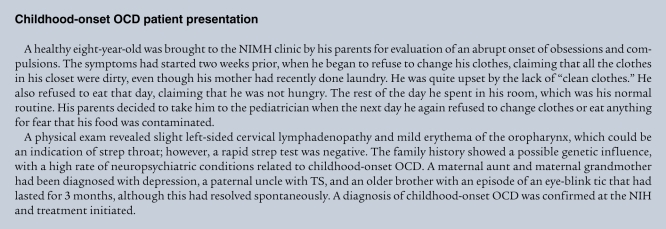
OCD is characterized as childhood-onset if symptoms present before puberty, whereas adult OCD starts during or after puberty. At puberty, the sex ratio of affected individuals switches from predominantly males to predominantly females (11, 12). Common comorbidities also change, from the attention-deficit/hyperactivity disorder (ADHD) and tics that are associated with childhood-onset OCD to depression and anxiety for those that develop OCD during or after puberty (13). However, the division between childhood- and adult-onset OCD is not clear-cut, and many prepubertal children have a more “adult” presentation. The symptoms can begin abruptly (see Childhood-onset OCD patient presentation) or begin subtly and slowly increase in severity.
Although childhood-onset OCD is generally similar to adult-onset OCD (14), as mentioned above there are some important differences in symptom presentation, patterns of comorbidity, and sex distribution. In addition, there appear to be differences in degree of insight and etiopathogenesis. With regard to symptom presentation and comorbidities, children are more likely than adults to have simple tic-like compulsions and to have comorbid tics and ADHD (7, 13). The relationship between OCD and motor and vocal tics, including Tourette syndrome (TS), is complex. Motor tics often have a premonitory urge similar to that seen with compulsive rituals, while the compulsions of childhood-onset OCD often lack obsessional triggers. Distinguishing between tics and compulsions is particularly difficult when the rituals are simple, repetitive movements such as tapping and touching. Further, comorbidity is common, with nearly two-thirds of children with OCD observed to have comorbid tics (11) and 20%–80% of children with TS reporting obsessive-compulsive symptoms (2). Studies in children with smaller caudate volumes and tic-related OCD and/or TS have demonstrated more severe symptoms and poorer outcomes with treatment (15). It is difficult to clearly differentiate the symptoms of OCD and TS, but studies suggest that the compulsions associated with TS may be less severe than those in children with OCD (without comorbid tics) and are more likely to involve symmetry, rubbing, touching, staring, or blinking rituals than washing and cleaning (2).
Boys are more commonly affected by childhood-onset OCD then girls, and the ratio of occurrence is 2–3:1 (11). This ratio reverses in those diagnosed with the disorder during or after puberty, with a male-to-female ratio of 1:1.35 (12). In terms of sex differences, when compared with girls, boys with childhood-onset OCD have a higher rate of comorbid tic disorders (7), a higher frequency of compulsions not preceded by obsessions (16), and a greater genetic contribution to the disease, as shown in mono- and dizygotic twin studies (17). Some studies have provided evidence for pathophysiologically distinctive subtypes of OCD that vary according to symptoms that had their onset in childhood versus those that emerge de novo in adulthood (16, 18, 19). However, the evidence for distinct subtypes is scant, and longitudinal studies are currently being conducted to elucidate further the differences between childhood- and adult-onset OCD.
Early mono- and dizygotic twin studies as well as genetic studies using more recent techniques provide evidence that genes play a role in the manifestation of OCD (20–22). Unfortunately, many twin studies are single-case reports or small studies with very few participants, and larger studies are needed to generalize the results (20). In 2005, van Grootheest and colleagues reviewed the literature and concluded that, in children, obsessive-compulsive symptoms are heritable, with genetic influences in the range of 45%–65% (22). Results of gene studies have been mixed regarding the contribution to OCD of genes in the serotonergic and dopaminergic systems, since results have not been consistently replicated. However, the recent studies with the glutamate transporter gene SLCL1A1 have been replicated and are intriguing, given our current knowledge of pathophysiology (23, 24). Despite this recent progress, further research is needed to elucidate the contributions of genetics to both childhood- and adult-onset OCD.
Both adult- and childhood-onset OCD patients commonly have other psychopathologies. In a study of 1,078 adults with OCD in northern California, 75% were found to have one or more comorbid psychiatric diagnosis (25). Similarly, a study of the National Institutes of Mental Health (NIMH) childhood-onset OCD cohort revealed that only 26% of patients had OCD as a single diagnosis (7). The most common comorbidities in children are ADHD (34%–51%), major depression (33%–39%), tics (26%), specific developmental disabilities (24%), TS (18%–25%), oppositional defiant disorder (17%–51%), and overanxious disorder (16%) (25–27). In the NIMH cohort, rates were also increased relative to a control group for simple phobias (17%), adjustment disorder with depressed mood (13%), oppositional disorder (11%), conduct disorder (7%), separation anxiety disorder (7%), and enuresis/encopresis (4%) (26).
Epidemiology
Both adult- and childhood-onset OCD were once thought to be a rare condition affecting less than 1 in 1,000 individuals; however, advances in diagnosis and treatment of have led to increased identification of the disorder (28). The Epidemiological Catchment Area (ECA) study was the first large-scale epidemiological study to determine the incidence and prevalence of OCD in the adult population (29). It included more than 18,500 adults at five sites in the United States (New Haven, Connecticut; Baltimore, Maryland; St. Louis, Missouri; Durham, North Carolina; and Los Angeles, California) (29). With the use of the Diagnostic Interview Schedule (DIS), a structured interview administered by lay interviewers, lifetime prevalence rates ranging from 1.9% to 3.3% were demonstrated. The ECA study determined that the mean age of onset was 20–25 years, but one-half of the participants reported having initial symptoms in childhood or adolescence (30). Reported prevalence rates in pediatric patients range from 0.5% to 4.0% (31, 32). Community studies of children and adolescents demonstrate a lifetime prevalence of 1%–2.3% and a 1-year prevalence rate of 0.7% (1, 33). On average, the prevalence of OCD in adolescents is reported to be approximately 2% (34).
The similar prevalence rates of childhood- and adult-onset OCD (1%–2.3% and 1.9%–3.3%, respectively), despite new cases presenting in adults, suggest that childhood-onset OCD may remit as patients enter their adult years (1, 29). A metaanalysis of 16 study samples that had follow-up times of 1–15.6 years showed that pooled mean persistence rates following diagnosis of OCD in childhood were 41% for full OCD and 60% for full or subthreshold OCD (35). Three factors found to affect the chance of persistence into adulthood were age of OCD onset, necessity of in-patient care, and duration of disease. One or more comorbid psychiatric illness and poor initial treatment response were also prognostic of symptom persistence.
Treatment
CBT.
The optimum treatment for childhood-onset OCD is a combination of CBT and pharmacotherapy (36). CBT (specifically, exposure of the patient to the triggers of their obsessions and compulsions with response prevention) is well documented as a successful treatment of childhood-onset OCD (37). Both intensive (daily) and weekly CBT are effective treatments for childhood-onset OCD (38). Intensive treatment may have small immediate advantages over weekly CBT, but the methods have similar outcomes after 3 months (38). Interestingly, studies have shown that group CBT is as effective as individual CBT in children and adolescents with OCD, as long as the family is involved in the treatment approach (39).
The main objectives of CBT are identifying the triggers of obsessions and compulsions and designing personalized exposure and response prevention (ERP) strategies that can be practiced outside the therapy sessions (37, 40). In adults with OCD and partial response to treatment with a serotonin reuptake inhibitor, such as clomipramine or various selective serotonin reuptake inhibitors (SSRIs) (discussed below), the addition of ERP is an effective strategy for reducing OCD symptoms (41). The Pediatric OCD Treatment Study demonstrated that CBT was superior to medications as a sole therapy (36). Special techniques can help engage children in CBT. For example, in 1998, March and Mulle suggested emphasizing to the child that it is the OCD, not the child, that is the problem (42). The OCD may also be given a nickname, and the “good guys” (child, parent, and therapist) can fight the “bad guys” (the OCD) (37). The ultimate goal is to have the child not feel anxiety and not feel compelled to succumb to a compulsive ritual when exposed to the threatening stimulus. In order for this to be successful, the child needs to understand abstract concepts and be willing to experience temporary discomfort for ultimate future relief (43). The abstract concepts of CBT can be difficult to communicate to a child, but a study by Freeman and colleagues demonstrated that children (5–8 years old) with early-onset OCD benefit from CBT tailored to their developmental needs (child-friendly examples and terms such as the “worry monster”) and family context (family included in treatment) (44). Young OCD patients with good insight usually benefit from CBT as an initial treatment approach (9). Using both CBT and pharmacological treatment might be more effective for children with poor insight; however, this is a question that requires further research to answer. Insight may prove useful as a means of triaging to appropriate treatments (9).
Pharmacotherapies that inhibit reuptake of serotonin.
