Abstract
Bacillus anthracis is the causative agent of anthrax. We have developed a novel whole-bacterial-cell anthrax vaccine utilizing B. anthracis that is killed but metabolically active (KBMA). Vaccine strains that are asporogenic and nucleotide excision repair deficient were engineered by deleting the spoIIE and uvrAB genes, rendering B. anthracis extremely sensitive to photochemical inactivation with S-59 psoralen and UV light. We also introduced point mutations into the lef and cya genes, which allowed inactive but immunogenic toxins to be produced. Photochemically inactivated vaccine strains maintained a high degree of metabolic activity and secreted protective antigen (PA), lethal factor, and edema factor. KBMA B. anthracis vaccines were avirulent in mice and induced less injection site inflammation than recombinant PA adsorbed to aluminum hydroxide gel. KBMA B. anthracis-vaccinated animals produced antibodies against numerous anthrax antigens, including high levels of anti-PA and toxin-neutralizing antibodies. Vaccination with KBMA B. anthracis fully protected mice against challenge with lethal doses of toxinogenic unencapsulated Sterne 7702 spores and rabbits against challenge with lethal pneumonic doses of fully virulent Ames strain spores. Guinea pigs vaccinated with KBMA B. anthracis were partially protected against lethal Ames spore challenge, which was comparable to vaccination with the licensed vaccine anthrax vaccine adsorbed. These data demonstrate that KBMA anthrax vaccines are well tolerated and elicit potent protective immune responses. The use of KBMA vaccines may be broadly applicable to bacterial pathogens, especially those for which the correlates of protective immunity are unknown.
Bacillus anthracis is a spore-forming gram-positive bacterium that is the causative agent of the disease anthrax. The primary determinants of B. anthracis pathogenesis are lethal toxin (LeTx), edema toxin (EdTx), and capsule, the genes for which are carried on the large virulence plasmids pXO1 and pXO2 (20, 57). LeTx and EdTx are each bipartite A-B toxins with a common subunit, protective antigen (PA), that mediates entry of the active toxin components lethal factor (LF) and edema factor (EF) into the host cell cytoplasm (reviewed in reference 4). The genes that encode PA, LF, and EF are pagA, lef, and cya, respectively (39, 47, 53, 58). Once in the cytosol, LF functions as a zinc metalloprotease that cleaves mitogen-activated protein kinase kinase, resulting in death in macrophages and dendritic cells (4, 15). EF is a calmodulin-dependent adenylate cyclase that causes an increase in cyclic AMP (31). In addition to promoting either cell death or edema, LeTx and EdTx have also been shown to have a wide range of immunomodulatory functions when added to macrophages, dendritic cells, neutrophils, and B and T lymphocytes in vitro (1, 3, 4, 14, 16, 40, 48, 54). The B. anthracis capsule consists of a polymer of gamma-linked d-glutamic acid (γDPGA) that is formed by products of the capBCADE operon on pXO2 (37). The B. anthracis γDPGA capsule is antiphagocytic and plays a major role in the virulence of the organism. Strains that lack pXO2 are dramatically reduced in virulence, whereas nontoxinogenic encapsulated strains of B. anthracis retain virulence in mice (22, 62).
Immunity to anthrax is mediated largely by an antibody (humoral) response, and the primary immune correlates of protection are circulating antibodies specific for PA that have LeTx-neutralizing activity (34, 42). The development of a pXO1+ pXO2− nonencapsulated vaccine strain was accomplished by Sterne in 1939 (52), and this vaccine is still used in livestock (56). A Sterne-like strain was also used to vaccinate humans in the former Soviet Union and was reported to reduce the incidence of cutaneous disease (51). Since pXO1+ pXO2− strains contain functional toxin genes and cause significant disease in mice, Brossier et al. developed a vaccine strain that expressed catalytically inactive forms of EF and LF (10). This strain was avirulent and induced a robust toxin-neutralizing response that protected mice from lethal subcutaneous (s.c.) B. anthracis challenge.
The only licensed vaccine for human use in the United States is a protein-based vaccine called anthrax vaccine adsorbed (AVA). AVA (now marketed as BioThrax) is composed of B. anthracis culture supernatant proteins containing variable amounts of PA, LF, and EF adsorbed to aluminum hydroxide gel as an adjuvant. The vaccination regimen for AVA requires six s.c. doses to be administered over an 18-month period, followed by annual boosters. This vaccination regimen is impractical and frequently causes significant local inflammation and occasionally severe adverse events (50). Since the bioterrorism attacks of 2001, there has been renewed interest in developing new vaccines that protect humans against inhalation anthrax and that do not require as rigorous a vaccination regimen or elicit adverse events. As the primary immune correlate of protection is circulating anti-PA antibody, an anthrax vaccine based on purified recombinant PA (rPA) has been developed for human use. This vaccine (called rPA102) is composed of rPA combined with aluminum hydroxide as an adjuvant (19). rPA-based vaccines have been shown to induce high-titer anti-PA responses in animals and can protect rabbits and nonhuman primates against lethal B. anthracis challenge (26, 35); however, in some studies, protection waned dramatically over 6 to 12 months (35). Another major drawback to rPA-based vaccines is that they stimulate immunity to only a single B. anthracis antigen, PA. Thus, it would be preferable to develop a multivalent anthrax vaccine that potently stimulates a broad immune response to rPA and other anthrax antigens, as well. Indeed, it has been demonstrated that immunity to capsule- and spore-specific antigens can also contribute to vaccine potency (9, 13).
Live-attenuated vaccines can provide robust and long-lived immunity but present potential safety risks among immunocompromised individuals. While vaccines based on killed bacteria are safer, they are often less potent. We have recently developed a new class of vaccines based on psoralen-killed but metabolically active (KBMA) bacteria that combine the safety of killed vaccines with the potency of live vaccines (7). Psoralens form covalent monoadducts and cross-links with pyrimidine bases of DNA and RNA upon exposure to long-wavelength UV (UVA) light (64). Amotosalen HCl (S-59) is a synthetic psoralen that has been developed for pathogen inactivation in blood products (33). Photochemical treatment (PCT) with S-59 and UVA inactivates a broad range of prokaryotic, eukaryotic, and viral pathogens by overwhelming the ability of the pathogens to repair the numerous lesions in their genomes. The primary mechanism by which bacteria repair psoralen-induced DNA damage is through nucleotide excision repair (NER). NER is initiated by the ABC exinuclease complex, a product of the UV light response (uvrA, uvrB, and uvrC) genes. Bacteria defective for NER are incapable of repairing cross-links in their DNA and are exquisitely sensitive to photochemical inactivation by combined treatment with psoralen and UVA light (7, 49). Replication can be blocked in NER-deficient bacteria with a single covalent cross-link in the chromosome, thus preserving the expression repertoire of the organism and its immunogenicity. The KBMA vaccine strategy was initially demonstrated with Listeria monocytogenes, and it was shown that photochemically inactivated NER-deficient L. monocytogenes maintained the ability to escape the host cell phagosome, deliver secreted antigens to the major histocompatibility complex class 1 pathway, and provide protective cell-mediated immunity (7). Recently, the KBMA vaccine strategy was extended to Salmonella enterica serovar Typhimurium vaccines (30). Here, we report the construction of a series of vaccine candidate strains with sequential unmarked mutations in the B. anthracis strain Sterne 7702 (Sterne) chromosome and on pXO1, culminating in a strain that is asporogenic, NER deficient, and nontoxinogenic that can be produced as a KBMA vaccine. We demonstrate that KBMA B. anthracis vaccines provide protective humoral immunity against lethal B. anthracis challenge in mice, rabbits, and guinea pigs. These results provide the rationale for the development of a new anthrax vaccine that elicits a greater breadth of immunity than existing subunit vaccines.
MATERIALS AND METHODS
Strain construction.
All B. anthracis vaccine strains were derived from Sterne (pXO1+ pXO2−), which was generously provided by Theresa M. Koehler (12). All genetic manipulations to construct vaccine candidates were performed by serial allelic exchange, using methods described previously (11), leaving unmarked mutations on the chromosome or pXO1 that were confirmed by PCR and sequence analysis. The ΔuvrAB mutant was described previously (7). The ΔspoIIE allele was constructed by splice overlap extension PCR (24), using Sterne genomic DNA as a template and the primers Spo2A (5′-TAACGACCGCGCTCCAAAAG-3′), Spo2B (5′-CGGCATATTTTTCTTCACTTTTGCCCACTTTACTCCTCCAAGCTGACC-3′), Spo2C (5′-GGTCAGCTTGGAGGAGTAAAGTGGGCAAAAGTGAAGAAAAATATGCCG-3′), and Spo2D (5′-TGCATTCATCCCGTATTGCT-3′). The resulting PCR product was first cloned into pCRII-TOPO (Invitrogen) and then subcloned into the EcoRI restriction sites of pKSV7, after allelic exchange, this resulted in an in-frame deletion of 2,328 bp from positions 33 to 2361 with respect to the start of the spoIIE coding region in either the Sterne background, to generate the ΔspoIIE strain, or the ΔuvrAB background, to generate the Sterne2 strain. Inactivating substitution mutations that abrogate the activity of EF [cya(K346/353Q)] and LF [lef(H686A)] have been described previously (27, 29, 65, 10) and were constructed by PCR primer-based mutagenesis followed by allelic exchange as described above. Briefly, the primers CyaF (5′-AGATAAAATACAGCAGACACAAGAC-3′) and CyaR (5′-TAGTTGAATCCGGTTTCCTC-3′) were used to amplify the cya gene. Codons for lysine at positions 346 and 353 of the mature protein were replaced with codons for glutamine using primers Cya1F (5′-GGTGTGGCTACACAGGGATTGAATGTTCATG-3′), Cya1R (5′-CATGAACATTCAATCCCTGTGTAGCCACACC-3′), Cya2F (5′-GATTGAATGTTCATGGACAGAGTTCGGATTGGG-3′), and Cya2R (5′-CCCAATCCGAACTCTGTCCATGAACATTCAATC-3′). The cya(K346/353Q) allele was introduced into pXO1 of Sterne2 to produce Sterne3. For construction of the lef(H686A) allele, primers LefF (5′-AAACCTGCAAATCTGTATAAGC-3′) and LefR (5′-TTATCACCAGATACTCGAGC-3′) were used to amplify a region of the lef gene and LefHAF (5′-AGTGAGGGTTTTATAGCCGAATTTGGACATGCTG-3′) and LefHAR (5′-CAGCATGTCCAAATTCGGCTATAAAACCCTCACT-3′) were used to replace the histidine codon with an alanine codon at position 686 of the mature LF protein. The lef(H686A) allele was introduced into pXO1 of Sterne2 to make Sterne3B or into Sterne3 to make Sterne4, as shown in Table 1.
