Abstract
Purpose: Limited data exist describing risk factors for mortality in patients having predominantly emphysema.
Subjects and Methods: A total of 609 patients with severe emphysema (ages 40–83 yr; 64.2% male) randomized to the medical therapy arm of the National Emphysema Treatment Trial formed the study group. Cox proportional hazards regression analysis was used to investigate risk factors for all-cause mortality. Risk factors examined included demographics, body mass index, physiologic data, quality of life, dyspnea, oxygen utilization, hemoglobin, smoking history, quantitative emphysema markers on computed tomography, and a modification of a recently described multifunctional index (modified BODE).
Results: Overall, high mortality was seen in this cohort (12.7 deaths per 100 person-years; 292 total deaths). In multivariate analyses, increasing age (p = 0.001), oxygen utilization (p = 0.04), lower total lung capacity % predicted (p = 0.05), higher residual volume % predicted (p = 0.04), lower maximal cardiopulmonary exercise testing workload (p = 0.002), greater proportion of emphysema in the lower lung zone versus the upper lung zone (p = 0.005), and lower upper-to-lower-lung perfusion ratio (p = 0.007), and modified BODE (p = 0.02) were predictive of mortality. FEV1 was a significant predictor of mortality in univariate analysis (p = 0.005), but not in multivariate analysis (p = 0.21).
Conclusion: Although patients with advanced emphysema experience significant mortality, subgroups based on age, oxygen utilization, physiologic measures, exercise capacity, and emphysema distribution identify those at increased risk of death.
Keywords: chronic obstructive pulmonary disease, computed tomography, mortality, prognosis, pulmonary function
Chronic obstructive pulmonary disease (COPD) is associated with significant morbidity and mortality (1), and studies defining long-term survival have documented widely varied survival rates (2). Numerous factors have been reported to influence prognosis, including FEV1 (1, 3, 4), inspiratory capacity (5), diffusion capacity for carbon monoxide (DlCO) (6–8), hypoxemia (2, 9), hypercarbia (2, 7, 8, 10), impaired exercise capacity (2, 4, 11–15), sex (16), body mass index (BMI) (4, 17–19), dyspnea (20), and health status (13, 21). The clinical phenotype of the patient with COPD may also impact prognosis (22), as early investigators suggested that emphysema is associated with a worse prognosis than chronic bronchitis or asthma (7, 23). More robust predictors of increased risk of death in advanced COPD would be useful clinically, and in investigating potential therapeutic interventions.
The National Emphysema Treatment Trial (NETT) offers a unique opportunity to define the natural history of a large group of patients with COPD with clinically and radiologically defined emphysema and severe chronic airflow obstruction (24, 25).
METHODS
Patient Selection
The study group of 609 patients includes all patients randomized to medical therapy at 17 clinics as part of the NETT (25), except for one patient who received lung volume reduction surgery outside of the NETT for whom the surgery date was unknown. A total of 35 of the 609 patients received lung volume reduction surgery outside of the NETT, and an additional 18 of the 609 patients received a lung transplant during the NETT; their mortality data are censored as of the date of surgery or transplant. The design and methods of the trial have been previously detailed, and are enumerated in the online supplement (24, 25). All patients provided written, informed consent, and the study was approved by the institutional review board at each clinic. Baseline measurements were completed after pulmonary rehabilitation but before randomization.
Clinical Assessment
Demographic data and smoking and medical history were collected by patient interview using standardized instruments. Health status was assessed using the Quality of Well-Being scale, the Medical Outcomes Study Short Form 36-item health survey, and the St. George's Respiratory Questionnaire (26). Dyspnea was quantified using the University of California, San Diego, Shortness of Breath Questionnaire (UCSD SOBQ) (27). Oxygen utilization was obtained by patient report and characterized as positive if patient was using oxygen at rest or during sleep or exercise.
Physiologic Testing
Patients underwent spirometry and plethysmographic lung volume measurement after the administration of albuterol; diffusing capacity, respiratory pressures, and arterial blood gases were also measured. The protocol used for 6-min-walk testing (6MWT) has been described in detail and provided the maximal distance walked (28). Maximal exercise capacity was measured on a cycle ergometer with an increment of 5 or 10 W/min after 3 min of unloaded pedaling with the patient breathing 30% oxygen.
Diagnostic Imaging Studies
The severity and distribution of emphysema were determined from chest computed tomography (CT) scans obtained during full inspiration. Data were evaluated using a standard reconstruction kernel, with image analysis performed using a custom-built software program (29). After segmentation, the image voxels within each field were labeled as being emphysema-like based upon their X-ray attenuation coefficient or Hounsfield unit. The distribution of the number of voxels at each Hounsfield unit was plotted with Hounsfield unit values less than −950 corresponding to severe emphysema. Hounsfield unit values of −910 and −850 have roughly corresponded to moderate or mild emphysema regions, respectively. Percent emphysema for the whole lung was calculated, as was the difference between the upper and lower lung regions in percent emphysema. The α value (see the online supplement) was calculated for the whole lung, as was the difference in α between the upper and lower lung regions. Lungs with greater proportions of small lesions have a steep slope and a large α, whereas lungs with larger lesions have a smaller α (30).
BMI, Airflow Obstruction, Dyspnea, Exercise Capacity Index
The BODE (Body mass index, airflow Obstruction, Dyspnea, Exercise capacity) index is an 11-point composite score (0–10) in which higher scores indicate poorer outcomes (4). We modified the original BODE by using the UCSD SOBQ as the dyspnea measure, as the Medical Research Council dyspnea scale was not used in the NETT. The contribution of dyspnea to the BODE score was based on quartile distribution of the UCSD SOBQ in our 609-person sample. A UCSD SOBQ score of less than or equal to 52 contributed 0 points toward the BODE score, whereas a score from 53 through 63 contributed 1 point, a score of 64 through 77 contributed 2 points, and a score of 78 or higher contributed 3 points.
Statistical Analysis
Means and standard deviations are reported for baseline characteristics. The overall mortality rate from all causes was calculated as number of deaths per 100 person-years of follow-up. Cause of death was obtained by review of death certificates in a subset of patients (see the online supplement). Univariate comparisons of mortality rates by risk factors were performed using Cox proportional hazards regression analysis. For continuous risk factor variables with no obvious clinical cut-off point for defining healthy versus unhealthy groups, a least-healthy group was identified as the poorest performing quintile on that measure. The reference group for these variables was then defined as the remaining 80% of the distribution. For maximal exercise capacity, the thresholds predictive of differential mortality after lung volume reduction surgery were used (25). For BMI, both upper and lower quintiles were examined, whereas the middle 60% of the BMI distribution was used as the reference. Importantly, the lower threshold was quite similar to a validated threshold (4). Kaplan-Meier mortality curves were created to display differences in mortality by selected risk factors. Differences between mortality curves were assessed using the log rank test.
Two multivariate Cox proportional hazards models were used to identify the variables that predicted mortality after adjusting for all other variables. In the first model, all variables tested with univariate analysis, except the modified BODE index, were included. The second model was the same as the first, except that the modified BODE index replaced BMI, FEV1, dyspnea, and 6MWT distance.
RESULTS
The study cohort consisted of 609 patients. Descriptive characteristics are enumerated in Table 1. The group overall was characterized by severe airflow obstruction, hyperinflation, impaired DlCO, mild hypoxemia, impaired 6MWT distance, decreased maximal wattage, impaired health status, and severe emphysema, as measured by CT.
TABLE 1.
