Abstract
The resumption of sexual activity after delivery is a key moment in the management of the risk of sexual HIV transmission within the couple for women who had been prenatally tested for HIV. In this study, we have investigated consistent condom use during the resumption of sexual activity and its evolution over time among women tested for HIV infection during pregnancy. We tested for HIV during pregnancy 546 HIV-infected and 393 HIV-negative women within the DITRAME Plus ANRS project in Abidjan; these women were followed-up for two years after delivery. Most HIV-negative women (96.7%) disclosed their HIV-test result to their partners, whereas only 45.6% of HIV-infected women did it (p<0.001). Partners of HIV-infected women were more likely to be tested for HIV before resuming sexual activity than partners of HIV-negative women (11.7% versus 7.4% p=0.054). Less than one third of both HIV-infected and HIV-negative women reported having systematically used condoms during the resumption of sexual activity. The proportions of HIV-infected and HIV-negative women having consistently used condom were respectively 26.2% and 19.8% (p=0.193) at 3 months post-partum, 12.1% and 15.9% (p=0.139) at 12 months post-partum, 8.4% and 10.6%, (p=0.302) at 18 months post-partum. In our study, although women had been prenatally tested for HIV and properly counselled on the sexual risk of HIV transmission, male partners were not tested for HIV before the resumption of sexual activity after delivery, very few couples were using condoms systematically and condom use was decreasing over time.
Keywords: Condoms, statistics & numerical data, Cote d'Ivoire, epidemiology, Female, Follow-Up Studies, HIV Infections, diagnosis, epidemiology, prevention & control, Humans, Male, Postnatal Care, Pregnancy, Prenatal Diagnosis, Truth Disclosure
Introduction
In 2006, 3.8 million adults became newly infected with HIV. Among those, 2.8 million (74%) lived in sub-Saharan Africa, the region with the largest burden of the AIDS epidemic (UNAIDS & WHO, 2006). HIV transmission among adult is mainly heterosexual in Africa where both the prevention of sexual and mother-to-child transmissions of HIV (PMTCT) are public health priorities.
Condom is the most effective to prevent the sexual transmission of HIV and other Sexually Transmitted Infections (STIs) (Ahmed et al., 2001; Davis & Weller, 1999; Holmes et al., 2004; Pinkerton & Abramson, 1997). It is also a contraceptive method if it is correctly used. But African people are still reluctant to use it, especially within the couple: less than 3% of married couples use condom on a regular basis (Ali et al., 2004; Allen et al., 2003). However, most cases of sexual transmission of HIV occur within stable relationships in high HIV prevalence African settings (Tabi et al., 2003). Condom is usually perceived as a means of prevention for risky sexual behaviours: men or women are more easily using condoms with occasional sexual partners than with their spouse or husband (ONU, 2002). Talks about condom use are rare within couples (Muhwana, 2004).
More and more women are offered prenatal HIV counselling and testing with the increasing implementation of PMTCT programmes in African settings. The majority of these women tested for HIV during antenatal care are in stable relationship. The resumption of sexual activity after delivery is therefore a key moment for the management of the risk of sexual HIV transmission within the couple for these women who were diagnosed as HIV-infected during pregnancy. In this study, we have investigated consistent condom use during the resumption of sexual activity and its evolution over time among women tested for HIV infection during pregnancy.
Study population
The PMTCT research programme ANRS 1201/1202/1253 DITRAME Plus was implemented in Abidjan, Côte d’Ivoire, in March 2001. HIV-testing was systematically proposed at the first antenatal consultation to any pregnant women aged at least 18 years attending one of the selected prenatal clinics located in two populated suburbs of Abidjan. After signing an informed consent form, women were regularly followed-up for two years after delivery: every three months during the first year and every six months during the second year.
Consenting HIV-infected women were systematically offered to be included in a cohort offering peripartum and postnatal PMTCT interventions fully described elsewhere (ANRS 1201–1202 DITRAME Plus Study Group, 2005, Becquet et al., 2007). A cohort of HIV-negative women was also constituted. These women were included in a study proposing HIV counselling and free access contraception to care and contraception methods (Brou et al., 2005). Both HIV-infected and uninfected women were informed on STIs including HIV/AIDS. Condom use was encouraged during pre and post-test counselling and post-partum follow-up. After delivery, women were freely provided a various range of contraceptive methods including condom.