TABLE 1.
B. anthracis strains used in this study
| Strain name | Plasmid content | Genotype | Relevant characteristic(s) | i.m. LD50 in DBA/2J mice | Reference |
|---|---|---|---|---|---|
| Sterne | pXO1+ pXO2− | Strain 7702 | Unencapsulated parental strain | 6.8 × 100 | 12 |
| ΔspoIIE | pXO1+ pXO2− | ΔspoIIE | Asporogenic | 9.1 × 100 | This study |
| ΔuvrAB | pXO1+ pXO2− | ΔuvrAB | NER deficient | NDa | 7 |
| Sterne2 | pXO1+ pXO2− | ΔspoIIE ΔuvrAB | Asporogenic, NER deficient | 1.4 × 101 | This study |
| Sterne3 | pXO1+ pXO2− | ΔspoIIE ΔuvrABcya(K346/353Q) | Asporogenic, NER deficient, inactive edema factor | 7.2 × 100 | This study |
| Sterne3B | pXO1+ pXO2− | ΔspoIIE ΔuvrABlef(H686A) | Asporogenic, NER deficient, inactive lethal factor | 4.5 × 108 | This study |
| Sterne4 | pXO1+ pXO2− | ΔspoIIE ΔuvrABcya(K346/353Q) lef(H686A) | Asporogenic, NER deficient, inactive edema factor, inactive lethal factor | >7.4 × 108 | This study |
| ΔSterne | pXO1−pXO2− | Unencapsulated, atoxinogenic | >9.0 × 108 | This study |
ND, not determined.
Vegetative-cell growth and storage.
All B. anthracis vegetative cells were grown in brain heart infusion (BHI) (Difco) to late log phase, harvested by centrifugation at 3,000 × g, and washed three times in cryopreservation solution (Hanks balanced salt solution with calcium and magnesium but without phenol red [HBSS]; HyClone) supplemented with 1% sucrose and either directly injected, or frozen in medium containing 8% dimethyl sulfoxide at −80°C. The titers of bacterial suspensions were determined by CFU analysis after plating serial dilutions on BHI agar plates; no adjustments were made for the chain lengths of the bacteria. To induce anthrax toxin production for immunoblotting and for analysis of LeTx activity, B. anthracis vegetative cells were grown overnight in BHI and diluted 1:10 in R medium containing 0.8% sodium bicarbonate (46). Cultures were incubated at 37°C in tightly sealed containers for 4 h. Bacterial pellets and culture supernatants were separated by centrifugation at 3,000 × g, and culture supernatants were filtered through 0.22-μm filters and added directly to J774A.1 cells (ATCC) for toxicity assays or were precipitated with 10% trichloroacetic acid for immunoblotting with anti-PA, anti-LF, or anti-EF monoclonal antibodies. Bacterial pellets were suspended in 2× final sample buffer and were boiled for 5 min prior to being immunoblotted with pooled sera from vaccinated mice. For Western blots to detect recombinant protein, 30 ng of PA and 100 ng of LF and EF were loaded onto gels and transferred to nitrocellulose membranes, cut into strips, and detected with pooled sera diluted 1:500. Reactive antibodies were detected with goat anti-mouse immunoglobulin G-horseradish peroxidase (IgG-HRP) (Jackson Laboratories) diluted 1:10,000, and ECL Plus reagent (GE Healthcare) was used for the autoradiography.
Preparation of photochemically inactivated bacteria.
Photochemical inactivation was performed as previously described (7). Briefly, vegetative cells were grown in BHI to an optical density at 600 nm (OD600) of 0.6, S-59 was added to the cultures at various concentrations, and the cultures were incubated for 1 h at 37°C. The cultures were transferred to polystyrene dishes and irradiated with 6.5 J/cm2 UVA. Inactivated bacteria were formulated in cryopreservation solution as described above for live bacteria and stored at −80°C prior to injection. The titers of vaccine stocks were determined by plating serial dilutions for CFU analysis and measuring the OD600 of the culture just prior to illumination. The OD600-to-CFU ratio of log-phase vegetative cells was determined to be as follows: an OD600 of 1.0 = 2 × 108 CFU. To ensure that equivalent doses of previously frozen photochemically inactivated vaccine stocks were administered to animals, the OD of each was measured by spectrophotometry after it was thawed, and the doses were normalized to CFU equivalents and referred to as particles.
Metabolic-activity assay.
The metabolic activities of inactivated vaccine stocks were measured using the Cell Titer 96 Aqueous Assay (Promega) according to the manufacturer's instructions. The assay measures the reduction in the tetrazolium compound 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium, inner salt (MTS), in the presence of the electron-coupling reagent phenazine methosulfate into a formazan product. The rate of formazan production corresponds to both the number and the metabolic activity of the cells (32). Serial dilutions of KBMA and live bacteria were prepared using BHI in 96-well plates, and 20 μl MTS/phenazine methosulfate solution was added. The absorbance of the formazan was measured at 490 nm every 15 min at 37°C in a Spectramax plus 384 plate reader (Molecular Devices).
Spore preparation.
To induce sporulation, B. anthracis strain Sterne derivatives were incubated in BHI for 8 h at 37°C and were diluted 1:1,000 in phage assay medium (20). The cultures were shaken at 250 rpm and incubated for at least 18 h at 37°C. The cultures were then heated at 68°C for 40 min to kill any remaining vegetative cells. Serial dilutions of the cultures before and after being heated were plated on BHI agar and used to determine the numbers of vegetative cells and spores. To produce Sterne spores for lethal challenge, Sterne 7702 was incubated in phage assay medium for 24 h at 37°C with vigorous shaking, at which time 2 volumes of sterile water was added and the spores were incubated for another 20 h. Spores were collected by centrifugation at 3,000 × g for 20 min at 4°C, washed three times in sterile phosphate-buffered saline (PBS), heated at 68°C for 40 min, and frozen in aliquots at −80°C. The titers of individual aliquots were determined by serial dilution and plating on BHI agar. Ames spores for challenge experiments were produced as described previously (41).
Mouse studies.
Six- to 12-week-old-female C57BL/6J, BALB/c, and DBA/2J mice were obtained from Charles River Laboratories (Wilmington, MA). The mice were housed in individually HEPA-filtered cages with autoclaved bedding. Food and water were supplied to the mice ad libitum. The animals were allowed to acclimate to their surroundings for at least 1 week prior to use. Vaccination and challenge studies were performed under animal protocols approved by the Cerus Institutional Animal Care and Use Committee. Intramuscular (i.m.) injections were performed, after the mice were anesthetized, with 50 μl per quadriceps muscle. Intraperitoneal (i.p.), s.c., and intravenous (i.v.) injections were performed by restraining the mice and delivering 100 μl of inoculum in the peritoneal cavity, under the skin on the flank near the base of the tail, or in the tail vein, respectively. Sterne spore challenges were delivered by s.c. administration. The i.m. 50% lethal dose (LD50) of live vegetative cells was calculated using the method of Reed and Muench (44), as described previously (8).
Preparation of rPA adsorbed to aluminum hydroxide gel for vaccination.
A suspension of 100 μg/ml rPA (List Biological Laboratories), 0.3% aluminum hydroxide (alhydrogel; Accurate Chemical), 150 mM NaCl was prepared and incubated at room temperature for 1 h as previously described (9). Each mouse was administered 10 μg rPA by i.m. injection of 50 μl of the suspension as described above.
Histopathology.
BALB/c mice were injected i.m. with 50 μl into each quadriceps separated by 21 days, delivering a total of 1 × 108 KBMA Sterne2 or Sterne4 vegetative cells or 1 × 107 live Sterne spores, 10 μg rPA, or HBSS or HBSS containing a trace amount of India ink to mark the injection site. One mouse per group was sacrificed at 2 h and 1, 3, 5, 7, 14, and 21 days after the prime vaccination and 1, 7, and 14 days after the boost vaccination. The quadriceps muscle was dissected and fixed in with 10% neutral buffered formalin. Paraffin-embedded tissues were sectioned and stained with hematoxylin and eosin for blinded histological analysis by a board-certified veterinary pathologist (Comparative Biosciences Inc.). Sections of injection sites from both quadriceps muscles for each animal were assessed for severity of inflammation based on three parameters: the relative infiltration of neutrophils (acute cells) and mononuclear cells (chronic cells) and myocyte damage (0 = normal; 1 = minimal; 2 = mild; 3 = moderate; 4 = severe).
ELISA.
