Abstract
Rationale and Objectives: Patients with severe asthma have a poor therapeutic response to corticosteroid therapy, and corticosteroid responsiveness cannot be easily measured in these patients. We hypothesized that this poor response is associated with a reduced effect of corticosteroids to inhibit cytokine release from activated peripheral blood mononuclear cells (PBMCs).
Methods: Patients with severe asthma were defined by American Thoracic Society criteria. We compared the suppression of LPS-induced cytokine release (monocyte chemotactic protein-1 [MCP-1], macrophage inflammatory protein [MIP] 1α, RANTES, tumor necrosis factor α, interleukin 1β (IL-1β), IL-8, IFN-γ, IL-6, IL-10, and granulocyte-macrophage colony–stimulating factor [GM-CSF]) by dexamethasone from PBMCs of patients with severe asthma (n = 16), patients with nonsevere asthma (n = 19), and normal volunteers (n = 10).
Results: There was no difference in baseline spontaneous or stimulated release of these cytokines among groups. LPS-induced release of 10 cytokines was less suppressed by dexamethasone (10−6 M) in patients with severe asthma compared with patients with nonsevere asthma, with statistical significance achieved for IL-1β (p < 0.03), IL-8 (p < 0.03), and MIP-1α (p < 0.003), and borderline significance for IL-6 (p = 0.054). There was less difference between the two groups for dexamethasone at 10−8 M. Nuclear histone deacetylase (HDAC) and histone acetyltransferase activities were reduced in patients with severe asthma compared with patients with nonsevere asthma (p < 0.01). HDAC activity reduction correlated directly to the degree of steroid insensitivity of GM-CSF (r = 0.57, p < 0.01) and IFN-γ (r = 0.56, p < 0.05) release. Reduction in histone acetyltransferase activity related to corticosteroid use rather than asthma severity.
Conclusions: Patients with severe asthma have diminished corticosteroid sensitivity of PBMCs when compared with patients with nonsevere asthma, associated with a reduction in HDAC activity that parallels the impaired corticosteroid sensitivity.
Keywords: corticosteroids, histone acetyltransferase, histone deacetylase, severe asthma
Patients with asthma usually control their symptoms well with inhaled corticosteroids and long-acting β2-agonists, but a minority of patients continue to have uncontrolled asthma despite these treatments. These latter patients with severe asthma suffer greater morbidity, face a higher risk of asthma death, and consume a greater proportion of health resources than other patients with asthma (1). Patients with severe asthma may present with more severe symptoms or greater lung function impairment or may experience more frequent exacerbations. The pattern of disease may differ between patients. Some patients with severe asthma have repeated exacerbations but minimal interval symptoms; others rarely exacerbate but have persistent airway obstruction. Therefore, a definition of severe asthma must encompass many aspects of severity to capture patients with severe asthma with differing clinical phenotypes. The definition put forth by the American Thoracic Society (ATS) requires the presence of at least two of seven minor criteria despite the use of high-dose inhaled corticosteroids or the long-term use of oral steroids (1). A European Respiratory Society workshop has proposed a definition for severe asthma that is equally broad (2).
The fact that patients with severe asthma have uncontrolled asthma despite taking high doses of inhaled corticosteroids, sometimes together with oral corticosteroids, has led to the hypothesis that patients with severe asthma are relatively resistant to the therapeutic effect of corticosteroids. Such patients are not absolutely resistant to the effects of corticosteroids because stopping corticosteroid therapy usually leads to a worsening of asthma in these patients. Rather, such patients, often labeled as having corticosteroid-dependent asthma, have a partial impaired response to corticosteroids. The cellular counterpart of steroid responsiveness has been studied, particularly in small groups of patients with asthma defined as having corticosteroid-resistant asthma, in whom there is persistence of airway obstruction and failure of the FEV1 to improve by 15% of baseline after 10 to 14 d of high-dose oral corticosteroids, typically 40 mg of prednisolone daily (3). In such patients, the induction of proliferation of peripheral blood mononuclear cells (PBMCs) is less suppressible by corticosteroids when compared with that from patients with corticosteroid-sensitive asthma (4, 5), indicating that such an in vitro response could be used as a measure of corticosteroid responsiveness. There are few data regarding release of cytokines in vitro from PBMCs of patients with severe asthma.
We have hypothesized that patients with severe asthma may be a subset of patients with asthma who have persistent symptoms and poor control despite receiving corticosteroid therapy because their asthmatic inflammatory response is relatively resistant to suppression, as reflected in the degree of corticosteroid suppression of cytokine release from PBMCs. We therefore measured the ability of dexamethasone to suppress the release of cytokines from PBMCs in patients with severe asthma compared with PBMCs from patients with nonsevere asthma. Because histone acetylation status as determined by histone deacetylase (HDAC) and histone acetyltransferase (HAT) activities is an important determinant of the inflammatory response and of corticosteroid responsiveness, we also assayed these activities in PBMCs.
Part of this work has been previously presented at the 2005 American Thoracic Society meeting (6).
METHODS
Patients
Asthma was diagnosed by a physician and had FEV1 reversibility of 12% or greater or methacholine PC20 of less than 8 mg/ml. Current and ex-smokers with more than 5 pack-years of smoking history were excluded. Patients with severe asthma (n = 16) were defined according to guidelines developed by the Severe Asthma Research Program based on ATS criteria (1). They had one or two major criteria for corticosteroid usage and had three or more minor criteria, with 13 having five or more. Patients who did not meet the criteria for severe asthma were classified as having nonsevere asthma (n = 19) and used 1,000 μg or less of inhaled beclomethasone dipropionate equivalent per day. Healthy volunteers (n = 10; two women; 37.6 ± 2.4 yr of age; FEV1%predicted = 98 ± 5.0) with no asthma, using no medications, and who had never smoked were recruited. All participants gave informed consent to a protocol approved by the ethics committee of Royal Brompton and Harefield NHS Trust/National Heart and Lung Institute.