BASELINE CHARACTERISTICS FOR 609 PATIENTS WITH SEVERE EMPHYSEMA MANAGED MEDICALLY AS PART OF THE NATIONAL EMPHYSEMA TREATMENT TRIAL
| Parameter | Mean ± SD or % |
|---|---|
| Age, yr | 66.7 ± 5.9 |
| Male, % | 64.2 |
| BMI, kg/m2 | 24.7 ± 3.5 |
| SF-36 | |
| PCS | 29.6 ± 7.6 |
| MCS | 54.1 ± 9.3 |
| QWB | 0.56 ± 0.11 |
| SGRQ | 53.6 ± 12.7 |
| UCSD SOBQ | 63.4 ± 18.6 |
| Oxygen use (at rest, exercise, or sleeping), % | 81.3 |
| FEV1% predicted | 26.7 ± 7.0 |
| TLC % predicted | 128.5 ± 15.0 |
| RV % predicted | 223.4 ± 48.9 |
| IC/TLC | 0.22 ± 0.06 |
| DlCO % predicted | 28.4 ± 9.7 |
| PaO2, mm Hg | 64.2 ± 10.1 |
| PaCO2, mm Hg | 43.0 ± 5.8 |
| Hemoglobin, g/dl | 14.3 ± 1.3 |
| 6MWT distance, m | 371.7 ± 96.4 |
| Maximal CPET workload, W | 39.5 ± 22.2 |
| Percent emphysema in whole lung* | 15.9 ± 10.6 |
| Perfusion ratio | 0.28 ± 0.23 |
| Cigarette smoking, pack-years | 66.2 ± 32.9 |
| Duration since stopped smoking, yr | 8.8 ± 7.5 |
| Duration of cigarette smoking, yr | 41.0 ± 8.3 |
Definition of abbreviations: BMI = body mass index; CPET = cardiopulmonary exercise testing; DlCO = diffusing capacity of carbon monoxide; IC = inspiratory capacity; MCS = mental component scale; PCS = physical component scale; QWB = Quality of Well-Being scale; RV = residual volume; SF-36 = Medical Outcomes Study 36-item Short Form health survey; SGRQ = St. George's Respiratory Questionnaire; 6MWT = 6-min-walk test; TLC = total lung capacity; UCSD SOBQ = University of California, San Diego Shortness of Breath Questionnaire.
At the −950 Hounsfield unit cutoff.
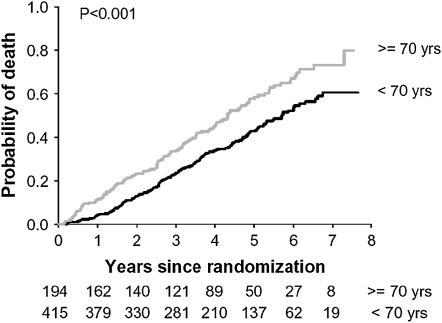
The median follow-up time as of September 2005 was 3.9 yr, with an observed mortality rate of 12.7 per 100 person-years. Figure 1 illustrates survival characteristics of the cohort segregated by age. Table 2 presents the results of univariate mortality analyses. Associated with reduced survival were: greater age, lower BMI, oxygen utilization, lower hemoglobin, lower Quality of Well-Being score, higher St. George's Respiratory Questionnaire score, higher UCSD SOBQ score, lower FEV1, higher residual volume (RV), lower inspiratory capacity/total lung capacity (TLC), lower DlCO % predicted, lower PaO2, higher PaCO2, lower 6MWT distance, lower maximal exercise capacity, more lower–lung zone emphysema, and a higher modified BODE index.
Figure 1.
Kaplan-Meier estimates of the probability of death as a function of number of years after randomization for medically treated patients segregated by age. The p value was derived from the log rank test for the comparison between subgroups over a median follow-up period of 3.9 yr.
TABLE 2.
UNIVARIATE MORTALITY MODEL IN 609 PATIENTS WITH SEVERE EMPHYSEMA
| Variable | n | Hazard Ratio (95% CI) | p Value |
|---|---|---|---|
| Demographic/Clinical | |||
| Age, yr | |||
| 70–83 | 194 | 1.56 (1.23–2.32) | < 0.0001 |
| 40–69 | 415 | Reference | |
| Sex | |||
| Male | 391 | 0.94 (0.63–1.19) | 0.60 |
| Female | 218 | Reference | |
| Race | |||
| Non-white | 35 | 1.06 (0.66–1.68) | 0.82 |
| White | 574 | Reference | |
| Annual income | |||
| < $15,000 | 112 | 1.04 (0.77–1.39) | 0.82 |
| ⩾ $15,000 | 496 | Reference | |
| BMI, kg/m2 | |||
| High (⩾ 28.1) | 123 | 0.77 (0.56–1.06) | 0.11 |
| Medium (reference) | 362 | Reference | |
| Low (⩽ 21.4) | 123 | 1.48 (1.13–1.95) | 0.005 |
| Oxygen use (rest, exercise, or sleeping) | |||
| Yes | 495 | 1.80 (1.30–2.49) | < 0.001 |
| No | 114 | Reference | |
| Hemoglobin, g/dl | |||
| 9.1–13.3 | 129 | 1.63 (1.26–2.12) | < 0.001 |
| 13.4–19.1 | 479 | Reference | |
| Health status | |||
| Quality of Well-Being (QWB) | |||
| 0.16–0.49 | 122 | 1.47 (1.13–1.93) | 0.005 |
| 0.50–0.89 | 487 | Reference | |
| SGRQ | |||
| 65.3–88.8 | 122 | 1.62 (1.24–2.10) | < 0.001 |
| 18.7–65.2 | 487 | Reference | |
| UCSD SOBQ | |||
| 79–109 | 131 | 1.89 (1.46–2.45) | < 0.001 |
| 9–78 | 478 | Reference | |
| Physiology | |||
| FEV1% predicted | |||
| 11–21 | 150 | 1.44 (1.11–1.85) | 0.005 |
| 22–54 | 459 | Reference | |
| TLC % predicted | |||
| 140–203 | 131 | 1.07 (0.81–1.41) | 0.65 |
| 95–139 | 478 | Reference | |
| Residual volume % predicted | |||
| 262–412 | 124 | 1.41 (1.07–1.85) | 0.01 |
| 97–261 | 485 | Reference | |
| IC/TLC | |||
| 0.04–0.17 | 122 | 1.80 (1.39–2.34) | < 0.001 |
| 0.18–0.45 | 487 | Reference | |
| DlCO, % predicted | |||
| 6–21 | 148 | 1.89 (1.48–2.41) | < 0.001 |
| 22–68 | 457 | Reference | |
| Pimax % predicted | |||
| 3–17 | 138 | 1.12 (0.86–1.47) | 0.39 |
| 18–57 | 462 | Reference | |
| Pemax % predicted | |||
| 4–14 | 140 | 1.02 (0.78–1.34) | 0.88 |
| 15–50 | 462 | Reference | |
| Arterial blood gas | |||
| PaO2, mm Hg | |||
| 36–55 | 133 | 1.65 (1.28–2.13) | < 0.001 |
| 56–95 | 475 | Reference | |
| PaCO2, mm Hg | |||
| 47–66 | 131 | 1.35 (1.04–1.77) | 0.03 |
| 29–46 | 477 | Reference | |
| Exercise testing | |||
| Maximal 6MWT distance, m | |||
| 144–288 | 123 | 2.02 (1.56–2.61) | < 0.001 |
| 289–652 | 486 | Reference | |
| Maximal CPET workload, W | |||
| Low* | 271 | 2.20 (1.74–2.78) | < 0.001 |
| High* | 338 | Reference | |
| Computed tomography | |||
| Percent emphysema in whole lung† | |||
| 25.7–48.5 | 111 | 1.14 (0.85–1.52) | 0.38 |
| 0.4–25.6 | 441 | Reference | |
| Missing | 57 | 0.96 (0.65–1.41) | 0.82 |
| Difference in % emphysema (upper lung:lower lung)† | |||
| −40.4 to −0.9 | 111 | 1.39 (1.04–1.85) | 0.02 |
| −0.8 to 63.6 | 441 | Reference | |
| Missing | 57 | 0.99 (0.68–1.46) | 0.98 |
| Alpha for whole lung† | |||
| 0.4–0.9 | 111 | 0.99 (0.73–1.34) | 0.94 |
| 1.0–1.8 | 441 | Reference | |
| Missing | 57 | 0.93 (0.63–1.36) | 0.71 |
| Difference in alpha (upper lung–lower lung)† | |||
| 0.4 to 1.6 | 111 | 1.22 (0.91–1.64) | 0.18 |
| −1.6 to 0.3 | 441 | Reference | |
| Missing | 57 | 0.97 (0.66–1.42) | 0.87 |
| Distribution of emphysema (radiologist) | |||
| Homogeneous | 274 | 1.14 (0.90–1.43) | 0.28 |
| Heterogeneous | 335 | Reference | |
| Nuclear perfusion scan | |||
| Perfusion ratio (upper lung:lower lung) | |||
| 0.04–0.14 | 136 | 1.28 (0.98–1. 68) | 0.07 |
| 0.15–3.13 | 472 | Reference | |
| Modified BODE index | |||
| 7–10 | 139 | 2.38 (1.86–3.04) | < 0.001 |
| 1–6 | 469 | Reference | |
| Cigarette smoking, pack-years | |||
| 90–280 | 126 | 1.15 (0.87–1. 51) | 0.34 |
| 0.15–3.13 | 481 | Reference | |
| Nuclear perfusion scan | |||
| Duration since stopped smoking, yr | |||
| ⩽ 2 | 127 | 1.14 (0.86–1. 51) | 0.36 |
| 3–42 | 480 | Reference |
Definition of abbreviations: BMI = body mass index; CI = confidence interval; CPET = cardiopulmonary exercise testing; DlCO = diffusing capacity for carbon monoxide; IC/TLC = ratio of inspiratory capacity to total lung capacity; Pemax = maximum expiratory pressure; Pimax = maximum inspiratory pressure; QWB = Quality of Well-Being scale; 6MWT = 6-min-walk test; SGRQ = St. George's Respiratory Questionnaire; UCSD SOBQ = University of California, San Diego Shortness of Breath Questionnaire.