Serum samples were tested for specific antibody responses by enzyme-linked immunosorbent assay (ELISA) using standard procedures (34). Blood samples were collected from the retro-orbital sinus of mice, and serum was assayed for PA-specific IgG antibody responses. Ninety-six-well maxiSorp immunoplates (Nunc) were coated with 3 μg of rPA/ml (List Biological Laboratories) in 0.1 M carbonate buffer (pH 9.6) overnight at 4°C and then washed with PBS containing 0.05% (vol/vol) Tween 20. The plates were then blocked with 5% (wt/vol) skim milk in PBS for 1 h. Each serum sample, diluted in PBS-Tween 20 to anti-PA IgG concentrations within the curve range, was plated in triplicate, and the plates were incubated for 1 h. Bound antibody was detected using HRP-conjugated polyclonal goat anti-mouse IgG (Jackson Immunoresearch) diluted 1:10,000 in wash buffer and incubated for 2 h. The plates were developed with 100 μl of TMB substrate (Calbiochem) for 5 to 10 min. The reaction was stopped by the addition of 50 μl 1 M sulfuric acid, and the OD450s of the plates were measured using a Spectramax plus 384 plate reader (Molecular Devices). A standard curve for each plate was generated using serial dilutions of a known concentration of monoclonal mouse anti-PA antibody clone BAP0105 (Fitzgerald Industries). Endpoint serum antibody titers (ng/ml IgG) were calculated from that curve using SoftmaxPro software and a four-parameter logistic equation and then corrected for dilution. Rabbit and guinea pig anti-PA IgGs were detected in serum samples using essentially the same methods described above with the following modifications: alkaline phosphatase-conjugated goat anti-rabbit IgG (Jackson ImmunoResearch) was used to detect rabbit IgG, and HRP-conjugated goat anti-guinea pig IgG (Jackson ImmunoResearch) was used to detect guinea pig IgG. For the rabbit ELISA, the detection reagent was para-nitrophenylphosphate dissolved in 40% diethanolamine substrate buffer, and the OD405 was read. For rabbit and guinea pig ELISAs, endpoint antibody titers were expressed as the maximum dilution of sample giving an absorbance of more than three times the absorbance due to nonspecific binding detected in wells without serum. The serum from each animal was tested individually in duplicate or triplicate, and the titers were calculated as the mean of the reciprocal of the dilution. The titers are presented as geometric means and 95% confidence intervals.
Anthrax LeTx-neutralizing assay.
Antibodies to LeTx were measured for the ability to neutralize the cytotoxicity of recombinant LeTx when added to J774A.1 macrophage cells. Anthrax LeTx-neutralizing assays were performed as described previously (23, 43). Antisera were pooled from groups of animals receiving the same vaccination treatment. The pools were serially diluted in cell culture medium and preincubated in quadruplicate with a final concentration of 250 ng/ml rPA and 50 ng/ml recombinant LF (List Biological Laboratories) for 30 min at room temperature. These concentrations of PA and LF were empirically determined to cause 100% J774A.1 cell lethality. A plate-to-plate transfer from the titration plate to another 96-well plate containing a subconfluent monolayer of J774A.1 cells (plated at 1 × 105 cells/well the day before) was performed. The plates were incubated for 2 to 3 h at 37°C in 5% CO2 until cytopathic effects in the toxin-only control wells were visible by light microscopy. Cell viability was measured using the Cell Titer 96 Aqueous Assay (Promega) as described above. Toxin without sera was used to determine 0% cell viability, cells without toxin were used to determine 100% viability, and 50% viability was calculated as the mean of these values for each plate. For each dilution series of pooled sera, the values were plotted, a curve was generated using a four-parametric-curve fit, and the dilution that achieved 50% viability was determined using SoftMax software and was expressed as the reciprocal of the dilution.
Demonstration of loss of anthrax toxin activity from vaccine candidates.
Frozen B. anthracis vegetative cells (1 × 109 CFU) were transferred to 6 ml R medium with 0.8% sodium bicarbonate in a 50-ml tube with the cap tightly screwed on. The cultures were incubated for 2 h at 37°C with shaking at 140 rpm. The culture supernatant was collected after centrifugation for 10 min at 3,000 × g and filtered through a 0.22-μm filter. The culture filtrates were added directly to subconfluent J774A.1 cells and incubated at 37°C with 5% CO2 until cytopathic effects were observed by microscopy (3.5 h), at which time a 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide assay was performed as described above.
Rabbit protection studies.
New Zealand White rabbits (Myrtles Rabbitry), five animals per group, were immunized i.m. with 1 ml vehicle (HBSS supplemented with 1% sucrose and 8% dimethyl sulfoxide), KBMA Sterne4 (at three concentrations: 1 × 1010, 2 × 109, and 5 × 108 particles/ml), or 500 μl AVA (Bioport Corp.), which is the full human dose. All animals were administered a boost vaccination 4 weeks later. For serum analysis, blood was drawn from the ear vein 2 weeks after the prime vaccination and 3 weeks after the boost vaccination. Four weeks after the boost vaccination, all animals were administered an Ames spore dose 131 times the LD50 into the lungs as a 1-ml instillation just above the tracheal bifurcation, using a bronchoscope. The experimentally determined titer of the challenge dose was 9.20 × 105 spores per animal. Ames challenge studies were performed within a registered select agent animal biosafety level 3 facility at the University of New Mexico Health Sciences Center. The animals were allowed at least 7 days to acclimate before being used in the study, and all protocols were approved by the University of New Mexico Health Sciences Center Institutional Animal Care and Use Committee.
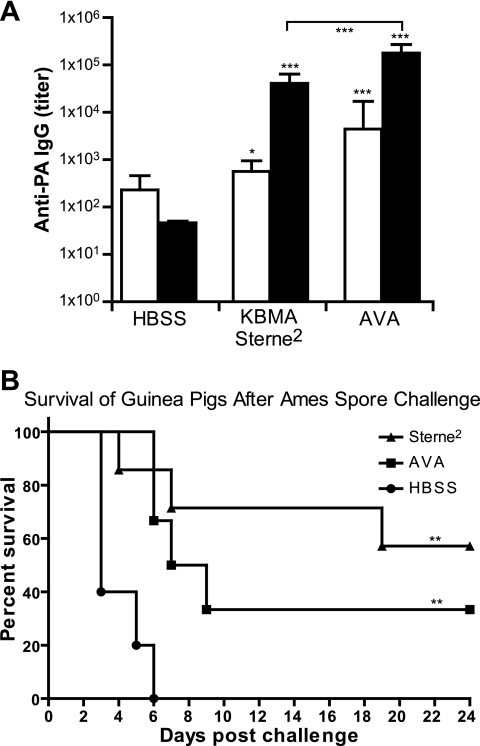
Guinea pig protection studies.
Female Hartley guinea pigs (Charles River), 10 to 12 animals per group, were immunized i.m. with 200 μl HBSS, KBMA Sterne2 (at 2 × 1010 particles/ml), or 200 μl AVA (BEI Resources). All animals were administered a boost vaccination 4 weeks later. For serum analysis, blood was drawn 2 weeks after the prime vaccination and 3 weeks after the boost vaccination. Four weeks after the boost vaccination, half the animals from each group were challenged by intranasal administration with 50 μl of either a 10-LD50 dose of 1.2 × 106 Ames spores (experimentally determined to be 1.35 ×106 CFU) or a 50-LD50 dose of 6 × 106 Ames spores (experimentally determined to be 7.4 × 106 CFU). Ames challenge studies were performed within a registered select agent animal biosafety level 3 facility at the University of Texas Medical Branch.
Statistics.
Analysis of survival data was carried out using the Kaplan-Meier method, and the log rank test was used to determine the statistical significance of observed survival differences using Prism software (GraphPad). For statistical analysis of anti-PA ELISA data, ln-transformed titers were analyzed using an unpaired t test with Welch's correction (allowing for unequal variances) using Prism software (GraphPad). One-tailed P values were reported for comparison of titers from vaccinated animals to the vehicle-only (HBSS) negative control animals, and two-tailed P values were calculated for comparisons between vaccinated groups. Unless otherwise indicated, analyses were compared with the HBSS negative control from the same time point. When multiple comparisons were performed on the same set of data, raw P values were reanalyzed to control for false-discovery or familywise error rates. For the preliminary screen (see Fig. 3A), the false-discovery rate was controlled at 0.05. For the analyses of the remainder of the ELISA data, the familywise error rate was controlled at 0.05 using the Hochberg step-up method. The multiple-comparison procedures were implemented using Stata Statistical Software version 10 (StataCorp).
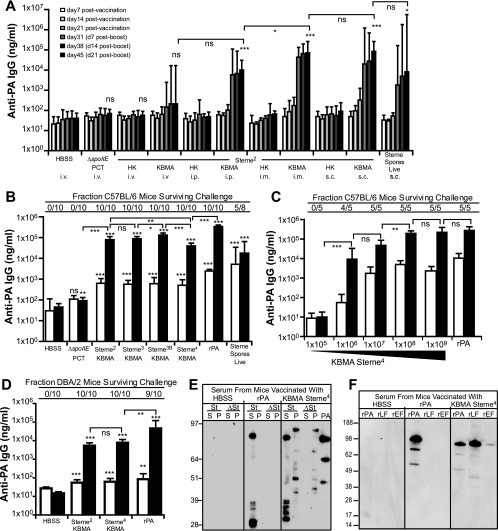
FIG. 3.
