Abstract
Using protection motivation theory, we examined racial differences in intent to complete a living will, rational problem solving (e.g., information seeking), and maladaptive coping responses (i.e., wishful thinking) to a health crisis. Sixty healthy, older adults without living wills responded to written vignettes, including information about living wills as an effective coping mechanism to avoid a health crisis. Use of adaptive coping responses predicted intent to execute a living will. A significant race-by-threat interaction predicted use of rational problem solving, with Caucasians more likely to seek information in response to perceived threat in comparison with African Americans. A significant race-by-adaptive-coping interaction predicted maladaptive coping, indicating that Caucasians were more variable in their maladaptive responses. The effectiveness of health care messages regarding living wills for older adults may be enhanced by focusing on racial differences in response to perceived health threat and perceived adaptive coping information.
Keywords: living wills, race/ethnicity and health, protection motivation theory, preventive health
INTRODUCTION
Since the passage of the Patient Self Determination Act (PSDA) in 1990 (Omnibus Budget Reconciliation Act, 1990), public policy in the United States has advocated the execution of advance directives such as living wills or durable powers of attorney for health care. The rapid adoption of advance directives as a solution to the need for advance care planning prior to potential life-threatening illness and incapacity is based on the ethical ascendancy of autonomy, or self-determination, as a personal value guiding medical care (Allen-Burge & Haley, 1997). Factors that influence execution of advance directives include age, education, health status, and culture; typically, older Caucasians with high educational attainment and poor health are most likely to execute an advance directive (Phipps et al., 2003; Rosnick & Reynolds, 2003).
However, recent critical reviews of the scientific basis of this approach to advance care planning indicate problems in the effective enactment of advance directives as guides for medical care near the end of life (Ditto & Hawkins, 2005; Kwak & Haley, 2005). Few studies have employed theory to examine the factors associated with an individual's intention to complete a living will (Kwak & Haley, 2005). Understanding psychosocial factors underlying individual completion of living wills is the first step in developing new and effective approaches to the use of advance directives as an advance care planning intervention near the end of life (Ditto & Hawkins, 2005).
Advance Care Planning and Race1
Kwak and Haley (2005) reviewed 33 empirical studies in which race or ethnicity were topics of investigation. They identified four domains of study: advance care planning (typically involving advance directives such as living wills); life support; disclosure and communication of diagnosis, prognosis, and preferences to physicians and family members; and designation of proxy decision makers. In general, non-Caucasian groups reported less knowledge of advance directives. Caucasians are more likely in comparison with African Americans to possess a living will (Hopp & Duffy, 2000; Phipps et al., 2003). By contrast, African Americans are more likely than Caucasians to opt for life-sustaining medical interventions (Phipps et al., 2003).
Based on this review, educating African Americans about the usefulness of living wills may be one avenue for future research. In fact, existence of a living will partially mediated the relationship between race and use of hospice services in the last year of life according to retrospective reports of bereaved family members (Greiner, Perera, & Ahluwalia, 2003). This suggests that greater theoretical understanding of individual, and perhaps cultural, processes surrounding the perception of living wills may inform future interventions to increase effective advance directive execution, including intention to complete living wills, across racial groups.
To advance this research area, a theory is needed that explains illness perceptions, or health threat, and how these perceptions result in diverse adaptive or maladaptive coping styles. Protection motivation theory (PMT) (Prentice-Dunn & Rogers, 1986; Rogers & Prentice-Dunn, 1997) explains the cognitive processes that are used when people receive health information. Information regarding living wills appears to be lacking among African American individuals (Kwak & Haley, 2005), and perhaps presenting African Americans with information regarding the potential of living wills to facilitate desired medical treatment during a time of medical crisis would increase intention to complete living wills. In contrast, Caucasians may not benefit as readily from additional information because they already perceive living wills as a preventive health behavior with the ability to reduce the likelihood of suffering and lessen the emotional toll on one's family near the end of life (Tilden, Tolle, Nelson, & Fields, 2001).
Protection Motivation Theory (PMT)
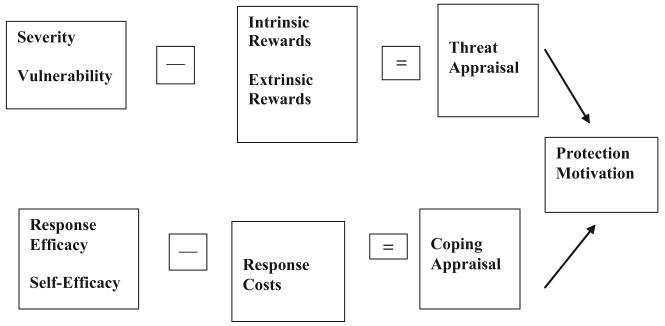
Information such as a pamphlet about living wills initiates two types of appraisals that determine the extent to which the individual will respond adaptively or maladaptively to potentially threatening health information (see Figure 1). Threat appraisal consists of the perceived severity of the health threat and the individual's vulnerability to experiencing the health threat. According to PMT, perceived threat should decrease individuals' likelihood of a maladaptive response such as avoidance of thinking about living wills. In contrast, any perceived rewards of not completing a living will reduce the perceived threat.