Low exercise is defined as a maximal workload at or below the sex-specific 40th percentile (25 W for females and 40 W for males); high exercise is defined as a workload above this threshold.
At the −950 Hounsfield unit cutoff.
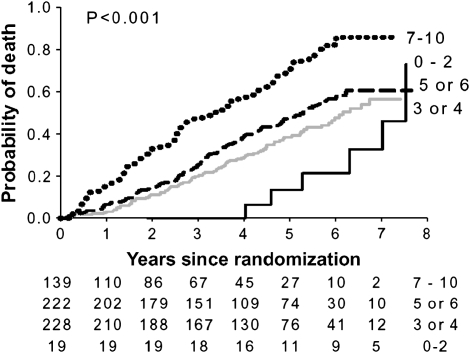
The variables in Table 2 were used to develop two multivariate models of mortality. Table 3 displays variables that remained predictive of mortality at the p ⩽ 0.05 level in either model after adjusting for all of the other variables included in the model; the adjusted hazard ratios are also shown. The variables that remained predictive in the multivariate model that included all variables but the modified BODE index were age, oxygen utilization, TLC, RV, maximal wattage during cardiopulmonary exercise testing, the difference between the upper and lower lungs in percent emphysema, and the perfusion ratio of upper to lower lung zones. The predictors of mortality with the largest hazard ratios were the difference in percent emphysema between the upper and lower lung zones and age. The second model, in which the BODE index replaced BMI, FEV1, 6MWT distance, and UCSD SOBQ score, gave similar, but not identical, results as the first model. In the second model, oxygen use and TLC were not as strong, whereas hemoglobin and DlCO were weakly predictive, A BODE score of at least 7 was predictive, with a hazard ratio of 1.48 (95% confidence interval = 1.07–2.05; p = 0.02). Figure 2 demonstrates mortality by modified BODE index. Similar results were obtained when the six patients with α1-antitrypsin deficiency were excluded from analysis.
TABLE 3.
SIGNIFICANT PREDICTORS IN MULTIVARIATE MORTALITY MODELS IN 609 PATIENTS WITH SEVERE EMPHYSEMA*
| Model 1‡
|
|
Model 2‡
|
|
|
|---|---|---|---|---|
| Predictor | Hazard Ratio (95% CI) | p Value | Hazard Ratio (95% CI) | p Value§ |
| Age, yr | ||||
| 70–83 | 1.64 (1.23–2.18) | 0.001 | 1.72 (1.31–2.26) | < 0.001 |
| 40–69 | Reference | Reference | ||
| BMI, kg/m2 | ||||
| High (> 28.1) | 0.86 (0.62–1.21) | 0.40 | NA | |
| Medium | Reference | BODE component | ||
| Low (< 21.4) | 1.32 (0.98–1.78) | 0.06 | ||
| Oxygen use (rest, exercise, or sleeping) | ||||
| Yes | 1.46 (1.02–2.10) | 0.04 | 1.40 (0.98–2.01) | 0.07 |
| No | Reference | Reference | ||
| Hemoglobin, g/dl | ||||
| 9.1–13.3 | 1.34 (0.97–1.85) | 0.08 | 1.38 (1.00–1.89) | 0.05 |
| 13.4–19.1 | Reference | Reference | ||
| UCSD SOBQ score | ||||
| 79–109 | 1.39 (0.98–1.97) | 0.06 | NA | |
| 9–78 | Reference | BODE component | ||
| TLC % predicted | ||||
| 140–203 | 0.68 (0.46–1.00) | 0.05 | 0.69 (0.47–1.01) | 0.06 |
| 95–139 | Reference | Reference | ||
| RV % predicted | ||||
| 262–412 | 1.57 (1.03–2.39) | 0.04 | 1.56 (1.04–2.37) | 0.03 |
| 97–261 | Reference | Reference | ||
| DlCO | ||||
| 6–21 | 1.34 (0.99–1.82) | 0.06 | 1.36 (1.01–1.84) | 0.04 |
| 22–68 | Reference | Reference | ||
| Maximal CPET workload, W | ||||
| Low† | 1.54 (1.17–2.03) | 0.002 | 1.48 (1.12–1.94) | 0.006 |
| High† | Reference | Reference | ||
| Difference in % emphysema (upper lung:lower lung) | ||||
| −40.4 to −0.8 | 1.74 (1.19–2.57) | 0.005 | 1.80 (1.22–2.66) | 0.003 |
| −0.7 to 63.6 | Reference | Reference | ||
| Missing | 0.84 (0.55–1.28) | 0.41 | 0.86 (0.57–1.31) | 0.49 |
| Perfusion ratio | ||||
| 0.04–0.14 | 1.57 (1.13–2.17) | 0.007 | 1.53 (1.11–2.12) | 0.01 |
| 0.15–3.13 | Reference | Reference | ||
| Modified BODE index‡ | ||||
| 7–10 | NA‡§ | NA | 1.48 (1.07–2.05) | 0.02 |
| 1–6 | Reference |
Definition of abbreviations: BMI = body mass index; CI = confidence interval; CPET = cardiopulmonary exercise testing; DLCO = diffusing capacity of carbon dioxide; IC/TLC = ratio of inspiratory capacity to total lung capacity; NA = not applicable; RV = residual volume; TLC = total lung capacity; UCSD SOBQ = University of California, San Diego, Shortness of Breath Questionnaire.
All variables listed in Table 2 were included in each model except as noted in the table; results are shown for those variables that were significant predictors at the p ⩽ 0.05 level in either model.
Low exercise is defined as a maximal workload at or below the sex-specific 40th percentile (25 W for females and 40 W for males); high exercise is defined as a workload above this threshold.
Includes all variables in Table 2 except components of modified BODE index: BMI, FEV1, UCSD SOBQ score, and 6MWT distance. The Model 2 was the same as the Model 1, except that the modified BODE index replaced BMI, FEV1, dyspnea, and 6MWT distance.
p Value for the four components for the modified BODE index = 0.12.