KBMA B. anthracis induces protective humoral immunity in mice. (A) Kinetics of the anti-PA response in BALB/c mice after different routes of administration. Five mice per group were vaccinated with 1 × 108 particles of KBMA or heat-killed Sterne2, 1 × 108 particles of ΔspoIIE inactivated with 1,000 nM S-59 and UVA (PCT), or 1 × 107 live Sterne spores on day 0 and day 21 by the indicated route: i.v., i.p., i.m., or s.c. Serum samples were taken from the mice every 7 days and analyzed for anti-PA IgG titers by ELISA. Day 45 titers that were significantly different from that of the negative control are indicated (ns, not significant; *, P < 0.05; **, P < 0.01; ***, P < 0.001), and statistical analyses between groups are indicated with brackets. The data are representative of two independent experiments. (B) KBMA B. anthracis vaccine candidates induce protective anti-PA responses in C57BL/6 mice. Ten mice per group were vaccinated i.m. with 1 × 108 particles of KBMA Sterne2, Sterne3, Sterne3B, or Sterne4; 1 × 108 particles of PCT ΔspoIIE; 1 × 105 live Sterne spores; or 10 μg rPA on day 0 and day 21. Two mice vaccinated with live Sterne spores died after the primary vaccination. Serum samples were obtained 3 days prior to (white bars) and 7 days after (black bars) the boost vaccination and were analyzed for anti-PA IgG titers by ELISA. All animals were challenged with 5 × 107 Sterne spores administered s.c., and the ratios of survivors to the number challenged are shown above the bars. (C) Dose response of KBMA Sterne4. C57BL/6 mice were vaccinated i.m. with the indicated doses of KBMA Sterne4 or 10 μg rPA on day 0 and day 21. Serum samples were obtained 3 days prior to (white bars) and 11 days after (black bars) the boost vaccination and analyzed for anti-PA IgG titers by ELISA. All animals were challenged s.c. with 5 × 107 Sterne spores, and the ratios of survivors to the number challenged are shown above the bars. (D) KBMA B. anthracis vaccine candidates induce anti-PA responses in C5-deficient DBA/2J mice. DBA/2J mice were vaccinated i.m. with HBSS, 1 × 108 KBMA particles of Sterne2 or Sterne4, or 10 μg rPA on day 0 and day 21. Serum samples were obtained 3 days prior to (white bars) and 7 days after (black bars) the boost vaccination and analyzed for anti-PA IgG titers by ELISA. Two weeks post-boost vaccination, the animals were challenged s.c. with 5e5 Sterne spores (∼500 times the LD50). (E) KBMA B. anthracis induces humoral responses against multiple B. anthracis proteins. Proteins from Sterne (St) and pXO1− Sterne (ΔSt) culture supernatants (S) or pellets (P) were separated by SDS-PAGE and immunoblotted with sera from C57BL/6 mice taken 7 days post-boost vaccination with HBSS, 10 μg rPA, or 1 × 108 particles of KBMA Sterne4. (F) KBMA B. anthracis induces humoral responses against multiple toxin components. Recombinant PA, LF, and EF were separated by SDS-PAGE and immunoblotted with sera from C57BL/6 mice taken 7 days post-boost vaccination with buffer (HBSS). In panels E and F, the numbers on the left are molecular sizes in kilodaltons.
RESULTS
Construction of vaccine candidates of B. anthracis.
Vaccine candidate strains were constructed by the introduction of sequential unmarked deletions and point mutations into the Sterne chromosome and pXO1 using allelic-exchange techniques (Table 1) (11). The Sterne strain was chosen as the background for our KBMA vaccine because it has been studied extensively and is an effective live-attenuated vaccine for livestock that does not form the antiphagocytic γDPGA capsule due to the absence of the pXO2 virulence plasmid. The Sterne strain does, however, form spores. Thus, in order to prepare a vaccine consisting entirely of photochemically killed bacteria, it was essential to construct an asporogenic strain of B. anthracis. The spoIIE gene encodes a transmembrane protein phosphatase required for the activation and release of the forespore-specific transcription factor sigma F and is required for sporulation of B. subtilis (5). We constructed in-frame deletions of the spoIIE coding sequence on the Sterne chromosome (ΔspoIIE) and also on the chromosome of a NER-deficient ΔuvrAB strain (7) to make a double-mutant vaccine candidate, known as Sterne2. Previously described inactivating substitution mutations were then introduced into cya and then the lef genes on the pXO1 virulence plasmid of the Sterne2 strain to produce the vaccine candidate strains Sterne3 and Sterne3B, respectively (10). The lef-inactivating-mutation was then introduced into Sterne3 to make the Sterne4 quadruple-mutant vaccine candidate strain. The genotypes of the constructed vaccine candidates are presented in Table 1.
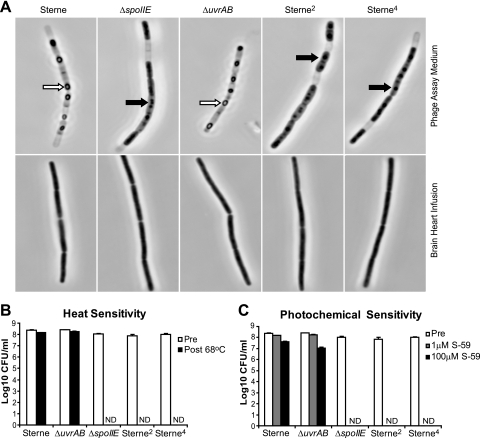
SpoIIE is required for spore formation in B. anthracis.
All vaccine candidate strains grew at rates identical to that of the parental Sterne strain (data not shown) with no morphological differences during vegetative growth in BHI culture (Fig. 1A). However, after being cultured for 16 h in phage assay medium (conditions that induced ∼70% spore formation of the parental strain), the ΔspoIIE mutants were unable to form phase-bright spores, remained sensitive to heat, and were completely inactivated with 1 or 100 μM S-59 psoralen (high-dose conditions) and UVA PCT (Fig. 1A, B, and C). As expected, Sterne and ΔuvrAB spores were highly resistant to heat and photochemical inactivation with S-59 and UVA (Fig. 1B and C). Under spore-inducing culture conditions, ΔspoIIE mutant strains underwent a morphological change characterized by a loss of phase-dense material over the surface of the bacilli and formation of foci of phase-dense material suggestive of an abortive attempt to sporulate, but at no time did these ΔspoIIE mutants form heat-resistant phase-bright spores (Fig. 1A). After longer-term cultivation in phage assay medium, the ΔspoIIE strains continued to lose phase-dense material and viability (data not shown). These data are the first demonstration that SpoIIE is required for sporulation in B. anthracis.
FIG. 1.
spoIIE is required for sporulation of B. anthracis. (A) ΔspoIIE mutants do not form phase-bright endospores. Cultures of B. anthracis were grown for 16 h in phage assay medium to induce sporulation (top row) or in BHI (bottom row) and were then fixed with 10% formalin and visualized by phase-contrast microscopy. White arrows indicate phase-bright spores; black arrows indicate phase-dense spores. (B) ΔspoIIE mutants are heat sensitive. B. anthracis strains were grown in phage assay medium for 16 h, serially diluted and plated for CFU (Pre), and then heated to 68°C for 30 min and plated (Post 68°C). For all ΔspoIIE strains (ΔspoIIE, Sterne2, and Sterne4), 10 ml of culture was plated for CFU, and none were detected (ND). (C) Spores of B. anthracis are resistant to photochemical inactivation. B. anthracis strains were grown in phage assay medium, serially diluted and plated for CFU (Pre), and then subjected to photochemical inactivation with 1 μM S-59 or 100 μM S-59 and 6.5 J/cm2 UVA light. Each plating was performed in triplicate, and the error bars represent the standard deviation within a representative experiment.
Asporogenic NER double mutants of B. anthracis are highly sensitive to photochemical inactivation.
To maximize the expression profiles and potencies of KBMA vaccines, it is essential to minimize the frequency of DNA cross-links by inactivating the bacteria with the lowest concentration of psoralen required to achieve complete inactivation (7). B. anthracis vaccine candidates were grown under vegetative culture conditions and exposed to various concentrations of S-59 and then inactivated with a UVA dose of 6.5 J/cm2. The majority of Sterne bacilli were killed at a dose of 1,000 nM S-59, but occasionally there were residual CFU that were resistant to high doses of S-59 and were also heat resistant (Fig. 2A and data not shown). These observations were likely due to stochastic formation of spores during vegetative growth, because the spoIIE mutant was inactivated with kinetics identical to those for the Sterne strain, with the exception that the asporogenic strain was reproducibly completely killed at a concentration of 1,000 nM S-59. As expected, the NER-deficient strains were much more sensitive to PCT, but because the ΔuvrAB mutant was capable of forming spores during vegetative growth, we were not able to consistently achieve full inactivation at any concentration of S-59 tested. In contrast, greater than 5 × 108 CFU/ml of the asporogenic NER-deficient strains (Sterne2 and Sterne4) were completely inactivated at a concentration of 50 nM S-59. Thus, in asporogenic bacteria, the ΔuvrAB deletion resulted in a 20-fold increase in sensitivity to inactivation by PCT.
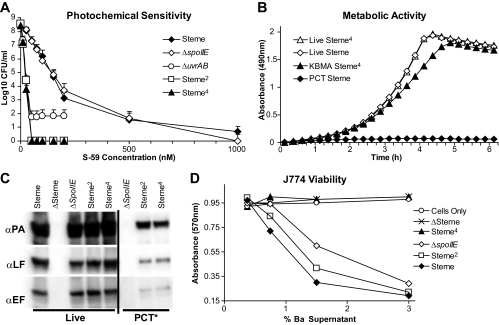
FIG. 2.
Increased sensitivity of ΔspoIIE ΔuvrAB strains to photochemical inactivation allows bacteria to retain metabolic activity and secrete critical antigens. (A) ΔspoIIE ΔuvrAB double mutants are exquisitely sensitive to PCT. S-59 was added to mid-log-phase cultures at the indicated concentrations for 1 h at 37°C, and then the cultures were illuminated with 6.5 J/cm2 UVA. The cultures were serially diluted and plated on BHI agar for enumeration of CFU. The symbols represent the mean titers from three independent experiments, and the error bars represent the standard deviations. (B) Photochemically killed ΔspoIIE ΔuvrAB strains retain a high degree of metabolic activity. Sterne or Sterne4 was grown in the presence of 1,000 nM or 50 nM S-59, respectively, for 1 h. The cultures were inactivated by exposure to 6.5 J/cm2 UVA or were not irradiated and then were serially diluted to 5 × 104 CFU per well and assayed for metabolic activity using an MTS assay at 37°C. (C) KBMA B. anthracis secretes critical antigens. Live or photochemically inactivated bacteria were transferred into R medium supplemented with 0.8% sodium bicarbonate to induce anthrax toxin production and incubated for 4.5 h at 37°C. The cell culture supernatants were precipitated with trichloroacetic acid, and culture supernatant equivalents were separated by SDS-PAGE and immunoblotted with anti-PA (αPA), anti-EF, or anti-LF monoclonal antibody. (D) Frozen vegetative cells (1 × 109 CFU) were incubated in R medium with 0.8% sodium bicarbonate for 2 h at 37°C. The culture filtrate was added directly to J774A.1 cell cultures for 3.5 h, at which time a 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide assay was used to determine the degree of metabolic activity of the cells. The data presented in panels B, C, and D are from representative experiments that were repeated at least twice.