FIGURE 1.
The cognitive mediating processes of protection motivation theory (adapted from Rogers & Prentice-Dunn, 1997).
The coping appraisal process evaluates one's ability to actively deal with the threatened danger. The belief that the recommended adaptive response (e.g., completing a living will) is effective (e.g., response efficacy) and that one can successfully complete a living will (e.g., self-efficacy) increase intention to complete a living will. This intention decreases with any perceived social, physical, or monetary costs of performing the recommended response.
A meta-analysis of 65 studies involving nearly 30,000 participants with various racial and ethnic backgrounds found PMT effective in explaining a variety of preventive health behaviors (Floyd, Prentice-Dunn, & Rogers, 2000). Among the health domains included were lung cancer, osteoporosis, AIDS, muscular dystrophy, alcohol abuse, breast self-examination, and exercise. An independent meta-analysis (Milne, Sheeran, & Orbell, 2000) corroborated these conclusions. Subsequent studies (e.g., Fry & Prentice-Dunn, 2005; Prentice-Dunn, Floyd, & Flournoy, 2001) indicated that threat information motivates individuals to act in a variety of ways and that coping information plays a vital role in channeling individuals' reactions in adaptive directions.
Need For and Aims Of This Study
Passage of the PSDA in the United States changed public policy to promote the use of advance directives such as living wills prior to the acquisition of knowledge regarding what motivates individuals to use living wills as a preventive health behavior. Recent reviews question whether this policy has had the desired effect of improving public health (Ditto & Hawkins, 2005). PMT predicts that individuals who perceive living wills as an effective means of avoiding perceived health threats will increase their intention to execute a living will. However, the severity of one potential health threat activated by considering living wills (i.e., death) makes unknown to what extent PMT may inform individuals' intention to execute a living will.
We explored racial similarities and differences in the usefulness of PMT-based information among older community-dwelling adults in increasing individual intention to completing a living will. We selected a community sample rather than a primary care sample due to the demonstrated effectiveness of PMT in promoting preventive health behaviors among community-dwelling adults. Moreover, individuals recruited from primary care settings would have pre-existing health threats that would be: (a) difficult to measure and “equate,” and (b) could influence study responses and threaten internal validity. We hypothesized that level of perceived threat and level of adaptive coping would predict individuals' intention to complete a living will, use of rational problem-solving (e.g., information seeking), and use of maladaptive coping in response to the health crisis described in the vignettes. We explored the main effect of race as well as the race by threat and race by adaptive coping interactions in relation to intention to complete a living will, rational problem solving, and maladaptive coping. We also explored associations between PMT variables, prior experience with end-of-life decision-making, crystal and fluid intelligence, subjective well-being, and religious problem-solving.
METHODS
Participants
Participants were recruited from local health fairs, informational talks held with community organizations, newspaper ads, congregate housing, and personal referrals. After individuals expressed interest in the study and provided their name and telephone number, we screened older adults for inclusion during an initial phone contact based on the following criteria: (a) age 55 or older, (b) not currently possessing a living will, (c) community residence, and (d) fair or better health. Sixty individuals (29 Caucasian, 31 African American) received a small honorarium (a $10 Wal-Mart gift certificate) for completing the study. There were no significant differences between Caucasians and African Americans in age, years of education, or subjective well-being (see Table 1). There also were no statistically significant racial differences in experience with decision making regarding end-of-life issues for a family member or close friend, [χ2(1, N = 59) = .95, p = .42], although 31% of Caucasians in comparison with 43% of African Americans reported having had such experiences.
TABLE 1.
Participant characteristics by racial group (standard deviations in parentheses)
| Variable | Caucasian (n = 29) |
African American (n = 31) |
t Value | p Value | ||
|---|---|---|---|---|---|---|
| Age (years) | 72.03 | (6.49) | 68.42 | (8.30) | 1.87 | .066 |
| Education (years) | 13.55 | (3.85) | 13.168 | (4.56) | 0.36 | .722 |
| Health status | 3.10 | (0.77) | 2.71 | (0.74) | 2.02 | .048* |
| Subjective Well Being | 7.81 | (1.23) | 8.09 | (1.08) | 1.13 | .261 |
| VIQ scale scorea | 9.34 | (3.25) | 7.23 | (3.16) | 2.56 | .013* |
| PIQ scale scorea | 11.70 | (3.13) | 8.29 | (2.87) | 4.39 | .0001** |
Note:
Verbal (VIQ) and nonverbal (PIQ) intelligence were estimated by the Wechsler Abbreviated Scale of Intelligence (WASI) Vocabulary and Matrix Reasoning subtests. Mean scale scores are 10 with a 95% confidence interval between the scores of 8 and 12.
p < .05.
p < .01.
