Abstract
Conducting scientific research within a clinical practice area presents a variety of challenges. When the specialty area is hospice and palliative care, the collaborative task is particularly daunting. In this paper, we describe an ongoing study being conducted as a partnership between the University of Illinois at Chicago and a large metropolitan hospice organization. Our research is focused on engaging patients and their caregivers in a study measuring the effects of massage on cancer pain. The purpose of this paper is to describe both the lessons learned and the benefits accrued from collaboration between hospice practitioners and academic researchers. We present these process findings as guideposts for others considering end-of-life or palliative care research. Upon completion of the study in 2009, we will disseminate outcome findings in future papers.
Keywords: Cancer pain, hospice, massage
Ms. K was determined to “normalize” her situation, as many dying mothers attempt to do. With her young sons, it was important for her to be productive, to participate and continue to relate to them as a functional mother. She entered her pain and symptom data daily, at exactly the same time each evening. She wanted to be a part of upcoming weddings, to attend and design her own hat and dress so that she could look her best, despite her illness... One of her sons was trained to provide the massage; it provided quiet time for both, a time to be together, intimate and alone. Although already a close family unit, the touch prompted discussions, laughter and tears...
Mrs. C, a computer-literate woman, became very frustrated when she could not enter pain and symptom data and could not focus. She used the computer as a barometer for the stage of her illness. Once the pain medications were titrated and she could participate in the research, her mood changed. She dressed up, used makeup, had her hair done and conducted herself like a professional working on a project. She entered her data religiously and checked the accuracy of the medication notes that her caregiver entered. She reported that following her participation in the “caregiver” project, there was less bickering in the house...
These patients are not atypical. Pain, or its anticipation, remains one of the most feared symptoms of the dying process. Thus, it is not surprising that nine out of ten cancer patients report that they use some form of complementary therapy along with standard treatment.1 Among such adjuvant interventions, massage has been one of the most popular. Improved pain relief, mood enhancement and relaxation are widely recognized benefits of a single massage,2-8 but few controlled studies have been reported to evaluate the effect of multiple massages on cancer symptoms. Within the growing population of patients receiving hospice and palliative care, the cumulative effect of regular massage and its impact on quality of life are virtually unknown. To address this knowledge gap, we are examining the outcomes of massage therapy provided to patients with terminal cancer who are being cared for under the auspices of hospice. Congruent with the hospice philosophy of living each day as fully as possible, participation in research provides the opportunity to contribute to our collective knowledge, while conferring an additional dimension to the meaning found within illness.
Toward this end, we secured funding (RO1 NR009092) from the National Institutes of Health (NIH), National Institute of Nursing Research (NINR), for a one-week randomized clinical trial (RCT) to compare the effect of home-level hospice care with that of such care supplemented by 60-minute, full-body massages administered by a licensed massage therapist on five consecutive days. To date, we remain in the data collection stage of this research. Thus far we have successfully recruited and enrolled seventy-five subjects. Conducting research with individuals so close to end of life requires a delicate balance between scientific expediency and clinical compassion. While the ultimate goal is the measurement of massage's impact upon cancer pain and symptom distress, in our journey towards that end we have learned essential lessons we believe are applicable to others contemplating research collaboration within a hospice setting. The purpose of this paper is to describe both the lessons learned and the benefits accrued from collaboration between hospice practitioners and academic researchers.
Conducting a scientific study within a clinical practice area presents a variety of challenges. Our experience thus far reflects some of the difficulties intrinsic to melding research with practice. Since the hospice population is by definition among the most frail of patient cohorts, the insights we have gleaned magnify both the rewards and pitfalls of marrying science to care. In seeking to expand our knowledge of the benefits of daily massage on cancer pain, we have deepened our understanding of the nature of collaboration necessary if we are to offer our patients the full breadth of healthcare expertise. In what follows, we offer our findings as this process continues to unfold. At the beginning of the third year of this four-year study, we continue to learn as we move toward our desired goal of 200 participants in the RCT. At that time, a subsequent paper will present outcomes and analysis. For purposes of clarity and organization, we will discuss our findings thus far in the form of four of the most essential collaborative lessons learned and the benefits accrued from them. Before doing so, however, we begin with a brief overview of the study design and methodology.