Isolation and Stimulation of PBMCs
Venous blood (80 ml) was diluted 1:1 with Hanks' buffered saline solution and layered on Ficoll-Hypaque-Plus (Amersham plc, Buckinghamshire, UK). After centrifugation (30 min at 1,100 × g and 18°C), PBMCs were collected, washed, and centrifuged (250 × g for 10 min). PBMCs were resuspended in culture media and counted using Kimura dye. They were plated (7.5 × 105 cells/well) and stimulated with LPS (10 μg/ml) with or without dexamethasone (10−6 or 10−8 M). Supernatants were removed 18 h later and analyzed for 10 cytokines. Nuclear extracts were obtained from PBMCs (4 × 106 cells) for assay of HDAC and HAT activities. To determine whether the sensitivity of PBMCs was reflected in that of monocytes, we isolated monocytes from unfractionated PBMCs by plate adherence and stimulated with LPS and dexamethasone as described previously.
Measurement of Cytokine Release
Cell-culture supernatants were mixed with microsphere beads (Beadlyte; Upstate Technology, Dundee, UK) coated with capture antibodies to monocyte chemotactic protein-1 (MCP-1), macrophage inflammatory protein 1α (MIP-1α), RANTES (regulated upon activation, normal T-cell expressed and secreted), tumor necrosis factor α (TNF-α), interleukin 1β (IL-1β), IL-8, IFN-γ, IL-6, IL-10, and granulocyte-macrophage colony–stimulating factor (GM-CSF). Biotinylated reporter antibodies were added to bind the microsphere bead–cytokine complexes. Finally, a fluorophore, streptavidin-phycoerythrin, was added to bind the biotinylated reporter, thus emitting a fluorescent signal, measured in a Luminex 100 laser spectrophotometer (Luminex, Austin, TX). Microsphere beads for each cytokine emitted a unique ratio of two other fluorophores. Cytokine concentrations were converted from mean fluorescence intensity from standard curves.
Measurement of HDAC and HAT Activities
HDAC activity was measured using a fluorescent derivative of an epsilon- acetyl lysine assay substrate (HDAC Fluorescent Activity Assay Kit; Biomol International, Exeter, UK), which was deacetylated by incubation with samples and combined with a developer to generate a measurable fluorophore. HAT activity was measured by ELISA (HAT Activity Assay Kit; Upstate Biotechnology). Samples were mixed with acetyl-CoA and incubated for 30 min on a plate precoated with histone H4. Acetylated histones were detected using an anti–acetyl-lysine rabbit polyclonal antibody followed by a horseradish peroxidase–based colorimetric assay.
Data Analysis
Results were expressed as means ± SEM. The differences in each cytokine released between LPS and LPS plus dexamethasone treatment were calculated and ranked, and multivariate analysis of variance (ANOVA) was performed to determine differences between severe and nonsevere asthma. Significance was taken at p < 0.05.
RESULTS
A comparison of the baseline data of patients with severe and nonsevere asthma is presented in Table 1. Patients with severe asthma had more severe airflow obstruction (p < 0.01) and bronchial hyperresponsiveness (p < 0.05).
TABLE 1.
CHARACTERISTICS OF PATIENTS WITH NONSEVERE AND SEVERE ASTHMA
| Nonsevere Asthma | Severe Asthma | p Value | |
|---|---|---|---|
| No. | 19 | 16 | |
| Sex, F/M | 9/10 | 13/3 | < 0.05 |
| Age, yr | 43.1 ± 10.9 | 41.9 ± 12.8 | NS |
| Race | 4 Asian, 15 white | 1 Asian, 15 white | NS |
| Duration of asthma | 19.5 ± 16.1 | 27.0 ± 15.0 | NS |
| Inhaled corticosteroid dose, μg BDP equivalent | 400 ± 750* (11) | 2,000 ± 1,720* (16) | < 0.0001 |
| Receiving oral corticosteroids (n) | 0 | 9 | |
| FEV1, L | 2.87 ± 0.76 (18) | 1.84 ± 0.70 (15) | < 0.001 |
| FEV1% predicted | 80.5 ± 21.6 (18) | 59.7 ± 21.3 (15) | < 0.01 |
| FEV1/VC, % | 71.8 ± 11.0 (18) | 66.2 ± 9.3 (15) | NS |
| Bronchodilator reversibility, % | 10.1 ± 8.0 (16) | 21.4 ± 19.8 (15) | NS |
| PC20, mg/ml (geometric SD)† | 1.51 (5.5) (17) | 0.35 (6.2) (8) | < 0.05 |
| Exhaled nitric oxide, ppb | 24.6 ± 70.1 (17) | 38.5 ± 39.7 (14) | NS |
| Blood eosinophils, % | 4 ± 3.2 (16) | 4.9 ± 5.2 (16) | NS |
| Blood neutrophils, % | 60.9 ± 10.8 (16) | 61.3 ± 18.8 (16) | NS |
| Blood lymphocytes, % | 24.6 ± 8.0 (16) | 24.3 ± 10.4 (16) | NS |
| Blood monocytes, % | 4.4 ± 1.2 (16) | 3.8 ± 1.6 (16) | NS |
| BAL neutrophils, % | 0.63 ± 0.66 (13) | 2.59 ± 1.82 (7) | < 0.002 |
| BAL eosinophils, % | 0.36 ± 0.44 (13) | 1.74 ± 2.1 (7) | < 0.05 |
| Serum IgE, IU/ml | 318.4 ± 320 (16) | 129.2 ± 187 (16) | NS |
Definition of abbreviations: BAL = bronchoalveolar lavage; BDP = beclomethasone dipropionate; F = female; M = male; NS = not significant; PBL = peripheral blood leukocyte; PC20 = provocative concentration of methacholine causing a 20% fall in FEV1.