There were, however, racial differences in self-reported health status and in verbal and nonverbal intelligence (see Table 1). Caucasians reported themselves to be in significantly better health than African Americans. Caucasians also had higher scaled scores on measures of verbal and nonverbal intelligence than did African Americans. Historically, however, Caucasian and African American individuals in the Southeastern United States did not receive the same quality of education, health care, or other cultural opportunities related to psychometric verbal and nonverbal intelligence scores. Thus, this finding is likely related to the substantial inequalities and racism faced by older African American adults in this sample during their formative years.
Vignettes (Available from Authors on Request)
Coping appraisal (low vs. high) was manipulated through vignettes that depicted a health crisis (persistent vegetative state, or PVS) resulting from a motor vehicle accident. A severe motor vehicle accident was chosen as the precipitating health event to induce perceived threat in all participants. Notably, landmark legal decisions advocating the use of advance directives such as living wills were prompted by families of severely injured individuals seeking relief from persistent vegetative states (Cruzan v. Director of the Missouri Department of Health, 1990).
Two versions of the paper-and-pencil vignette were used: (a) a low-coping version containing information about living wills that was not directly related to avoidance of a PVS, and (b) a high-coping version presenting more information about living wills as a means of coping with the potential of a PVS resulting from the motor vehicle accident. Persistent vegetative states were defined as conditions in which “a person can not talk, work with their hands, or feed themselves.” Both vignettes stated that “there is no treatment for persistent vegetative states; doctors can only provide nutrition and try to prevent infection” and “patients can remain in vegetative states for years or even decades.” Both vignettes also included a picture of an individual with a nasogastric tube for time-limited artificial nutrition. Vignettes were stratified by racial group and then distributed randomly to the participants.
Measures
A demographic questionnaire measured age, race, gender, years of education, health status, and prior experience with end-of-life issues personally or among friends and family.
The living will survey contained 41 randomly arranged statements including items measuring PMT constructs of: (a) threat, (b) adaptive coping, and (c) maladaptive coping with respect to decisions about executing a living will (see Table 2). The survey also contained items summed to produce outcome variables including intention to complete a living will, rational problem-solving, and maladaptive coping. Finally, items were included and summed to assess the perceived “credibility” of the vignettes to participants (see Table 2).
TABLE 2.
Exemplar items used in the subscales of the living will survey
| Threat 7 (items) |
| “It is stressful for others to decide whether or not to initiate life sustaining treatments on a patient.” |
| “As an adult, I am at risk for having my wishes about life sustaining treatments ignored during a medical crisis.” |
|
Adaptive Coping (6 items) Response Efficacy |
| “Having a living will is the best, most effective method for preventing my family from being emotionally burdened by having to decide my wishes about life sustaining treatments.” |
| “If I have a living will, then my chances of having an influence over my end-of-life medical care are extremely high.” |
| Self-Efficacy |
| “Even if I had a living will, I don't know if I would fill it out correctly.” |
| “I am capable of executing a living will that clearly defines my wishes about life-sustaining medical care.” |
|
Maladaptive Coping (16 items) Avoidance |
| “I sometimes wish I could avoid situations that confront me with the facts about living wills and dying.” |
| Wishful Thinking |
| “I like to pretend that I will never have to face death.” |
| “I believe that my family and physician will just know what I will want at the time if I am ever in a vegetative state.” |
| Fatalism |
| “If you are destined to be kept alive on machines, you will be; there is really little you can do about it.” |
| Hopelessness |
| “Life is so unpredictable that it sometimes seems a hopeless task to prepare for end of life issues.” |
| Intention - 4 items |
| “At present I am not planning on completing a living will.” |
| “Not only do I plan on completing a living will, I will give copies of the living will to my family and friends.” |
| Rational Problem Solving / Information Seeking - 4 items |
| “I will feel better about the possibility of facing a medical crisis if I obtain a living will.” |
| “The essay made me want a living will because living wills solve many problems that occur in a medical crisis.” |
| Credibility - 4 items |
| “I did not really believe what I read in the essay.” |
| “The information on living wills was presented in a clear and simple way.” |
Both adaptive and maladaptive coping reactions are useful to the person receiving health information, but they differ in how directly they address the threat felt by the individual. Thus, “maladaptive” coping mechanisms may help reduce individuals' distress initially, but may fail to effectively address the health threat and lead to poor long-term outcomes. In addition, “rational problem solving” (McRae, 1984) refers to seeking more information about a health problem and has been shown to be a precursor to direct action.