Figure 2.
Kaplan-Meier estimates of the probability of death as a function of number of years after randomization for medically treated patients segregated by modified BODE index. The p value was derived from the log rank test for the comparison between subgroups over a median follow-up period of 3.9 yr.
DISCUSSION
In this study of patients with severe emphysema randomized to the medical arm of the NETT, we document that increased mortality was independently associated with the following: (1) greater age, (2) use of oxygen supplementation, (3) lower hemoglobin, (4) higher RV (as % predicted), (5) lower DlCO % predicted, (7) lesser maximal exercise performance on cardiopulmonary exercise testing, (8) a higher modified BODE, and (9) greater lower–lung zone emphysema.
In this well-characterized cohort of patients with severe emphysema, multivariate analyses indicated increasing age to be associated with increased mortality. These data support the findings of others, who have suggested that increased age is associated with worsened survival (31, 32). Interestingly, no difference in mortality was noted between males and females with severe emphysema in univariate or multivariate analyses. Our data are in contrast with reports that female patients with COPD have a better prognosis compared with males (16, 33). Importantly, we confirm a weak, independent, predictive ability of a lower BMI, a marker for the systemic manifestations of COPD (34), for increased mortality. This supports the findings of other investigators who have noted a similar predictive ability of low BMI in COPD (4, 17–19). We extend these findings by confirming this relationship, even after adjusting for the extent of emphysema using state of the art chest computed tomographic quantification of emphysema percent. As there was an upper limit for BMI in the NETT, we cannot address whether a high BMI is associated with mortality. The importance of systemic disease is also supported by the greater mortality associated with decreased hemoglobin. Anemia has been reported to be present in patients with severe COPD (35). We demonstrate that decreased hemoglobin is independently associated with greater mortality.
Our results demonstrate the strengths and limitations of physiologic testing in predicting survival in patients with COPD. Although many investigators have suggested that FEV1 is inversely associated with mortality (2, 3, 23, 31, 36, 37), it was not predictive in our cohort using multivariate analysis. Similarly, in contrast to others who have described a decreased DlCO as strongly predictive of mortality (6–8, 36), we found that lower DlCO was strongly predictive in univariate models, but its impact weakened in multivariate modeling. Both of these discrepancies may reflect the relatively severe reduction and narrow range of FEV1 and DlCO in our patients. We confirm the importance of hyperinflation by demonstrating increased mortality with a higher RV, and a trend toward lower inspiratory capacity/TLC. On the other hand, in the multivariate model, after including RV in the model, TLC in fact is inversely associated with mortality, most likely reflecting the relative impact of chest wall compliance on vital capacity, and hence ventilatory reserve. Lower PaO2 was associated with decreased survival, although only in univariate modeling. Using multivariate modeling, this parameter had no independent influence on mortality, in contrast to the findings of others (2, 9). Intriguingly, the use of oxygen therapy was associated with impaired survival in our cohort. Whether oxygen prescription is an epimarker of more severe impairment, or truly had a negative effect on patient outcome (38), is impossible to discern from our data.
Our univariate analysis data suggest that distance walked and maximal exercise capacity are important predictors of mortality. Importantly, in multivariate analyses, 6MWT distance was no longer predictive, although maximal wattage remained a strong predictor. Although others have associated impaired exercise capacity with decreased survival (4, 11–13, 15), our data extend these findings by incorporating both 6MWT distance and maximal exercise wattage in the analyses. Our study is strengthened by the use of sex thresholds that have been demonstrated to result in differing mortality effects of lung volume reduction surgery (25). A higher dyspnea score, quantified using the UCSD SOBQ, was strongly predictive of decreased survival only in univariate analysis. This finding contrasts with that of other studies suggesting the independent value of dyspnea quantification using other symptom-specific instruments (4, 20). Similarly, we found predictive value to health status measurements only during univariate analyses. This also contrasts with the findings of other investigators (13, 21, 39), and may reflect the relatively narrow range of dyspnea and health status measurements in a more severely diseased population.
One group has recently demonstrated that a multifunctional index, incorporating BMI, FEV1, 6MWT distance, dyspnea measurement, and the BODE index, performs better than the individual measurements in a large cohort of patients with COPD (4). Although we did not utilize the Medical Research Council dyspnea instrument, we were able to construct a modified BODE index by using the UCSD SOBQ. In our cohort, this instrument proved an independent predictor of mortality, although in multivariate analyses its predictive value was less notable than previously reported. This may represent differing operating characteristics of the dyspnea parameter in the modified BODE index, although the hazard ratio was quantitatively similar to that previously reported (4). More likely, this reflects the predominantly emphysematous population of our patients, or the greater predictive value of maximal achieved wattage during oxygen-supplemented exercise testing. Our data may have important clinical implications, as they suggest that a modified BODE index should be interpreted carefully in clinical situations that are critically dependent on accurate prognostication in patients with COPD, such as the timing of listing for lung transplantation. Additional data in this patient population are desperately required.
Surprisingly, in our patients, the overall percentage of emphysema was not associated with increased mortality in univariate or multivariate analyses. As such, our data suggest that the overall percentage of emphysema does not independently influence survival in a large cohort of patients with severe emphysema. This contrasts with a recent study showing that the percentage of emphysema is predictive of survival in α1-antitrypsin–induced emphysema (40). The differences between those results and the findings of our study may reflect different patient population (patients with α1-antitrypsin deficiency were a minority of our cohort), age, and disease severity. In addition, enrollment in the NETT required that patients have bilateral emphysema (identified by chest CT imaging) that was at least moderately severe, but neither too severe nor too homogeneous. Therefore, narrow clustering of emphysema severity in our dataset probably limits this variable's independent predictive value for mortality in our study. Nevertheless, the distribution of emphysema in our cohort was predictive of mortality, with improved survival in patients with greater emphysema in the upper compared with the lower lung zones. Because typical, centrilobular emphysema generally is most prominent in the upper lung zones early in disease, and becomes more diffuse as severity progresses (41), apical predominance may be a marker of reduced disease severity. Alternatively, lower-lobe emphysema may represent a phenotypic or pathobiologic variant of emphysema.
The major limitation of this study comes from its sample population. As all subjects were part of the NETT, the patient population exhibited emphysema and severe chronic airflow obstruction. In addition, selection bias was imposed by requirements for sustained smoking cessation and absence of significant comorbidities that precluded surgical therapy. As a result, the findings may not be applicable to all patients with COPD. On the other hand, the survival characteristics of our cohort are similar to those of other published series (42), including the more severe subgroups of the intermittent positive-pressure breathing trial (3) and other more recent series (4).
In summary, we show that mortality in patients with COPD with moderate to severe emphysema, as defined by high-resolution CT scan, plus severe, chronic airflow obstruction, is influenced by numerous clinical and physiologic factors. We note increased mortality in patients with greater age, lower BMI, oxygen utilization (in contrast to PaO2), and greater hyperinflation. Exercise capacity, as quantified by cardiopulmonary exercise testing in contrast to 6MWT distance, proves a powerful independent predictor of survival. By contrast, a multidimensional index, the modified BODE index, proved a weak independent predictor in patients with severe emphysema. These data suggest that readily available clinical parameters may be useful in predicting outcome in severe emphysema.
NETT CREDIT ROSTER
Members of the NETT Research Group
Office of the Chair of the Steering Committee, University of Pennsylvania, Philadelphia, Pennsylvania: Alfred P. Fishman, M.D. (Chair); Betsy Ann Bozzarello; Ameena Al-Amin.
Clinical Centers.