Values represent mean ± SD (with number of measurements in parentheses), except where otherwise noted.
Median ± SD.
Geometric mean (geometric SD).
Baseline and LPS-stimulated Cytokine Release
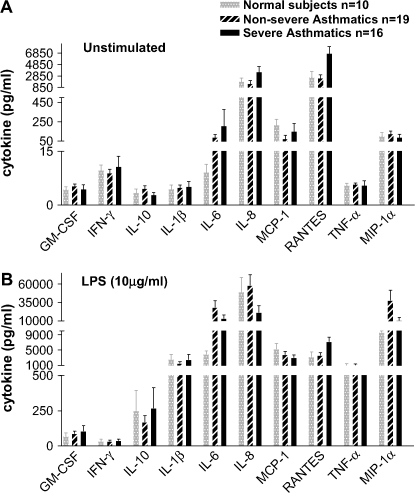
Baseline release of GM-CSF, IFN-γ, IL-10, IL-1β, and TNF-α was close to the limit of detection, thus reducing the validity of between-group comparisons for these cytokines (Figure 1A). Among the other five cytokines, levels did not significantly differ between patients with severe asthma and patients with nonsevere asthma. LPS-stimulated cytokine release was also similar between patients with severe asthma and patients with nonsevere asthma (Figure 1B).
Figure 1.
Concentrations of 10 different cytokines in cell culture supernatants of unstimulated peripheral blood mononuclear cells (PBMCs) (A) and of PBMCs stimulated with LPS (10 μg/ml) (B) from normal volunteers, patients with nonsevere asthma, and patients with severe asthma. There were no significant differences between patients with severe asthma and patients with nonsevere asthma. GM-CSF = granulocyte-macrophage colony–stimulating factor; IFN-γ = interferon-γ; IL = interleukin; MCP-1 = monocyte chemotactic protein-1; MIP = macrophage inflammatory protein; TNF = tumor necrosis factor.
Corticosteroid Suppression of Cytokine Release
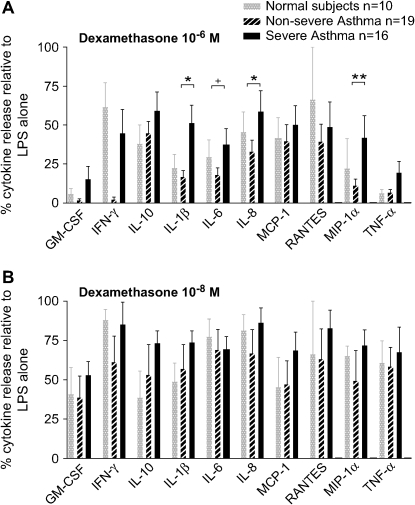
For each patient, cytokine release after dexamethasone preincubation, together with LPS stimulation, was expressed as a percentage of the value of cytokine release after LPS stimulation alone above baseline (Figure 2). There was a trend to less cytokine suppression by dexamethasone 10−6 M (Figure 2A) in PBMCs from patients with severe asthma compared with patients with nonsevere asthma for all 10 cytokines. We used a multivariate ANOVA to analyze the suppressed level of each cytokine by dexamethasone (10−6 M). There was significance for IL-1β (p < 0.03), IL-8 (p < 0.03), and MIP-1α (p < 0.003), and borderline significance for IL-6 (p = 0.054). There was no difference in the suppression of any of the 10 cytokines by dexamethasone at 10−8 M between the severe and the nonsevere asthma groups (Figure 2B).
Figure 2.
Effect of dexamethasone 10−6 M (A) and 10−8 M (B) on the suppression of release of 10 cytokines from PBMCs stimulated by LPS (10 μg/ml). Data are expressed as the percentage of cytokine release after exposure to LPS. *p < 0.05; **p < 0.01 between patients with severe and nonsevere asthma.
In three subjects, unfractionated PBMCs were compared with monocytes (Figure 3), and the degree of steroid suppression of each individual cytokine correlated extremely highly between the two cell populations. Two data points for Patients A (IFN-γ and RANTES) and B (GM-CSF and IFN-γ) and one data point for Patient C (GM-CSF) are omitted because cytokine levels for monocytes or PBMCs in these cases failed to rise with LPS stimulation.
Figure 3.
Comparison of sensitivity to dexamethasone (10−6 M) between PBMCs and monocytes of a patient with severe asthma (A) and two patients with nonsevere asthma (B and C). Each panel shows the correlation between percentage cytokine release in monocytes and percentage cytokine release in PBMCs for eight different cytokines.