During each follow-up visit, standardised questionnaires were administered to all women to document the disclosure of HIV-status to the partner, the resumption of sexual activity and the use of condoms. The same questionnaire was used for HIV-infected and HIV-uninfected women.
From March 2001 to June 2003, 980 pregnant women tested for HIV during antenatal visits and having delivered, were included in the DITRAME Plus cohort. After exclusion of 23 women lost to follow-up before delivery and 18 women having remained without any partner all over the post-partum followup, 939 women were eligible for this analysis, of which 546 were HIV-infected and 393 HIV-uninfected.
Methods
We studied the post-partum condom use among women who had resumed a regular sexual activity after delivery. Our main outcome was the systematic use of condoms at the time of the resumption of a sexual activity. The proportion of women having consistently used condoms was compared according to maternal HIV-status. The factors associated with the consistent use of condoms at the time of the resumption of sexual activity were identified in logistic regressions. We analysed the dynamics of the protection of sexual intercourses over time tanks to the proportion of women systematically using condoms at 3, 6, 12, 18 and 24 months postpartum (M3, M6, M12, M18 and M24, respectively).
Univariate analysis comprised: variables related to the woman (age, religion, education level, remunerated activity, age at first sexual intercourse, parity, existence of a co-spouse, type of housing, number of cohabiting family members, HIV-status and clinical AIDS stage [for HIV-infected women, according to the WHO Staging System of HIV Infection and Disease]), variables related to the partner (age, education level and HIV-status) and variables related to the infant characteristics (i.e. infant feeding practice implemented at birth and child survival). Group comparisons used non-parametric Mann–Whitney U-test for quantitative variables, and Pearson Chi-2 or Fisher’s exact tests for qualitative variables. Multivariable logistic regressions were performed and included all the variables described previously. A stepwise descendant procedure was then applied. All statistical analyses were carried out using SPSS software (version 12.0; SPSS Inc.).
Results
Baseline socio-demographic characteristics are detailed in Table 1. Compared to HIV-negative women, HIV-infected women were older and were more likely to live in a polygamous household or a shared housing. Most HIV-negative women (96.7%) disclosed their HIV-test result to their partners, whereas only 45.6% of HIV-infected women did it (p<0.001) (Table 1).
Table 1.
Socio-demographic characteristics of women at enrolment (DITRAME Plus, Abidjan, 2001–2005)
| HIV-infected women N=546 | HIV-negative women N=393 | p * | Overall N=939 | |
|---|---|---|---|---|
| Median age, in years (IQR) | 26 (23 – 30) | 25 (22 – 29) | 0.002 | 26 (22 – 30) |
| Median number of pregnancies (IQR) | 3 (2 – 5) | 3 (2 – 4) | 0.002 | 3 (2 – 5) |
| Median number of alive children (IQR) | 2 (1 – 3) | 2 (1 – 3) | 0.371 | 2 (1 – 3) |
| Education level (%) | ||||
| No education | 196 (35.9) | 123 (31.3) | 0.148 | 319 (34.0) |
| Primary school | 206 (37.7) | 145 (36.9) | 351 (37.4) | |
| Secondary school and above | 144 (26.4) | 125 (31.8) | 269 (28.6) | |
| Religion (%) | ||||
| Christian | 303 (55.5) | 241 (61.3) | 0.025 | 544 (57.9) |
| Muslim | 187 (34.2) | 130 (33.1) | 317 (33.8) | |
| Animist or no religion | 56 (10.3) | 22 (5.6) | 78 (8.3) | |
| Cohabiting with her partner (%) | 368 (67.4) | 269 (68.4) | 0.734 | 637 (67.8) |
| Declaring at least one co-spouse (%) | 119 (21.8) | 49 (12.5) | <0.001 | 168 (17.9) |
| Having a remunerated activity (%) | 280 (51.2) | 179 (45.5) | 0.083 | 459 (48.9) |
| Living in a shared housing † (%) | 358 (65.6) | 224 (57.0) | 0.008 | 582 (62.0) |
| Woman having disclosed her HIV-status to her partner (%) | 249 (45.6) | 381 (96.9) | <0.001 | 630 (67.1) |
| Woman having told her partner that she was included in a PMTCT project (%) | 267 (48.9) | 338 (86.0) | <0.001 | 605 (64.4) |
| Woman partner’s age (%) | n=194 | n=367 | N=561 | |
| 20 – 29 years | 50 (25.8) | 99 (27.0) | 0.836 | 149 (26.6) |
| 30 – 39 years | 105 (54.1) | 189 (51.5) | 294 (52.4) | |
| 40 years and above | 39 (20.1) | 79 (21.5) | 118 (21.0) | |
| Woman partner’s education level (%) | n=202 | n=373 | n=575 | |
| No education | 42 (20.8) | 70 (18.8) | 0.487 | 112 (19.5) |
| Primary school | 25 (12.4) | 54 (14.5) | 79(13.7) | |
| Secondary school | 100 (49.5) | 199 (53.3) | 299 (52.0) | |
| Higher education level | 35 (17.3) | 50 (13.4) | 85 (14.8) |
IQR, interquartile range.
