Abstract
We formulated PA-824, a nitroimidazopyran with promise for the treatment of tuberculosis, for efficient aerosol delivery to the lungs in a dry powder porous particle form. The objectives of this study were to prepare and characterize a particulate form of PA-824, assess the stability of this aerosol formulation under different environmental conditions, and determine the pharmacokinetic parameters for the powder after pulmonary administration. The drug was spray dried into porous particles containing a high drug load and possessing desirable aerosol properties for efficient deposition in the lungs. The physical, aerodynamic, and chemical properties of the dry powder were stable at room temperature for 6 months and under refrigerated conditions for at least 1 year. Pharmacokinetic parameters were determined in guinea pigs after the pulmonary administration of the PA-824 powder formulation at three doses (20, 40, and 60 mg/kg of body weight) and compared to those after the intravenous (20 mg/kg) and oral (40 mg/kg) delivery of the drug. Oral and inhaled delivery of PA-824 achieved equivalent systemic delivery at the same body dose within the first 12 h of dosing. However, animals dosed by the pulmonary route showed drug loads that remained locally in the lungs for 32 h postexposure, whereas those given the drug orally cleared the drug more rapidly. Therefore, we expect from these pharmacokinetic data that pulmonary delivery may achieve the same efficacy as oral delivery at the same body dose, with a potential improvement in efficacy related to pulmonary infection. This may translate into the ability to deliver lower body doses of this drug for the treatment of tuberculosis by aerosol.
The global epidemic caused by the infectious disease tuberculosis (TB) has recently garnered attention due to the growing concern over the emergence of multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), which are caused by Mycobacterium tuberculosis strains that show resistance to multiple first-line drugs or that are virtually untreatable by existing anti-TB antibiotics (7). An investigational nitroimidazopyran, PA-824, is one of the most promising anti-TB drug candidates to have been discovered in 30 years. PA-824 appears to have bactericidal activity against both active replicating and persisting or latent M. tuberculosis strains and has the potential to be used for the treatment of MDR-TB (21). It has been proposed that this activity against static bacilli could help sterilize TB lesions faster (26). Therefore, reduced treatment times may be possible with drug regimens that include PA-824. Any advance in anti-TB therapy that addresses drug-resistant TB and that reduces the frequency of dosing, the dose required, and the duration of treatment has the potential to improve patient treatment.
Preclinical evaluation with animal models of PA-824 alone and in combination with moxifloxacin, rifampin (rifampicin), isoniazid, and/or pyrazinamide indicated the potential of the use of PA-824 alone and in combination for the treatment of TB and MDR-TB (10, 13-15, 21, 22, 25). In those studies, the drugs were delivered orally, with likely only a fraction of the administered dose reaching the lung tissue, the primary infection site of M. tuberculosis. Thus, the direct delivery of PA-824 to the lungs could improve the effectiveness of treatment by increasing the local concentration of drug in the lungs, thereby targeting pulmonary TB, while still delivering drug systemically for nonpulmonary TB. It is also possible that this noninvasive route of administration may require smaller doses than standard oral treatment, thus potentially reducing side effects and shortening the time of treatment. Inhaled antibiotics have been demonstrated to improve the treatment of TB (18) and other diseases, such as cystic fibrosis (19). However, these treatments were given by nebulization, a process which requires lengthy treatment times and sterile water to achieve relatively low delivery efficiencies (9).
The dry powder inhaler is an alternative method for pulmonary drug delivery and has the ability to deliver stable formulations easily from simple inhalers. The porous particle system, a dry powder formulation, is well suited for efficient delivery to the lungs (2). Use of this novel particulate aerosol has also been explored for the treatment of TB with the tuberculostatic agents para-aminosalicyclic acid (PAS) and capreomycin (3, 4, 23). PAS, delivered as a dry powder, was shown to achieve greater lung exposure in rats at a lower total body drug dose than the typical oral dose (23). The pulmonary delivery of capreomycin gave promising efficacy results in a guinea pig model of TB, with lower wet organ weights and bacterial burdens in the lungs of animals given treatment by aerosol delivery than animals given intravenous (i.v.) or intramuscular treatment (3, 4). Thus, the pulmonary administration of PA-824 in a porous particle form may provide an additional therapeutic advantage for this promising new drug. In the present study, PA-824 was formulated for aerosol delivery to a porous particle form and the powder was characterized for its physical and aerosol properties. The powder was tested for its physical, aerodynamic, and chemical stability under a variety of environmental conditions over a period of 1 year.