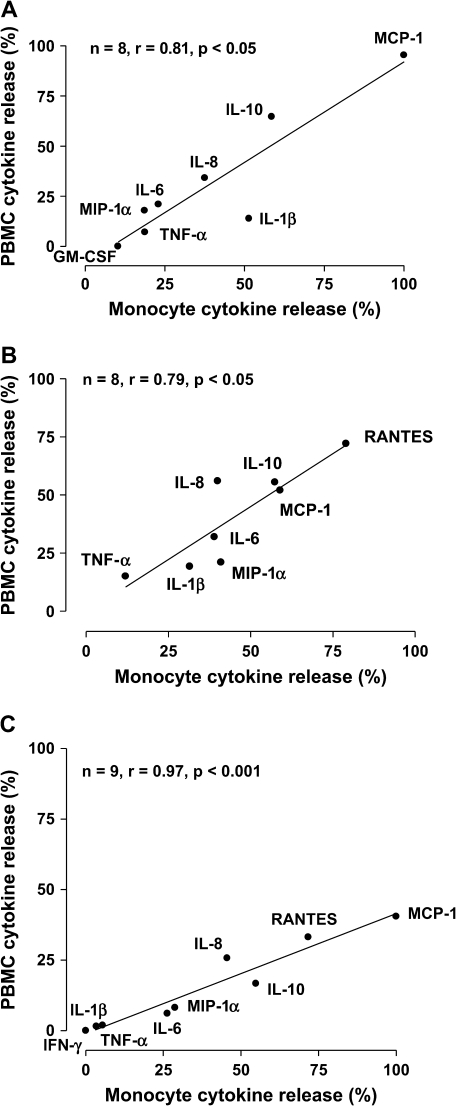
HDAC Activity
PBMCs from patients with severe asthma had less HDAC activity (4.59 ± 0.72 vs. 7.97 ± 0.68 μM/10 μg protein; p < 0.01) than PBMCs from patients with nonsevere asthma (Figure 4). The difference was significant regardless of whether the latter subjects were taking inhaled corticosteroids (4.59 ± 0.72 vs. 8.14 ± 0.91 μM/10 μg protein; p < 0.01) or not (4.59 ± 0.72 vs. 7.73 ± 1.10 μM/10 μg protein; p < 0.05; Figure 4). Among patients with nonsevere asthma, there was no difference in HDAC activity between those taking inhaled corticosteroids and those who were not (8.14 ± 0.91 vs. 7.73 ± 1.10 μM/10 μg protein; p = not significant [NS]).
Figure 4.
Individual histone-deacetylase (HDAC) activities in PBMCs from normal individuals, patients with nonsevere asthma, and patients with severe asthma. The patients with nonsevere asthma are divided into those not receiving inhaled corticosteroids (ICS−) and those receiving inhaled corticosteroids (ICS+). *p < 0.05; **p < 0.01; NS = not significant.
HAT Activity
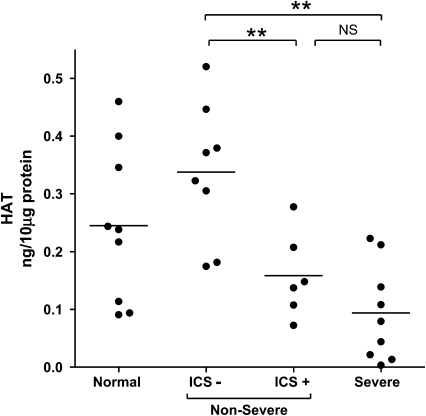
PBMCs from patients with severe asthma had lower HAT activity (0.093 ± 0.029 vs. 0.261 ± 0.036 ng/10 μg protein; p < 0.01) than PBMCs from patients with nonsevere asthma. When patients with nonsevere asthma were stratified according to their use of inhaled corticosteroids (Figure 5), HAT activity was still lower in PBMCs from patients with severe asthma than in those from patients with steroid-naive nonsevere asthma (0.093 ± 0.029 vs. 0.338 ± 0.042 ng/10 μg protein; p < 0.01). However, there was no difference in HAT activity between patients with severe asthma and patients with nonsevere asthma who were taking inhaled corticosteroids (0.093 ± 0.029 vs. 0.158 ± 0.030 ng/10 μg protein; p = NS). Among patients with nonsevere asthma, there was significantly less HAT activity in those who were taking inhaled steroids (0.158 ± 0.030 vs. 0.338 ± 0.042 ng/10 μg protein; p < 0.01) than in those who were not.
Figure 5.
Individual histone acetyltransferase (HAT) activities in PBMCs from normal individuals, patients with nonsevere asthma, and patients with severe asthma. The patients with nonsevere asthma are divided into those not receiving inhaled corticosteroids (ICS−) and those receiving inhaled corticosteroids (ICS+). **p < 0.01.