Photochemically treated asporogenic NER mutants of B. anthracis are KBMA.
To determine whether the increase in sensitivity to photochemical inactivation was correlated with a higher degree of metabolic activity, we photochemically treated the Sterne parental strain or the asporogenic NER mutants with 1,000 nM or 50 nM S-59 (the lowest psoralen concentrations required for full inactivation of parental or NER-deficient strains, respectively) and measured the capacities of the bacteria to reduce the tetrazolium compound MTS to a formazan. There were no detectable CFU in either culture after PCT in these experiments. At physiological temperatures, the asporogenic NER-deficient vaccine candidate Sterne4 maintained metabolic activity that was comparable to that of live B. anthracis for greater than 5 h (Fig. 2B). In contrast, the parental Sterne strain demonstrated no detectable metabolic activity when treated with the minimal concentration of S-59 required to inactivate 100% of the bacteria, likely due to the increase in number of photochemical cross-links required to overwhelm the NER system. An essential feature of KBMA vaccines is their ability to continue to transcribe, translate, and secrete antigenic proteins post-PCT (7). Significantly, when the photochemically inactivated bacteria were induced to secrete virulence determinants (by transfer to media that contained sodium bicarbonate), the Sterne2 and Sterne4 strains were still able to secrete critical antigens, including PA, LF, and EF (Fig. 2C), whereas the photochemically inactivated ΔspoIIE strain with intact NER was not able to secrete detectable quantities of these antigens into the media. Together, these data demonstrate that abrogation of the NER pathway allows B. anthracis to maintain metabolic activity and antigen secretion after photochemical inactivation.
The Sterne4 vaccine candidate is nontoxinogenic and avirulent in mice.
We have demonstrated that ΔspoIIE ΔuvrAB mutant bacteria can maintain metabolic activity after being photochemically inactivated with low doses of S-59 and UVA light. However, a possible safety concern could be that the Sterne2 strain secretes active toxin components, and a single bacterium surviving PCT might grow and cause disease. The substitution of glutamine residues for lysine residues at positions 346 and 353 of EF [cya(K346/353Q)] prevented adenylate cyclase activity (29, 65) but had little effect on virulence when vegetative cells of Sterne3 were injected i.m. into highly susceptible DBA/2J mice (Table 1). DBA/2J mice carry a defect in the Hc locus, which encodes complement factor 5 (C5), and thus are highly susceptible to B. anthracis infection (60, 61). The substitution of alanine for histidine 686 in LF [lef(H686A)] abrogated metalloprotease activity (27) and rendered B. anthracis spores avirulent in mice (10). Culture filtrates of both the Sterne and Sterne2 strains contained toxin components that caused a dose-dependent decrease in the viability of J774A.1 cells (Fig. 2D). In contrast, the Sterne4 and pXO1− (ΔSterne) negative control did not produce culture filtrates that were toxic to J774A.1 cells. Importantly, the point mutations in EF and LF did not affect the levels of secretion of these proteins into culture supernatants compared to those of the native toxins (Fig. 2C). We next determined whether the reduction in toxinogenicity of Sterne4 measured in vitro was correlated with attenuated virulence in mice. Vegetative cells of the parental Sterne strain were delivered i.m., and the median lethal dose in C5-deficient DBA/2J mice was approximately 6 CFU (Table 1). In striking contrast, the Sterne4 strain was essentially avirulent, as no deaths were observed even at doses up to 7.4 × 108 CFU. This result demonstrated that the live Sterne4 vaccine candidate is attenuated by at least 8 log units. The attenuated virulence of Sterne4 was mostly attributable to the point mutation in the lef gene, as the LD50 of the EF-deficient Sterne3 strain was comparable to that of the parental Sterne strain.
Vaccination with KBMA B. anthracis induces potent humoral responses in mice.
The immune correlates of protection against pneumonic B. anthracis challenge are circulating antibodies that bind PA and neutralize LeTx (23, 43). We evaluated the abilities of KBMA B. anthracis vaccine candidates to elicit anti-PA antibodies in mice when administered through the i.v., i.p., s.c., or i.m. route. Highly resistant BALB/c mice were vaccinated with 1 × 108 particles (heat-killed or PCT vegetative cells) of KBMA Sterne2, heat-killed Sterne2, or photochemically inactivated ΔspoIIE, and the results were compared to those of immunization with 1 × 107 CFU live Sterne spores. The mice were vaccinated by a prime-and-boost regimen separated by 3 weeks. The levels of anti-PA IgG in serum were determined, using an anti-PA ELISA, from blood samples collected at 1-week intervals following each vaccination (Fig. 3A). As expected, there was no significant increase in the anti-PA titer after vaccination with buffer, heat-killed Sterne2, or PCT ΔspoIIE (i.e., with intact NER) after the prime or boost vaccination. Surprisingly, i.v. administration of KBMA Sterne2 did not induce a significant anti-PA response. However, within 1 week after the boost vaccination, there were significant increases in the anti-PA IgG titers in the groups vaccinated i.p., i.m., or s.c. with KBMA Sterne2. The highest titers of anti-PA IgG were observed 3 weeks after the boost vaccination in the groups immunized by the s.c. or i.m. route, and these titers were significantly higher than those for the groups immunized i.v. or i.p. but were not distinguishable from each other. Anti-PA titers in animals vaccinated s.c. with live Sterne spores were highly variable but trended higher over the 3 weeks following the boost vaccination, which was likely due to longer persistence of Sterne spores.
To determine which route of administration induced the highest titer of LeTx-neutralizing antibody, we compared the ability of serum collected 3 weeks after boost vaccination (day 45) to protect J774A.1 murine macrophage cells from recombinant LeTx challenge. Mice vaccinated i.m. with KBMA Sterne2 produced the highest levels of toxin-neutralizing antibody, with a reciprocal mean 50% neutralizing titer of 989. This titer was approximately 20-fold higher than that for i.v. administration (titer, 54), 4-fold higher than for s.c. administration (titer, 263), and, 2-fold higher than for s.c. administration (titer, 500) of live Sterne spores. These data, combined with the near equivalence between the i.m. and s.c. routes, as measured by the anti-PA IgG titer, led us to select the i.m. route for further studies.
Detoxified KBMA vaccine candidates provide protective immunity in mice.
The purified toxins of B. anthracis have immunomodulatory functions in vitro and in vivo (1, 3, 4, 14, 16, 40, 48, 54); however, the impact of the toxin's enzymatic activities on the ability of the host to mount a protective humoral response to B. anthracis is not known. While Brossier et al. (10) demonstrated that a genetically detoxified live vaccine is capable of inducing high-titer anti-PA responses, it was not possible to compare equivalent doses to the parental strain because the parental strain retained virulence in mice. Since KBMA vaccines are avirulent, we were able to compare equivalent doses of vaccine candidates expressing enzymatically active or inactive EF and/or LF (Sterne2, Sterne3, Sterne3B, and Sterne4) and to measure the effects of toxin activities on anti-PA responses and protection. Each KBMA vaccine candidate was formulated under identical conditions, and C57BL/6 mice were immunized twice with 1 × 108 particles of KBMA vaccine. ΔspoIIE mutant bacilli were photochemically inactivated with 1,000 nM S-59 and used as a negative control. Ten micrograms of rPA adsorbed to alhydrogel and 0.1 LD50 of live Sterne spores were used as positive controls. There were slight but significant increases in the anti-PA titer after vaccination with the photochemically inactivated ΔspoIIE mutant, suggesting a low level of residual activity. However, immunization with each of the KBMA vaccine strains induced dramatically higher levels of PA-specific IgG (P < 0.001). Of the KBMA vaccine candidates tested, the Sterne3B vaccine (expressing inactive LF) induced the highest titers, while Sterne4 (expressing inactive EF and LF) induced the lowest anti-PA IgG titers, which is consistent with the titers reported for live strains with the same point mutations (10) and could suggest that a functional EF may enhance humoral responses. However, in other studies, KBMA Sterne4 induced anti-PA titers that were equivalent to those for Sterne2 (Fig. 3D and data not shown). rPA-immunized mice had significantly higher titers than all of the KBMA-immunized animals, and mice vaccinated with live Sterne spores had comparable titers after the boost (despite receiving a dose of spores that resulted in 20% death).
Two weeks after a boost vaccination, mice were challenged s.c. with 20 LD50 Sterne spores. All mice vaccinated with KBMA B. anthracis vaccine candidates survived, regardless of whether the vaccine strains encoded functional or nonfunctional EF and/or LF. Animals vaccinated with rPA also survived lethal challenge. Surprisingly, only 63% of the mice that survived vaccination with live Sterne spores were protected against a subsequent lethal challenge with Sterne spores, which was significantly less protective than vaccination with KBMA vaccines (P < 0.05) but still more than vehicle alone (P < 0.001). None of the animals vaccinated with buffer or nonmetabolically active PCT ΔspoIIE mutant bacilli were afforded protection, although animals in the PCT ΔspoIIE cohort survived 1 day longer on average (P < 0.05). These results demonstrated that there is a requirement for the photochemically inactivated vaccines to be metabolically active in order to provide full protection, which requires abrogation of the NER pathway. These data also demonstrate that the functional activities of EdTx and LeTx do not negatively impact the ability of mice to mount a protective immune response after KBMA vaccination and suggest that the Sterne4 strain is an attractive vaccine candidate based on the decreased virulence of the live organism.
We then performed a titration of KBMA Stern4 immunization to determine the dose range that elicited protective immunity (Fig. 3C). Tenfold serial dilutions ranging from 1 × 109 to 1 × 105 particles of KBMA Sterne4 were administered i.m. to C57BL/6 mice, and the anti-PA titers were compared to those with 10 μg rPA. After a boost vaccination with 1 × 109 or 1 × 108 particles of KBMA Sterne4, the anti-PA IgG titers were comparable to those after rPA vaccination, but there was a significant decrease in anti-PA IgG titers at a10-fold-lower dose. After lethal s.c. challenge with Sterne spores, all mice that were vaccinated with rPA or ≥1 × 107 particles of KBMA Sterne4 survived, and 80% of the mice vaccinated with 1 × 106 particles of KBMA Sterne4 survived. Although there were no surviving mice in the group immunized with 1 × 105 KBMA particles, there was a single-day delay in the mean time to death compared with animals vaccinated with buffer alone (P < 0.05). These data demonstrate that there was a 3-log-unit dose range of KBMA B. anthracis vaccine that provided 100% protection in mice that correlated with anti-PA responses.