The disposition of PA-824 after oral delivery was previously determined in mice (11, 13), rats (20), and dogs and monkeys (16), but not after pulmonary delivery to guinea pigs. The M. tuberculosis-infected guinea pig model is a clinically relevant animal model with respect to the disease in humans because the pathogenesis and lung pathology in guinea pigs mimic those in humans with active TB (12, 17, 24). It is likely that the disposition of the drug will be different in M. tuberculosis-infected animals than in healthy animals. As the initial step in the determination of the disposition of PA-824 in guinea pigs, the present studies were conducted with healthy animals to define the baseline pharmacokinetic (PK) parameters of PA-824 after i.v. administration of the solution form and pulmonary administration of the dry powder formulation, and the PK parameters were compared to those obtained after delivery by the standard oral route. In addition, local PA-824 concentrations were determined in the lungs after the drug concentration became undetectable in the systemic circulation to evaluate the efficiency of delivery by both routes of administration.
MATERIALS AND METHODS
Materials.
l-Leucine was obtained from Spectrum Chemicals & Laboratory Products (Gardena, CA), and the phospholipid 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC) was obtained from Genzyme Pharmaceuticals (Cambridge, MA). PA-824 was received from the Global Alliance for TB Drug Development (New York, NY). Acetonitrile, ethanol (USP grade), and methanol were purchased from Pharmco Products Inc. (Brookfield, CT). Water from a Millipore Corp. (Billerica, MA) Milli-Q water purification system was used.
Preparation of porous particles.
The spray drying solution was prepared by dissolving l-leucine in pure water at 55°C. PA-824 and DPPC were then added to ethanol with heating and stirring. The aqueous solution was added to the ethanol mixture immediately before it was spray dried to achieve a final solids concentration of 4 g/liter and a solvent ratio of 70% ethanol and 30% water (vol/vol). The final formulation consisted of 75% PA-824, 20% l-leucine, and 5% DPPC (wt %).
Porous particles were prepared by using a Niro, Inc., Mobile Minor spray dryer (Columbia, MD). The inlet temperature was set at 107°C, and the solution feed rate was set at 60 ml/min. The solution was pumped into the two-fluid nozzle of the spray dryer at a gas flow rate of 25 g/min. The spray dried powders were collected in a container at the outlet of the cyclone.
Particle characterization. (i) Characterization of dry powders.
The volume diameter of the spray dried powder was measured by laser diffraction with a HELOS system and RODOS dry dispersing unit (Sympatec Inc., Lawrenceville, NJ). Each measurement was performed in triplicate at an applied pressure of 2 bar.
The aerodynamic properties and particle distribution of the powder (fine particle fraction [FPF], mass median aerodynamic diameter [MMAD], geometric standard deviation [GSD]) were determined by the standard methodology with an eight-stage Andersen cascade impactor (Copley Scientific Limited, Nottingham, United Kingdom). The FPF of the total dose (FPFTD) of powder less than or equal to an effective cutoff aerodynamic diameter of 5.8 μm was calculated by dividing the powder mass recovered from stages 1 to 7 of the impactor by the total particle mass.
The morphology of the dry particles was evaluated with a 982 field emission scanning electron microscope (LEO; Carl Zeiss, Inc., Thornwood, NY) after the powder samples were coated with a platinum-palladium layer (208HR sputter coater; Cressington Scientific Instruments Inc., Watford, United Kingdom).
(ii) Drug load of powders.
The PA-824 load of the spray dried powder was determined by a reverse-phase high performance liquid chromatography (HPLC) method with an 1100 series HPLC system with Zorbax columns and ChemStation software (Agilent Technologies Inc., Palo Alto, CA). The mobile phase was run on a linear gradient from 20% acetonitrile and 80% water to 60% acetonitrile and 40% water over 30 min with 5 min of equilibration time. Analysis was performed with 50 μl injected at a flow rate of 1.5 ml/min through an Agilent Zorbax Eclipse XDB-C18 column (4.6 by 150 mm), and the absorbance at 330 nm was recorded. An Agilent Zorbax Eclipse XDB-C18 analytical guard column was also used.
(iii) Powder stability study.