Study Overview: Design and Methods
This one-week RCT includes pretest and posttest measures to compare effects of standard hospice care with effects of standard hospice care as supplemented by massages given on five consecutive days by a licensed massage therapist. We will measure the effects on pain, symptom distress (including pain, fatigue, insomnia, nausea, appetite, bowel patterns, concentration, appearance, breathing, outlook, and cough), sleep and mood in 200 cancer patients receiving home level hospice care in their homes or within nursing homes. Concurrently, in a one-week descriptive study with 60 caregivers of the RCT patients, we are exploring the caregiver burden associated with caregivers administering 30-minute massages on three consecutive days after they have completed two training sessions with a licensed massage therapist.
Our research team partnered with a hospice organization serving a large metropolitan area with diverse ethnic representation. The mission of this not-for-profit, community-based organization is to provide comfort and preserve dignity at the end of life. In keeping with this goal, the hospice agency instituted a complementary and alternative medicine (CAM) component that includes massage therapy, with the costs absorbed by the organization. Since most third-party reimbursement does not cover such “alternative” therapies, access to these palliative measures are prohibitive to many potential recipients.
Marketing our study to hospice staff and patients was important for study enrollment. Together with the hospice staff, we developed brochures describing the study, its risks and benefits, and inclusion/exclusion criteria. These brochures are colorful and can be placed in the orientation packet that the admitting nurse provides to all new patients. To strengthen retention and assure comfort and satisfaction, the study design includes daily telephone contact with both experimental and control subjects. The study was designed to be conducted with hospice patients living in their own homes and within skilled-care facilities.
Our inclusion criteria require that the patient: (1) be admitted and receiving home level hospice or palliative care; (2) have a diagnosis of advanced cancer; (3) be experiencing self-defined pain or taking pain medications on a daily basis; (4) be 18 years or older; (5) speak, read and write English; and (6) have a life expectancy of 2.5 to 3 weeks as suggested by a score of 40 or higher on the Palliative Performance Scale (PPS).9, 10 The PPS is a scale used to predict survival time by measuring a patient's level of consciousness and his/her ability to eat, drink, move around, perform activities, and take care of self. Patients are excluded if they: (1) are legally blind; (2) have cognitive or physical impairments inhibiting communication and/or the completion of computerized study instruments; (3) have platelet counts of less than 10,000 mm3 or other signs/symptoms of thrombocytopenia; or (4) have participated in the hospice's CAM program that includes massage therapy.
Eligible subjects are referred to the study by the hospice nurse, who introduces the possibility of participation to newly admitted patients. Participating patients use a small, touch screen laptop computer (pentablet) to report in detail their pain, symptom distress, mood state, sleep quality and demographic information at baseline (Figure 1). Subjects are also instructed how to complete a short daily log using the pentablet, which remains in the home for the duration of the study, so they can report their pain, mood and sleep for the previous 24 hours. Subjects are asked to complete the log each evening at approximately the same time (6-10 pm) for two weeks. Those completing 90% of the requested data during the “run-in” (first week) and willing to continue are then randomized during the second week to receive either usual hospice care (control group) or usual care supplemented by five daily massages (experimental group). All subjects are asked to complete the detailed computerized questionnaire again before and after a five-day period and to complete the computerized daily log. Experimental group subjects are also asked to enter their pain and mood scores before and after each massage. Participants in the control group will receive two study-funded massages after completion of the RCT as an incentive to participate in the study.
Figure 1.