C5-deficient DBA/2J mice are highly susceptible to B. anthracis infection, and the animals die in a toxin-dependent manner when challenged with low doses of the Sterne strain, with pathology that resembles that of encapsulated B. anthracis challenge in rabbits and primates (21). When mice were vaccinated twice with KBMA Sterne2 or Sterne4, we were able to measure a greater-than-1,000-fold increase in the anti-PA IgG titer (Fig. 3D) and a 10,000-fold increase in the anti-PA titer after vaccination with rPA. The immunized mice were challenged via the s.c. route 2 weeks after boost vaccination with 500 times the LD50 of Sterne spores. Despite their extreme sensitivity to B. anthracis, 100% of the KBMA Sterne2- or Sterne4-immunized DBA/2J mice were protected (Fig. 3D). Interestingly, even though all animals vaccinated with rPA had high anti-PA titers, only 90% of them were protected against the lethal challenge.
While the difference in protection between the KBMA and rPA vaccines was not statistically significant, it may reflect factors other than anti-PA titers that may have contributed to protection. To begin to address this possibility, we compared the breadths of humoral immunity elicited in response to immunization with KBMA and rPA vaccines. Samples of B. anthracis grown in the presence of sodium bicarbonate to induce anthrax toxin production were prepared, and then secreted proteins and proteins from whole bacterial lysates were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a nitrocellulose membrane. We evaluated the breadths of vaccine-induced antibodies specific for the fractionated B. anthracis proteins by blotting the membrane with serum from immunized C57BL/6 mice. Mice immunized with rPA adsorbed to alhydrogel elicited antibodies that recognized PA and a few lower-molecular-weight species that were most likely degradation products of PA (Fig. 3E). These sera did not react with any bacterium-associated proteins from Sterne or ΔSterne. In contrast, sera from mice vaccinated with KBMA Sterne4 contained antibodies that recognized numerous bacterium-associated proteins from both the Sterne and ΔSterne strains. Interestingly, the KBMA-vaccinated animals elicited antibodies that detected numerous secreted bacterial proteins from the Sterne strain but none from the ΔSterne strain, highlighting the immunodominance of pX01-derived proteins. Unlike rPA vaccination, sera from the KBMA-vaccinated animals also induced antibodies that recognized recombinant PA, LF, and EF proteins (Fig. 3F). These data provided strong evidence that vaccination with KBMA B. anthracis vaccines induced a humoral response of substantially greater breadth than that elicited by rPA-based vaccines.
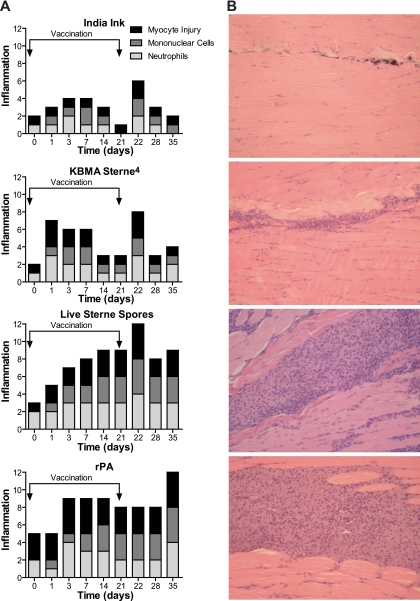
Vaccination with KBMA B. anthracis induces less inflammation in muscle than adjuvanted rPA.
AVA is administered s.c. and causes injection site reactions in approximately 28% of vaccinees, while systemic and severe reactions occur at lower rates (1 to 4%) (38, 50). The rPA102 vaccine is injected i.m., and when these vaccines were directly compared, significantly fewer adverse events were reported with rPA102 than with AVA (19). We compared the degree of inflammation at the injection site in mouse muscle following immunization with KBMA vaccines or rPA adjuvanted with alhydrogel (Fig. 4). Injection sites were evaluated blindly for severity of inflammation based on the presence of neutrophils and mononuclear cells or myocyte damage. Inflammation in the KBMA-vaccinated group peaked 1 day after the prime vaccination and was indistinguishable from that with HBSS injected after 1 week. Inflammation peaked again 1 day after a boost vaccination and waned rapidly thereafter. For animals vaccinated with live Sterne spores, inflammation increased progressively until day 14, remained high until day 21, and peaked again 1 day later, after the boost vaccination. With rPA and alhydrogel, inflammation peaked 3 days after the primary vaccination and remained high throughout the course of the experiment, with a peak of inflammation on day 35 (2 weeks postboost). Inflammation induced by KBMA Sterne2 was indistinguishable from that with Sterne4 with the exception that there was slightly increased inflammation after immunization with Sterne2 at day 28 (not shown). These data demonstrated that the degree of inflammation induced by vaccination with KBMA B. anthracis was less pronounced and persisted for a shorter time than that after vaccination with rPA and alhydrogel or live Sterne spores.
FIG. 4.
KBMA vaccine induces less inflammation than rPA and alhydrogel. BALB/c mice were vaccinated on day 0 and day 21 with HBSS containing a trace amount of India ink (A), 1 × 108 KBMA Sterne4 vegetative cells (B), 1 × 107 live Sterne spores (C), or 10 μg rPA (D). Individual mice were sacrificed at 2 h (day zero) and 1, 3, 5, 7, 14, and 21 days after the prime vaccination and 1, 7, and 14 days after the boost vaccination. The quadriceps muscle was dissected and stained with hematoxylin and eosin. (A) The severity of inflammation was scored based on three parameters: infiltration of neutrophils (acute cells) and mononuclear cells (chronic cells) and myocyte damage (0 = normal; 1 = minimal; 2 = mild; 3 = moderate; 4 = severe). Thus, total inflammation scores are represented on a scale of 0 to 12. (B) Stained sections from day 35 muscles (14 days postboost) were visualized by transmitted-light microscopy.
Vaccination with KBMA B. anthracis protects rabbits from lethal bronchial instillation challenge with Ames spores.
While mice can be used to determine the immunogenicity of vaccine candidates, they are a poor model of protection against encapsulated strains of B. anthracis (22, 60). A rabbit model of pulmonary anthrax has been developed because the pathology of the disease caused by virulent encapsulated B. anthracis resembles that in nonhuman primates and humans (17, 66). We evaluated the ability of KBMA Sterne4 vaccine to confer protective immunity in rabbits against a lethal bronchial-instillation challenge with spores of the fully virulent Ames strain of B. anthracis (Fig. 5). Rabbits were vaccinated i.m. two times, separated by 4 weeks, with 500 μl of AVA or three different dose levels of KBMA Sterne4 (5 ×108, 2 × 109, or 1 × 1010 particles) with the same prime-boost immunization regimen. The circulating anti-PA IgG titer and the levels of LeTx-neutralizing activity in serum were measured, and the animals were challenged with a lethal dose of Ames spores 4 weeks after the boost vaccination. All three doses of KBMA Sterne4 induced robust anti-PA and toxin-neutralizing titers (Fig. 5A and B). The anti-PA and toxin-neutralizing titers elicited by AVA vaccination were approximately 10-fold higher than for KBMA vaccination after the boost. Rabbits immunized with all three dose levels of KBMA vaccine or with AVA were completely protected against a pulmonary Ames spore challenge that was 131 times greater than the LD50 (Fig. 5C). We have also observed that rabbits vaccinated twice with109 KBMA Sterne2 and exposed to doses up to 9.8 × 108 Ames spores (140,000 times the LD50) were 100% protected (data not shown). These data demonstrate that while AVA induced higher-titer anti-PA responses, KBMA B. anthracis afforded complete protective immunity in rabbits against a vigorous challenge.
FIG. 5.
Vaccination with KBMA Sterne4 protects rabbits from a lethal pulmonary Ames spore challenge. New Zealand White rabbits were vaccinated i.m. on day 0 and day 28 with HBSS, KBMA Sterne4, or 500 μl AVA. (A) Serum samples were obtained 14 days prior to and 21 days after the boost vaccination (black bars) and analyzed for anti-PA IgG titers by ELISA. (B) A toxin-neutralizing antibody assay was performed on pooled samples from the same animals. (C) Four weeks after the boost vaccination, all animals were challenged with 9.20 × 105 Ames spores (131 times the LD50) via bronchoscope instillation, and survival was monitored for 2 weeks after challenge. The data are representative of three independent rabbit challenge studies. The error bars represent the 95% confidence interval. ***, P < 0.001; ns, not significant.
Vaccination with KBMA B. anthracis protects guinea pigs from lethal intranasal Ames spore challenge.
Guinea pigs have also been utilized as a model for anthrax protection studies. Guinea pigs are less consistently protected by AVA vaccination (17) but appear to be more completely protected by live Sterne spore vaccination (36). We evaluated the ability of KBMA Sterne2 vaccine to confer protective immunity in guinea pigs against lethal intranasal challenge with Ames spores. Hartley guinea pigs were vaccinated i.m. in a 4-week prime-and-boost regimen with 200 μl of AVA or 4 × 109 particles of KBMA Sterne2. As in rabbits, AVA induced anti-PA titers that were significantly higher than in KBMA Sterne2-immunized animals (Fig. 6A). Anti-PA responses induced by vaccination with Sterne2 and Sterne4 vaccines in guinea pigs were indistinguishable (data not shown). Upon challenge with 50 times the intranasal LD50 of Ames spores, 33% of the animals vaccinated with AVA survived, and 50% of the animals vaccinated with KBMA B. anthracis survived (Fig. 6B). The survival benefit, while incomplete, was statistically significant compared with vehicle alone (P < 0.01). The observed survival difference between the KBMA and AVA groups was not statistically significant. Similar results (incomplete protection that was not statistically different between AVA and KBMA) were also observed when guinea pigs were challenged with 10 times the LD50 of Ames spores (data not shown). These data demonstrated that KBMA B. anthracis vaccines protected against a lethal Ames spore challenge even in an animal model in which the correlates of protection are not as well established as in rabbits. Collectively, the vaccine potency studies conducted in this investigation demonstrate that KBMA B. anthracis vaccines confer significant protective immunity against lethal B. anthracis challenge in three animal species and elicit antibodies against the known correlate of protection (PA), as well as other bacterial determinants.