A spray dried PA-824 formulation of 75% PA-824, 20% l-leucine, and 5% DPPC (wt %) was stored under different environmental conditions to assess its physical, aerodynamic, and chemical stability over time. Powder aliquots were transferred to glass vials in a controlled environment held at 10% relative humidity and were then placed at temperatures of 4°C, 25°C, and 40°C, which represent refrigerated, room temperature and accelerated storage conditions, respectively. Sealed sample vials were stored protected from the light in polyethylene jars with anhydrous calcium sulfate desiccant (W. A. Hammond Drierte Co., Xenia, OH). Samples were removed from storage at 0, 0.5, 1, 3, 6, and 12 months and were allowed to equilibrate to room temperature before analysis. The powders were analyzed in triplicate for particle size, FPFTD, and drug content. Statistical significance was determined by linear regression analysis, where P values of <0.05 were considered statistically significant.
PK studies. (i) Experimental design.
Male guinea pigs weighing 463.86 ± 65.11 g were employed in the PK studies. Animals were housed under a cycle of 12 h of light and 12 h of dark and in an environment with a constant temperature of 22°C. A standard diet and water were supplied ad libitum. All animal procedures were approved by the Institutional Animal Care and Use Committee of the University of North Carolina. Twenty-four hours before the study, each animal underwent cannulation of the right external jugular vein for continuous blood sampling (5, 6).
The animals were randomly divided into five groups (n = 6 or 7) that received PA-824 as follows: i.v. in solution at a dose of 20 mg/kg of body weight; as an oral gavage of the drug in a mixed micelle suspension at 40 mg/kg; and as a dry powder via intratracheal insufflation by the pulmonary route as porous powders at nominal doses of 20, 40, and 60 mg/kg. For the insufflation procedure, each animal was anesthetized and the trachea was visualized with a laryngoscope. A small animal insufflator (Penn Century, Philadelphia, PA) was inserted into the trachea and placed at a distance of 1 cm from the carina. PA-824 powders were dispersed with the help of 5 ml of air from an empty syringe. The insufflator chamber and tube containing the dose of PA-824 powder were weighed carefully before and after delivery to the animal to estimate the actual dose delivered to be used for the PK analysis for each animal.
PA-824 was formulated into a micelle suspension for oral dosing with 10% hydroxypropyl-β-cyclodextrin and 10% lecithin, as described previously (15). PA-824 doses were based on the results of a study of the efficacy of oral administration of PA-824 in a guinea pig model of TB in which a dose of 40 mg/kg delivered daily for 30 days showed a statistically significant reduction in the numbers of bacilli in the lungs and spleen (21). After drug administration, blood samples (0.35 ml) were collected from each animal and placed into heparinized tubes at 0, 0.08, 0.25, 0.5, 1, 2, 3, 4, 5, 6, 8, 12, and 24 h. Additional samples were collected at 28 and 32 h from animals dosed with the powder at 60 mg/kg. Sterile saline solution was used to replace the blood volume lost through sample collection. Plasma was separated and stored at −80°C until analysis. After collection of the last blood sample, the animals were euthanized by exanguination and bronchoalveolar lavage (BAL) fluid was collected (with 5 ml sterile saline). The BAL fluid sample was centrifuged, and the pellet and the supernatant were separated.
(ii) Sample analysis.
Plasma and BAL samples were analyzed for their drug contents by a validated HPLC assay. Serum concentrations of PA-824 were determined with a system consisting of a ThermoFinnegan P4000 HPLC pump (San Jose, CA) with a model AS1000 fixed-volume autosampler, a model UV2000 UV detector, a Gateway Series e computer (Poway, CA), and the Chromquest HPLC data management system. The plasma standard concentration curve for PA-824 ranged from 0.20 to 50 μg/ml. The absolute recovery of PA-824 from plasma was 88.2%. The overall precision of the validation assay across all standards was 0.67 to 5.38%. Sample preparation for the BAL fluid supernatant was an adaptation of the method for plasma, and an HPLC method identical to that used for plasma was used.
(iii) PK analysis.
The PK parameters area under the curve (AUC), elimination rate constant (K), mean residence time (MRT), half-life (t1/2), and bioavailability (F) were obtained by noncompartmental methods (WinNonlin program; Pharsight Corporation, Mountain View, CA). The maximum PA-824 concentration (Cmax) and the time to obtain Cmax (Tmax) were determined from the nonfitted plasma concentration-versus-time profiles for each individual animal. F was calculated by the following equation: (AUClung, oral/AUCi.v.) × (Di.v./Dlung, oral), where D is the dose. The subscripts indicate the routes of administration: i.v., pulmonary (lung), and gastrointestinal (oral).