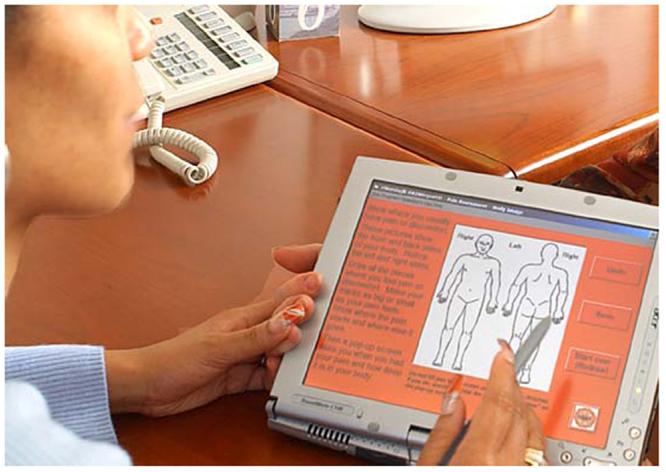
A research assistant tests the PAINReportIt® program on a touch screen, pentablet computer. © 2008, Diana Wilkie, used by permission.
All licensed massage therapists are trained on study procedures by a study team member who is also a massage therapist and is, in turn, supervised by the project director and principal investigator. To ensure continuity of care and consistency, the same therapist administers all massages to those within the experimental group. Before and after each treatment, the massage therapist records 60-second heart and respiratory rates. Following the massage, the therapist enters pertinent details related to the intervention on the massage therapy record, such as actual length of the massage, body areas massaged and any pain felt by the patient. The treatment protocol is adhered to as closely as is possible, but because of the unique characteristics of the vulnerable hospice population, there is freedom and flexibility to adapt treatment to individual needs. If, for instance, the patient feels too frail to sustain 60 minutes of massage, the sessions can be curtailed, as long as the treatment lasts a minimum of 30 minutes per session.
Following the completion of the five treatments, the licensed massage therapist provides two training sessions for those caregivers that are interested in learning about massage and giving massages to their loved ones. Given the high cost of trained massage therapists, this approach will let us determine the feasibility of and strain on the caregiver giving massages to their loved ones or family members. The benefits of such an approach are considered in the concluding section. At this point, we shift focus from methodology to obstacles encountered and lessons learned.
Collaborative Lessons and Benefits
Lesson One: Collaborating with Sensitivity
The process of conducting an RCT with seriously ill patients and their often exhausted caregivers is rife with both challenge and opportunity for improvement in the science and care of the dying. The research team was stretched to adapt and redefine the study design from paper to the daily realities of hospice care. Similarly, the hospice organization was called upon to address the stringent requirements of rigorous scientific study. It was not, for example, an easy adjustment for hospice providers to remain “blind” to who participated in the study. Reciprocally, researchers accustomed to controlled conditions and precise protocol were required to remain open and flexible when confronted by the continual flux and occasional chaos attendant to life with the dying.
As we conceived of the steps necessary for implementation, we strove to remain mindful of the cultural differences not only among study participants but between researchers and clinicians as well. Thus, we required that the research staff be familiar with and trained in dealing with very ill, frail and terminal patients. In addition, they were expected to respect and reflect the concerns of the caregivers, who were both concerned and protective of their loved ones. To facilitate the necessary sensitivity, the research team employed a nurse with considerable experience in hospice and home care to act as the Research Specialist (RS) and liaison to the hospice staff and patients. She was thus well equipped to deal with such emotionally charged situations as visiting a home when the patient's death was imminent or the patient has died while the RS was traveling to the home.
Lesson Two: Collaborating with Collegiality
Researchers and clinicians both found the road toward collaboration a bit bumpy at times. Hospice staff expressed confusion, dissatisfaction or both on multiple levels, including disappointment that the massages were not provided at their discretion. Some also acknowledged feelings of impotence as case managers who were accustomed to orchestrating all services provided to their patients because study protocol, not the case manager, guided the way that the massages were provided to study patients. Thoughtful recognition of the feelings of loss was important to finding a solution that clarified the roles of the researchers and clinicians and empowered the hospice massage coordinator to schedule the massages according to the study protocol.