Comparison HIV-infected vs. HIV-negative women: non-parametric Mann–Whitney U-test for quantitative variables, and Chi-2 or Fisher’s exact tests for qualitative variables.
Typical housing in Abidjan with several houses organized around a yard, where inhabitants share kitchen and restroom and live in crowded accommodations.
By 24 months post-partum, 80.2% and 90.8% of HIV-infected and uninfected women had regularly resumed a sexual activity, respectively (p<0.001). The median durations of postpartum abstinence were 20 weeks (range: 9 – 41) among HIV-infected women and 20 weeks also (range: 10 – 32) among the uninfected ones (p=0.20). Forty eight (11.4%) partners of HIV-infected women and 26 (7.3%) of HIV-negative women had been tested for HIV before resuming sexual intercourses (p=0.054).
Overall, 28% of women had systematically used condoms when they resumed their sexual activity after delivery; this proportion was very similar among HIV-infected and uninfected women (Odds ratio [OR] =1.02; 95% confidence interval [IC]: 0.63–1.65; p=0.934) (Table 2). Women with higher levels of education (secondary school or higher) were more likely to use condom systematically compared to those who were less educated (36.8% vs. 20.5%; OR=1.78; IC: 1.11–2.85; p=0.016). Muslim women compared to Christians (18% vs. 34.2%; OR=0.54; IC: 0.35–0.83; p=0.005) and those who were living with their partners compared to those living alone (25.7% vs. 35.1%; OR=0.68; IC: 0.47–1.00; p=0.05) were less likely to use condom during the resumption of the sexual activity. Neither women’s HIV-status nor disclosure of women’s HIV-status to their partners was significantly associated with the systematic use of condom during the resumption of sexual intercourses after delivery (Table 2). On the contrary, couples for which the male partner had been tested for the HIV before the resumption of the sexual activity were more likely to use condoms during the first intercourse after delivery (40.5% vs. 27.2%; p=0.016). This difference was no longer significative after adjustment on the variables detailed in the methods section (OR=1.52; IC: 0.90–2.58; p=0.115).
Table 2.