Drugs that inhibit the reuptake of the neurotransmitter serotonin by presynaptic cells and therefore increase the concentration of serotonin in the synapse have been successfully used to treat individuals with childhood-onset OCD for many years. These are currently thought to work by influencing structures in the cortico-striato-thalamo-cortical circuit (discussed below), especially in the caudate. This circuit is hypothesized to have a role in the regulation of obsessions and compulsions, but the specific details of the role of serotonin in OCD still need to be elucidated. Clomipramine was one of the first serotonin reuptake inhibitors to be used in adults and children with OCD (45–47). However, it does not selectively inhibit serotonin reuptake, as the SSRIs do. The SSRIs, which include fluoxetine, fluvoxamine, sertraline, and paroxetine, have fewer adverse side effects than clomipramine and have been shown in multicenter double-blind placebo-controlled trials to be effective at controlling OCD symptoms in the pediatric population (47). They are the drugs of choice for treating childhood-onset OCD (48). If one medication is found to be ineffective after an adequate trial (at least 10–12 weeks at maximum dose), a different SSRI is usually tried next. Only 50%–60% of adult patients respond to the initial SSRI with which they are treated; however, 70%–80% respond to at least one SSRI (49). Response rates seem to be similar in pediatric patients, although few experience complete symptom relief after treatment with CBT and SSRIs (27, 36). As yet, no standardized predictors for determining whether a patient with childhood-onset OCD will respond to treatment with an SSRI have been established, but studies have shown a poorer response among children with comorbid ADHD, oppositional defiant disorder, conduct disorder, and tic disorders (50), as well as those with more severe symptoms of OCD, higher parental stress, and greater functional impairment (51, 52). For adult patients who do not, or only partially, respond to SSRIs, a combination of an SSRI and a drug that antagonizes dopamine function (e.g., pimozide, haloperidol, and risperidone) has been shown to be beneficial (49). Investigation into whether a similar strategy will work for children is required. However, clomipramine should be considered for treatment or augmentation of treatment responses in more severe or treatment-resistant cases of childhood-onset OCD, as it seems to be the most efficacious agent overall (47).
The 2004 Pediatric OCD Treatment Study was the first randomized controlled trial to compare the efficacy of an established SSRI medication (sertraline) with the efficacy of CBT, the combination of CBT and sertraline, and a placebo, in the treatment of childhood-onset OCD (36). The 12-week trial was conducted at three academic centers in the United States (Duke University, the University of Pennsylvania, and Brown University), with a total of 112 participants (aged 7–17 years) with a primary DSM-IV diagnosis of OCD and a CY-BOCS score of 16 or higher. All three treatments were shown to be substantially more effective at reducing symptoms than placebo. Clinical remission was achieved in 54% of the patients who received combined treatment and in 40% and 21% who received CBT alone and sertraline alone, respectively, in comparison with 3% on placebo. The results of this trial suggest that children and adolescents with OCD should be treated first with CBT alone or with an SSRI and CBT in combination.
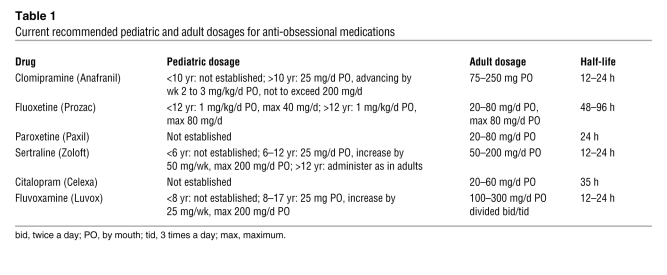
As for adults, it is recommended that SSRI treatment of children and adolescents with OCD should start with a low dose that is titrated up slowly over a few weeks to avoid adverse effects. Table 1 shows the current recommended pediatric and adult dosages for anti-obsessional medications. For both adults and children, the most common side effects of these drugs include sedation, nausea, diarrhea, insomnia, anorexia, tremor, and hyperstimulation (53, 54). Rare side effects include serotonin syndrome, apathy syndrome, extrapyramidal symptoms, and hypomania. In 2004, the FDA determined, based on 24 placebo-controlled trials involving more than 4,400 children and adolescents, that SSRIs may have the potential to increase the risk of suicidal thinking and behavior among pediatric patients (4% in the medication group and 2% in the placebo group) (55). The FDA therefore applied the “black box” warning universally to all antidepressants, including those that did not yield a single episode of suicidal thinking and behavior, simply because limited statistical power could not exclude the possibility that the absence of such events was due to small sample sizes and limited periods of observations (55). Even with this caveat, the risk-to-benefit ratio supports the use of SSRIs to treat childhood-onset OCD as well as other anxiety disorders, as the number of children with beneficial effects far outweighs that of children with adverse side effects (56).
Table 1 .
Current recommended pediatric and adult dosages for anti-obsessional medications
Other pharmacotherapies.
Clonazepam is a benzodiazepine with anxiolytic properties. It functions primarily by enhancing the activity of GABA, the principal inhibitory neurotransmitter in the CNS, but it also has serotonergic effects. The exact serotonergic mechanism is not known. Benzodiazepines have a rapid onset of action, whereas SSRIs may require several weeks or more for therapeutic effect. In a double-blind, placebo-controlled study of adults with OCD and comorbid anxiety disorders, benzodiazepines were shown to be efficacious when combined with an SSRI for patients who had a limited response to monotherapy with an SSRI (57, 58). The benefit in childhood-onset OCD still requires study, but case reports do support its utility (59).
Risperidone and other neuroleptics, many of which have highly specific antidopaminergic activity (through their ability to specifically block D2 and/or D3 receptors), have also been shown to be useful to treat adult-onset OCD when used in combination with an SSRI, as shown in a metaanalysis of multiple randomized placebo-controlled trials (60, 61). The neuroleptics are especially beneficial when OCD is associated with comorbid tic disorders or if the adult patients have poor insight into the irrationality of their obsessions (62–65). Research on the efficacy of neuroleptics as agents that augment treatment response for childhood-onset OCD is limited, but benefits for children with comorbid OCD and tic disorders has been demonstrated (2).
Riluzole, a glutamate antagonist, has shown possible benefit in some open-label trials in adults with OCD (66). A small open-label trial in children with OCD resistant to treatment with CBT and SSRIs found riluzole to be beneficial for 4 of 6 participants (67). A placebo-controlled trial of the drug in children with OCD is currently underway at the NIMH ( http://clinicaltrials.gov; trial no. NCT00251303).
Pathophysiology
Many of the treatments for childhood-onset OCD, in particular the pharmacotherapies, have numerous side effects, some of which can be severe. If we are to develop more targeted therapies with fewer side effects, it is important that we learn more about the pathophysiology of the disorder. This information might also help clinicians predict the response of a patient to different treatments and monitor their progress, as well as facilitate the development of effective prevention strategies.
Basal ganglia dysfunction.
The basal ganglia are a group of nuclei (caudate, putamen, globus pallidus interna [GPi], globus pallidus externa [GPe], substantia nigra, and subthalamic nucleus) in the brain that are interconnected with the cerebral cortex, thalamus, and brainstem and that are associated with functions such as motor control, cognition, emotions, and learning. The first identification of OCD resulting from basal ganglia dysfunction came from Constantin von Economo’s 1931 treatise on postencephalitic Parkinson disease, which described patients who experienced destruction of the basal ganglia as a result of severe influenza infections (68). Von Economo noted the “compulsory nature” of the motor tics and ritual-like behaviors and described his patients as “having to” act, while “not wanting to,” which is similar to current descriptions of individuals with OCD.
Research in the last two decades has shown that OCD may be associated with dysfunction of the cortico-striato-thalamo-cortical circuitry (69). A postulated model for such dysfunction in individuals with OCD (Figure 1) is that increased glutamatergic signals from the frontal cortex lead to increased excitation in the striatum (composed of the caudate and putamen), which increases inhibitory GABA signal to the GPi and the substantia nigra (pars reticulata) (SNr) (67, 69). This then decreases the inhibitory output via GABA from the GPi and SNr to the thalamus, resulting in thalamic excitatory glutamatergic output to the frontal cortex. This positive feedback loop could lead to repetitive thoughts (obsessions) and behaviors (compulsions) (67, 69). An indirect external loop composed of GPe and subthalamic nucleus is postulated to contribute to a steady state of excitation/inhibition in this model (67, 69). Two points in the circuit that can lead to the increased glutamatergic signal from the thalamus to the frontal cortex are the GPi/SNr interaction with the thalamus and the interactions between the striatum and GPe (67, 70). If the GPi/SNr is dysfunctional (Figure 1A), it cannot inhibit the thalamus, so the thalamus sends more glutamatergic signal (70). The relationship between this postulated dysfunction and the positive effects of SSRIs is unknown but might be explained by the numerous areas in which serotonergic neurons modulate activity. Similarly, if the striatum is dysfunctional, it cannot inhibit the GPe (Figure 1B), which then increases inhibition on the subthalamic nucleus, resulting in decreased excitation of GPi/SNr and decreased inhibition of the thalamus, so it sends more glutamatergic signals. Evidence supports the hypothesis that the caudate nucleus (part of the striatum) may be the site of this dysfunction (69). Functional neuroimaging studies in adults who were diagnosed with OCD in childhood provided direct evidence of this, demonstrating alterations in glucose metabolism in the caudate nucleus associated with OCD symptom severity and treatment response (71, 72). The caudate is densely innervated by serotonin-containing neurons (73). It is hypothesized to be the primary site of the effects of SSRIs in individuals with OCD and to be responsible for the preferential response of OCD patients to SSRIs (72, 74). Glutamatergic-serotonin modulation in the caudate nucleus may also be involved (75). In a functional cortico-striato-thalamo-cortical circuit (Figure 2), the thalamus receives signals from the GPi/SNr and thus sends fewer excitatory signals to the frontal cortex, decreasing the number of repetitive thoughts and behaviors. A review of the OCD functional brain imaging literature also reveals data suggesting abnormalities in the orbitofrontal cortex (76, 77), anterior cingulated gyrus, caudate, and thalamus, structures linked by well-described neuroanatomic circuits (69, 78). In addition, individuals with neurological disorders known to be caused by basal ganglia dysfunction, including TS, Sydenham chorea, and Huntington chorea, frequently exhibit obsessive-compulsive symptoms (79).