A written record of pain medications taken by the patient was needed as a study outcome, but often was missing when the researcher visited a study patient. Although clinicians teach patients' caregivers to record the dose and time that each drug is taken, many obstacles prevented them from doing so. Examples of common obstacles include stress, information overload, memory problems, lack of clarity about the task, and homes with little space for papers to be kept reliably from week to week. Together the RS and clinicians found a plan for a common medication sheet to be placed in a patient-designated location for safekeeping as a way to share the valuable medication information and reduce the patient's and caregiver's burden of repeating the information to multiple people.
Lesson Three: Collaboration with Humility
Despite the best laid plans and most rigorous methodology, some phenomena defy control. So it is with death. The research team attempted to design a referral process that would engender information relevant to determining eligibility and would disclose factors in the home environment that might jeopardize enrollment: for example, very protective caregivers. This plan proved to be a humbling undertaking, as hospice clinicians know all too well. Hospice nurses who provide care in the home frequently lament that insufficient information renders them ill-equipped to manage their patients with the precision and efficiency they desire. One of the primary tools for determining hospice care as well as study eligibility, the Palliative Performance Scale (PPS), can be notoriously unreliable in predicting an individual patient's decline. PPS scores, determined at the time of admission, may undergo drastic fluctuations within a period of 24-48 hours, thus dramatically affecting patient eligibility.
Patients' schedules also proved to be obstacles to study design. From previous work in our pilot study, we found that patients alive three to five days after enrollment were more likely to live long enough to complete a five day study. We thus designed a “run-in” period as a method to reduce attrition after randomization, always a dire threat to study external validity. Our data thus far supports the value of such a period in that we have little attrition after day five. Therefore, our protocol calls for five massages on five consecutive days beginning at the conclusion of the “run-in” period. Daily realities, however, were frequently less orderly. Unexpected visitors, outside commitments, and sudden lurches in physical decline or hospitalizations all can interfere with the protocol plan but are random, often unpredictable events that are part of the fluctuating course during the last weeks of life. Confronted by such unexpected contingencies, the only possible response is a humble restructuring of expectations. To ensure optimal consistency, the hospice massage coordinator reassessed patient status and communicated directly with the RS. As for the discrepancies in protocol, while all efforts are made to conform to the prescribed schedule, we have learned that when an individual has limited time remaining, study protocol must never be a burden or take priority over other life closure activities. The research team members, some of whom are experienced hospice clinicians themselves, skillfully adapt the protocol to maintain the rigor of a randomized clinical trial and document changes required because of the patient's context.
Lesson Four: Collaborating with Ambivalence
As pain is such a highly individualized experience, objective measurement is slippery at best. To obtain optimal applicability, we considered baseline pain as a multidimensional phenomenon. Our measurement tool, PAINReportIt®,11 is a software program developed by eNursing llc in Seattle, WA (www.enursingllc.com) that includes an electronic version of the McGill Pain Questionnaire (MPQ) (1970 version).12 Ron Melzack, who holds the copyright to the MPQ, authorized the modifications of his tool. An interactive, touch screen method for multidimensional pain assessment, PAINReportIt® can be self-administered and requires little to no prior computer experience. Directions from the MPQ were modified to address the touch screen method of recording patient responses. In PAINReportIt®, the patient simply touches the computer screen with a plastic stylus to indicate painful areas, appropriate descriptive words and other item responses. For what had been the handwritten, narrative portion of the MPQ, the patient types on a standard keyboard or touches the keys on a virtual layout. Though this might prove to be a challenge to debilitated or heavily medicated patients, our subjects proved to be eager to learn and capable of utilizing the keyboard. Indeed, our preliminary findings suggest this has been a source of great personal satisfaction for many of the participants.
Despite these adaptations and revisions, the measurement of pain was often an arduous and laborious task. As the hospice patient became weaker and frailer, it took longer to complete even the streamlined questionnaires. What we had anticipated as a 30- to 45-minute process became much longer, with patients needing frequent rests due to fatigue. At the beginning or the study, it was not unusual for individuals to require 2-3 hours to tell their story as they completed the eligibility, consent, and data collection process. This amount of time concerned the researchers until the timed feature of PAINReportIt® revealed that the longest amount of time it took a hospice patient to complete the MPQ part of the tool was 46 minutes. And some patients completed the tool in only 6 minutes. Most patients did it in about 10 to 20 minutes, not much longer than the paper tool12, 13 or the computer tool when used in other populations.11 Yet, it is a challenge to measure pain in the grip of exhaustion. To reduce the ambivalence with which one approaches pain measurement, the RS will read the questions and assist the patients to input their answers as needed and note the amount of assistance in the research record.