Determinants of consistent condom use among sexually active women, at the time of resumption of sexual intercourses. Univariate analysis and multivariate logistic regression (DITRAME Plus, Abidjan, 2001–2005)
| Variables | N = 776 | Women having used condom at resumption of sexual activity |
Multivariate analysis § |
|||
|---|---|---|---|---|---|---|
| % | p* | aOR# | 95% IC | p** | ||
| HIV status | 0.886 | 0.934 | ||||
| HIV-positive | 421 | 28.3 | 1.02 | 0.63 – 1.65 | ||
| VIH-negative | 355 | 28.7 | 1 | |||
| Age (in years) | 0.134 | 0.109 | ||||
| 18–19 | 50 | 32.0 | 1 | |||
| 20–24 | 261 | 32.2 | 1.10 | 0.56 – 2.18 | 0.773 | |
| 25–29 | 268 | 24.6 | 0.77 | 0.38 – 1.54 | 0.461 | |
| 30–34 | 133 | 24.1 | 0.85 | 0.40 – 1.84 | 0.694 | |
| 35 and above | 64 | 35.9 | 1.65 | 0.71 – 3.82 | 0.240 | |
| Education level | <0.001 | 0.051 | ||||
| No education | 254 | 20.5 | 1 | |||
| Primary school | 299 | 29.1 | 1.31 | 0.85 – 2.02 | 0.225 | |
| Secondary school and above | 223 | 36.8 | 1.78 | 1.11 – 2.85 | 0.016 | |
| Religion | <0.001 | 0.017 | ||||
| Christian | 456 | 34.2 | 1 | |||
| Muslim | 261 | 18.0 | 0.54 | 0.35 – 0.83 | 0.005 | |
| Animist or no religion | 59 | 30.5 | 0.91 | 0.49 – 1.67 | 0.761 | |
| Cohabiting with her partner | 0.008 | 0.050 | ||||
| No | 231 | 35.1 | 1 | |||
| Yes | 545 | 25.7 | 0.68 | 0.47 – 1.00 | ||
| Declaring at least one co-spouse | 0.025 | 0.072 | ||||
| No | 644 | 30.1 | 1 | |||
| Yes | 132 | 20.5 | 0.63 | 0.39 – 1.04 | ||
| Living in shared housing † | 0.328 | 0.199 | ||||
| No | 302 | 30.5 | 1 | |||
| Yes | 474 | 27.2 | 1.27 | 0.88 – 1.82 | ||
| Woman having disclosed her status to her partner | 0.314 | 393 | ||||
| No | 231 | 26.0 | 1 | |||
| Yes | 545 | 29.5 | 1.21 | 0.77 – 1.89 | ||
| Partner tested for HIV before the resumption of sexual activity | 0.016 | 0.115 | ||||
| No | 702 | 27.2 | 1 | |||
| Yes | 74 | 40.5 | 1.52 | 0.90 – 2.58 | ||
Chi-2 tests.
14 women whose data are not complete were excluded for analysis.
aOR, adjusted odds ratio. CI, confidence interval.
Wald test.
Typical housing in Abidjan with several houses organized around a yard, where inhabitants share kitchen and restroom and live in crowded accommodations
Among the 74 couples in which the male partners had been tested for HIV before the resumption of sexual activity, condom had been used by 7 of the 15 sero-concordant HIV-positive couples (60%), 17 of the 35 sero-discordant with an HIV-infected women couples (54%) and 2 of the 2 sero-discordant with an HIV-infected man couples.
The proportions of sexually active HIV-infected and HIV-negative women having consistently used condom were respectively 26.2% and 19.8% (p=0.193) at 3 months post-partum, 12.1% and 15.9% (p=0.139) at 12 months post-partum, 8.4% and 10.6%, (p=0.302) at 18 months post-partum (Figure 1). Only one sero-concordant HIV-positive couple and two sero-discordant couples reported having consistently used condoms at each visit.
Figure 1.
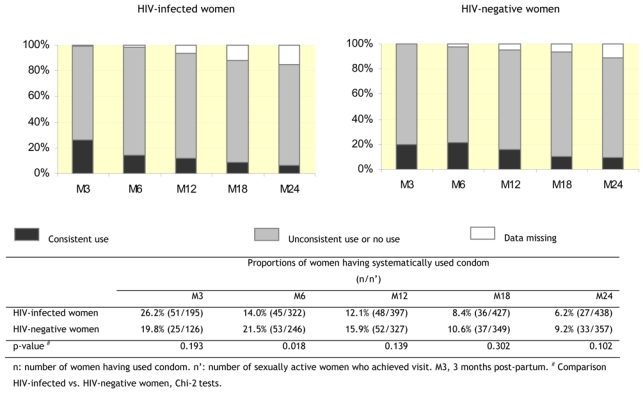
Proportions of sexually active women having declared to use condom systematically, at each post-partum visit (DITRAME Plus 3, Abidjan, 2001–2005)
Discussion
Less than one third of women were systematically using condom at the time of the resumption of the sexual activity after a pregnancy, in this cohort of women tested for HIV infection during pregnancy. This proportion was the same in HIV-infected and uninfected women. Disclosure of women’s HIV-status to their partners had no significant effect on this condom use. By 24 months post-partum, the proportion of women reporting having consistently used condom was divided by four among HIV-infected women and by two among HIV-negative women.