Figure 1. Model for the cortico-striato-thalamo-cortical circuit dysfunction in individuals with OCD.
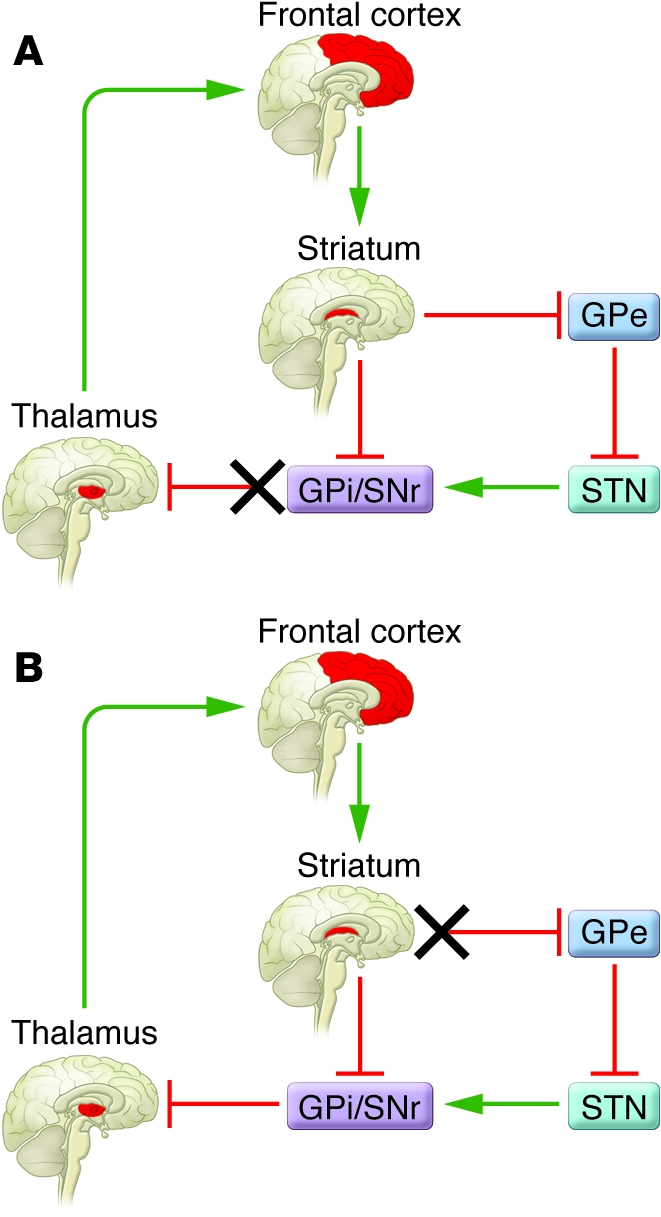
This model outlines the hypothesis that the cortico-striato-thalamo-cortical circuit is dysfunctional in individuals with OCD. Increased glutamatergic signals from the frontal cortex are hypothesized to increase excitation in the striatum, which increases inhibitory GABA signals to the GPi and SNr. (A) One possibility is that this then decreases the inhibitory output via GABA from the GPi and SNr to the thalamus, resulting in thalamic excitatory glutamatergic output to the frontal cortex. This positive feedback loop leads to repetitive thoughts (obsessions) and behaviors (compulsions). An indirect external loop composed of the GPe and subthalamic nucleus (STN) is postulated to contribute to a steady state of excitation/inhibition in this model. (B) A second possibility is that there is an unknown dysfunction at the striatum and GPe. Decreased inhibition on the GPe leads to increased inhibition of the STN, which decreases its excitation of the GPi/SNr. The GPi/SNr then decreases its inhibitory output on the thalamus, resulting in excitatory output to the frontal cortex (adapted from ref. 67).
Figure 2. The cortico-striato-thalamo-cortical circuit in a healthy individual.
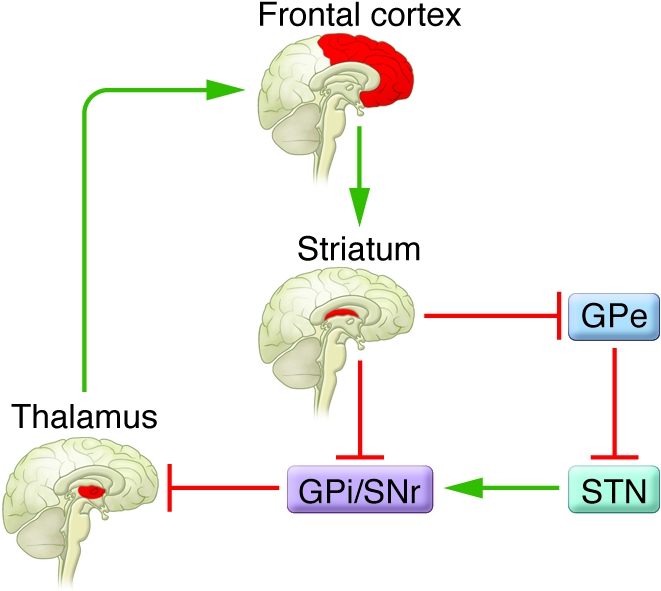
In the normally functioning cortico-striato-thalamo-cortical circuit, glutamatergic signals from the frontal cortex lead to excitation in the striatum, which increases inhibitory GABA signals to the GPi and the SNr. This then decreases the inhibitory output via GABA from the GPi and SNr to the thalamus, resulting in thalamic excitatory glutamatergic output to the frontal cortex. This is a positive feedback loop. An indirect external loop composed of the GPe and subthalamic nucleus (STN) is postulated to contribute to a steady state of excitation/inhibition. The striatum inhibits the GPe, which decreases its inhibition on the STN. The STN is then free to excite the GPi/SNr and therefore inhibit the thalamus (adapted from ref. 67).
Indirect evidence of basal ganglia dysfunction in both adults and children with OCD comes from observations of a decrease in OCD symptoms after psychosurgical lesions that disconnect the basal ganglia from the frontal cortex, as done in an anterior capsulotomy. Anterior capsulotomy has been used as a treatment for intractable OCD since the early 1950s, and in 1997, a supplement published in the Journal of Clinical Psychiatry (80) concluded that for adults with extremely severe and unremitting OCD, neurosurgical treatment to interrupt specific brain circuits that are malfunctioning could be helpful (81). In an anterior capsulotomy, bilateral basal lesions are made in the anterior limb of the internal capsule in the frontal lobe, interrupting the frontal-cingulate projections, but the surgical target lies within frontal-thalamic white matter between the caudate nucleus and putamen, which are part of the basal ganglia. Many studies have shown that psychosurgeries in adults with OCD substantially reduce obsessions and compulsions that were previously refractory to treatment (81). In general, psychosurgical procedures are not performed in children; however, Christensen and colleagues reported in 2002 a case of an 18-year-old boy with treatment-refractory OCD (no improvement with behavior or medication therapy) who improved substantially after capsulotomy (81). He was able to complete high school, and later married. Months after the procedure, he scored a 0 on the Y-BOCS and was on no medication. Despite the effectiveness of the psychosurgical procedures, it is important to note that this not conclusive evidence of a basal ganglia defect in OCD, since the defect could be anywhere upstream from the site of lesion (81, 82).
Examination of the brain with MRI using voxel-based morphometry has demonstrated greater orbital frontal gray matter volume in patients with childhood-onset OCD compared with healthy volunteers (83). Results have been inconclusive among adults, but this could be secondary to treatment effects, since reduction in gray matter has been noted after treatment with neuroleptics and other drugs (83). MRI studies among drug-naive patients with childhood-onset OCD compared with healthy volunteers have shown smaller globus pallidus volumes and more total gray matter in the anterior cingulate gyrus, a major limbic area contributing to emotions and drive-related behaviors (84). A smaller globus pallidus could conceivably decrease inhibition on the thalamus, resulting in the increased obsessions and compulsions present in individuals with childhood-onset OCD. More anterior cingulate gray matter in adults and children with OCD could reflect a neurodevelopmental abnormality and suggests new areas for investigation of etiopathogenesis (84). PET scans have demonstrated hypermetabolism in the cingulate cortex, thalamus, and pallidum/putamen complex in adults who were first diagnosed with OCD in childhood before treatment (85). After treatment with SSRIs, substantial improvement in obsessive-compulsive symptoms on the Y-BOCS scale was associated with a marked bilateral decrease in metabolism in the whole cingulate cortex. Functional MRI studies have provided additional support for the hypothesis that action-monitoring processes in both the rostral and caudal anterior cingulate cortex are hyperactive in adults with OCD (86). Similar investigations in children are needed to determine whether the same conclusions can be made in those with childhood-onset OCD. Elucidation of the exact dysfunction in the basal ganglia in childhood-onset OCD should lead to specifically targeted treatments and better symptom control.