The challenges presented by the need for increased sensitivity, collegiality, humility and tolerance of ambivalence are some of the more formidable obstacles with which we have grappled thus far. The union of science and practice can be problematic—even contentious—at times. But the rewards are deeply gratifying, as the benefits of these hard-won lessons convey. It is always within the lived experiences of our patients that true significance is revealed.
Benefit: The Gratification of Learning
Mr. K is an African American gentleman in his mid-seventies. Having worked the majority of his life as a day laborer, he regretted the missed opportunities to address his own vibrant sense of curiosity. The demands of providing a livelihood for support of his family left little time or energy for intellectual pursuits. He was thus thrilled to be offered the chance to experience and master the intricacies of computer technology and the massage study design. He stood in his doorway each morning awaiting the arrival of the RS. Always, he made a point to include his seven-year-old nephew so that he could demonstrate his newly acquired technological proficiency. When he encountered difficulty in entering the data, he refused the help of his computer-savvy younger family members, insisting on calling the RS for computer assistance and solving the problem himself. In the final days of his life, he articulated to the RS his great pride in his role as a research subject entering his own data for posterity.
Benefit: The Gratification of Giving Back
A teacher by profession, Ms. R had lived as a paragon of organizational efficiency. Her church had been the primary recipient of her skills, but in her final weeks of life she wanted to demonstrate to her 16-year-old grandson, with whom she lived, the importance of full engagement in life and the obligation to give back, to leave something behind. She used her participation in the study as an opportunity to model willingness to undertake new challenges while remaining open to all life has to offer and all that it demands.
Benefit: The Gratification of Physical and Psychological Intimacy
Mr. C was 50 years old, diagnosed with advanced pancreatic cancer. He lived with his wife, a busy corporate executive, in the western suburbs of Chicago, Illinois. Despite a demanding schedule, which often kept her at work until late at night, Mrs. C was adamant in her desire to learn the massage technique so she could offer that gift to her husband. In separate interviews, the couple testified to the enormous comfort they drew from the experience. The administration and reception of therapeutic and intentional touch gave them both a “special feeling” that they could “grasp hold of.” It was, they explained, like making a “marriage date,” a way to normalize a highly stressful and uncertain time. They were less interested in the physiological benefits than in the deep psychological value they found in such physical intimacy. It relaxed them both and allowed them a measure of peace. Together they found respite “far from the maddening crowd.”
Conclusion
We are only into the third year of our study. There will be more obstacles (such as shorter length of stay), further challenges (such as more Spanish-speaking patients who do not meet eligibility criteria), and with them, increased insight into the complexities of collaboration. Hospice and palliative care practitioners need the objective validity that scientific study affords. In a climate of often cold and indifferent budget allocations, only clear evidence makes a credible argument for funding. Intuitively, we believe that massage provides a potent analgesia. Our challenge is to forge a pathway toward knowledge on which researchers and clinicians travel in partnership toward establishing evidentiary truth.
The patients and subjects we have met thus far have taught us well. As Mrs. C discovered, there is far less in-house “bickering” when we cooperate toward a mutually beneficial and worthwhile goal. We must work together to integrate these lessons into our collective knowledge for the sake of those awaiting the release promised by the touch that seeks to ease the pain and other symptoms.
Acknowledgement
This publication was made possible by Grant Number RO1 NR009092 from the National Institutes of Health, National Institute of Nursing Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Nursing Research.
We are grateful to Kevin Grandfield for editorial assistance, Marilyn Ward for administrative assistance, David Shuey for graphics, and the hospice patients who shared their wisdom as study participants.