Statistical analysis.
Data for the PK study were subjected to analysis of variance and the least-squares significant-differences multiple-comparison method. A probability level of 5% (P < 0.05) was considered statistically significant.
RESULTS
Particle manufacture and characterization.
Porous particles with a load of approximately 75% (wt/wt) PA-824 were prepared by spray drying. The resulting dry powder formulation consisted of thin-walled porous particle structures, as shown in Fig. 1. The median volume diameter of the particles was 4.14 ± 0.04 μm; and the particles had desirable aerosol properties for human pulmonary delivery (1, 8), as indicated by a mass median aerodynamic diameter of 4.74 ± 0.08 μm with a geometric standard deviation of 1.53 ± 0.02, and an FPFTD of 53.3 ± 2.7%. The PA-824 content of the powder was 74.8 ± 0.5% of the total mass, as estimated by HPLC with UV detection.
FIG. 1.
Scanning electron micrograph of spray dried PA-824 porous particles. Bar, 2 μm.
Powder stability study.
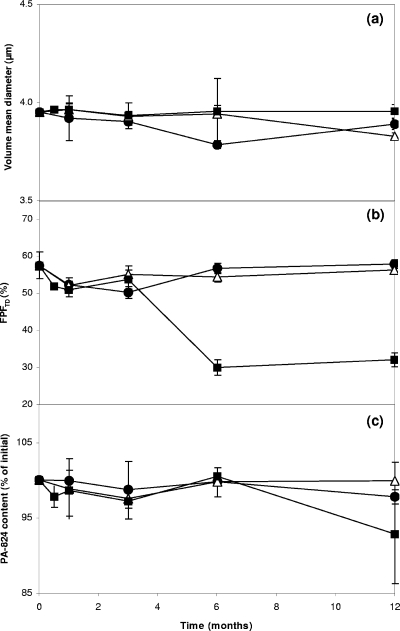
The stability of a PA-824 powder formulation composed of 75% PA-824, 20% l-leucine, and 5% DPPC (wt %) was studied for 1 year at a refrigerated temperature (4°C), at room temperature (25°C), and under accelerated conditions (40°C). The results of the volume median diameter, FPFTD, and PA-824 content analysis over time are shown in Fig. 2. The powder showed no statistically significant differences (P > 0.05) in physical or aerodynamic characteristics or chemical content after storage for 1 year under refrigerated conditions and for at least 6 months at room temperature compared with those before storage. Under the accelerated condition (40°C), the powder maintained its stability for at least 3 months and showed a significant decline in aerosol properties only at 6 months (P = 0.00) and in PA-824 content only at 1 year (P = 0.04).
FIG. 2.
PA-824 porous powder stability data for volume median diameter (a), fine particle fraction of the total dose (b), and PA-824 content (c) as a percentage of the initial value at 4°C (•), 25°C (Δ), and 40°C (▪) over a period of 12 months.
PK studies.
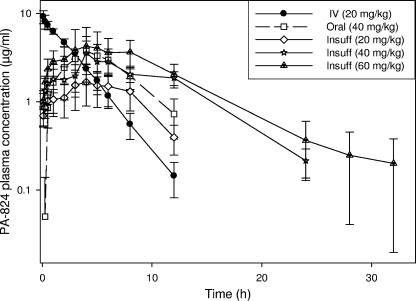
Average PA-824 plasma concentration-versus-time curves are shown in Fig. 3. The terminal phases of these curves appear to be linear for all treatments. A dose dependency was observed among groups receiving particles by the pulmonary route, with animals receiving the largest dose having the highest plasma concentration and with PA-824 remaining detectable for a longer period of time. Interestingly, the plasma concentration-versus-time profiles for animals dosed with 40 mg/kg of PA-824 by the oral and pulmonary routes almost appeared to be superimposable for the first 8 h, but PA-824 was detectable in the plasma of animals receiving an oral dose only for 12 h after dosing, whereas it remained detectable in the plasma of animals dosed by the pulmonary route for 24 h after dose administration.
FIG. 3.