Neurotransmitter abnormalities.
The hypothesis that abnormalities in serotonin function have a central role in the pathophysiology of both adult- and childhood-onset OCD is based primarily on the observation that serotonergic drugs effectively relieve symptoms of the disorder (87–89). Serotonin reuptake inhibitors, including clomipramine and SSRIs, have been the most effective medications in reducing OCD symptoms in children (90). In addition to blocking serotonin reuptake, the tricyclic antidepressant clomipramine blocks histamine H2, cholinergic, and adrenergic receptors and has antidopaminergic properties. The superior efficacy of clomipramine over desipramine — an anticholinergic drug that has antidepressant efficacy similar to that of clomipramine — in reducing OCD symptoms in both children and adults provides further support for hypothesizing a role for serotonin in OCD (45, 87, 88).
Research is still needed to determine the exact role of serotonin in the pathophysiology of OCD, but it has been demonstrated that the serotonin agonists sumatriptan (91) and meta-chlorophenylpiperazine (m-CPP) (92–94) can cause an acute exacerbation in OCD symptoms in adults. Due to ethical constraints, similar studies cannot be done in children. In contrast, OCD patients who received pretreatment with metergoline, a serotonin receptor antagonist, before m-CPP administration experienced no significant changes from baseline in OCD or other neuropsychiatric symptoms (94), providing further evidence that serotonin abnormalities have a role in the pathophysiology of OCD. Aberrations in serotonin do not, however, explain the entirety of the complex OCD puzzle.
Dopaminergic dysfunction in individuals with OCD is suggested by reports of obsessive-compulsive symptoms among adult patients with basal ganglia disorders such as TS, Sydenham chorea, and Huntington chorea (discussed above) (79); the increase in obsessive-compulsive symptoms following high-dose stimulant administration (95); and the utility of dopamine-blocking agents to augment treatment responses (rarely effective as primary therapy) in adults with OCD (49, 96, 97). A single-case report by Storch and colleagues in 2008 showed a substantial reduction in CY-BOCS scores in a 13-year-old boy following addition of low-dose aripiprazole, an antipsychotic with partial dopamine receptor agonist properties, to SSRI and CBT treatment, and he was eventually weaned off the SSRI (98). This case report is intriguing, but systematic investigations are required to confirm this effect. It is unclear whether OCD symptoms are exacerbated by an increase in dopamine or a decrease in serotonin inhibition, each of which would lead to an imbalance in dopamine and serotonin concentration that favored dopamine. There is evidence for both. For example, single photon emission computed tomography (SPECT) scans demonstrated enhanced dopamine transporter density in the left caudate and left putamen nuclei in drug-naive subjects with adult-onset OCD (99). In contrast, a primary lack of serotonin results in an inability to inhibit normal dopaminergic activity, leading to the manifestation of obsessions and compulsions (100). The beneficial effects of neuroleptics (dopamine antagonists) in treating children with SSRI-refractory OCD and those with a comorbid tic disorder also support a role for dopamine dysfunction in OCD (60, 65).
Glutamate (the primary excitatory neurotransmitter in the brain) plays a key role in the functioning of the fronto-striato-thalamo-cortical circuit. A recent report shows that cerebrospinal fluid samples from drug-naive patients with adult-onset OCD had substantially higher glutamate levels than samples taken from healthy volunteers (101). Further evidence is provided by two open-label trials of riluzole, a potent antiglutamatergic agent, which demonstrated benefits for 5 of 13 adult subjects with OCD and 4 of 6 children (61, 66). The therapeutic effects of riluzole are postulated to result from a reduction in frontal cortical excitatory output to the striatum, which would reduce the striatal inhibition of the globus pallidus and substantia nigra and allow greater inhibition of the thalamus, resulting in less cortical excitation.
Neuroimmune dysfunction.
The role of the immune system in the etiology and pathophysiology of OCD is still unclear, but parallels do exist between Sydenham chorea, the neurological manifestation of rheumatic fever, and childhood-onset OCD. Both have evidence of dysfunction of the cortico-striato-thalamo-cortical circuit, particularly in the orbitofrontal-striatal circuit, which is involved in the mediation of emotional responses to biologically significant stimuli (102, 103). It has been documented that exacerbation of obsessive-compulsive symptoms and tics can be triggered by a variety of infections. Group A β-hemolytic streptococci (GABHS) are the most studied initial autoimmune response–inciting event (discussed below), while others may include viruses (104), mycoplasma pneumonia (105), and Borrelia burgdorferi (106). Additionally, more than 70% of children with Sydenham chorea report that they experienced an abrupt onset of repetitive, unwanted thoughts and behaviors 2–4 weeks prior to the onset of the chorea (107). These psychiatric symptoms wane concomitantly with the neurologic improvements over a few months. A subgroup of patients with childhood-onset OCD has been noted to have a similar symptom course, i.e., the abrupt onset of OCD symptoms and their gradual resolution. Among these children, OCD symptoms began abruptly or worsened substantially following infection with GABHS and were accompanied by comorbid emotional lability, separation anxiety, and attention difficulties (108). Observations of the unique nature of the symptom onset and progression led to the identification of a subgroup of children with OCD known by the acronym PANDAS — pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (108). The PANDAS subgroup of childhood-onset OCD is defined by 5 clinical features: the presence of OCD and/or a tic disorder; prepubertal symptom onset; abrupt onset or exacerbation of symptoms with an episodic (relapsing-remitting) course; temporal association between presence of symptoms and infection with GABHS; and associated neurological abnormalities, including choreiform movements (103). The PANDAS profile is seen most often among young patients (6.5 ± 3 years for tics and 7.4 ± 2.7 years for OCD) and boys with the disorder outnumber girls 2.6 to 1 (103).
Psychiatric comorbidities are common among children with PANDAS. These include ADHD (40%), oppositional defiant disorder (40%), depression (36%), dysthymia (12%), sleep anxiety (20%), overanxiousness (28%), and enuresis (20%) (103). Additional symptoms during OCD exacerbations include choreiform movements (95%), emotional lability (66%), school performance changes (60%), personality changes (54%), bedtime fears (50%), fidgetiness (50%), separation fears (40%), sensory defensiveness (40%), irritability (40%), and impulsivity and distraction (38%) (103). The choreiform movements are most frequently present during symptom exacerbations and can be used to track the course of a child’s illness because they produce secondary deteriorations in handwriting.
The pathogenesis of obsessive-compulsive symptoms in the PANDAS subgroup of childhood-onset OCD is hypothesized to result from basal ganglia dysfunction produced by antibodies cross-reactive between GABHS epitopes and the human caudate (109). These antibodies are thought to induce calcium/calmodulin-dependent protein kinase II activity, increasing tyrosine hydroxylase activity and thereby dopamine release, which could result in neuropsychiatric symptoms (110). Systematic investigations suggest that obsessive-compulsive symptoms in the PANDAS subgroup of childhood-onset OCD result from a combination of regional and systemic immunological abnormalities (111). The occurrence of regional autoimmune reactions is suggested by the demonstration that monoclonal antibodies specific for mammalian lysoganglioside and N-acetyl-β-d-glucosamine (GlcNAc) (a dominant epitope of group A streptococci [GAS], including GABHS, carbohydrate) can be derived from the serum of patients with PANDAS (110). These monoclonal antibodies cross-react with neurons of the caudate, putamen, and globus pallidus (109, 110). Further, introduction of these antibodies into the basal ganglia of rats produced stereotypies, which are repetitive movements, sounds, or positions (i.e. wood-chip eating, self-gnawing, biting, licking not associated with grooming, repetitive paw-to-mouth movements, vacuous chewing, and head and paw shaking) (112, 113). Molecular mimicry has been suggested to be responsible for the effects of these antibodies. Several studies have shown the presence of similar cross-reactive antibodies in serum from patients with childhood-onset OCD and/or tic disorders (109, 114, 115). An interesting study by Liu and colleagues demonstrated a reduction in stereotypic behaviors in those rats microinfused intrastriatally with TS sera that then underwent transplantation with rat neural stem cells (116). Future TS research with stem cells holds great potential. Interestingly, serum from acutely ill individuals showed reactivity, while serum from those convalescing and after treatment with plasma exchange did not (117). Evidence in support of molecular mimicry as a cause of childhood-onset OCD and/or tic disorders comes from demonstrated efficacy of antibiotic prophylaxis against infection with GAS; the beneficial effects of immunomodulatory therapies, such as plasma exchange and intravenous Ig (IVIG); and the identification of neuron-specific antibodies in serum samples taken from acutely ill children.
The use of prophylactic penicillin is based on the hypothesis that if OCD and/or tics are sequelae of infection with GABHS, then preventing such infections should be effective in preventing post-streptococcal exacerbations of OCD and tics. In an 8-month-long placebo-controlled trial of penicillin prophylaxis for 37 children in the PANDAS subgroup of childhood-onset OCD, 35 GABHS infections occurred: 14 during penicillin and 21 during placebo administration (118). Thus, penicillin was not superior to placebo in preventing infection with GABHS, perhaps because of poor adherence to the two-times-a-day dosing schedule. Given the frequency of GABHS infections in both arms of the trial, it was not surprising that there were no substantial differences in OCD or tic severity. However, depression and anxiety symptoms were alleviated during the penicillin phase, and 15 of 20 parents rated penicillin better “overall” (118). A subsequent double-blind, parallel-design study of treatment with azithromycin and penicillin has also been completed (119). All 23 participants received either penicillin or azithromycin for 12 months. Both penicillin and azithromycin were found to be effective in preventing infections with GABHS and subsequent exacerbation of neuropsychiatric symptoms during the year of study observation (119).