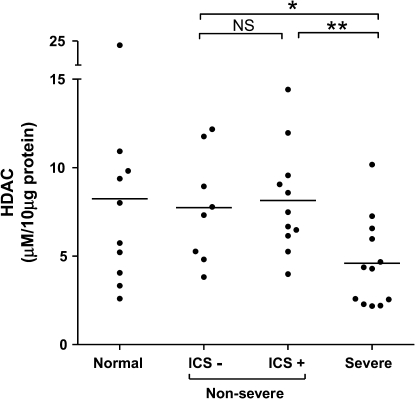
Relationship between Steroid Suppression of Cytokine Release to HDAC Activity
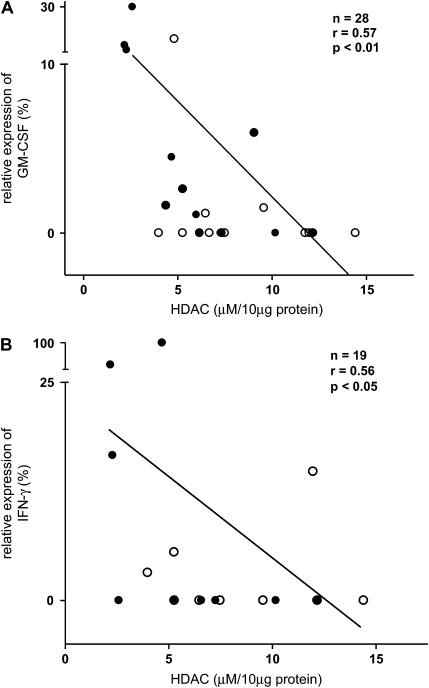
HDAC activity correlated inversely to the percentage of cytokine release with dexamethasone (10−6 M), of GM-CSF (r = −0.569; p < 0.01; Figure 6A), and IFN-γ (r = −0.556; p < 0.05; Figure 6B), such that the lower the HDAC activity, the greater the steroid insensitivity. In contrast to HDAC, HAT activity did not correlate to the degree of steroid suppression of any cytokine.
Figure 6.
Correlation between relative steroid suppression of cytokine release for GM-CSF (A) and IFN-γ (B) and total HDAC activity. Closed circles indicate severe asthma; open circles indicate nonsevere asthma.
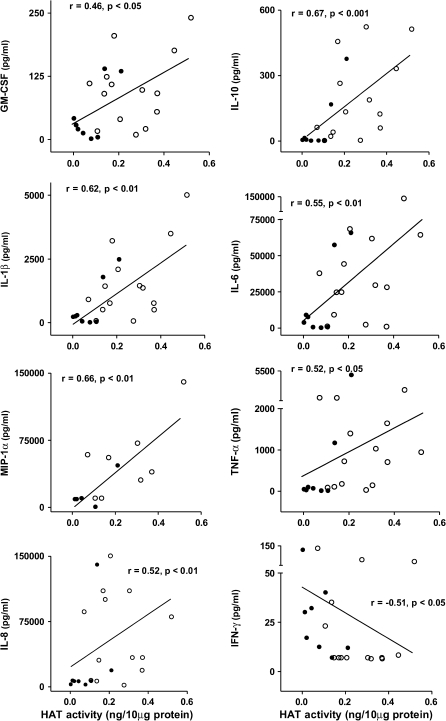
Relationship of LPS-induced Cytokine Release to HAT Activity
There were significant correlations between LPS-induced cytokine release for seven cytokines (GM-CSF, IL-10, IL-1β, IL-6, IL-8, TNF-α, and MIP-1α) and HAT activity (Figure 7). In contrast, LPS-induced IFN-γ release was inversely correlated to HAT activity. LPS-induced cytokine release correlated with HDAC activity for only IL-6 (r = 0.39, p < 0.05) and TNF-α (r = 0.43, p < 0.05).
Figure 7.
Relationship between LPS-induced release of eight cytokines and total HAT activity in PBMCs. There was a positive correlation between the levels of cytokine release and HAT activity for seven of the cytokines, except for IFN-γ, where there was a negative correlation. Closed circles indicate severe asthma; open circles indicate nonsevere asthma.
DISCUSSION
Our results show that patients with severe asthma, defined according to ATS criteria, have diminished corticosteroid sensitivity of their circulating PBMCs when compared with patients with nonsevere asthma. We used LPS as a stimulator of these cells and measured the release of 10 cytokines. We showed that at the higher dose of 10−6 M of dexamethasone, there was less reduction of cytokine release in cells from patients with severe asthma compared that from patients with nonsevere asthma; however, this difference was not observed at the concentration of 10−8 M of dexamethasone. In addition, we found that the total activities of the two enzymes that determine histone acetylation status, HDAC and HAT, were reduced in patients with severe asthma compared with patients with nonsevere asthma, indicating potential involvement of these enzymes in determining the relative corticosteroid insensitivity in PBMCs from patients with severe asthma.
The lack of inhibition of a monocyte-derived neutrophil activating factor and of cytokines such as TNF-α, IL-1β, and GM-CSF from blood monocytes by corticosteroids of patients with corticosteroid-resistant asthma as compared with patients with corticosteroid-sensitive asthma has been described (7, 8). TNF-α–induced GM-CSF release from PBMCs was also found to be less suppressible by exogenous dexamethasone in a group of patients with corticosteroid-resistant and corticosteroid-dependent asthma (9). In these studies, the severity of the patients with asthma was not clearly defined. Our study is the first to indicate that there is an impairment of corticosteroid suppression of cytokine release measured in PBMCs from patients with severe asthma. The corticosteroid sensitivity of different cytokines released from PBMCs compared with that from monocytes in three patients with asthma indicates that the monocyte within the PBMC population is likely to be the cell being tested for corticosteroid sensitivity. This makes sense because LPS is known to activate monocytes to cause release of the cytokines that we have measured, but this does not exclude potential interactions between monocytes and lymphocytes in the response of PBMCs to LPS. A reduction in the inhibitory effects of corticosteroids on the proliferation of blood lymphocytes from patients with corticosteroid-resistant asthma has been reported (4, 5).