Average PA-824 plasma concentration-versus-time curves (log scale) after administration of PA-824 as the following treatments and at the indicated doses: i.v. solution (IV) at 20 mg/kg; oral mixed micelle suspension (Oral) at 40 mg/kg; and insufflated (Insuff) PA-824 dry powder porous particles at 20, 40, and 60 mg/kg. Values are mean ± standard deviations (n = 6 or 7).
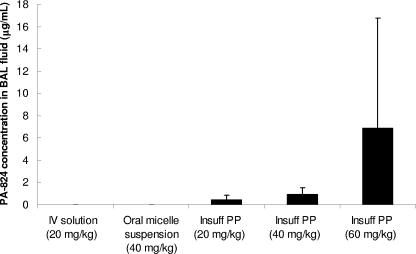
The local PA-824 concentrations remaining in the lungs 32 h after administration of the drug to the different groups are shown in Fig. 4. PA-824 was detectable at levels well above the detection threshold of the analytical method in the lungs of the three groups of animals dosed by the pulmonary route in a dose-dependent manner, whereas no drug was detected in the lungs of animals receiving PA-824 by the i.v. or oral route.
FIG. 4.
PA-824 concentrations in BAL fluid 32 h after dosing. While no PA-824 was found in the lung fluid for drug given as an i.v. solution or an oral mixed micelle suspension, powders given by insufflation (Insuff) showed sustained levels of PA-824 in the lungs after 32 h. There also appeared to be a dose dependency on the drug levels remaining in the lungs. Values are means ± standard deviations (n = 6 or 7). PP, porous particles.
The PK parameters obtained by noncompartmental methods are presented in Table 1. The AUC and Cmax after PA-824 administration by the pulmonary route increased linearly with the dose (R2 = 0.999), with statistically significant differences existing between the three values. The AUCs were statistically comparable in animals receiving 40 mg/kg by the oral and the pulmonary routes. However, PA-824 was eliminated (K) at a lower rate when it was given at doses of 40 and 60 mg/kg by the pulmonary route, correlating with significantly longer t1/2 and MRTs. Notably, among the animals receiving 40 mg/kg PA-824, the t1/2 by the pulmonary route was almost double that among the animals receiving the drug by the oral route. Cmax and Tmax were statistically comparable in the groups of animals receiving the 40- and 60-mg/kg doses. F was approximately 60% and was statistically comparable in all treatment groups.
TABLE 1.
PK parameters obtained by noncompartmental analysis after administration of PA-824 formulations by different routes and at different dosesa
| Route of administration (dose [mg/kg]) | AUC0-t (μg·h/ml) | K (h−1) | t1/2 (h) | MRT (h) | Cmax (μg/ml) | Tmax (h) | F0-∞ | F′ |
|---|---|---|---|---|---|---|---|---|
| i.v. (20) | 26.54 ± 2.202 | 0.37 ± 0.041 | 1.91 ± 0.243 | 2.69 ± 0.313 | 9.19 ± 1.541 | 0.11 ± 0.072 | ||
| Oral (40) | 25.77 ± 6.402 | 0.30 ± 0.052 | 2.43 ± 0.563 | 5.37 ± 0.532 | 4.14 ± 0.782 | 4.00 ± 0.631 | 0.56 ± 0.121 | |
| Insufflation | ||||||||
| 20 | 14.80 ± 3.843 | 0.24 ± 0.012 | 2.83 ± 0.102,3 | 5.17 ± 0.452 | 2.01 ± 0.553 | 4.33 ± 1.031 | 0.59 ± 0.161 | 2.11 ± 0.561 |
| 40 | 32.34 ± 16.792 | 0.17 ± 0.053 | 4.38 ± 1.062 | 7.52 ± 1.911 | 3.42 ± 1.142,3 | 3.25 ± 2.091 | 0.63 ± 0.321 | 1.12 ± 0.572 |
| 60 | 50.96 ± 9.531 | 0.13 ± 0.053 | 5.91 ± 2.511 | 8.26 ± 1.801 | 4.58 ± 2.492 | 3.60 ± 2.881 | 0.62 ± 0.101 | 0.74 ± 0.122 |
Values are means ± standard deviations (n = 6 to 7). AUC0-t, AUC from time zero to time t; F0-∞, F from time zero to infinity; F′, relative F compared to that of oral treatment. The other abbreviations are defined in the text. Numeric superscripts show the relative ranks of the values (starting from the highest values). When the means are not significantly different, the same superscript is used.