FIG. 6.
Vaccination with KBMA Sterne4 protects guinea pigs from a lethal intranasal Ames spore challenge. Hartley guinea pigs were vaccinated i.m. on day 0 and day 28 with HBSS, 4 × 109 particles of KBMA Sterne2, or 200 μl AVA. (A) Serum samples were obtained 14 days prior to (white bars) and 21 days after the boost vaccination (black bars) and analyzed for anti-PA IgG titers by ELISA. (B) Four weeks after the boost vaccination, the animals were challenged intranasally with 1.48 × 108 Ames spores. Survival after vaccination with Sterne2 or AVA was statistically different from the HBSS control (**, P < 0.01) but not statistically different from each other. The data are representative of two independent guinea pig challenge studies. The error bars represent the 95% confidence interval. *, P < 0.05; ***, P < 0.001.
DISCUSSION
In this study, we demonstrated that mutant B. anthracis strains engineered to be asporogenic and NER deficient are exquisitely sensitive to photochemical inactivation with S-59 psoralen and UVA light. The inactivated vaccine candidates maintained metabolic activity and secreted PA, LF, and EF antigens. While all of the KBMA vaccine strains were avirulent in mice, the potential safety profile of the vaccine was improved by mutating EF and LF toxin components, which rendered the live (i.e., not photochemically inactivated) vaccine strain avirulent but retained the antigenicity of these toxins. After an immunization regimen consisting of a prime and a single boost in mice, rabbits, and guinea pigs, KBMA B. anthracis vaccines elicited potent toxin-neutralizing and humoral antibody responses against multiple bacterial proteins. The degree to which this broad spectrum of antigens contributes to the protective response has yet to be determined, but vaccination with KBMA B. anthracis provided 100% protection in mice against a lethal Sterne spore challenge and in rabbits against a lethal Ames spore challenge. Together, these data demonstrate that KBMA B. anthracis vaccines provide a broad and protective immune response. The protection observed was similar to that of other, previously described vaccines: rPA, live Sterne spores, and the licensed anthrax vaccine AVA. Neither AVA nor KBMA B. anthracis provided full protection against a lethal Ames spore challenge in guinea pigs. AVA has been shown to provide incomplete protection against Ames spore challenge in this model, but for unknown reasons, AVA is more protective against other challenge strains, such as Vollum1b (17, 66). Comparison of KBMA B. anthracis and AVA in a challenge model using such a strain may allow a better comparison of the protective efficacies of these vaccines.
Numerous vaccination strategies have been developed to prevent B. anthracis infection. To date, the only vaccine licensed for human use in the United States is AVA, which is composed of B. anthracis culture filtrate from a toxinogenic strain that is adsorbed to aluminum hydroxide as an adjuvant. While AVA is a potent stimulator of toxin-neutralizing immunity, it is poorly characterized and frequently reactogenic (38, 50). Additionally, the results from the first clinical trial with rPA102 demonstrated that it has a higher rate of systemic reactogenicity than AVA (19). The reactogenicity of these vaccines is likely due to the use of aluminum hydroxide as an adjuvant. KBMA vaccines may not require adjuvants because the metabolically active bacteria produce a repertoire of immunomodulatory molecules sufficient to induce a protective immune response. The decrease in the severity and duration of inflammation in the muscles of mice vaccinated with KBMA B. anthracis compared to mice vaccinated with rPA provides early evidence that the KBMA vaccine may induce a low level of reactogenicity. There are numerous other anthrax vaccines in development that combine rPA with adjuvants other than aluminum hydroxide that may also reduce the reactogenicity of rPA-based vaccines, but the reactogenicities of these vaccines have not been described (25, 45, 55, 63).
While PA-targeted antibodies provide protection in rabbit and nonhuman primate models, B. anthracis pathogenesis is not solely a function of anthrax toxins. This point is substantiated by observations that anti-PA responses do not always correlate with protection in all animal models. Anthrax vaccines that elicit immune responses against multiple antigenic targets may be conceptually desirable for human development. The γDPGA capsule is also a major virulence determinant. In mice, encapsulated B. anthracis strains that do not express PA are as virulent as wild-type strains, and anti-PA responses provide no protection against encapsulated strains (22, 59). The presence of capsule and other less well characterized virulence determinants raise concern about relying solely on an antibody response against a single protective antigen. In a biodefense setting, it is important to consider that weaponized strains could be engineered to subvert a vaccine based on a single antigen. Under these extreme circumstances, an rPA-based vaccine may provide less protective benefit. In order to provide the highest degree of immunity against potentially weaponized strains of B. anthracis, however, live or KBMA whole-cell vaccines may enhance protection due to induction of a broader repertoire of immune responses against B. anthracis antigens. The live Sterne strain is commonly used in livestock to protect against environmental exposure to B. anthracis spores, but the organism secretes active toxins, remains highly virulent in mice, and is reactogenic. Brossier et al. (10) have developed EF- and LF-inactive live vaccine strains that provide modest protective immunity against a lethal dose of spores of a toxinogenic encapsulated strain in mice. This live-attenuated strain can be formulated as a spore, and thus, it can be prepared as a highly stable vaccine. However, the bacteria can still grow and therefore could potentially cause disease in an immunocompromised host. This potential for infection is overcome by the use of KBMA vaccines.
For continued development, possible practical limitations of KBMA B. anthracis vaccines may need to be addressed. To achieve complete photochemical inactivation, the bacteria must be asporogenic, making the vaccine inherently less stable than spore-based vaccines. While loss of stability can be overcome by storage at −80°C, this is not a suitable formulation for stockpiling. We are currently in the process of developing dried formulations of KBMA B. anthracis vaccine that maintain metabolic activity after storage at elevated temperatures. Additionally, the prototype KBMA vaccine does not encode spore antigens, which may contribute to protection (9, 18). Another factor that may contribute to protective immunity is anticapsule immunity (28). It has been demonstrated that conjugation of γDPGA to proteins (including PA) induces high anticapsule titers (45, 63), but these protein conjugates are still limited in the number of antigens that are presented. Both AVA and KBMA vaccines failed to protect against a lethal atoxigenic encapsulated challenge (data not shown). Since the KBMA B. anthracis vaccine is attenuated genetically by inactivation of the toxins and by photochemcial cross-linking of the DNA, it would be possible to produce a KBMA B. anthracis vaccine that is encapsulated (6), but addition of pXO2 it would make it a select agent and unlikely to be acceptable for development. However, chemical conjugation of capsular polypeptides to KBMA vaccines could overcome this limitation but would complicate manufacturing processes.
We have previously demonstrated that KBMA L. monocytogenes vaccine elicits potent protective cell-mediated immunity (7). In this study, we demonstrated that KBMA B. anthracis vaccines elicit potent protective humoral immunity. Together, these studies have demonstrated that bacterial pathogens formulated as KBMA vaccines maintain the ability to induce the protective response in a manner that is similar to that of the live organism. This does not hold true for vaccines killed by traditional methods, primarily because they lose their ability to secrete key determinants of protection (e.g., listeriolysin O or PA) (2). These studies suggest that the KBMA vaccine strategy is broadly applicable to bacterial pathogens and can be applied to diseases for which the correlates of immunity are unknown.
Acknowledgments
This work was supported by Public Health Service grant 1 U01 AI061199 and also by the Small Animal Models for Selected Pathogens-Anthrax Contract number N01-AI-30065 from the National Institutes of Health.
We thank Ian Glomski for numerous protocols, insightful discussions, and critical review of the manuscript. We thank Kristen Debord, Melissa Drysdale, Carl Hanson, Terry Koehler, Tam Mignot, and Pete Lauer for their advice and counsel. We thank Kathryn Bush, Jennifer Pawlik, Tony Garcia, and Steve Killian for assistance with animal studies and Jinous Bayat, David Chen, Margaret Dahlgren, Melissa Drysdale, Betsy Donnelly, Ellyn Shocron, and Hilde Stubal for technical assistance. We thank Maureen Lahiff for assistance with statistical analysis.
T. W. Dubensky, Jr., W. Liu, W. Luckett, and J. Skoble are employees of Anza Therapeutics Inc., which owns intellectual property covering the compositions and methods described in the article. In addition, Anza employees hold stock and/or stock options in the company. D.A.P. consults for and has a financial interest in Anza Therapeutics. Y. Gao is an employee and holder of stock and/or stock options in Cerus Corporation, which is an Anza shareholder. The remaining authors have no known financial interest in Anza or Cerus.
Editor: S. R. Blanke
Footnotes
Published ahead of print on 21 January 2009.