Participants were asked whether they never, seldom, occasionally, frequently, or always agreed with each statement. Threat (α = .71) consisted of a sum of items assessing severity (n = 4 items) and vulnerability (n = 3 items). Adaptive Coping (α = .63) was a sum of items tapping perceived response efficacy (n = 2 items) and perceived self-efficacy (n = 4 items). Maladaptive Coping (α = .85) consisted of items measuring avoidance (n = 4 items), wishful thinking (n = 4 items), fatalism (n = 3 items) and hopelessness (n = 5 items). Both outcome scales including intention to complete a living will (α = .82) and rational problem-solving (α = .85) consisted of four items each. The credibility scale (α = .75) also consisted of four items.
Subjective well-being (Tran, Wright, & Chatters, 1991)
Psychological well-being was assessed via the sum of three questions regarding the participant's perception of life-satisfaction, overall happiness, and goal attainment. Scores on this scale range from 3 to 9 (M = 7.44, SD = 1.40), with higher values indicating greater subjective well-being. We found moderate internal consistency for this scale (α = .56), with inter-item correlations ranging between .2 and .4.
Wechsler Abbreviated Scale of Intelligence (WASI; Psychological Corporation, 1999)
The WASI is a reliable, individually administered measure of intelligence designed for use with individuals aged from 6 to 89 years. We used Vocabulary, a measure of semantic, crystallized verbal knowledge and Matrix Reasoning, a measure of nonverbal fluid abilities. The reliability coefficient for Vocabulary among individuals 17 to 89 years of age is .94, with a range of .90 to .98. Matrix Reasoning has a reliability correlation coefficient of .94 for the same age group with a range of .88 to .96. Test-retest reliability is .90 for Vocabulary and .81 for Matrix Reasoning.
Religious Problem Solving Scales (Short Version; Pargament et al., 1988)
This 18-item scale assessed participant's use of three religious coping strategies to solve problems. The test-retest reliability for the three scales ranges from .87 to .93 (Pargament et al., 1988). Response categories are never, seldom, occasionally, frequently, or always agree. The collaborative scale (α = .93) indicates joint problem-solving between the individual and God (e.g., “When it comes to deciding how to solve a problem, God and I work together as partners”). The self-directing scale (α = .94) taps into a belief that the responsibility to resolve problems rests on the individual (e.g., “When I have a difficulty, I decide what it means by myself without help from God”). The deferring scale (α = .89) contains statements such as “Rather than trying to come up with the right solution to a problem myself, I let God decide how to deal with it.”
Procedure
After meeting inclusion criteria via a telephone screening, participants completed a formal informed consent and 1-hour assessment in a convenient location, either their homes or at community centers. Care was taken to ensure privacy and confidentiality during these assessments. The study was explained to participants and any questions regarding participation were answered. Except for the WASI, questionnaires were self-administered. Participants first completed the demographic questionnaire. Next, a trained research assistant supervised by a licensed clinical geropsychologist administered the WASI to the older adult. If research assistants were uncertain about discontinuation criteria on the subscales of this measure, they continued to administer items until they were certain that discontinuation criteria were met. Scoring of the WASI was corrected after the interview if necessary.
The participants then read the vignettes and underlined phrases and passages they considered particularly relevant and compelling. This facilitated participants' attention to and comprehension of the material presented in the written vignettes. Next, individuals read and completed the living will survey, followed by the religious problem solving scales. The participants were thanked and debriefed at the end of the experiment and received a $10 Wal-Mart gift certificate for participation.
RESULTS
All analyses were run after first centering the summed variables. Bivariate associations among study variables revealed that involvement with end-of-life care, subjective well-being, verbal and nonverbal ability, and religious problem-solving generally were unrelated to PMT variables such as threat, adaptive coping, intention to complete a living will, rational problem-solving, or maladaptive coping; thus, covariates were not utilized in the analyses.
We examined differences in participants' responses to the amount of coping information (high/low) contained in the vignettes regarding the effectiveness of living wills to prevent the outcome of living in a persistent vegetative state. There were no significant differences in participants' responses and responses for the two vignettes were combined in all further analyses.