Baylor College of Medicine, Houston, Texas: Marcia Katz, M.D. (Principal Investigator); Carolyn Wheeler, R.N., B.S.N. (Principal Clinic Coordinator); Elaine Baker, R.R.T., R.P.F.T.; Peter Barnard, Ph.D., R.P.F.T.; Phil Cagle, M.D.; James Carter, M.D.; Sophia Chatziioannou, M.D.; Karla Conejo-Gonzales; Kimberly Dubose, R.R.T.; John Haddad, M.D.; David Hicks, R.R.T., R.P.F.T.; Neal Kleiman, M.D.; Mary Milburn-Barnes, C.R.T.T.; Chinh Nguyen, R.P.F.T.; Michael Reardon, M.D.; Joseph Reeves-Viets, M.D.; Steven Sax, M.D.; Amir Sharafkhaneh, M.D.; Owen Wilson, Ph.D.; Christine Young, P.T.; Rafael Espada, M.D. (Principal Investigator 1996–2002); Rose Butanda (1999–2001); Minnie Ellisor (2002); Pamela Fox, M.D. (1999–2001); Katherine Hale, M.D. (1998–2000); Everett Hood, R.P.F.T. (1998–2000); Amy Jahn (1998–2000); Satish Jhingran, M.D. (1998–2001); Karen King, R.P.F.T. (1998–1999); Charles Miller III, Ph.D. (1996–1999); Imran Nizami, M.D. (Co–Principal Investigator, 2000–2001); Todd Officer (1998–2000); Jeannie Ricketts (1998–2000); Joe Rodarte, M.D. (Co–Principal Investigator 1996–2000); Robert Teague, M.D. (Co–Principal Investigator 1999–2000); Kedren Williams (1998–1999).
Brigham and Women's Hospital, Boston, Massachusetts: John Reilly, M.D. (Principal Investigator); David Sugarbaker, M.D. (Co–Principal Investigator); Carol Fanning, R.R.T. (Principal Clinic Coordinator); Simon Body, M.D.; Sabine Duffy, M.D.; Vladmir Formanek, M.D.; Anne Fuhlbrigge, M.D.; Philip Hartigan, M.D.; Sarah Hooper, E.P.; Andetta Hunsaker, M.D.; Francine Jacobson, M.D.; Marilyn Moy, M.D.; Susan Peterson, R.R.T.; Roger Russell, M.D.; Diane Saunders; Scott Swanson, M.D. (Co–Principal Investigator, 1996–2001).
Cedars-Sinai Medical Center, Los Angeles, California: Rob McKenna, M.D. (Principal Investigator); Zab Mohsenifar, M.D. (Co–Principal Investigator); Carol Geaga, R.N. (Principal Clinic Coordinator); Manmohan Biring, M.D.; Susan Clark, R.N., M.N.; Jennifer Cutler, M.D.; Robert Frantz, M.D.; Peter Julien, M.D.; Michael Lewis, M.D.; Jennifer Minkoff-Rau, M.S.W.; Valentina Yegyan, B.S., C.P.F.T.; Milton Joyner, B.A. (1996–2002).
Cleveland Clinic Foundation, Cleveland, Ohio: Malcolm DeCamp, M.D. (Principal Investigator); James Stoller, M.D. (Co–Principal Investigator); Yvonne Meli, R.N.-C. (Principal Clinic Coordinator); John Apostolakis, M.D.; Darryl Atwell, M.D.; Jeffrey Chapman, M.D.; Pierre DeVilliers, M.D.; Raed Dweik, M.D.; Erik Kraenzler, M.D.; Rosemary Lann, L.I.S.W.; Nancy Kurokawa, R.R.T., C.P.F.T; Scott Marlow, R.R.T.; Kevin McCarthy, RCPT; Pricilla McCreight, R.R.T., C.P.F.T; Atul Mehta, M.D.; Moulay Meziane, M.D.; Omar Minai, M.D.; Mindi Steiger, R.R.T.; Kenneth White, R.P.F.T.; Janet Maurer, M.D. (Principal Investigator, 1996–2001); Terri Durr, R.N. (2000–2001); Charles Hearn, D.O. (1998–2001); Susan Lubell, P.A.-C. (1999–2000); Peter O'Donovan, M.D. (1998–2003); Robert Schilz, D.O. (1998–2002).
Columbia University, New York, New York, in consortium with Long Island Jewish Medical Center, New Hyde Park, New York: Mark Ginsburg, M.D. (Principal Investigator); Byron Thomashow, M.D. (Co–Principal Investigator); Patricia Jellen, M.S.N, R.N. (Principal Clinic Coordinator); John Austin, M.D.; Matthew Bartels, M.D.; Yahya Berkmen, M.D.; Patricia Berkoski, M.S., R.R.T. (Site Coordinator, Long Island Jewish Medical Center); Frances Brogan, M.S.N, R.N.; Amy Chong, B.S., C.R.T.; Glenda DeMercado, B.S.N; Angela DiMango, M.D.; Sandy Do, M.S., P.T.; Bessie Kachulis, M.D.; Arfa Khan, M.D.; Berend Mets, M.D.; Mitchell O'Shea, B.S., R.T., C.P.F.T; Gregory Pearson, M.D.; Leonard Rossoff, M.D.; Steven Scharf, M.D., Ph.D. (Co–Principal Investigator, 1998–2002); Maria Shiau, M.D.; Paul Simonelli, M.D.; Kim Stavrolakes, M.S., P.T.; Donna Tsang, B.S.; Denise Vilotijevic, M.S., P.T.; Chun Yip, M.D.; Mike Mantinaos, M.D. (1998–2001); Kerri McKeon, B.S., R.R.T., R.N. (1998–1999); Jacqueline Pfeffer, MPH, P.T. (1997–2002).
Duke University Medical Center, Durham, North Carolina: Neil MacIntyre, M.D. (Principal Investigator); R. Duane Davis, M.D. (Co–Principal Investigator); John Howe, R.N. (Principal Clinic Coordinator); R. Edward Coleman, M.D.; Rebecca Crouch, R.P.T.; Dora Greene; Katherine Grichnik, M.D.; David Harpole, Jr., M.D.; Abby Krichman, R.R.T.; Brian Lawlor, R.R.T.; Holman McAdams, M.D.; John Plankeel, M.D.; Susan Rinaldo-Gallo, M.ED.; Sheila Shearer, R.R.T.; Jeanne Smith, A.C.S.W.; Mark Stafford-Smith, M.D.; Victor Tapson, M.D.; Mark Steele, M.D. (1998–1999); Jennifer Norten, M.D. (1998–1999).
Mayo Foundation, Rochester, Minnesota: James Utz, M.D. (Principal Investigator); Claude Deschamps, M.D. (Co–Principal Investigator); Kathy Mieras, C.C.R.P. (Principal Clinic Coordinator); Martin Abel, M.D.; Mark Allen, M.D.; Deb Andrist, R.N.; Gregory Aughenbaugh, M.D.; Sharon Bendel, R.N.; Eric Edell, M.D.; Marlene Edgar; Bonnie Edwards; Beth Elliot, M.D.; James Garrett, R.R.T.; Delmar Gillespie, M.D.; Judd Gurney, M.D.; Boleyn Hammel; Karen Hanson, R.R.T.; Lori Hanson, R.R.T.; Gordon Harms, M.D.; June Hart; Thomas Hartman, M.D.; Robert Hyatt, M.D.; Eric Jensen, M.D.; Nicole Jenson, R.R.T.; Sanjay Kalra, M.D.; Philip Karsell, M.D.; Jennifer Lamb; David Midthun, M.D.; Carl Mottram, R.R.T.; Stephen Swensen, M.D.; Anne-Marie Sykes, M.D.; Karen Taylor; Norman Torres, M.D.; Rolf Hubmayr, M.D. (1998–2000); Daniel Miller, M.D. (1999–2002); Sara Bartling, R.N. (1998–2000); Kris Bradt (1998–2002).