Monocytes and macrophages are sensitive to LPS, which induces an array of cytokines through the transmembrane signaling receptor Toll-like receptor 4, which activates several intracellular signaling pathways, such as nuclear factor-κB (NF-κB) and the mitogen-activated protein kinase pathways (10, 11). For example, the transcriptional induction of GM-CSF, IL-8, TNF-α, or RANTES is dependent on the activation of IκB kinase NF-κB, which binds to and activates coactivator molecules through the acetylation of core histones, leading to increased cytokine gene transcription (12–14). Corticosteroids are likely to inhibit the expression of these cytokines through the reversal of histone acetylation at the site of the cytokine gene expression by direct binding of the activated corticosteroid receptor to NF-κB–associated coactivators or by recruitment of HDACs to the activated transcription complex (15, 16). There was no difference in the spontaneous release or in the LPS-stimulated release of these cytokines between patients with severe and patients with nonsevere asthma, indicating that the differences in steroid sensitivity observed were not related to a greater expression of cytokines, probably reflecting no differences in intracellular signaling induced by LPS between the two groups. We found that in terms of differences between severe and nonsevere asthma, there was less suppression of at least 7 of the 10 cytokines assayed in PBMCs of severe asthma, with significant differences for IL-8, MIP-1α, and IL-1β (and with borderline significance for IL-6). Differences were less obvious for the release of IL-10, MCP-1, and RANTES. One potential explanation for these different sensitivities may be the differential contribution of corticosteroid-sensitive intracellular pathways, such as NF-κB or mitogen-activated protein kinase activation, induced by LPS.
HAT and HDAC are families of enzymes that regulate the structure of chromatin which ultimately modulates the gene expression of inflammatory genes (17). Acetylation of histones by coactivator proteins, such as cAMP response element binding (CREB)-binding protein p300 and TAFII250, which possess HAT activity, leads to DNA unwinding, which allows transcription factors and RNA polymerase II to initiate gene transcription (18). On the other hand, deacetylation of histones leads to the repression of transcription (19). It has therefore been proposed that the balance of histone acetylation and of histone deacetylation may determine the inflammatory state. Glucocorticoids have been shown to suppress inflammatory gene expression, and this effect may involve the recruitment of HDACs to the transcriptional machinery complex by the activated glucocorticoid receptor (20, 21).
Changes in HDAC and HAT activity have been previously described in bronchial biopsies of patients with nonsevere asthma (21). Compared with normal subjects, these subjects had a reduction in HDAC activity and a reciprocal increase in HAT activity. In patients treated with inhaled corticosteroids, the reduction in HDAC and the increase in HAT activity were attenuated (21). Because repression of HAT activity and recruitment of HDAC activity is caused by corticosteroids in vitro (21, 22), these results were interpreted as reflecting the effect of corticosteroids in inhibiting HAT and recruiting HDAC activities. In our study, HDAC and HAT activities were significantly reduced in PBMCs from patients with severe asthma compared with patients with nonsevere asthma, indicating that changes in chromatin modification in severe asthma are more complex than the reciprocal change in the activities of HAT and HDAC described in nonsevere asthma.
Our key finding was that HDAC activity in PBMCs from patients with severe asthma was reduced when compared with patients with nonsevere asthma. Furthermore, HDAC activity in patients with nonsevere asthma was not influenced by inhaled corticosteroid use, suggesting that inhaled steroids do not contribute to changes in HDAC activity in PBMCs. The reduction in HDAC activity in PBMCs from patients with severe asthma correlated with the impairment of steroid responsiveness of GM-CSF and IFN-γ release, supporting a link between diminished HDAC activity and the development of steroid insensitivity in severe asthma. By contrast, the reduction in HAT activity in PBMCs from patients with severe asthma is probably due to the use of high-dose inhaled (and oral) corticosteroids rather than asthma severity because HAT activity in patients with severe asthma was not significantly different from the subgroup of patients with nonsevere asthma taking inhaled corticosteroids. Furthermore, HAT activity was reduced in patients with nonsevere asthma on inhaled corticosteroids when compared with those not on this therapy. These findings are consistent with the in vitro inhibition of histone acetylation by glucocorticoids found previously (17). We also found that among patients with asthma, HAT activity was reduced in parallel with the reduction of inflammatory gene expression by dexamethasone for 7 of the 10 cytokines (except IFN-γ) assayed, indicating that the reduction in HAT activity is related to corticosteroid use but dissociated from asthma severity. We do not have an adequate explanation for the inverse relationship obtained for IFN-γ.
Prior treatment with corticosteroids was unlikely to have influenced PBMC responsiveness because we found no difference in corticosteroid sensitivity among the patients with severe asthma who took regular oral prednisolone in comparison to those that did not take oral corticosteroids. The effect of oral prednisolone therapy on corticosteroid responsiveness is unknown, but a 10-d course of prednisolone at a dose of 40 mg/d had no effect on the number or affinity of corticosteroid receptors on PBMCs (23). The reduced sensitivity of PBMCs to corticosteroid in patients with corticosteroid-dependent asthma has been reproduced by incubating PBMCs from nonasthmatic volunteers with a combination of IL-2 and IL-4, and this was associated with a reduction in affinity of the glucocorticoid receptor (GR) on PBMCs, including T cells (23, 24). In this study of steroid-dependent severe asthma, the binding affinity of dexamethasone to the glucocorticoid receptor was threefold higher than that of patients with corticosteroid-dependent asthma, which could account for the differences in cytokine inhibition by corticosteroids.