DISCUSSION
The continuing TB epidemic, including a growing number of cases of MDR- and XDR-TB, and the increasing coincidence of the synergy between human immunodeficiency virus (HIV) infection and TB, requires new and improved treatment as part of the strategy for containing and reducing the incidence of the infection. The first drug demonstrating promise for the treatment of both active and latent TB is the nitroimidazopyran PA-824, which is typically administered orally. Our goal was to develop PA-824 in a form suitable for delivery as an aerosol directly into the lungs, the primary site of M. tuberculosis infection.
We have shown the potential for the antibiotic PA-824 to be formulated into a dry powder porous particle form that can be delivered efficiently by the pulmonary route. This high-drug-load formulation maintained its physical, aerodynamic, and chemical stability under refrigerated conditions (4°C) for over a year and at room temperature (25°C) for more than 6 months. This stability at room temperature may reduce the need for a cold chain for storage and distribution. Under accelerated conditions (40°C), the stability of the chemical was maintained throughout the 12-month study duration, while its aerodynamic properties showed a significant decline at 6 months at this elevated temperature. This heat sensitivity is typical for dry powders to be delivered by inhalation (3). In summary, the stability of the formulation is temperature dependent, with chemical and physical stability being maintained during the 12-month study duration under refrigerated conditions and for more than 6 months under room temperature conditions, and the stability of the formulation will likely allow the drug to tolerate short-term storage excursions at higher temperatures.
PK parameters in guinea pigs were determined after the oral administration of PA-824 in the present study and revealed that the disposition of PA-824 differed from that reported in the literature for other species. After oral administration, the t1/2 in guinea pigs (2.43 h) was comparable to that in monkeys and rats (2 to 5 h) (16), but it was slightly longer than that in dogs (1 to 2 h), confirming the observation that systemic absorption in dogs may be low due to poor absorption and rapid metabolism (16). The Tmax after oral administration to guinea pigs (4 h) was also similar to that in monkeys (3.33 h), but it was significantly shorter than that in rats (6 to 8 h), which may indicate a shorter absorption time in guinea pigs. Cmax 14- and 17-fold higher than the MIC of PA-824 for M. tuberculosis (0.015 to 0.25 μg/ml) (21) was observed in guinea pigs after pulmonary and oral administration of a 40-mg/kg dose, respectively. In contrast, Nuermberger et al. (13) reported Cmax of 80- to 110-fold higher than the MIC in mice after the oral administration of a 100-mg/kg dose. These observations may be the result of the administration of different doses but also variations in the disposition of this drug in the two species. Therefore, caution should be exercised when PK parameters from one species are selected to identify a dose or a dosing regimen that includes PA-824 for the treatment of TB in another species.
In the present study, Cmax and AUC showed a linear dose dependency for powders administered to guinea pigs by the pulmonary route, as was previously reported for mice after the oral administration of PA-824 (11).
Differences in the disposition of PA-824 were observed in guinea pigs when the drug was administered by different routes at the same dose. The systemic PA-824 levels appeared to be similar following delivery by the pulmonary and oral routes within the first 12 h after dosing of 40 mg/kg. However, the drug was not detectable in plasma after 12 h in animals receiving oral doses, whereas systemic drug levels remained detectable in animals dosed by the pulmonary route until 24 h. This observation is consistent with the slower elimination rates and longer t1/2 and MRT obtained for animals dosed by the pulmonary route. Most notably, PA-824 concentrations were sustained locally in the lung for 32 h after dosing, even after systemic concentrations were undetectable. Tissue concentrations three- to eightfold higher than those in plasma have also been reported after the oral administration of PA-824 to rats (20). However, these observations were made at much earlier time points (4 to 6 h) than they were made in the present study (32 h). Thus, we show that delivery of the drug directly to the lungs confers the advantage of increasing the tissue concentrations of drug at the primary site of M. tuberculosis infection for longer periods of time than the times for the drug delivered orally.
The PK data for guinea pigs reported in the present study indicate that aerosol administration to the lungs achieves systemic exposure either comparable to or lower than that achieved by administration by the oral route and achieves elevated local lung concentrations compared with those achieved after delivery by the oral route. Therefore, we propose that pulmonary delivery may achieve the same efficacy as oral delivery at the same body dose, with a potential improvement in effectiveness related to pulmonary infection. This may translate into the ability to deliver lower body doses with less frequency than the frequency required for the standard dosing regimens.