Our analytic models consisted of the three main effects of race, Adaptive Coping (self-efficacy + response efficacy), and Threat (severity + vulnerability), along with all possible two-way interactions and the three-way interaction. There was little multicolinearity among these three predictors. As a check of our manipulation, we examined participants' responses to questions (n = 4) embedded within the living will questionnaire regarding the credibility of the health crisis depicted in the vignette. The overall model was significant, F(7, 47) = 8.85, p < .0001, R2 = .57, adjusted R2 = .50. Caucasians and African Americans responded similarly to the vignettes. Only the main effect of adaptive coping was significant, F(1, 47) = 19.38, p < .0001. Individuals higher in perceived adaptive coping perceived the vignette as more credible.
Our primary outcomes included: (a) intention to complete a living will, (b) rational problem-solving (i.e., information seeking), and (c) maladaptive coping. With regard to intention to complete a living will, our overall model was significant, F(7, 47) = 4.86, p = .0001, R2 = .42, adjusted R2 = .33. Only the main effect of adaptive coping was significant, F(1,47) = 15.01, p = .0001. Individuals higher in adaptive coping showed higher intentions to complete a living will. In other words, those individuals with higher self-efficacy who perceived the execution of a living will to be an effective response to the health crisis depicted in the vignette intended to complete a living will. The main effect of race and any interactions with race were not significant predictors of intention to complete a living will.
Regarding use of rational problem solving strategies (or tendency to respond to health threat by seeking information), our overall model was significant, F(7, 47) = 7.08, p = .0001, R2 = .51, adjusted R2 = .44. There was a significant race by threat interaction, F(1, 47) = 4.30, p = .044 (see Figure 2). African Americans who perceived greater threat in the vignette were less likely to use rational problem solving to seek information in response to the health crisis. Of course, information seeking is only one possible active coping mechanism involving direct action on the part of the individual with the potential for positive long-range health outcomes. In comparison, Caucasians who perceived greater threat used more rational problem-solving and Caucasians who perceived low levels of threat did not use rational problem-solving. There was also a significant main effect of coping, F(1, 47) = 20.81, p = .0001, with individuals higher in perceived adaptive coping making greater use of rational problem-solving skills.
FIGURE 2.
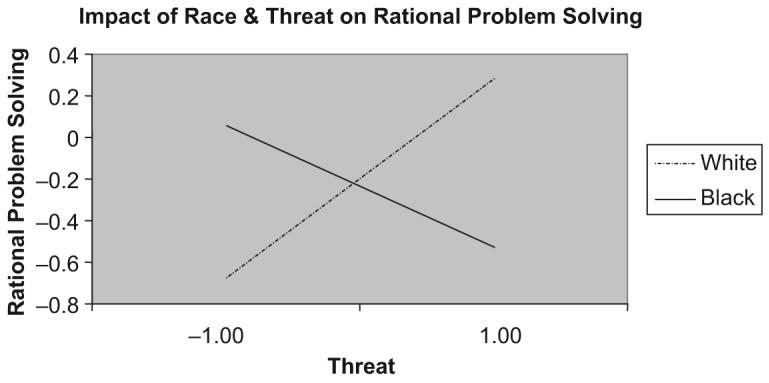
Race by threat interaction predicting use of rational problem solving in response to the threat of living in a persistent vegetative state. Values along the horizontal and vertical axes are presented as z scores.
According to PMT, threat appraisal may precipitate emotional response without direct coping action. In other words, a perceived threat may lead to reactions such as avoidance, wishful thinking, fatalism, or hopelessness. Such responses have been termed “maladaptive” within the preventive health literature because they do not instigate active responses to health threat. Our model for use of maladaptive coping mechanisms was significant, F(7, 48) = 6.47, p < .0001, R2 = .48, adjusted R2 = .41. There was a significant race by adaptive coping interaction, F(1, 49) = 5.98, p = .018 (see Figure 3). African Americans responded to the vignette with similarly moderate levels (i.e., surrounding the mean) of maladaptive responses regardless of their adaptive coping skills. Thus, African Americans were not particularly avoidant, wishful in their thinking about the health threat, fatal-istic, or hopeless. Caucasians were much more variable in their maladaptive responses to the health crisis depicted in the vignette depending on whether they reported high or low adaptive coping. Specifically, Caucasians low in perceived adaptive coping reported more maladaptive responses. There also was a significant main effect of coping, F(1, 49) = 15.04, p < .0001, with higher perceived adaptive coping associated with fewer maladaptive coping responses to the vignette.
FIGURE 3.