National Jewish Medical and Research Center, Denver, Colorado: Barry Make, M.D. (Principal Investigator); Marvin Pomerantz, M.D. (Co–Principal Investigator); Mary Gilmartin, R.N., R.R.T. (Principal Clinic Coordinator); Joyce Canterbury; Martin Carlos; Phyllis Dibbern, P.T.; Enrique Fernandez, M.D.; Lisa Geyman, M.S.P.T.; Connie Hudson; David Lynch, M.D.; John Newell, M.D.; Robert Quaife, M.D.; Jennifer Propst, R.N.; Cynthia Raymond, M.S.; Jane Whalen-Price, P.T.; Kathy Winner, OTR; Martin Zamora, M.D.; Reuben Cherniack, M.D. (Principal Investigator, 1997–2000).
Ohio State University, Columbus, Ohio: Philip Diaz, M.D. (Principal Investigator); Patrick Ross, M.D. (Co–Principal Investigator); Tina Bees (Principal Clinic Coordinator); Jan Drake; Charles Emery, Ph.D.; Mark Gerhardt, M.D., Ph.D.; Mark King, M.D.; David Rittinger; Mahasti Rittinger.
St. Louis University, St. Louis, Missouri: Keith Naunheim, M.D. (Principal Investigator); Robert Gerber, M.D. (Co–Principal Investigator); Joan Osterloh, R.N., M.S.N (Principal Clinic Coordinator); Susan Borosh; Willard Chamberlain, D.O.; Sally Frese; Alan Hibbit; Mary Ellen Kleinhenz, M.D.; Gregg Ruppel; Cary Stolar, M.D.; Janice Willey; Francisco Alvarez, M.D. (Co–Principal Investigator, 1999–2002); Cesar Keller, M.D. (Co–Principal Investigator, 1996–2000).
Temple University, Philadelphia, Pennsylvania: Gerard Criner, M.D. (Principal Investigator); Satoshi Furukawa, M.D. (Co–Principal Investigator); Anne Marie Kuzma, R.N., M.S.N (Principal Clinic Coordinator); Roger Barnette, M.D.; Neil Brister, M.D.; Kevin Carney, R.N., C.C.T.C.; Wissam Chatila, M.D.; Francis Cordova, M.D.; Gilbert D'Alonzo, D.O.; Michael Keresztury, M.D.; Karen Kirsch; Chul Kwak, M.D.; Kathy Lautensack, R.N., B.S.N; Madelina Lorenzon, C.P.F.T; Ubaldo Martin, M.D.; Peter Rising, M.S.; Scott Schartel, M.D.; John Travaline, M.D.; Gwendolyn Vance, R.N., CCTC; Phillip Boiselle, M.D. (1997–2000); Gerald O'Brien, M.D. (1997–2000).
University of California, San Diego, San Diego, California: Andrew Ries, M.D., M.P.H. (Principal Investigator); Robert Kaplan, Ph.D. (Co–Principal Investigator); Catherine Ramirez, B.S., R.C.P. (Principal Clinic Coordinator); David Frankville, M.D.; Paul Friedman, M.D.; James Harrell, M.D.; Jeffery Johnson; David Kapelanski, M.D.; David Kupferberg, M.D., M.P.H.; Catherine Larsen, M.P.H.; Trina Limberg, R.R.T.; Michael Magliocca, R.N., C.N.P.; Frank J. Papatheofanis, M.D., Ph.D.; Dawn Sassi-Dambron, R.N.; Melissa Weeks.
University of Maryland at Baltimore, Baltimore, Maryland, in consortium with Johns Hopkins Hospital, Baltimore, Maryland: Mark Krasna, M.D. (Principal Investigator); Henry Fessler, M.D. (Co–Principal Investigator); Iris Moskowitz (Principal Clinic Coordinator); Timothy Gilbert, M.D.; Jonathan Orens, M.D.; Steven Scharf, M.D., Ph.D.; David Shade; Stanley Siegelman, M.D.; Kenneth Silver, M.D.; Clarence Weir; Charles White, M.D.
University of Michigan, Ann Arbor, Michigan: Fernando Martinez, M.D. (Principal Investigator); Mark Iannettoni, M.D. (Co–Principal Investigator); Catherine Meldrum, B.S.N, R.N., C.C.R.N. (Principal Clinic Coordinator); William Bria, M.D.; Kelly Campbell; Paul Christensen, M.D.; Kevin Flaherty, M.D.; Steven Gay, M.D.; Paramjit Gill, R.N.; Paul Kazanjian, M.D.; Ella Kazerooni, M.D.; Vivian Knieper; Tammy Ojo, M.D.; Lewis Poole; Leslie Quint, M.D.; Paul Rysso; Thomas Sisson, M.D.; Mercedes True; Brian Woodcock, M.D.; Lori Zaremba, R.N.
University of Pennsylvania, Philadelphia, Pennsylvania: Larry Kaiser, M.D. (Principal Investigator); John Hansen-Flaschen, M.D. (Co–Principal Investigator); Mary Louise Dempsey, B.S.N, R.N. (Principal Clinic Coordinator); Abass Alavi, M.D.; Theresa Alcorn; Selim Arcasoy, M.D.; Judith Aronchick, M.D.; Stanley Aukberg, M.D.; Bryan Benedict, R.R.T.; Susan Craemer, B.S., R.R.T., C.P.F.T; Ron Daniele, M.D.; Jeffrey Edelman, M.D.; Warren Gefter, M.D.; Laura Kotler-Klein, M.S.S; Robert Kotloff, M.D.; David Lipson, M.D.; Wallace Miller, Jr., M.D.; Richard O'Connell, R.P.F.T.; Staci Opelman, M.S.W; Harold Palevsky, M.D.; William Russell, R.P.F.T.; Heather Sheaffer, M.S.W; Rodney Simcox, B.S.R.T., R.R.T.; Susanne Snedeker, R.R.T., C.P.F.T; Jennifer Stone-Wynne, M.S.W.; Gregory Tino, M.D.; Peter Wahl; James Walter, R.P.F.T.; Patricia Ward; David Zisman, M.D.; James Mendez, M.S.N, C.R.N.P (1997–2001); Angela Wurster, M.S.N, C.R.N.P (1997–1999).
University of Pittsburgh, Pittsburgh, Pennsylvania: Frank Sciurba, M.D. (Principal Investigator); James Luketich, M.D. (Co–Principal Investigator); Colleen Witt, M.S. (Principal Clinic Coordinator); Gerald Ayres; Michael Donahoe, M.D.; Carl Fuhrman, M.D.; Robert Hoffman, M.D.; Joan Lacomis, M.D.; Joan Sexton; William Slivka; Diane Strollo, M.D.; Erin Sullivan, M.D.; Tomeka Simon; Catherine Wrona, R.N., B.S.N; Gerene Bauldoff, R.N., M.S.N. (1997–2000); Manuel Brown, M.D. (1997–2002); Elisabeth George, R.N., M.S.N. (Principal Clinic Coordinator 1997–2001); Robert Keenan, M.D. (Co–Principal Investigator 1997–2000); Theodore Kopp, M.S. (1997–1999); Laurie Silfies (1997–2001).
University of Washington, Seattle, Washington: Joshua Benditt, M.D. (Principal Investigator), Douglas Wood, M.D. (Co–Principal Investigator); Margaret Snyder, M.N. (Principal Clinic Coordinator); Kymberley Anable; Nancy Battaglia; Louie Boitano; Andrew Bowdle, M.D.; Leighton Chan, M.D.; Cindy Chwalik; Bruce Culver, M.D.; Thurman Gillespy, M.D.; David Godwin, M.D.; Jeanne Hoffman; Andra Ibrahim, M.D.; Diane Lockhart; Stephen Marglin, M.D.; Kenneth Martay, M.D.; Patricia McDowell; Donald Oxorn, M.D.; Liz Roessler; Michelle Toshima; Susan Golden (1998–2000).
Other participants.