Our data show that PBMCs of patients with severe asthma express relative corticosteroid insensitivity. It is not known whether this abnormality would be reflected in lung macrophages, such as bronchoalveolar lavage macrophages. A recent study has demonstrated that nuclear translocation of the glucocorticoid receptor α by dexamethasone is impaired in alveolar macrophages of patients with glucocorticoid-insensitive asthma, indicating that this abnormality could occur in alveolar macrophages of patients with severe asthma (25). Whether this is an intrinsic defect of PBMCs or an acquired defect (e.g., secondary to the effect of circulating mediators) is not known. In addition, it is not known whether the degree of corticosteroid sensitivity measured in the PBMCs reflects disease severity, although our corticosteroid sensitivity does not seem to correlate with various markers of severity of asthma.
In summary, severe asthma is characterized by a greater degree of steroid insensitivity measured in PBMCs than nonsevere asthma, along with a reduction in HDAC and HAT activities. Our results indicate that diminished HDAC activity may be linked to the presence of relative steroid insensitivity in severe asthma, whereas reduced HAT activity probably relates to corticosteroid use rather than disease severity. Determining the mechanisms underlying impaired steroid responsiveness may yield new therapeutic targets for severe asthma.
Acknowledgments
The authors thank Dr. Trevor Hansel and Dr. Terry Tetley for the use of Luminex equipment.
Supported by NIH-RO1 grant HL-69155.
Originally Published in Press as DOI: 10.1164/rccm.200512-1930OC on April 13, 2006
Conflict of Interest Statement: M.H. has no financial relationship with a commercial entity that has an interest in the subject of the manuscript. P.B. has no financial relationship with a commercial entity that has an interest in the subject of the manuscript. A.T. has no financial relationship with a commercial entity that has an interest in the subject of the manuscript. S.M. has no financial relationship with a commercial entity that has an interest in the subject of the manuscript. N.K. has no financial relationship with a commercial entity that has an interest in the subject of the manuscript. P.J.B. has received research funding and has served on scientific advisory boards for GlaxoSmithKline (GSK), AstraZeneca, Boehringer Ingelheim, Novartis, Altana, Scios, and Pfzier. I.A. has no financial relationship with a commercial entity that has an interest in the subject of the manuscript. K.F.C. has received $4,700 in 2005 for participation on the advisory boards of AstraZeneca, Altana, Colgene, and Novartis and $5,700 for lecturing at meetings sponsored by AstraZeneca, Altana, GSK, and Novartis. He has been reimbursed by Boehringer Ingelheim and by Novartis for traveling to international conferences. He has received an unrestricted research grant from GSK ($50,000 in 2005) and $25,000 in 2005 from Novartis for participation in a clinical trial.
The Severe Asthma Research Program (SARP) is a multicenter asthma research group funded by the NHLBI and consists of the following contributors (Steering Committee members are indicated with an asterisk): Brigham and Women's Hospital—Elliot Israel,* Bruce D. Levy, Gautham Marigowda; Cleveland Clinic Foundation—Serpil C. Erzurum,* Raed A. Dweik, Suzy A.A. Comhair, Abigail R. Lara, Marcelle Baaklini, Daniel Laskowski, Jacqueline Pyle; Emory University—W. Gerald Teague,* Anne M. Fitzpatrick, Eric Hunter; Imperial College School of Medicine—K. Fan Chung,* Mark Hew, Pankaj Bhavsar, Alfonso Torrego, Sally Meah, Mun Lim; National Jewish Medical and Research Center—Sally E. Wenzel,* Diane Rhodes; University of Pittsburgh & University of Texas Medical Branch—William J. Calhoun,* Bill T. Ameredes, Melissa P. Clark, Renee Folger, Rebecca Z. Wade, Dori Smith; University of Virginia—Benjamin Gaston,* Robin Kelly, Peter Urban; University of Wisconsin—William W. Busse,* Nizar Jarjour, Erin Billmeyer, Cheri Swenson, Gina Crisafi; Wake Forest University—Eugene R. Bleecker,* Deborah Meyers, Wendy Moore, Stephen Peters, Annette Hastie, Gregory Hawkins, Jeffrey Krings, Regina Smith; Washington University in St. Louis—Mario Castro,* Leonard Bacharier, Iftikhar Hussain, Jaime Tarsi; Data Coordinating Center—James R. Murphy,* Douglas Curran-Everett; NHLBI—Patricia Noel.*
References
- 1.American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med 2000;162:2341–2351. [DOI] [PubMed] [Google Scholar]
- 2.Chung KF, Godard P, Adelroth E, Ayres J, Barnes N, Barnes P, Bel E, Burney P, Chanez P, Connett G, et al. Difficult/therapy-resistant asthma: the need for an integrated approach to define clinical phenotypes, evaluate risk factors, understand pathophysiology and find novel therapies. ERS Task Force on Difficult/Therapy-Resistant Asthma. European Respiratory Society. Eur Respir J 1999;13:1198–1208. [DOI] [PubMed] [Google Scholar]