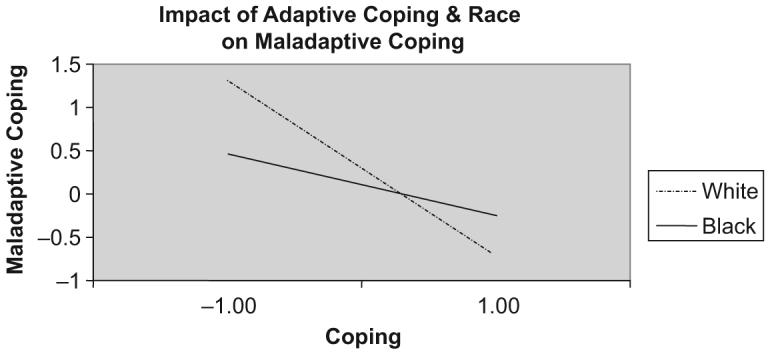
Race by coping interaction predicting older adults' use of maladaptive coping responses to the health threat of living in a persistent vegetative state. Values along the horizontal and vertical axes are presented as z scores.
DISCUSSION
These data suggest that protection motivation theory may facilitate the intention to complete living wills among Caucasian and African American older adults who perceive living wills as a potentially useful preventive health measure (i.e., response efficacy) that can easily be executed (i.e., self-efficacy) to avoid the health threat of life in a persistent vegetative state. Specifically, the perception of adaptive coping information (i.e., self-efficacy and response efficacy) predicted intent to execute a living will; there were no racial/ethnic differences. These results are consistent with recent studies in other health domains in which self-efficacy and response efficacy information lead people to take preventive actions (Fry & Prentice-Dunn, 2005; McMath & Prentice-Dunn, 2005), but are remarkable in light of the many racial differences found in advance care planning research (Kwak & Haley, 2005). Notably, there were no racial/ethnic differences in the perceived credibility of the vignettes. This may indicate that educational interventions targeted at providing threat and coping information regarding the use of living wills as effective preventive health measures might increase intentions to execute living wills among African Americans, a racial group that typically lacks information about such documents (Kwak & Haley, 2005). Discussion of end-of-life treatment preferences with potential proxy decision makers and execution of advance directive documents may alleviate stress for older adults and their family caregivers (Ditto et al., 2001; Tilden et al., 2001).
Our results based on this initial study suggest that, in the PMT model (Figure 1), the coping appraisal process plays a more vital role than the threat appraisal process in intention to execute a living will among older Caucasian and African American adults. We hypothesized that there would be no racial/ethnic differences in the threat appraisal process initiated by the health information regarding living wills contained in the vignettes. Instead, we found a race by threat interaction in the use of rational problem solving (e.g., information seeking), with Caucasians using more rational problem solving in response to greater perceived threat and African Americans using less (see Figure 2). Our measure of “threat” included only perceived severity of living in a persistent vegetative state and perception of vulnerability to experience this health threat after having a motor vehicle accident. Recent qualitative research findings elicited via focus groups with African Americans suggest that mechanical life support, artificial nutrition and hydration, and other measures that may prolong life may not be perceived as inducing suffering in African American culture (Bullock, 2006). Thus, there may be culturally mediated qualitative differences in perceived threat that were not adequately measured in our quantitative living will survey. Future research should build upon the promise of PMT-based interventions to increase intention to execute living wills by incorporating qualitative measures of the threat appraisal and coping appraisal process across racial/ethnic and other cultural groups. Moreover, cultural variation in the usefulness of rational problem-solving, or information seeking, in response to one's potential death needs to be further explored and additional “adaptive” coping responses based on direct confrontation of the danger need to be identified.
We also found a race by adaptive coping interaction with regard to maladaptive coping responses (see Figure 3). Maladaptive coping consisted of avoidance of thinking about the health threat, wishful thinking, fatalism, and hopelessness (see Table 2). Whereas African Americans responded with moderate levels of maladaptive coping, Caucasians reported more maladaptive responses when their perceived adaptive coping skills were low and fewer maladaptive coping responses when their perceived adaptive coping was high. It would appear, based on our data, that African Americans did not react to the health threat presented in these vignettes with inactive and “maladaptive” emotional responses. Previous research with dementia care-givers has shown that African Americans report more positive aspects of caregiving and less perceived burden and depression in response to the caregiving experience (Haley et al., 1996; Roff et al., 2004). Additionally, African Americans report preferences for life-sustaining treatment regardless of the subsequent state of health of the individual in question (Allen-Burge & Haley, 1997; Duffy et al., 2006; Kwak & Haley, 2005). Perhaps African American culture endorses certain values and preferences, such as the sanctity of life, making individual African Americans' process toward end-of-life decision making more uniform compared with that of Caucasians. Future research regarding cultural differences in advance care planning and end-of-life decision making should attend more to individual quality of life determinations and process preferences (Hawkins, Ditto, Danks, & Smucker, 2005) than to the execution of formal advance directives such as living wills.