Agency for Healthcare Research and Quality, Rockville, Maryland: Lynn Bosco, M.D., M.P.H.; Yen-Pin Chiang, Ph.D.; Carolyn Clancy, M.D.; Harry Handelsman, D.O.
Centers for Medicare and Medicaid Services, Baltimore, Maryland: Steven M Berkowitz, Ph.D.; Tanisha Carino, Ph.D.; Joe Chin, M.D.; JoAnna Baldwin; Karen McVearry; Anthony Norris; Sarah Shirey; Claudette Sikora; Steven Sheingold, Ph.D. (1997–2004).
Coordinating Center, the Johns Hopkins University, Baltimore, Maryland: Steven Piantadosi, M.D., Ph.D. (Principal Investigator); James Tonascia, Ph.D. (Co–Principal Investigator); Patricia Belt; Amanda Blackford, Sc.M.; Karen Collins; Betty Collison; Ryan Colvin, M.P.H.; John Dodge; Michele Donithan, M.H.S.; Vera Edmonds; Gregory L. Foster, M.A.; Julie Fuller; Judith Harle; Rosetta Jackson; Shing Lee, Sc.M.; Charlene Levine; Hope Livingston; Jill Meinert; Jennifer Meyers; Deborah Nowakowski; Kapreena Owens; Shangqian Qi, M.D.; Michael Smith; Brett Simon, M.D.; Paul Smith; Alice Sternberg, Sc.M.; Mark Van Natta, M.H.S.; Laura Wilson, Sc.M.; Robert Wise, M.D.
Cost-Effectiveness Subcommittee: Robert M. Kaplan, Ph.D. (Chair); J. Sanford Schwartz, M.D. (Co-Chair); Yen-Pin Chiang, Ph.D.; Marianne C. Fahs, Ph.D.; A. Mark Fendrick, M.D.; Alan J. Moskowitz, M.D.; Dev Pathak, Ph.D.; Scott Ramsey, M.D., Ph.D.; Steven Sheingold, Ph.D.; A. Laurie Shroyer, Ph.D.; Judith Wagner, Ph.D.; Roger Yusen, M.D.
Cost-Effectiveness Data Center, Fred Hutchinson Cancer Research Center, Seattle, Washington: Scott Ramsey, M.D., Ph.D. (Principal Investigator); Ruth Etzioni, Ph.D.; Sean Sullivan, Ph.D.; Douglas Wood, M.D.; Thomas Schroeder, M.A.; Karma Kreizenbeck; Kristin Berry, M.S.; Nadia Howlader, M.S.
CT Scan Image Storage and Analysis Center, University of Iowa, Iowa City, Iowa: Eric Hoffman, Ph.D. (Principal Investigator); Janice Cook-Granroth, B.S.; Angela Delsing, R.T.; Junfeng Guo, Ph.D.; Geoffrey McLennan, M.D.; Brian Mullan, M.D.; Chris Piker, B.S.; Joseph Reinhardt, Ph.D.; Blake Robinswood; Jered Sieren, R.T.R; William Stanford, M.D.
Data and Safety Monitoring Board: John A. Waldhausen, M.D. (Chair); Gordon Bernard, M.D.; David DeMets, Ph.D.; Mark Ferguson, M.D.; Eddie Hoover, M.D.; Robert Levine, M.D.; Donald Mahler, M.D.; A. John McSweeny, Ph.D.; Jeanine Wiener-Kronish, M.D.; O. Dale Williams, Ph.D.; Magdy Younes, M.D.
Marketing Center, Temple University, Philadelphia, Pennsylvania: Gerard Criner, M.D. (Principal Investigator); Charles Soltoff, M.B.A.
Project Office, National Heart, Lung, and Blood Institute, Bethesda, Maryland: Gail Weinmann, M.D. (Project Officer); Joanne Deshler (Contracting Officer); Dean Follmann, Ph.D.; James Kiley, Ph.D.; Margaret Wu, Ph.D. (1996–2001).
Supplementary Material
Acknowledgments
The authors thank Arthur Gelb, M.D., Lakewood Regional Medical Center, Lakewood, California.
Supported by contracts with the National Heart, Lung, and Blood Institute (N01HR76101, N01HR76102, N01HR76103, N01HR76104, N01HR76105, N01HR76106, N01HR76107, N01HR76108, N01HR76109, N01HR76110, N01HR76111, N01HR76112, N01HR76113, N01HR76114, N01HR76115, N01HR76116, N01HR76118, and N01HR76119), the Centers for Medicare and Medicaid Services, and the Agency for Healthcare Research and Quality.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200510-1677OC on March 16, 2006
Conflict of Interest Statement: F.J.M. has received less than $10,000 from Intermune, and has had no consulting or speaker bureau activities with Intermune during the present calendar year. He was previously a co-investigator in the GIPF-007 study. He has been a site principal investigator at the University of Michigan for the BUILD 1 study sponsored by Actelion, and his total personal compensation was less than $10,000. He has, in the past, been a member of the Encysive steering committee for a selective endothelin antagonist and of the Co-Therix steering committee for an inhaled vasodilator. He has been a member of several Pfizer advisory boards, CME committees, and the Speaker's Bureau for Pfizer, relating exclusively to COPD, with total compensation greater than $10,000, but less than $20,000. He has been a member of several Boehringer advisory boards, CME committees, and the Speaker's Bureau for Boehringer Ingelheim, relating exclusively to COPD, with total compensation greater than $10,000, but less than $20,0000. G.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. J.L.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. G.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. G.W. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. A.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.M.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. J.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. F.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. B.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. Z.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. P.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. E.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. R.W. received consulting fees from GlaxoSmithKline, Pfizer, Sanofi-Aventis, Emphasys, and Spiration in the past 3 yr for research oversight and review committees. He has served on advisory boards for Boehringer-Ingelheim, Pfizer, GlaxoSmithKline, Hill-Rom, Otsuka, Ortho, and Amgen. He has also received research grants from Boehringer-Ingleheim, Ostuka, and Pfizer. Conflicts of interest regarding human research are managed by the Johns Hopkins University.