This lack of condom use had been reported previously in studies conducted in Côte d’Ivoire (Desgrees-du-Loû et al., 2002) and Burkina Faso (Nebié et al., 2001) among HIV-infected women only. However, in these studies, the use of condom was associated with the notification of women’s HIV-status to their partners: women having notified their seropositivity to their partner were more likely to use condoms during their sexual intercourse. On the contrary, in our study, we showed that couples were more likely to consistently use condoms when the male partner had been tested for HIV before the resumption of sexual activity; but this practice was long-term sustained. The impact of HIV testing on the adoption of safe sexual practices is therefore maximal when both women and men have been tested for HIV (Voluntary HIV-1 Counseling and Testing Efficacy Study Group, 2000).
Sexually active HIV-infected women were more likely to consistently use condom than HIV-negative women. However the proportion of women who declared systematically using condoms during their sexual intercourses decreased over time and this tendency was even stronger among HIV-infected women. By 24 months post-partum, condom use was as low as the one reported as a contraceptive method in the general population (INS & ORC Macro, 2001). In our study, the beneficial effect of counselling on the reduction of sexual transmission of HIV was important immediately after HIV testing. Similarly, a study conducted among patients of STIs clinics in the United States showed that the rate of condom use was high during the immediate period after HIV testing, and then decreased gradually for tending towards the rate of condom use observed in the general population (DiFranceisco et al., 2005).
The low rates of consistent condom use within African couples had been reported previously (Bauni & Obonyo, 2003; Muhwava, 2004; Cleland et al., 2006). Sexual intercourses within stable relationship are not considered as risky in terms of acquisition of HIV in comparison to extramarital sexual intercourses with occasional partners (Najjumba et al., 2003). The fact that condom is also a contraceptive method could be used by women to convince their partner to use it (Williamson et al., 2006; Cleland et al., 2006).
As a conclusion, although women had been prenatally tested for HIV and properly counselled on the sexual risk of HIV transmission, male partners were not tested for HIV before the resumption of sexual activity after delivery, very few couples were using condoms systematically and condom use was decreasing over time. Preventive sexual behaviours had not been adopted by either women who had not notified their partner of their HIV status, or by those who had. Among HIV-infected women, the risk management of HIV within the couples is also interfering with urgent social and/or emotional requirements such as the desire of pregnancy or the need for a normal sexual life. It is particularly difficult to deal with these two components at the same time. There is now an urgent need for innovative methods of the long-term prevention of the sexual transmission of HIV.
References
- Ahmed S, Lutalo T, Wawer M, Serwadda D, Sewankambo NK, Nalugoda F, et al. HIV incidence and sexually transmitted disease prevalence associated with condom use: a population study in Rakai, Uganda. AIDS. 2001;15:2171–2179. doi: 10.1097/00002030-200111090-00013. [DOI] [PubMed] [Google Scholar]
- Ali MM, Cleland J, Shah IH. Condom use within marriage: a neglected HIV intervention. Bulletin of the World Health Organization. 2004;82:180–186. [PMC free article] [PubMed] [Google Scholar]
- Allen S, Meinzen-Derr J, Kautzman M, Zulu I, Trask S, Fideli U, et al. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS. 2003;17:733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- ANRS 1201–1202 DITRAME PLUS Study Group. Field efficacy of zidovudine, lamivudine and single-dose nevirapine to prevent peripartum HIV transmission. AIDS. 2005;19:309–318. [PMC free article] [PubMed] [Google Scholar]