- 3.Woolcock AJ. Corticosteroid-resistant asthma: definitions. Am J Respir Crit Care Med 1996;154:S45–S48. [DOI] [PubMed] [Google Scholar]
- 4.Corrigan J, Brown PH, Barnes NC, Tsai J-J, Frew AJ, Kay AB. Glucocorticoid resistance in chronic asthma. Am Rev Respir Dis 1991;144:1016–1025. [DOI] [PubMed] [Google Scholar]
- 5.Spahn JD, Landwehr LP, Nimmagadda S, Surs W, Leung DY, Szefler SJ. Effects of glucocorticoids on lymphocyte activation in patients with steroid-sensitive and steroid-resistant asthma. J Allergy Clin Immunol 1996;98:1073–1079. [DOI] [PubMed] [Google Scholar]
- 6.Hew M, Bhavsar PK, Torrego A, Barnes PJ, Adcock I, Chung KF. Cytokine profiling of peripheral blood mononuclear cells in severe asthma: decreased suppression of GM-CSF, IFNγ and IL-6 by dexamethasone. Proc Am Thorac Soc 2005;2:A369. [Google Scholar]
- 7.Wilkinson JRW, Crea AEG, Clark TJH, Lee TH. Identification and characterization of a monocyte-derived neutrophil-activating factor in corticosteroid-resistant bronchial asthma. J Clin Invest 1989;84:1930–1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lane SJ, Wilkinson JR, Cochrane GM, Lee TH, Arm JP. Differential in vitro regulation by glucocorticoids of monocyte-derived cytokine generation in glucocorticoid-resistant bronchial asthma. Am Rev Respir Dis 1993;147:690–696. [DOI] [PubMed] [Google Scholar]
- 9.Matthews JG, Ito K, Barnes PJ, Adcock IM. Defective glucocorticoid receptor nuclear translocation and altered histone acetylation patterns in glucocorticoid-resistant patients. J Allergy Clin Immunol 2004;113:1100–1108. [DOI] [PubMed] [Google Scholar]
- 10.Guha M, Mackman N. LPS induction of gene expression in human monocytes. Cell Signal 2001;13:85–94. [DOI] [PubMed] [Google Scholar]
- 11.Sweet MJ, Hume DA. Endotoxin signal transduction in macrophages. J Leukoc Biol 1996;60:8–26. [DOI] [PubMed] [Google Scholar]
- 12.Koch A, Giembycz M, Ito K, Lim S, Jazrawi E, Barnes PJ, Adcock I, Erdmann E, Chung KF. MAP-kinase modulation of NF-κB-induced GM-CSF release from human alveolar macrophages. Am J Respir Cell Mol Biol 2004;30:342–349. [DOI] [PubMed] [Google Scholar]
- 13.Koch A, Giembycz M, Stirling RG, Lim S, Adcock I, Wassermann K, et al. Effect of smoking on MAP kinase-induced modulation of IL-8 in human alveolar macrophages. Eur Respir J 2004;23:805–812. [DOI] [PubMed] [Google Scholar]
- 14.Shakhov AN, Collart MA, Vassalli P, Nedospasov SA, Jongeneel CV. Kappa B-type enhancers are involved in lipopolysaccharide-mediated transcriptional activation of the tumor necrosis factor alpha gene in primary macrophages. J Exp Med 1990;171:35–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kagoshima M, Ito K, Cosio B, Adcock IM. Glucocorticoid suppression of nuclear factor-kappa B: a role for histone modifications. Biochem Soc Trans 2003;31:60–65. [DOI] [PubMed] [Google Scholar]
- 16.Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids: new mechanisms for old drugs. N Engl J Med 2005;353:1711–1723. [DOI] [PubMed] [Google Scholar]
- 17.Barnes PJ, Adcock IM, Ito K. Histone acetylation and deacetylation: importance in inflammatory lung diseases. Eur Respir J 2005;25:552–563. [DOI] [PubMed] [Google Scholar]
- 18.Ogryzko VV, Schiltz RL, Russanova V, Howard BH, Nakatani Y. The transcriptional coactivators p300 and CBP are histone acetyltransferases. Cell 1996;87:953–959. [DOI] [PubMed] [Google Scholar]
- 19.Roth SY, Denu JM, Allis CD. Histone acetyltransferases. Annu Rev Biochem 2001;70:81–120. [DOI] [PubMed] [Google Scholar]
- 20.Ito K, Barnes PJ, Adcock IM. Glucocorticoid receptor recruitment of histone deacetylase 2 inhibits interleukin-1beta-induced histone H4 acetylation on lysines 8 and 12. Mol Cell Biol 2000;20:6891–6903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ito K, Caramori G, Lim S, Oates T, Chung KF, Barnes PJ, et al. Expression and activity of histone deacetylases in human asthmatic airways. Am J Respir Crit Care Med 2002;166:392–396. [DOI] [PubMed] [Google Scholar]
- 22.Ito K, Jazrawi E, Cosio B, Barnes PJ, Adcock IM. p65-Activated histone acetyltransferase activity is repressed by glucocorticoids: mifepristone fails to recruit HDAC2 to the p65-HAT complex. J Biol Chem 2001;276:30208–30215. [DOI] [PubMed] [Google Scholar]
- 23.Irusen E, Matthews JG, Takahashi A, Barnes PJ, Chung KF, Adcock IM. p38 Mitogen-activated protein kinase-induced glucocorticoid receptor phosphorylation reduces its activity: role in steroid-insensitive asthma. J Allergy Clin Immunol 2002;109:649–657. [DOI] [PubMed] [Google Scholar]
- 24.Kam JC, Szefler SJ, Surs W, Sher ER, Leung DY. Combination IL-2 and IL-4 reduces glucocorticoid receptor-binding affinity and T cell response to glucocorticoids. J Immunol 1993;151:3460–3466. [PubMed] [Google Scholar]
- 25.Goleva E, Li LB, Eves PT, Strand MJ, Martin RJ, Leung DY. Increased glucocorticoid receptor β alters steroid response in glucocorticoid-insensitive asthma. Am J Respir Crit Care Med 2006;173:607–616. [DOI] [PMC free article] [PubMed] [Google Scholar]