Acknowledgments
This work was supported by a grant (grant 5 U01 61336) from the National Institutes of Health/NIAID and a National Science Foundation Graduate Research Fellowship.
We acknowledge the Global Alliance for TB Drug Development for the PA-824 material used in this study and Melvin Spigelman and Doris Rouse for their assistance. We also thank Plastiape for its generous donation of inhaler devices.
Footnotes
Published ahead of print on 12 January 2009.
REFERENCES
- 1.Bates, D. V., B. R. Fish, T. F. Hatch, T. T. Mercer, and P. E. Morrow. 1966. Deposition and retention models for internal dosimetry of the human respiratory tract. Task group on lung dynamics. Health Physics 12:173-207. [PubMed] [Google Scholar]
- 2.Edwards, D. A., J. Hanes, G. Caponetti, J. Hrkach, A. Ben-Jebria, M. L. Eskew, J. Mintzes, D. Deaver, N. Lotan, and R. Langer. 1997. Large porous particles for pulmonary drug delivery. Science 276:1868-1872. [DOI] [PubMed] [Google Scholar]
- 3.Fiegel, J., L. Garcia-Contreras, M. Thomas, J. VerBerkmoes, K. Elbert, A. Hickey, and D. Edwards. 2008. Preparation and in vivo evaluation of a dry powder for inhalation of capreomycin. Pharm. Res. 25:805-811. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Contreras, L., J. Fiegel, M. J. Telko, K. Elbert, A. Hawi, M. Thomas, J. VerBerkmoes, W. A. Germishuizen, P. B. Fourie, A. J. Hickey, and D. Edwards. 2007. Inhaled large porous particles of capreomycin for treatment of tuberculosis in a guinea pig model. Antimicrob. Agents Chemother. 51:2830-2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garcia-Contreras, L., and A. J. Hickey. 2002. Pharmacokinetics of aerosolized rifampicin in the guinea pig, p. 699-702. In R. N. Dalby, P. R. Byron, J. Peart, and S. Farr (ed.), Respiratory drug delivery VIII, vol. 2. Davis Horwood International Publishing, Ltd., Raleigh, NC. [Google Scholar]
- 6.García-Contreras, L., J. Sung, K. Elbert, A. Hawi, M. Robinson, D. A. Edwards, and A. J. Hickey. 2006. Pharmacokinetics of aerosolized rifampicin large porous particles in the guinea pig, p. 873-876. In R. N. Dalby, P. R. Byron, J. Peart, J. D. Suman, and S. Farr (ed.), Respiratory drug delivery X, vol. 3. Davis Healthcare International Publishing, LCC, River Grove, IL. [Google Scholar]
- 7.Goldman, R. C., K. V. Plumley, and B. E. Laughon. 2007. The evolution of extensively drug resistant tuberculosis (XDR-TB): history, status and issues for global control. Infect. Disorders Drug Targets 7:73-91. [DOI] [PubMed] [Google Scholar]
- 8.Hickey, A. J. 2004. Summary of common approaches to pharmaceutical aerosol administration, p. 385-421. In A. J. Hickey (ed.), Pharmaceutical inhalation aerosol technology, vol. 134. Marcel Dekker, New York, NY. [Google Scholar]
- 9.Le Brun, P. P. H., A. H. de Boer, H. W. Frijlink, and H. G. M. Heijerman. 2000. A review of the technical aspects of drug nebulization. Pharm. World Sci. 22:75-81. [DOI] [PubMed] [Google Scholar]
- 10.Lenaerts, A. J., V. Gruppo, K. S. Marietta, C. M. Johnson, D. K. Driscoll, N. M. Tompkins, J. D. Rose, R. C. Reynolds, and I. M. Orme. 2005. Preclinical testing of the nitroimidazopyran PA-824 for activity against Mycobacterium tuberculosis in a series of in vitro and in vivo models. Antimicrob. Agents Chemother. 49:2294-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lillibridge, J. H., C. S. Nywall, R. M. Shawar, and J. T. Slattery. 1996. PA-824, a nitroimidazopyran antitubercular agent: favorable pharmacokinetic parameters in mice after delivery of a novel oral formulation, abstr. F216, p.137. Abstr. 36th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 12.McMurray, D. N. 1994. Guinea pig model of tuberculosis, p. 135-148. In B. R. Bloom (ed.), Tuberculosis: pathogenesis, protection and control. ASM Press, Washington, DC.