We acknowledge several limitations of this study. Our vignette manipulation of coping information was not successful; however, subsequent correlational analyses produced an array of results that were interesting and interpretable. Our preliminary investigation of the usefulness of PMT to understand intention to complete living wills targeted community-dwelling Caucasians and African Americans over the age of 55 in one relatively small sample from one southeastern city in the United States. Although our Caucasian and African American participants varied in verbal and nonverbal intelligence scores, verbal and nonverbal intelligence shared little variance with perceived threat, adaptive coping, intention to complete a living will, rational problem-solving, or maladaptive coping responses, thereby reducing our concern about this finding. This study also did not have sufficient power to explore age differences between young-old (e.g., age 55 to 70 years) and old-old (e.g., age 71 years and older) adults. Replication of these findings in a larger and more diverse sample of community-dwelling individuals across a broad age range is needed.
This research is the first to examine protection motivation theory as a potential avenue for understanding individual and cultural differences in the intention to execute living wills. Because religious and spiritual beliefs may provide a cognitive framework that actively reduces stress among African American elders in the face of illness (Crowther, Parker, Larimore, Achenbaum, & Koenig, 2002), it may be that some aspect of religiousness or spirituality not measured in the current study better captures active engagement with health threats among African American elders. Further qualitative research and use of more precise quantitative measures may distinguish factors that would inform PMT studies in which the intention to execute a living will is conceptualized as a preventive health behavior.
Acknowledgments
Funding from the National Institute on Aging (K01AG00943) to Rebecca S. Allen partially supported data collection for this project and preparation of this manuscript. Additionally, funding for data collection was provided by the Department of Psychology at The University of Alabama as part of Dorothy Pekmezi's undergraduate honors thesis.
Footnotes
Portions of this article were presented at the 56th annual scientific meeting of the Gerontological Society of America, San Diego, CA, November 2003.
We recognize in this manuscript that “race” is a physiological term that does not apply well to psychosocial phenomena; however, because our sample is limited in “ethnicity” to Caucasian and African American adults, we use the term “race” throughout the manuscript.
Contributor Information
REBECCA S. ALLEN, University of Alabama and Center for Mental Health and Aging, Tuscaloosa, Alabama, USA.
LAURA L. PHILLIPS, Houston Veterans Affairs Medical Centers, Houston, Texas, USA.
DOROTHY PEKMEZI, The Miriam Hospital and Brown Medical School Centers for Behavioral and Preventive Medicine, Providence, Rhode Island, USA.
MARTHA R. CROWTHER, University of Alabama and Center for Mental Health and Aging, Tuscaloosa, Alabama, USA.
STEVEN PRENTICE-DUNN, University of Alabama, Tuscaloosa, Alabama, USA.
REFERENCES
- Allen-Burge R, Haley WE. Individual differences and surrogate medical decisions: Differing preferences for life-sustaining treatments. Aging and Mental Health. 1997;1(2):121–131. [Google Scholar]
- Bullock K. Promoting advance directives among African Americans: A faith-based model. Journal of Palliative Medicine. 2006;9:183–195. doi: 10.1089/jpm.2006.9.183. [DOI] [PubMed] [Google Scholar]
- Crowther M, Parker M, Larimore W, Achenbaum A, Koenig H. Rowe and Kahn's model of successful aging revisited: Spirituality the missing construct. The Gerontologist. 2002;42(5):613–620. doi: 10.1093/geront/42.5.613. [DOI] [PubMed] [Google Scholar]
- Cruzan v. Director of the Missouri Department of Health. 1990;497 [Google Scholar]
- Ditto PH, Danks JH, Smucker WD, Bookwala J, Coppola KM, Dresser R, Fagerlin A, Gready RM, Houts R, Lockhart LK, Zyzanski S. Advance directives as acts of communication: A randomized controlled trial. Archives of Internal Medicine. 2001;161:421–430. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- Ditto PH, Hawkins NA. Advance directives and cancer decision making near the end of life. Health Psychology. 2005;24:S63–S70. doi: 10.1037/0278-6133.24.4.S63. [DOI] [PubMed] [Google Scholar]
- Duffy SA, Jackson FC, Schim SM, Ronis DL, Fowler KE. Racial/ethnic preferences, sex preferences, and perceived discrimination related to end-of-life care. Journal of the American Geriatrics Society. 2006;54:150–157. doi: 10.1111/j.1532-5415.2005.00526.x. [DOI] [PubMed] [Google Scholar]