- Bauni EK, Obonyo J. The low acceptability and use of condoms within marriage: evidence from Nakuru District, Kenya. African Population Studies. 2003;18:51–65. [Google Scholar]
- Becquet R, Bequet L, Ekouevi DK, Viho I, Sakarovitch C, et al. Two-year morbidity–mortality and alternatives to prolonged breast-feeding among children born to HIV-infected mothers in Côte d’Ivoire . PLoS Medicine. 2007;4:e17–e31. doi: 10.1371/journal.pmed.0040017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brou H, Agbo H, Desgrées-du-Loû A. Impact of HIV counseling and testing during antenatal consultation for HIV-negative women in Abidjan (Côte d’Ivoire): a quantitative and qualitative study (DITRAME Plus 3 project, ANRS 1253) Cahiers Santé. 2005;15:81–91. [PubMed] [Google Scholar]
- Cleland J, Ali MM, Shah I. Trends in protective behaviour among single vs. married young women in Sub-Saharan Africa: the big picture. Reproductive Health Matters. 2006;14:17–22. doi: 10.1016/S0968-8080(06)28250-8. [DOI] [PubMed] [Google Scholar]
- Davis KR, Weller SC. The effectiveness of condoms in reducing heterosexual transmission of HIV. Family Planning Perspectives. 1999;31:272–279. [PubMed] [Google Scholar]
- Desgrées-du-Loû A, Msellati P, Viho I, Yao A, Yapi D, Kassi P, et al. Contraceptive use, protected sexual intercourse and incidence of pregnancies among African HIV-infected women. DIRAME ANRS 049 project, Abidjan 1995–2000. International Journal of STD & AIDS. 2002;13:462–468. doi: 10.1258/09564620260079617. [DOI] [PubMed] [Google Scholar]
- DiFranceisco W, Pinkerton S, Dyatlov R, Swain GR. Evidence of a brief surge in safer sex practices after HIV testing among a sample of high-risk men and women. Journal of Acquired Immune Deficiency Syndromes. 2005;39:606–612. [PubMed] [Google Scholar]
- Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bulletin of the World Health Organization. 2004;82:454–461. [PMC free article] [PubMed] [Google Scholar]
- Institut National de la Statistique (INS), & ORC Macro. Calverton. Maryland (USA): INS & Macro; 2001. Enquête démographique et de santé, Côte d’Ivoire 1998–1999. [Google Scholar]
- Muhwana W. Condom use within marriage and consensual unions in era of HIV/AIDS in Zimbabwe. African Population Studies. 2004;19:118–141. [Google Scholar]
- Najjumba MI, Ntozi J, Ahimbisibwe F, Odwee J, Ayiga N. Risk perception and condom use in Uganda. African Population Studies. 2003;18:67–80. [Google Scholar]
- Nebié Y, Meda N, Leroy V, Mandelbrot L, Yaro S, Sombié I, et al. Sexual and reproductive life of women informed of their HIV seropositivity: a prospective cohort study in Burkina Faso. Journal of Acquired Immune Deficiency Syndromes. 2001;28:367–372. doi: 10.1097/00126334-200112010-00010. [DOI] [PubMed] [Google Scholar]
- ONU. Sensibilisation au VHI/sida et comportements. New York: ONU, Départements des Affaires économiques et sociales, Division de la population; 2002. [Google Scholar]
- Pinkerton SD, Abramson PR. Effectiveness of condom in preventing HIV transmission. Social Science & Medicine. 1997;44:1303–1312. doi: 10.1016/s0277-9536(96)00258-4. [DOI] [PubMed] [Google Scholar]
- Tabi MM, Frimpong S. HIV infection of women in African countries. International Nursing Review. 2003;50:242–250. doi: 10.1046/j.1466-7657.2003.00206.x. [DOI] [PubMed] [Google Scholar]
- UNAIDS, & WHO. AIDS epidemic update: December 2006 2006 [Google Scholar]
- Voluntary HIV-1 Counseling and Testing Efficacy Study Group. Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: a randomised trial. Lancet. 2000;356:103–112. [PubMed] [Google Scholar]
- Williamson NE, Liku J, McLoughlin K, Nyamongo K, Nakayima F. A qualitative study of condom use among married couples in Kampala, Uganda. Reproductive Health Matters. 2006;14:89–98. doi: 10.1016/S0968-8080(06)28268-5. [DOI] [PubMed] [Google Scholar]