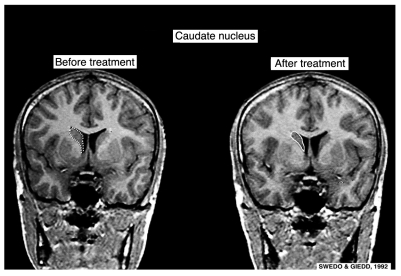
Evidence of systemic immune system involvement in the PANDAS subgroup of childhood-onset OCD is provided by the striking improvements in obsessive-compulsive symptoms following immunomodulatory therapies such as therapeutic plasma exchange and IVIG, which is hypothesized to remove the pathogenic cross-reactive antibodies (120). A controlled trial of plasma exchange versus IVIG versus placebo produced striking results — both plasma exchange and IVIG led to a substantial decrease in OCD severity one month after treatment when compared with placebo (120). At one-year follow-up, the CY-BOCS ratings were still below baseline for the treatment groups. A single-case study demonstrated decreased symptom severity and reduction in the size of the globus pallidus, caudate, and putamen following plasma exchange treatment for an acute OCD exacerbation (121). Subsequent MRI studies demonstrated enlargements of the caudate, putamen, and globus pallidus among symptomatic children with PANDAS and subsequent decrease in size after plasma exchange (Figure 3), compared with healthy volunteers (120–123). Because IVIG and plasma exchange both carry a substantial risk of adverse effects, use of these modalities should be reserved for children with particularly severe symptoms and a clear-cut PANDAS presentation. In general, children in the PANDAS subgroup of childhood-onset OCD can be treated with the same agents as those with idiopathic OCD; i.e., they will respond well to treatment with anti-obsessional medications and/or CBT. The PANDAS subgroup of childhood-onset OCD provides a uniquely homogeneous cohort of children in whom further research may elucidate the pathophysiology of their disorder as well as open avenues for research in the pathogenesis of all forms of childhood-onset OCD.
Figure 3. Serial T1-weighted brain MRIs of a 14-year-old male patient with severe worsening of OCD symptoms after an infection with GABHS.
MRI was performed before and after treatment with plasma exchange. Note the decreased caudate size after treatment (outlined with dotted and solid lines). This provides further support for basal ganglia–mediated dysfunction in OCD and the potential for immunological treatments for PANDAS. Adapted with permission from Oxford University Press (124).
Summary
Childhood-onset OCD is a chronic disabling disorder that warrants more clinical investigations. The exact pathophysiology has yet to be elucidated, but evidence points to dysfunction in the cortico-striato-thalamo-cortical circuitry and the serotonergic system. Current treatments with CBT and SSRIs have shown great efficacy, particularly when used in combination, but further investigations are needed to discover new effective treatments for children who have treatment-resistant OCD. Future research must elucidate the mysteries of both adult- and childhood-onset OCD if new, more effective treatments for these disorders are to be developed.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Nonstandard abbreviations used: ADHD, attention-deficit/hyperactivity disorder; CBT, cognitive-behavioral therapy; CY-BOCS, children’s Y-BOCS; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders (4th edition); GABHS, group A β-hemolytic streptococci; GPe, globus pallidus externa; GPi, globus pallidus interna; IVIG, intravenous Ig; OCD, obsessive-compulsive disorder; PANDAS, pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections; SNr, substantia nigra (pars reticulata); SSRI, selective serotonin reuptake inhibitor; TS, Tourette syndrome; Y-BOCS, Yale-Brown obsessive-compulsive scale.
Citation for this article: J. Clin. Invest. 119:737–746 (2009). doi:10.1172/JCI37563
References
- 1. American Psychiatric Association and American Psychiatric Association Task Force on DSM-IV. 2000.Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Association. Washington, DC, USA. 943 pp. [Google Scholar]
- 2.Leckman J.F., et al. Symptoms of obsessive-compulsive disorder. Am. J. Psychiatry. 1997;154:911–917. doi: 10.1176/ajp.154.7.911. [DOI] [PubMed] [Google Scholar]
- 3.Goodman W.K., et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch. Gen. Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 4.Poyurovsky M., Faragian S., Shabeta A., Kosov A. Comparison of clinical characteristics, co-morbidity and pharmacotherapy in adolescent schizophrenia patients with and without obsessive-compulsive disorder. Psychiatry Res. 2008;159:133–139. doi: 10.1016/j.psychres.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Storch E.A., et al. Clinical features associated with treatment-resistant pediatric obsessive-compulsive disorder. Compr. Psychiatry. 2008;49:35–42. doi: 10.1016/j.comppsych.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Karno M., Golding J.M., Sorenson S.B., Burnam M.A. The epidemiology of obsessive-compulsive disorder in five US communities. Arch. Gen. Psychiatry. 1988;45:1094–1099. doi: 10.1001/archpsyc.1988.01800360042006. [DOI] [PubMed] [Google Scholar]
- 7.Swedo S.E., Rapoport J.L., Leonard H., Lenane M., Cheslow D. Obsessive-compulsive disorder in children and adolescents. Clinical phenomenology of 70 consecutive cases. Arch. Gen. Psychiatry. 1989;46:335–341. doi: 10.1001/archpsyc.1989.01810040041007. [DOI] [PubMed] [Google Scholar]
- 8.Eisen J.L., et al. The Brown Assessment of Beliefs Scale: reliability and validity. Am. J. Psychiatry. 1998;155:102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- 9.Storch E.A., et al. Insight in pediatric obsessive-compulsive disorder: associations with clinical presentation. Psychiatry Res. 2008;160:212–220. doi: 10.1016/j.psychres.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Tumkaya S., et al. Schizophrenia with obsessive-compulsive disorder and obsessive-compulsive disorder with poor insight: a neuropsychological comparison. Psychiatry Res. 2009;165:38–46. doi: 10.1016/j.psychres.2007.07.031. [DOI] [PubMed] [Google Scholar]
- 11.Leonard H.L., et al. Tics and Tourette’s disorder: a 2- to 7-year follow-up of 54 obsessive-compulsive children. Am. J. Psychiatry. 1992;149:1244–1251. doi: 10.1176/ajp.149.9.1244. [DOI] [PubMed] [Google Scholar]
- 12.Castle D.J., Deale A., Marks I.M. Gender differences in obsessive compulsive disorder. Aust. N. Z. J. Psychiatry. 1995;29:114–117. doi: 10.3109/00048679509075899. [DOI] [PubMed] [Google Scholar]
- 13.Mancebo M.C., et al. Juvenile-onset OCD: clinical features in children, adolescents and adults. Acta Psychiatr. Scand. 2008;118:149–159. doi: 10.1111/j.1600-0447.2008.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bloch M.H., Landeros-Weisenberger A., Rosario M.C., Pittenger C., Leckman J.F. Meta-analysis of the symptom structure of obsessive-compulsive disorder. Am. J. Psychiatry. 2008;165:1532–1542. doi: 10.1176/appi.ajp.2008.08020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bloch M.H., Leckman J.F., Zhu H., Peterson B.S. Caudate volumes in childhood predict symptom severity in adults with Tourette syndrome. Neurology. 2005;65:1253–1258. doi: 10.1212/01.wnl.0000180957.98702.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Geller E., et al. Rasmussen encephalitis: complementary role of multitechnique neuroimaging. AJNR Am. J. Neuroradiol. 1998;19:445–449. [PMC free article] [PubMed] [Google Scholar]
- 17.Pauls D.L., Alsobrook J.P., 2nd, Goodman W., Rasmussen S., Leckman J.F. A family study of obsessive-compulsive disorder. Am. J. Psychiatry. 1995;152:76–84. doi: 10.1176/ajp.152.1.76. [DOI] [PubMed] [Google Scholar]
- 18.Eichstedt J.A., Arnold S.L. Childhood-onset obsessive-compulsive disorder: a tic-related subtype of OCD? Clin. Psychol. Rev. 2001;21:137–157. doi: 10.1016/S0272-7358(99)00044-6. [DOI] [PubMed] [Google Scholar]
- 19.Busatto G.F., et al. Regional cerebral blood flow abnormalities in early-onset obsessive-compulsive disorder: an exploratory SPECT study. . J. Am. Acad. Child Adolesc. Psychiatry. 2001;40:347–354. doi: 10.1097/00004583-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Pauls D.L. The genetics of obsessive compulsive disorder: a review of the evidence. Am J. Med. Genet. C Semin. Med. Genet. 2008;148:133–139. doi: 10.1002/ajmg.c.30168. [DOI] [PubMed] [Google Scholar]