- 13.Nuermberger, E., I. Rosenthal, S. Tyagi, K. N. Williams, D. Almeida, C. A. Peloquin, W. R. Bishai, and J. H. Grosset. 2006. Combination chemotherapy with the nitroimidazopyran PA-824 and first-line drugs in a murine model of tuberculosis. Antimicrob. Agents Chemother. 50:2621-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nuermberger, E., S. Tyagi, R. Tasneen, K. N. Williams, D. Almeida, I. Rosenthal, and J. H. Grosset. 2008. Powerful bactericidal and sterilizing activity of a regimen containing PA-824, moxifloxacin, and pyrazinamide in a murine model of tuberculosis. Antimicrob. Agents Chemother. 52:1522-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nuermberger, E., S. Tyagi, K. N. Williams, I. Rosenthal, W. R. Bishai, and J. H. Grosset. 2005. Rifapentine, moxifloxacin, or DNA vaccine improves treatment of latent tuberculosis in a mouse model. Am. J. Respir. Crit. Care Med. 172:1452-1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O'Brien, R. J., and M. K. Spigelman. 2005. New drugs for tuberculosis: current status and future prospects. Clin. Chest Med. 26:327-340. [DOI] [PubMed] [Google Scholar]
- 17.Ordway, D., G. Palanisamy, M. Henao-Tamayo, E. E. Smith, C. Shanley, I. M. Orme, and R. J. Basaraba. 2007. The cellular immune response to Mycobacterium tuberculosis infection in the guinea pig. J. Immunol. 179:2532-2541. [DOI] [PubMed] [Google Scholar]
- 18.Sacks, L. V., S. Pendle, D. Orlovic, M. Andre, M. Popara, G. Moore, L. Thonell, and S. Hurwitz. 2001. Adjunctive salvage therapy with inhaled aminoglycosides for patients with persistent smear-positive pulmonary tuberculosis. Clin. Infect. Dis. 32:44-49. [DOI] [PubMed] [Google Scholar]
- 19.Sermet-Gaudelus, I., Y. Le Cocguic, A. Ferroni, M. Clairicia, J. Barthe, J. Delaunay, V. Brousse, and G. Lenoir. 2002. Nebulized antibiotics in cystic fibrosis. Pediatr. Drugs 4:455-467. [DOI] [PubMed] [Google Scholar]
- 20.Spigelman, M. K. 2007. New tuberculosis therapeutics: a growing pipeline. J. Infect. Dis. 196:S28-S34. [DOI] [PubMed] [Google Scholar]
- 21.Stover, C. K., P. Warrener, D. R. VanDevanter, D. R. Sherman, T. M. Arain, M. H. Langhorne, S. W. Anderson, J. A. Towell, Y. Yuan, D. N. McMurray, B. N. Kreiswirth, C. E. Barry, and W. R. Baker. 2000. A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis. Nature 405:962. [DOI] [PubMed] [Google Scholar]
- 22.Tasneen, R., S. Tyagi, K. Williams, J. Grosset, and E. Nuermberger. 2008. Enhanced bactericidal activity of rifampin and/or pyrazinamide when combined with PA-824 in a murine model of tuberculosis. Antimicrob. Agents Chemother. 52:3664-3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsapis, N., D. Bennett, K. O'Driscoll, K. Shea, M. M. Lipp, K. Fu, R. W. Clarke, D. Deaver, D. Yamins, and J. Wright. 2003. Direct lung delivery of para-aminosalicylic acid by aerosol particles. Tuberculosis 83:379-385. [DOI] [PubMed] [Google Scholar]
- 24.Turner, O. C., R. J. Basaraba, and I. M. Orme. 2003. Immunopathogenesis of pulmonary granulomas in the guinea pig after infection with Mycobacterium tuberculosis. Infect. Immun. 71:864-871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tyagi, S., E. Nuermberger, T. Yoshimatsu, K. Williams, I. Rosenthal, N. Lounis, W. Bishai, and J. Grosset. 2005. Bactericidal activity of the nitroimidazopyran PA-824 in a murine model of tuberculosis. Antimicrob. Agents Chemother. 49:2289-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams, K. J., and K. Duncan. 2007. Current strategies for identifying and validating targets for new treatment-shortening drugs for TB. Curr. Mol. Med. 7:297-307. [DOI] [PubMed] [Google Scholar]