References
- 1.Celli BR, MacNee W; ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2006;27:242. [DOI] [PubMed] [Google Scholar]
- 2.Hodgkin JE. Prognosis in chronic obstructive pulmonary disease. Clin Chest Med 1990;11:555–569. [PubMed] [Google Scholar]
- 3.Anthonisen NR. Prognosis in chronic obstructive pulmonary disease: results from multicenter clinical trials. Am Rev Respir Dis 1989;140:S95–S99. [DOI] [PubMed] [Google Scholar]
- 4.Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, Pinto-Plata V, Cabral HJ. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004;350:1005–1012. [DOI] [PubMed] [Google Scholar]
- 5.Casanova C, Code C, de Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V, Celli BR. Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2005;171:591–597. [DOI] [PubMed] [Google Scholar]
- 6.Bates DV, Knott JMS, Christie RV. Respiratory function in emphysema in relation to prognosis. Q J Med 1956;25:137–157. [PubMed] [Google Scholar]
- 7.Boushy SF, Thompson HK Jr, North LB, Beale AR, Snow TR. Prognosis in chronic obstructive pulmonary disease. Am Rev Respir Dis 1973;108:1373–1383. [DOI] [PubMed] [Google Scholar]
- 8.Kanner RE, Renzetti AD Jr, Stanish WM, Barkman HW Jr, Klauber MR. Predictors of survival in subjects with chronic airflow limitation. Am J Med 1983;74:249–255. [DOI] [PubMed] [Google Scholar]
- 9.Chailleux E, Fauroux B, Binet G, Dautzenberg B, Polu JM. Predictors of survival in patients receiving domiciliary oxygen therapy or mechanical ventilatory: a 10-year analysis of ANTADIR observatory. Chest 1996;109:741–749. [DOI] [PubMed] [Google Scholar]
- 10.Foucher P, Baudouin N, Merati M, Pitard A, Bonniaud P, Reybet-Degat O, Jeannin L. Relative survival analysis of 252 patients with COPD receiving long-term oxygen therapy. Chest 1998;113:1580–1587. [DOI] [PubMed] [Google Scholar]
- 11.Gerardi DA, Lovett L, Benoit-Connors ML, Reardon JZ, ZuWallack RL. Variables related to increased mortality following out-patient pulmonary rehabilitation. Eur Respir J 1996;9:431–435. [DOI] [PubMed] [Google Scholar]
- 12.Bowen JB, Votto JJ, Thrall RS, Campbell Haggerty M, Stockdale-Woodley R, Bandyopadhyay T, ZuWallack RL. Functional status and survival following pulmonary rehabilitation. Chest 2000;118:697–703. [DOI] [PubMed] [Google Scholar]
- 13.Oga T, Nishimura K, Tsukino M, Sato S, Hajiro T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am J Respir Crit Care Med 2003;167:544–549. [DOI] [PubMed] [Google Scholar]
- 14.Hiraga T, Maekura R, Okuda Y, Okamoto T, Hirotani A, Kitada S, Yoshimura K, Yokota S, Ito M, Ogura T. Prognostic predictors for survival in patients with COPD using cardiopulmonary exercise testing. Clin Physiol Funct Imaging 2003;23:324–331. [DOI] [PubMed] [Google Scholar]
- 15.Pinto-Plata VM, Cote C, Cabral H, Taylor J, Celli BR. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J 2004;23:28–33. [DOI] [PubMed] [Google Scholar]
- 16.Miyamoto K, Aida A, Nishimura M, Aiba M, Kira S, Kawakami Y, The Respiratory Failure Research Group in Japan. Gender effect on prognosis of patients receiving long-term home oxygen therapy. Am J Respir Crit Care Med 1995;152:972–976. [DOI] [PubMed] [Google Scholar]
- 17.Gray-Donald K, Gibbons L, Shapiro SH, MacKlem P.T., Martin JG. Nutritional status and mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1996;153:961–966. [DOI] [PubMed] [Google Scholar]
- 18.Schols AMWJ, Slangen J, Volovics L, Wouters EFM. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1791–1797. [DOI] [PubMed] [Google Scholar]
- 19.Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999;160:1856–1861. [DOI] [PubMed] [Google Scholar]
- 20.Nishimura K, Izumi T, Tsukino M, Oga T, on Behalf of the Kansai COPD Registry and Research Group in Japan. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 2002;121:1434–1440. [DOI] [PubMed] [Google Scholar]
- 21.Domingo-Salvany A, Lamarac R, Ferrer M, Garcia-Aymerich J, Alonso J, Felez M, Khalaf A, Marrades RM, Monso E, Serra-Battles J, et al. Health-related quality of life and mortality in male patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:680–685. [DOI] [PubMed] [Google Scholar]
- 22.Burrows B, Bloom JW, Traver GA, Cline MG. The course and prognosis of different forms of chronic airways obstruction in a sample from the general population. N Engl J Med 1987;317:1309–1314. [DOI] [PubMed] [Google Scholar]
- 23.Burrows B, Earle RH. Prediction of survival in patients with chronic airways obstruction. Am Rev Respir Dis 1969;99:865–871. [DOI] [PubMed] [Google Scholar]
- 24.National Emphysema Treatment Trial Research Group. Rationale and design of the National Emphysema Treatment Trial: a prospective randomized trial of lung volume reduction surgery. Chest 1999;116:1750–1761. [DOI] [PubMed] [Google Scholar]
- 25.National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059–2073. [DOI] [PubMed] [Google Scholar]
- 26.Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A self-complete measure of health status for chronic airflow limitation: the St. George's Respiratory Questionnaire. Am Rev Respir Dis 1992;145:1321–1327. [DOI] [PubMed] [Google Scholar]
- 27.Eakin EG, Resnikoff PM, Prewitt LM, Ries AL, Kaplan RM. Validation of a new dyspnea measure: the UCSD Shortness of Breath Questionnaire: University of California, San Diego. Chest 1998;113:619–624. [DOI] [PubMed] [Google Scholar]
- 28.Sciurba F, Criner GJ, Lee SM, Mohsenifar Z, Shade D, Slivka WA, Wise RA, for the National Emphysema Treatment Trial Research Group. Six-minute walk distance in chronic obstructive pulmonary disease: reproducibility and effect of walking course layout and length. Am J Respir Crit Care Med 2003;167:1522–1527. [DOI] [PubMed] [Google Scholar]
- 29.Hoffman EA, Reinhardt JM, Sonka M, Simon BA, Guo J, Saba O, Chon D, Samrah S, Shikata H, Tschirren J, et al. Characterization of the interstitial lung diseases via density-based and texture-based analysis of computed tomography images of lung structure and function. Acad Radiol 2003;10:1104–1118. [DOI] [PubMed] [Google Scholar]
- 30.Mishima M, Oku Y, Kawakami K, Sakai N, Fukui M, Hirai T, Chin K, Ohi M, Nishimura K, Itoh H, et al. Quantitative assessment of the spatial distribution of low attenuation areas on X-ray CT using texture analysis in patients with chronic pulmonary emphysema. Front Med Biol Eng 1997;8:19–34. [PubMed] [Google Scholar]
- 31.Piccioni P, Caria E, Bignamini E, Forconi G, Nebiolo F, Arossa W, Bugiani M. Predictors of survival in a group of patients with chronic airflow obstruction. J Clin Epidemiol 1998;51:547–555. [DOI] [PubMed] [Google Scholar]
- 32.Hansen EF, Pharaneth K, Laursen LC, Kok-Jensen A, Dirksen A. Reversible and irreversible airflow obstruction as predictor of overall mortality in asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999;159:1267–1271. [DOI] [PubMed] [Google Scholar]
- 33.Sunyer J, Anto JM, McFarlane D, Domingo A, Tobias A, Barcelo MA, Munoz A. Sex differences in mortality of people who visited emergency rooms for asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;158:851–856. [DOI] [PubMed] [Google Scholar]
- 34.Agusti AGN, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J 2003;21:347–360. [DOI] [PubMed] [Google Scholar]
- 35.John M, Hoernig S, Doehner W, Okonko DD, Witt C, Anker SD. Anemia and inflammation in COPD. Chest 2005;127:825–829. [DOI] [PubMed] [Google Scholar]
- 36.Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease: a 15-year follow-up study. Am Rev Respir Dis 1979;119:895–902. [DOI] [PubMed] [Google Scholar]
- 37.Anthonisen NR, Wright EC, Hodgkin JE, Group IPPB Trial. Prognosis in chronic obstructive pulmonary disease. Am Rev Respir Dis 1986;133:14–20. [DOI] [PubMed] [Google Scholar]
- 38.Carpagnano GE, Kharitonov SA, Foschino-Barbaro MP, Resta O, Gramiccioni E, Barnes PJ. Supplementary oxygen in healthy subjects and those with COPD increases oxidative stress and airway inflammation. Thorax 2004;59:1016–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sprenkle MD, Niewoehner DE, Nelson DB, Nichol KL. The Veterans Short Form 36 Questionnaire is predictive of mortality and health-care utilization in a population of veterans with a self-reported diagnosis of asthma or COPD. Chest 2004;126:81–89. [DOI] [PubMed] [Google Scholar]
- 40.Dawkins PA, Dowson LJ, Guest PJ, Stockley RA. Predictors of mortality in α1-antitrypsin deficiency. Thorax 2003;58:1020–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Goldin JG. Quantitative CT of emphysema and the airways. J Thorac Imaging 2004;19:235–240. [DOI] [PubMed] [Google Scholar]
- 42.Martinez FJ, Kotloff R. Prognostication in chronic obstructive pulmonary disease: implications for lung transplantation. Semin Respir Crit Care Med 2001;22:489–498. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.