- Floyd DL, Prentice-Dunn S, Rogers RW. A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology. 2000;30:407–429. [Google Scholar]
- Fry RB, Prentice-Dunn S. The effects of coping information and value affirmation on responses to a perceived health threat. Health Communication. 2005;17:133–147. doi: 10.1207/s15327027hc1702_2. [DOI] [PubMed] [Google Scholar]
- Greiner KA, Perera S, Ahluwalia JS. Hospice usage by minorities in the last year of life: Results from the national mortality followback survey. Journal of the American Geriatrics Society. 2003;51:970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- Haley WE, Roth DL, Coleton MI, Ford GR, West CAC, Collins RP, Isobe TL. Appraisal, coping, and social support as mediators of well-being in Black and Caucasian family caregivers of patients with Alzheimer's disease. Journal of Consulting & Clinical Psychology. 1996;64:121–129. doi: 10.1037//0022-006x.64.1.121. [DOI] [PubMed] [Google Scholar]
- Hawkins NA, Ditto PH, Danks JH, Smucker WD. Micromanaging death: Process preferences, values and goals in end-of-life medical decision making. The Gerontologist. 2005;45:107–117. doi: 10.1093/geront/45.1.107. [DOI] [PubMed] [Google Scholar]
- Hopp FP, Duffy SA. Racial variations in end-of-life care. Journal of the American Geriatrics Society. 2000;48:658–663. doi: 10.1111/j.1532-5415.2000.tb04724.x. [DOI] [PubMed] [Google Scholar]
- Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. The Gerontologist. 2005;45:634–641. doi: 10.1093/geront/45.5.634. [DOI] [PubMed] [Google Scholar]
- McMath BF, Prentice-Dunn S. Protection motivation theory and skin cancer risk: The role of individual differences in responses to persuasive appeals. Journal of Applied Social Psychology. 2005;35:621–635. [Google Scholar]
- McRae RR. Situational determinates of coping responses: Loss, threat, and challenge. Journal of Personality and Social Psychology. 1984;46:919–928. doi: 10.1037//0022-3514.46.4.919. [DOI] [PubMed] [Google Scholar]
- Milne S, Sheeran P, Orbell S. Prediction and intervention in health related behavior: A meta-analytic review of protection motivation theory. Journal of Applied Social Psychology. 2000;30:106–143. [Google Scholar]
- Omnibus Budget Reconciliation Act of 1990, P. L. 101–508, §4206, and 4715, codified at 42 U.S.C. §§ 1395cc (a) (1) (q), 1395 mm (c) (8), 1395cc (f), 1396a (57), (58), 1396a (w).
- Pargament KI, Kennell J, Hathaway W, Grevengoed N, Newman J, Jones W. Religion and the problem-solving process: three styles of coping. Journal for the Scientific Study of Religion. 1988;27:90–104. [Google Scholar]
- Phipps E, True G, Harris D, Chong U, Tester W, Chavin SI, Braitman LE. Approaching the end of life: Attitudes, preferences, and behaviors of African American and Caucasian patients and their family caregivers. Journal of Clinical Oncology. 2003;21:549–554. doi: 10.1200/JCO.2003.12.080. [DOI] [PubMed] [Google Scholar]
- Prentice-Dunn S, Floyd DL, Flournoy JM. Effects of persuasive message order coping with breast cancer information. Health Education Research. 2001;16:81–84. doi: 10.1093/her/16.1.81. [DOI] [PubMed] [Google Scholar]
- Prentice-Dunn S, Rogers RW. Protection Motivation Theory and preventive health: beyond the health belief model. Health Education Research. 1986;1:153–161. [Google Scholar]
- Psychological Corporation . The Wechsler Abbreviated Scale of Intelligence. Harcourt Brace & Company; San Antonio: 1999. [Google Scholar]
- Rogers RW, Prentice-Dunn S. Protection motivation theory. In: Gochman D, editor. Handbook of Health Behavior Research: Vol. 1 Determinants of Health Behavior: Personal and Social. Plenum; New York: 1997. pp. 113–132. [Google Scholar]
- Roff LL, Burgio LD, Gitlin L, Nichols L, Chaplin W, Hardin JM. Positive aspects of caregiving: The role of race. Journal of Gerontology: Psychological Science. 2004;59(4):185–190. doi: 10.1093/geronb/59.4.p185. [DOI] [PubMed] [Google Scholar]
- Rosnick CB, Reynolds SL. Thinking ahead: Factors associated with executing advance directives. Journal of Aging and Health. 2003;15:409–429. doi: 10.1177/0898264303015002005. [DOI] [PubMed] [Google Scholar]
- Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nursing Research. 2001;50:105–115. doi: 10.1097/00006199-200103000-00006. [DOI] [PubMed] [Google Scholar]
- Tran TV, Wright R, Chatters L. Health, stress, psychological resources, and subjective well-being among older Blacks. Psychology and Aging. 1991;6:100–108. doi: 10.1037//0882-7974.6.1.100. [DOI] [PubMed] [Google Scholar]