- 21.Jonnal A.H., Gardner C.O., Prescott C.A., Kendler K.S. Obsessive and compulsive symptoms in a general population sample of female twins. Am. J. Med. Genet. 2000;96:791–796. doi: 10.1002/1096-8628(20001204)96:6<791::AID-AJMG19>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 22.van Grootheest D.S., Cath D.C., Beekman A.T., Boomsma D.I. Twin studies on obsessive-compulsive disorder: a review. Twin Res. Hum. Genet. 2005;8:450–458. doi: 10.1375/183242705774310060. [DOI] [PubMed] [Google Scholar]
- 23.Arnold P.D., Sicard T., Burroughs E., Richter M.A., Kennedy J.L. Glutamate transporter gene SLC1A1 associated with obsessive-compulsive disorder. Arch. Gen. Psychiatry. 2006;63:769–776. doi: 10.1001/archpsyc.63.7.769. [DOI] [PubMed] [Google Scholar]
- 24.Stewart S.E., et al. Association of the SLC1A1 glutamate transporter gene and obsessive-compulsive disorder. Am J. Med. Genet. B Neuropsychiatr. Genet. 2007;144B:1027–1033. doi: 10.1002/ajmg.b.30533. [DOI] [PubMed] [Google Scholar]
- 25.Fireman B., Koran L.M., Leventhal J.L., Jacobson A. The prevalence of clinically recognized obsessive-compulsive disorder in a large health maintenance organization. Am. J. Psychiatry. 2001;158:1904–1910. doi: 10.1176/appi.ajp.158.11.1904. [DOI] [PubMed] [Google Scholar]
- 26.Leonard H.L., et al. Obsessive-compulsive disorder and related conditions. Pediatr. Ann. 2001;30:154–160. doi: 10.3928/0090-4481-20010301-09. [DOI] [PubMed] [Google Scholar]
- 27.Geller D.A. Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatr. Clin. North Am. 2006;29:353–370. doi: 10.1016/j.psc.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 28.Weissman M.M., et al. The cross national epidemiology of obsessive compulsive disorder. The Cross National Collaborative Group. J. Clin. Psychiatry. 1994;55(Suppl.):5–10. [PubMed] [Google Scholar]
- 29.Robins L., Helzer J., Crougham J., Ratcliffe. K. The NIMH Epidemiological Catchment Area study. Arch. Gen. Psychiatry. . 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 30. Karno, M., and Golding, J. 1990. Obsessive-compulsive disorder. InPsychiatric disorders in America: the Epidemiologic Catchment Area Study. L.N. Robins and D.A. Regier, editors. The Free Press. New York, New York, USA. 204–219. [Google Scholar]
- 31.Wittchen H.U., Nelson C.B., Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol. Med. 1998;28:109–126. doi: 10.1017/S0033291797005928. [DOI] [PubMed] [Google Scholar]
- 32.Douglass H.M., Moffitt T.E., Dar R., McGee R., Silva P. Obsessive-compulsive disorder in a birth cohort of 18-year-olds: prevalence and predictors. J. Am. Acad. Child Adolesc. Psychiatry. 1995;34:1424–1431. doi: 10.1097/00004583-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Flament M.F., et al. Obsessive compulsive disorder in adolescence: an epidemiological study. J. Am. Acad. Child Adolesc. Psychiatry. 1988;27:764–771. doi: 10.1097/00004583-198811000-00018. [DOI] [PubMed] [Google Scholar]
- 34.Zohar A.H. The epidemiology of obsessive-compulsive disorder in children and adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 1999;8:445–460. [PubMed] [Google Scholar]
- 35.Stewart S.E., et al. Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr. Scand. 2004;110:4–13. doi: 10.1111/j.1600-0447.2004.00302.x. [DOI] [PubMed] [Google Scholar]
- 36.Pediatric OCD Treatment Study (POTS) Team. . Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA. 2004;292:1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- 37.Rapoport J.L., Inoff-Germain G. Treatment of obsessive-compulsive disorder in children and adolescents. J. Child Psychol. Psychiatry. 2000;41:419–431. doi: 10.1111/1469-7610.00627. [DOI] [PubMed] [Google Scholar]
- 38.Storch E.A., et al. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: comparison of intensive and weekly approaches. J. Am. Acad. Child Adolesc. Psychiatry. 2007;46:469–478. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- 39.Barrett P., Healy-Farrell L., March J.S. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. J. Am. Acad. Child Adolesc. Psychiatry. 2004;43:46–62. doi: 10.1097/00004583-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 40.Baer L., Greist J.H. An interactive computer-administered self-assessment and self-help program for behavior therapy. J. Clin. Psychiatry. 1997;58(Suppl. 12):23–28. [PubMed] [Google Scholar]
- 41.Simpson H.B., et al. A randomized, controlled trial of cognitive-behavioral therapy for augmenting pharmacotherapy in obsessive-compulsive disorder. Am. J. Psychiatry. 2008;165:621–630. doi: 10.1176/appi.ajp.2007.07091440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. March, J.S., and Mulle, K. 1998.OCD in children and adolescents: a cognitive-behavioral treatment manual. Guilford Press. New York, New York, USA. 298 pp. [Google Scholar]
- 43.Piacentini J. Cognitive behavioral therapy of childhood OCD. Child Adolesc. Psychiatr. Clin. N. Am. 1999;8:599–616. [PubMed] [Google Scholar]
- 44.Freeman J.B., et al. Early childhood OCD: preliminary findings from a family-based cognitive-behavioral approach. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:593–602. doi: 10.1097/CHI.0b013e31816765f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leonard H.L., et al. Treatment of obsessive-compulsive disorder with clomipramine and desipramine in children and adolescents. A double-blind crossover comparison. Arch. Gen. Psychiatry. 1989;46:1088–1092. doi: 10.1001/archpsyc.1989.01810120030006. [DOI] [PubMed] [Google Scholar]
- 46.[No authors listed]. . Clomipramine in the treatment of patients with obsessive-compulsive disorder. The Clomipramine Collaborative Study Group. Arch. Gen. Psychiatry. 1991;48:730–738. doi: 10.1001/archpsyc.1991.01810320054008. [DOI] [PubMed] [Google Scholar]
- 47.Geller D.A., et al. Which SSRI? A meta-analysis of pharmacotherapy trials in pediatric obsessive-compulsive disorder. Am. J. Psychiatry. 2003;160:1919–1928. doi: 10.1176/appi.ajp.160.11.1919. [DOI] [PubMed] [Google Scholar]
- 48.Grados M., Scahill L., Riddle M.A. Pharmacotherapy in children and adolescents with obsessive-compulsive disorder. Child Adolesc. Psychiatr. Clin. N. Am. 1999;8:617–634, x. [PubMed] [Google Scholar]
- 49.McDougle C.J. Update on pharmacologic management of OCD: agents and augmentation. J. Clin. Psychiatry. 1997;58(Suppl. 12):11–17. [PubMed] [Google Scholar]
- 50.March J.S., et al. Tics moderate treatment outcome with sertraline but not cognitive-behavior therapy in pediatric obsessive-compulsive disorder. Biol. Psychiatry. 2007;61:344–347. doi: 10.1016/j.biopsych.2006.09.035. [DOI] [PubMed] [Google Scholar]
- 51.Grados M., Riddle M.A. Do all obsessive-compulsive disorder subtypes respond to medication? Int. Rev. Psychiatry. 2008;20:189–193. doi: 10.1080/09540260801889153. [DOI] [PubMed] [Google Scholar]
- 52.Storch E.A., et al. Impact of comorbidity on cognitive-behavioral therapy response in pediatric obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:583–592. doi: 10.1097/CHI.0b013e31816774b1. [DOI] [PubMed] [Google Scholar]
- 53.March J.S., Curry J.F. Predicting the outcome of treatment. J. Abnorm. Child Psychol. 1998;26:39–51. doi: 10.1023/A:1022682723027. [DOI] [PubMed] [Google Scholar]
- 54.Riddle M.A., et al. Fluvoxamine for children and adolescents with obsessive-compulsive disorder: a randomized, controlled, multicenter trial. . J. Am. Acad. Child Adolesc. Psychiatry. 2001;40:222–229. doi: 10.1097/00004583-200102000-00017. [DOI] [PubMed] [Google Scholar]
- 55.Vasa R.A., Carlino A.R., Pine D.S. Pharmacotherapy of depressed children and adolescents: current issues and potential directions. Biol. Psychiatry. 2006;59:1021–1028. doi: 10.1016/j.biopsych.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 56.March J.S., Klee B.J., Kremer C.M. Treatment benefit and the risk of suicidality in multicenter, randomized, controlled trials of sertraline in children and adolescents. J. Child. Adolesc. Psychopharmacol. 2006;16:91–102. doi: 10.1089/cap.2006.16.91. [DOI] [PubMed] [Google Scholar]