Contributor Information
Geraldine Gorman, Dept. of Public Health, Mental Health, and Administrative Nursing University of Illinois at Chicago.
Jeannine Forest, Dept. of Medical-Surgical Nursing, University of Illinois at Chicago.
Stephen J. Stapleton, University of Illinois at Chicago, College of Nursing.
Noreen A. Hoenig, Dept. of Medical-Surgical Nursing, University of Illinois at Chicago.
Michael Marschke, Horizon Hospice and Palliative Care 833 W. Chicago Ave. Chicago, IL 60622.
Jan Durham, Horizon Hospice and Palliative Care 833 W. Chicago Ave. Chicago, IL 60622.
Marie L. Suarez, Dept. of Medical-Surgical Nursing, University of Illinois at Chicago.
Diana J. Wilkie, Dept. of Medical-Surgical Nursing (MC 802), University of Illinois at Chicago, 845 S. Damen Ave., Room 660, Chicago, IL 60612-7350, diwilkie@uic.edu.
References
- 1.Yates JS, Mustian KM, Morrow GR, et al. Prevalence of complementary and alternative medicine use in cancer patients during treatment. Support Care Cancer. 2005 Oct;13(10):806–811. doi: 10.1007/s00520-004-0770-7. [DOI] [PubMed] [Google Scholar]
- 2.Meek SS. Effects of slow stroke back massage on relaxation in hospice clients. Image J Nurs Sch. 1993;25(1):17–21. doi: 10.1111/j.1547-5069.1993.tb00748.x. [DOI] [PubMed] [Google Scholar]
- 3.Ferrell-Torry AT, Glick OJ. The use of therapeutic massage as a nursing intervention to modify anxiety and the perception of cancer pain. Cancer Nurs. 1993;16(2):93–101. [PubMed] [Google Scholar]
- 4.Simpson J. Massage: positive strokes in palliative care. N Z Nurs J. 1991;84(6):15–7. [PubMed] [Google Scholar]
- 5.Sims SER. Relaxation training as a technique for helping patients cope with the experience of cancer: a selective review of the literature. Journal of Advanced Nursing. 1987;12(5):583–91. doi: 10.1111/j.1365-2648.1987.tb03048.x. [DOI] [PubMed] [Google Scholar]
- 6.Weinrich SP, Weinrich MC. The effect of massage on pain in cancer patients. Appl Nurs Res. 1990;3(4):140–5. doi: 10.1016/s0897-1897(05)80135-1. [DOI] [PubMed] [Google Scholar]
- 7.Grealish L, Lomasney A, Whiteman B. Foot massage. A nursing intervention to modify the distressing symptoms of pain and nausea in patients hospitalized with cancer. Cancer Nurs. 2000;23(3):237–43. doi: 10.1097/00002820-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Post-White J, Kinney ME, Savik K, Gau JB, Wilcox C, Lerner I. Therapeutic massage and healing touch improve symptoms in cancer. Integr Cancer Ther. 2003;2(4):332–44. doi: 10.1177/1534735403259064. [DOI] [PubMed] [Google Scholar]
- 9.Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative performance scale (PPS): a new tool. J Palliat Care. 1996;12(1):5–11. [PubMed] [Google Scholar]
- 10.Virik K, Glare P. Validation of the palliative performance scale for inpatients admitted to a palliative care unit in Sydney, Australia. J Pain Symptom Manage. 2002;23(6):455–7. doi: 10.1016/s0885-3924(02)00407-4. [DOI] [PubMed] [Google Scholar]
- 11.Wilkie DJ, Judge MK, Berry DL, Dell J, Zong S, Gilespie R. Usability of a computerized PAINReportIt in the general public with pain and people with cancer pain. Journal of Pain & Symptom Management. 2003;25(3):213–24. doi: 10.1016/s0885-3924(02)00638-3. [DOI] [PubMed] [Google Scholar]
- 12.Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–99. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 13.McGuire DB. Assessment of pain in cancer patients using the McGill pain Questionnaire. Oncology Nursing Forum. 1984;11:32–7. [PubMed] [Google Scholar]