- 57.Hollander E., Kaplan A., Stahl S.M. A double-blind, placebo-controlled trial of clonazepam in obsessive-compulsive disorder. World J. Biol. Psychiatry. 2003;4:30–34. doi: 10.3109/15622970309167908. [DOI] [PubMed] [Google Scholar]
- 58.Pigott, T.A., L’Heureux, F., and Rubenstein, C. 1992. A controlled trial of clonazepam augmentation in OCD patients tested with clomipramine or fluoxetine [abstract no. 144]. Presented at the 145th Annual Meeting of the American Psychiatric Association. May 2–7. Washington, DC, USA. T.A. Pigott, editor. American Psychiatric Association. Washington, DC, USA. 82 pp. [Google Scholar]
- 59.Leonard H.L., et al. Clonazepam as an augmenting agent in the treatment of childhood-onset obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry. 1994;33:792–794. doi: 10.1097/00004583-199407000-00003. [DOI] [PubMed] [Google Scholar]
- 60.Skapinakis P., Papatheodorou T., Mavreas V. Antipsychotic augmentation of serotonergic antidepressants in treatment-resistant obsessive-compulsive disorder: a meta-analysis of the randomized controlled trials. Eur. Neuropsychopharmacol. 2007;17:79–93. doi: 10.1016/j.euroneuro.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 61.Saxena S., Wang D., Bystritsky A., Baxter L.R., Jr. Risperidone augmentation of SRI treatment for refractory obsessive-compulsive disorder. J. Clin. Psychiatry. 1996;57:303–306. [PubMed] [Google Scholar]
- 62.Bloch M.H., et al. A systematic review: antipsychotic augmentation with treatment refractory obsessive-compulsive disorder. Mol. Psychiatry. 2006;11:622–632. doi: 10.1038/sj.mp.4001823. [DOI] [PubMed] [Google Scholar]
- 63.McDougle C.J., et al. Haloperidol addition in fluvoxamine-refractory obsessive-compulsive disorder. A double-blind, placebo-controlled study in patients with and without tics. Arch. Gen. Psychiatry. 1994;51:302–308. doi: 10.1001/archpsyc.1994.03950040046006. [DOI] [PubMed] [Google Scholar]
- 64.Matsunaga H., et al. Obsessive-compulsive disorder with poor insight. Compr. Psychiatry. 2002;43:150–157. doi: 10.1053/comp.2002.30798. [DOI] [PubMed] [Google Scholar]
- 65.Lombroso P.J., et al. Risperidone treatment of children and adolescents with chronic tic disorders: a preliminary report. J. Am. Acad. Child Adolesc. Psychiatry. 1995;34:1147–1152. doi: 10.1097/00004583-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 66.Coric V., et al. Riluzole augmentation in treatment-resistant obsessive-compulsive disorder: an open-label trial. Biol. Psychiatry. 2005;58:424–428. doi: 10.1016/j.biopsych.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 67.Grant P., Lougee L., Hirschtritt M., Swedo S.E. An open-label trial of riluzole, a glutamate antagonist, in children with treatment-resistant obsessive-compulsive disorder. J. Child Adolesc. Psychopharmacol. 2007;17:761–767. doi: 10.1089/cap.2007.0021. [DOI] [PubMed] [Google Scholar]
- 68. Von Economo, C. 1931.Encephalitis lethargica: its sequelae and treatment. Oxford University Press. London, United Kingdom. 200 pp. [Google Scholar]
- 69.Saxena S., Rauch S.L. Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr. Clin. North Am. 2000;23:563–586. doi: 10.1016/S0193-953X(05)70181-7. [DOI] [PubMed] [Google Scholar]
- 70.Saxena S., Brody A.L., Schwartz J.M., Baxter L.R. Neuroimaging and frontal-subcortical circuitry in obsessive-compulsive disorder. Br. J. Psychiatry Suppl. 1998;35:26–37. [PubMed] [Google Scholar]
- 71.Schwartz J.M., Stoessel P.W., Baxter L.R., Jr., Martin K.M., Phelps M.E. Systematic changes in cerebral glucose metabolic rate after successful behavior modification treatment of obsessive-compulsive disorder. Arch. Gen. Psychiatry. 1996;53:109–113. doi: 10.1001/archpsyc.1996.01830020023004. [DOI] [PubMed] [Google Scholar]
- 72.Baxter L.R., Jr., et al. Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Arch. Gen. Psychiatry. 1992;49:681–689. doi: 10.1001/archpsyc.1992.01820090009002. [DOI] [PubMed] [Google Scholar]
- 73.Smith Y., Hazrati L.N., Parent A. Efferent projections of the subthalamic nucleus in the squirrel monkey as studied by the PHA-L anterograde tracing method. J. Comp. Neurol. 1990;294:306–323. doi: 10.1002/cne.902940213. [DOI] [PubMed] [Google Scholar]
- 74.Baxter L.R., Jr., et al. Brain mediation of obsessive-compulsive disorder symptoms: evidence from functional brain imaging studies in the human and nonhuman primate. Semin. Clin. Neuropsychiatry. 1996;1:32–47. doi: 10.1053/SCNP00100032. [DOI] [PubMed] [Google Scholar]
- 75.Rosenberg D.R., Keshavan M.S. A.E. Bennett Research Award. Toward a neurodevelopmental model of obsessive-compulsive disorder. Biol. Psychiatry. 1998;43:623–640. doi: 10.1016/S0006-3223(97)00443-5. [DOI] [PubMed] [Google Scholar]
- 76.Chamberlain S.R., et al. Orbitofrontal dysfunction in patients with obsessive-compulsive disorder and their unaffected relatives. Science. 2008;321:421–422. doi: 10.1126/science.1154433. [DOI] [PubMed] [Google Scholar]
- 77.Menzies L., et al. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci. Biobehav. Rev. 2008;32:525–549. doi: 10.1016/j.neubiorev.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Alexander G.E., DeLong M.R., Strick P.L. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu. Rev. Neurosci. 1986;9:357–381. doi: 10.1146/annurev.ne.09.030186.002041. [DOI] [PubMed] [Google Scholar]
- 79.Cummings J.L., Cunningham K. Obsessive-compulsive disorder in Huntington’s disease. Biol. Psychiatry. 1992;31:263–270. doi: 10.1016/0006-3223(92)90049-6. [DOI] [PubMed] [Google Scholar]
- 80.Rasmussen S.A., Eisen J.L. Treatment strategies for chronic and refractory obsessive-compulsive disorder. J. Clin. Psychiatry. 1997;58(Suppl. 13):9–13. [PubMed] [Google Scholar]
- 81.Christensen D.D., Laitinen L.V., Schmidt L.J., Hariz M.I. Anterior capsulotomy for treatment of refractory obsessive-compulsive disorder: results in a young and an old patient. Stereotact. Funct. Neurosurg. 2002;79:234–244. doi: 10.1159/000070837. [DOI] [PubMed] [Google Scholar]
- 82.Greenberg B.D., Murphy D.L., Rasmussen S.A. Neuroanatomically based approaches to obsessive-compulsive disorder. Neurosurgery and transcranial magnetic stimulation. Psychiatr. Clin. North Am. 2000;23:671–686, xii. doi: 10.1016/S0193-953X(05)70188-X. [DOI] [PubMed] [Google Scholar]
- 83.Szeszko P.R., et al. Gray matter structural alterations in psychotropic drug-naive pediatric obsessive-compulsive disorder: an optimized voxel-based morphometry study. Am. J. Psychiatry. 2008;165:1299–1307. doi: 10.1176/appi.ajp.2008.08010033. [DOI] [PubMed] [Google Scholar]
- 84.Szeszko P.R., et al. Brain structural abnormalities in psychotropic drug-naive pediatric patients with obsessive-compulsive disorder. Am. J. Psychiatry. 2004;161:1049–1056. doi: 10.1176/appi.ajp.161.6.1049. [DOI] [PubMed] [Google Scholar]
- 85.Perani D., et al. [18F]FDG PET study in obsessive-compulsive disorder. A clinical/metabolic correlation study after treatment. Br. J. Psychiatry. 1995;166:244–250. doi: 10.1192/bjp.166.2.244. [DOI] [PubMed] [Google Scholar]
- 86.Maltby N., Tolin D.F., Worhunsky P., O’Keefe T.M., Kiehl K.A. Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive-compulsive disorder: an event-related fMRI study. Neuroimage. 2005;24:495–503. doi: 10.1016/j.neuroimage.2004.08.041. [DOI] [PubMed] [Google Scholar]
- 87.Ananth J., Pecknold J.C., van den Steen N., Engelsmann F. Double-blind comparative study of clomipramine and amitriptyline in obsessive neurosis. Prog. Neuropsychopharmacol. 1981;5:257–262. doi: 10.1016/0364-7722(81)90077-1. [DOI] [PubMed] [Google Scholar]
- 88.Insel T.R., Mueller E.A., Alterman I., Linnoila M., Murphy D.L. Obsessive-compulsive disorder and serotonin: is there a connection? Biol. Psychiatry. 1985;20:1174–1188. doi: 10.1016/0006-3223(85)90176-3. [DOI] [PubMed] [Google Scholar]
- 89.DeVeaugh-Geiss J., Katz R., Landau P., Goodman W., Rasmussen S. Clinical predictors of treatment response in obsessive compulsive disorder: exploratory analyses from multicenter trials of clomipramine. Psychopharmacol. Bull. 1990;26:54–59. [PubMed] [Google Scholar]
- 90.Goddard A.W., Shekhar A., Whiteman A.F., McDougle C.J. Serotoninergic mechanisms in the treatment of obsessive-compulsive disorder. Drug Discov. Today. 2008;13:325–332. doi: 10.1016/j.drudis.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 91.Bastani B., Nash J.F., Meltzer H.Y. Prolactin and cortisol responses to MK-212, a serotonin agonist, in obsessive-compulsive disorder. Arch. Gen. Psychiatry. 1990;47:833–839. doi: 10.1001/archpsyc.1990.01810210041006. [DOI] [PubMed] [Google Scholar]
- 92.Zohar J., Mueller E.A., Insel T.R., Zohar-Kadouch R.C., Murphy D.L. Serotonergic responsivity in obsessive-compulsive disorder. Comparison of patients and healthy controls. Arch. Gen. Psychiatry. 1987;44:946–951. doi: 10.1001/archpsyc.1987.01800230026006. [DOI] [PubMed] [Google Scholar]
- 93.Zohar J., Insel T.R., Zohar-Kadouch R.C., Hill J.L., Murphy D.L. Serotonergic responsivity in obsessive-compulsive disorder. Effects of chronic clomipramine treatment. Arch. Gen. Psychiatry. 1988;45:167–172. doi: 10.1001/archpsyc.1988.01800260081011. [DOI] [PubMed] [Google Scholar]
- 94.Pigott T.A., et al. Metergoline blocks the behavioral and neuroendocrine effects of orally administered m-chlorophenylpiperazine in patients with obsessive-compulsive disorder. Biol. Psychiatry. 1991;29:418–426. doi: 10.1016/0006-3223(91)90264-M. [DOI] [PubMed] [Google Scholar]
- 95.Frye P.E., Arnold L.E. Persistent amphetamine-induced compulsive rituals: response to pyridoxine(B6). Biol. Psychiatry. 1981;16:583–587. [PubMed] [Google Scholar]
- 96.Goodman W.K., et al. Beyond the serotonin hypothesis: a role for dopamine in some forms of obsessive compulsive disorder? J. Clin. Psychiatry. 1990;51(Suppl.):36–43; discussion 55–38. [PubMed] [Google Scholar]
- 97.Stein D.J., Bouwer C., Hawkridge S., Emsley R.A. Risperidone augmentation of serotonin reuptake inhibitors in obsessive-compulsive and related disorders. J. Clin. Psychiatry. 1997;58:119–122. doi: 10.4088/jcp.v58n0306. [DOI] [PubMed] [Google Scholar]
- 98.Storch E.A., Lehmkuhl H., Geffken G.R., Touchton A., Murphy T.K. Aripiprazole augmentation of incomplete treatment response in an adolescent male with obsessive-compulsive disorder. Depress. Anxiety. 2008;25:172–174. doi: 10.1002/da.20303. [DOI] [PubMed] [Google Scholar]
- 99.van der Wee N.J., et al. Enhanced dopamine transporter density in psychotropic-naive patients with obsessive-compulsive disorder shown by [123I]{beta}-CIT SPECT. Am. J. Psychiatry. 2004;161:2201–2206. doi: 10.1176/appi.ajp.161.12.2201. [DOI] [PubMed] [Google Scholar]
- 100. Swedo, S., and Rapoport, J.L. 1990. Neurochemical and neuroendocrine consideration of obsessive-compulsive disorder in childhood. InApplication of basic neuroscience to child psychiatry. Plenum Medical Books. New York, New York, USA. 275–284. [Google Scholar]
- 101.Chakrabarty K., Bhattacharyya S., Christopher R., Khanna S. Glutamatergic dysfunction in OCD. Neuropsychopharmacology. 2005;30:1735–1740. doi: 10.1038/sj.npp.1300733. [DOI] [PubMed] [Google Scholar]
- 102.Zald D.H., Kim S.W. Anatomy and function of the orbital frontal cortex, I: anatomy, neurocircuitry; and obsessive-compulsive disorder. J. Neuropsychiatry. Clin. Neurosci. 1996;8:125–138. doi: 10.1176/jnp.8.2.125. [DOI] [PubMed] [Google Scholar]
- 103.Garvey M.A., Giedd J., Swedo S.E. PANDAS: the search for environmental triggers of pediatric neuropsychiatric disorders. Lessons from rheumatic fever. J. Child Neurol. 1998;13:413–423. doi: 10.1177/088307389801300901. [DOI] [PubMed] [Google Scholar]
- 104.Budman C.L., Kerjakovic M., Bruun R.D. Viral infection and tic exacerbation. J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:162. doi: 10.1097/00004583-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 105.Ercan T.E., Ercan G., Severge B., Arpaozu M., Karasu G. Mycoplasma pneumoniae infection and obsessive-compulsive disease: a case report. J. Child Neurol. 2008;23:338–340. doi: 10.1177/0883073807308714. [DOI] [PubMed] [Google Scholar]
- 106.Riedel M., Straube A., Schwarz M.J., Wilske B., Muller N. Lyme disease presenting as Tourette’s syndrome. Lancet. 1998;351:418–419. doi: 10.1016/S0140-6736(05)78357-4. [DOI] [PubMed] [Google Scholar]
- 107.Swedo S.E., et al. Sydenham’s chorea: physical and psychological symptoms of St Vitus dance. Pediatrics. 1993;91:706–713. [PubMed] [Google Scholar]
- 108.Swedo S.E., et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am. J. Psychiatry. 1998;155:264–271. doi: 10.1176/ajp.155.2.264. [DOI] [PubMed] [Google Scholar]
- 109.Kiessling L.S., Marcotte A.C., Culpepper L. Antineuronal antibodies: tics and obsessive-compulsive symptoms. J. Dev. Behav. Pediatr. 1994;15:421–425. [PubMed] [Google Scholar]
- 110.Kirvan C.A., Swedo S.E., Snider L.A., Cunningham M.W. Antibody-mediated neuronal cell signaling in behavior and movement disorders. J. Neuroimmunol. 2006;179:173–179. doi: 10.1016/j.jneuroim.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 111.Hamilton C.S., Garvey M.A., Swedo S.E. Therapeutic implications of immunology for tics and obsessive-compulsive disorder. Adv. Neurol. 2001;85:311–318. [PubMed] [Google Scholar]
- 112.Hallett J.J., Harling-Berg C.J., Knopf P.M., Stopa E.G., Kiessling L.S. Anti-striatal antibodies in Tourette syndrome cause neuronal dysfunction. J. Neuroimmunol. 2000;111:195–202. doi: 10.1016/S0165-5728(00)00320-9. [DOI] [PubMed] [Google Scholar]
- 113.Taylor J.R., et al. An animal model of Tourette’s syndrome. Am. J. Psychiatry. 2002;159:657–660. doi: 10.1176/appi.ajp.159.4.657. [DOI] [PubMed] [Google Scholar]
- 114.Singer H.S., et al. Antibodies against human putamen in children with Tourette syndrome. Neurology. 1998;50:1618–1624. doi: 10.1212/wnl.50.6.1618. [DOI] [PubMed] [Google Scholar]
- 115.Morshed S.A., et al. Antibodies against neural, nuclear, cytoskeletal, and streptococcal epitopes in children and adults with Tourette’s syndrome, Sydenham’s chorea, and autoimmune disorders. Biol. Psychiatry. 2001;50:566–577. doi: 10.1016/S0006-3223(01)01096-4. [DOI] [PubMed] [Google Scholar]
- 116.Liu X., Wang Y., Li D., Ju X. Transplantation of rat neural stem cells reduces stereotypic behaviors in rats after intrastriatal microinfusion of Tourette syndrome sera. Behav. Brain Res. 2008;186:84–90. doi: 10.1016/j.bbr.2007.07.040. [DOI] [PubMed] [Google Scholar]
- 117.Kirvan C.A., Swedo S.E., Heuser J.S., Cunningham M.W. Mimicry and autoantibody-mediated neuronal cell signaling in Sydenham chorea. Nat. Med. 2003;9:914–920. doi: 10.1038/nm892. [DOI] [PubMed] [Google Scholar]
- 118.Garvey M.A., et al. A pilot study of penicillin prophylaxis for neuropsychiatric exacerbations triggered by streptococcal infections. Biol. Psychiatry. 1999;45:1564–1571. doi: 10.1016/S0006-3223(99)00020-7. [DOI] [PubMed] [Google Scholar]
- 119.Snider L.A., Lougee L., Slattery M., Grant P., Swedo S.E. Antibiotic prophylaxis with azithromycin or penicillin for childhood-onset neuropsychiatric disorders. Biol. Psychiatry. 2005;57:788–792. doi: 10.1016/j.biopsych.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 120.Perlmutter S.J., et al. Therapeutic plasma exchange and intravenous immunoglobulin for obsessive-compulsive disorder and tic disorders in childhood. Lancet. 1999;354:1153–1158. doi: 10.1016/S0140-6736(98)12297-3. [DOI] [PubMed] [Google Scholar]
- 121.Giedd J.N., Rapoport J.L., Leonard H.L., Richter D., Swedo S.E. Case study: acute basal ganglia enlargement and obsessive-compulsive symptoms in an adolescent boy. J. Am. Acad. Child Adolesc. Psychiatry. 1996;35:913–915. doi: 10.1097/00004583-199607000-00017. [DOI] [PubMed] [Google Scholar]
- 122.Giedd J.N., Rapoport J.L., Garvey M.A., Perlmutter S., Swedo S.E. MRI assessment of children with obsessive-compulsive disorder or tics associated with streptococcal infection. Am. J. Psychiatry. 2000;157:281–283. doi: 10.1176/appi.ajp.157.2.281. [DOI] [PubMed] [Google Scholar]
- 123.Elia J., et al. PANDAS with catatonia: a case report. Therapeutic response to lorazepam and plasmapheresis. J. Am. Acad. Child Adolesc. Psychiatry. 2005;44:1145–1150. doi: 10.1097/01.chi.0000179056.54419.5e. [DOI] [PubMed] [Google Scholar]
- 124. Martin, A. 2003.Pediatric psychopharmacology: principles and practice. Oxford University Press. Oxford, United Kingdom/New York, New York, USA. 175–181. [Google Scholar]