REFERENCES
- 1.Agrawal, A., J. Lingappa, S. H. Leppla, S. Agrawal, A. Jabbar, C. Quinn, and B. Pulendran. 2003. Impairment of dendritic cells and adaptive immunity by anthrax lethal toxin. Nature 424329-334. [DOI] [PubMed] [Google Scholar]
- 2.Bahjat, K. S., W. Liu, E. E. Lemmens, S. P. Schoenberger, D. A. Portnoy, T. W. Dubensky, Jr., and D. G. Brockstedt. 2006. Cytosolic entry controls CD8+-T-cell potency during bacterial infection. Infect. Immun. 746387-6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baldari, C. T., F. Tonello, S. R. Paccani, and C. Montecucco. 2006. Anthrax toxins: a paradigm of bacterial immune suppression. Trends Immunol. 27434-440. [DOI] [PubMed] [Google Scholar]
- 4.Banks, D. J., S. C. Ward, and K. A. Bradley. 2006. New insights into the functions of anthrax toxin. Exp. Rev. Mol. Med. 81-18. [DOI] [PubMed] [Google Scholar]
- 5.Barak, I., and P. Youngman. 1996. SpoIIE mutants of Bacillus subtilis comprise two distinct phenotypic classes consistent with a dual functional role for the SpoIIE protein. J. Bacteriol. 1784984-4989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourgogne, A., M. Drysdale, S. G. Hilsenbeck, S. N. Peterson, and T. M. Koehler. 2003. Global effects of virulence gene regulators in a Bacillus anthracis strain with both virulence plasmids. Infect. Immun. 712736-2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brockstedt, D. G., K. S. Bahjat, M. A. Giedlin, W. Liu, M. Leong, W. Luckett, Y. Gao, P. Schnupf, D. Kapadia, G. Castro, J. Y. Lim, A. Sampson-Johannes, A. A. Herskovits, A. Stassinopoulos, H. G. Bouwer, J. E. Hearst, D. A. Portnoy, D. N. Cook, and T. W. Dubensky, Jr. 2005. Killed but metabolically active microbes: a new vaccine paradigm for eliciting effector T-cell responses and protective immunity. Nat. Med. 11853-860. [DOI] [PubMed] [Google Scholar]
- 8.Brockstedt, D. G., M. A. Giedlin, M. L. Leong, K. S. Bahjat, Y. Gao, W. Luckett, W. Liu, D. N. Cook, D. A. Portnoy, and T. W. Dubensky, Jr. 2004. Listeria-based cancer vaccines that segregate immunogenicity from toxicity. Proc. Natl. Acad. Sci. USA 10113832-13837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brossier, F., M. Levy, and M. Mock. 2002. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 70661-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brossier, F., M. Weber-Levy, M. Mock, and J. C. Sirard. 2000. Role of toxin functional domains in anthrax pathogenesis. Infect. Immun. 681781-1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Camilli, A., L. G. Tilney, and D. A. Portnoy. 1993. Dual roles of plcA in Listeria monocytogenes pathogenesis. Mol. Microbiol. 8143-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cataldi, A., E. Labruyere, and M. Mock. 1990. Construction and characterization of a protective antigen-deficient Bacillus anthracis strain. Mol. Microbiol. 41111-1117. [DOI] [PubMed] [Google Scholar]
- 13.Chabot, D. J., A. Scorpio, S. A. Tobery, S. F. Little, S. L. Norris, and A. M. Friedlander. 2004. Anthrax capsule vaccine protects against experimental infection. Vaccine 2343-47. [DOI] [PubMed] [Google Scholar]
- 14.Crawford, M. A., C. V. Aylott, R. W. Bourdeau, and G. M. Bokoch. 2006. Bacillus anthracis toxins inhibit human neutrophil NADPH oxidase activity. J. Immunol. 1767557-7565. [DOI] [PubMed] [Google Scholar]
- 15.Duesbery, N. S., C. P. Webb, S. H. Leppla, V. M. Gordon, K. R. Klimpel, T. D. Copeland, N. G. Ahn, M. K. Oskarsson, K. Fukasawa, K. D. Paull, and G. F. Vande Woude. 1998. Proteolytic inactivation of MAP-kinase-kinase by anthrax lethal factor. Science 280734-737. [DOI] [PubMed] [Google Scholar]
- 16.Fang, H., L. Xu, T. Y. Chen, J. M. Cyr, and D. M. Frucht. 2006. Anthrax lethal toxin has direct and potent inhibitory effects on B cell proliferation and immunoglobulin production. J. Immunol. 1766155-6161. [DOI] [PubMed] [Google Scholar]
- 17.Fellows, P. F., M. K. Linscott, B. E. Ivins, M. L. Pitt, C. A. Rossi, P. H. Gibbs, and A. M. Friedlander. 2001. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine 193241-3247. [DOI] [PubMed] [Google Scholar]
- 18.Glomski, I. J., J. P. Corre, M. Mock, and P. L. Goossens. 2007. Cutting edge: IFN-gamma-producing CD4 T lymphocytes mediate spore-induced immunity to capsulated Bacillus anthracis. J. Immunol. 1782646-2650. [DOI] [PubMed] [Google Scholar]
- 19.Gorse, G. J., W. Keitel, H. Keyserling, D. N. Taylor, M. Lock, K. Alves, J. Kenner, L. Deans, and M. Gurwith. 2006. Immunogenicity and tolerance of ascending doses of a recombinant protective antigen (rPA102) anthrax vaccine: a randomized, double-blinded, controlled, multicenter trial. Vaccine 245950-5959. [DOI] [PubMed] [Google Scholar]
- 20.Green, B. D., L. Battisti, T. M. Koehler, C. B. Thorne, and B. E. Ivins. 1985. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 49291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harvill, E. T., G. Lee, V. K. Grippe, and T. J. Merkel. 2005. Complement depletion renders C57BL/6 mice sensitive to the Bacillus anthracis Sterne strain. Infect. Immun. 734420-4422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heninger, S., M. Drysdale, J. Lovchik, J. Hutt, M. F. Lipscomb, T. M. Koehler, and C. R. Lyons. 2006. Toxin-deficient mutants of Bacillus anthracis are lethal in a murine model for pulmonary anthrax. Infect. Immun. 746067-6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hering, D., W. Thompson, J. Hewetson, S. Little, S. Norris, and J. Pace-Templeton. 2004. Validation of the anthrax lethal toxin neutralization assay. Biologicals 3217-27. [DOI] [PubMed] [Google Scholar]
- 24.Horton, R. M., Z. L. Cai, S. N. Ho, and L. R. Pease. 1990. Gene splicing by overlap extension: tailor-made genes using the polymerase chain reaction. BioTechniques 8528-535. [PubMed] [Google Scholar]
- 25.Huang, J., J. A. Mikszta, M. S. Ferriter, G. Jiang, N. G. Harvey, B. Dyas, C. J. Roy, R. G. Ulrich, and V. J. Sullivan. 2007. Intranasal administration of dry powder anthrax vaccine provides protection against lethal aerosol spore challenge. Hum. Vaccin. 390-93. [DOI] [PubMed] [Google Scholar]
- 26.Ivins, B. E., M. L. Pitt, P. F. Fellows, J. W. Farchaus, G. E. Benner, D. M. Waag, S. F. Little, G. W. Anderson, Jr., P. H. Gibbs, and A. M. Friedlander. 1998. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine 161141-1148. [DOI] [PubMed] [Google Scholar]
- 27.Klimpel, K. R., N. Arora, and S. H. Leppla. 1994. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol. Microbiol. 131093-1100. [DOI] [PubMed] [Google Scholar]
- 28.Kozel, T. R., W. J. Murphy, S. Brandt, B. R. Blazar, J. A. Lovchik, P. Thorkildson, A. Percival, and C. R. Lyons. 2004. mAbs to Bacillus anthracis capsular antigen for immunoprotection in anthrax and detection of antigenemia. Proc. Natl. Acad. Sci. USA 1015042-5047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Labruyere, E., M. Mock, W. K. Surewicz, H. H. Mantsch, T. Rose, H. Munier, R. S. Sarfati, and O. Barzu. 1991. Structural and ligand-binding properties of a truncated form of Bacillus anthracis adenylate cyclase and of a catalytically inactive variant in which glutamine substitutes for lysine-346. Biochemistry 302619-2624. [DOI] [PubMed] [Google Scholar]
- 30.Lankowski, A. J., and E. L. Hohmann. 2007. Killed but metabolically active Salmonella typhimurium: application of a new technology to an old vector. J. Infect. Dis. 1951203-1211. [DOI] [PubMed] [Google Scholar]
- 31.Leppla, S. H. 1982. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc. Natl. Acad. Sci. USA 793162-3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leverone, M. R., T. C. Owen, F. S. Tieder, G. J. Stewart, and D. V. Lim. 1996. Resting-cell dehydrogenase assay measuring a novel water-soluble formazan detects catabolic differences among cells. J. Microbiol. Methods 2549-55. [Google Scholar]
- 33.Lin, L., D. N. Cook, G. P. Wiesehahn, R. Alfonso, B. Behrman, G. D. Cimino, L. Corten, P. B. Damonte, R. Dikeman, K. Dupuis, Y. M. Fang, C. V. Hanson, J. E. Hearst, C. Y. Lin, H. F. Londe, K. Metchette, A. T. Nerio, J. T. Pu, A. A. Reames, M. Rheinschmidt, J. Tessman, S. T. Isaacs, S. Wollowitz, and L. Corash. 1997. Photochemical inactivation of viruses and bacteria in platelet concentrates by use of a novel psoralen and long-wavelength ultraviolet light. Transfusion 37423-435. [DOI] [PubMed] [Google Scholar]
- 34.Little, S. F., B. E. Ivins, P. F. Fellows, M. L. Pitt, S. L. Norris, and G. P. Andrews. 2004. Defining a serological correlate of protection in rabbits for a recombinant anthrax vaccine. Vaccine 22422-430. [DOI] [PubMed] [Google Scholar]
- 35.Little, S. F., B. E. Ivins, W. M. Webster, P. F. Fellows, M. L. Pitt, S. L. Norris, and G. P. Andrews. 2006. Duration of protection of rabbits after vaccination with Bacillus anthracis recombinant protective antigen vaccine. Vaccine 242530-2536. [DOI] [PubMed] [Google Scholar]
- 36.Little, S. F., and G. B. Knudson. 1986. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect. Immun. 52509-512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Makino, S., I. Uchida, N. Terakado, C. Sasakawa, and M. Yoshikawa. 1989. Molecular characterization and protein analysis of the cap region, which is essential for encapsulation in Bacillus anthracis. J. Bacteriol. 171722-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McNeil, M. M., I. S. Chiang, J. T. Wheeling, and Y. Zhang. 2007. Short-term reactogenicity and gender effect of anthrax vaccine: analysis of a 1967-1972 study and review of the 1955-2005 medical literature. Pharmacoepidemiol. Drug Saf. 16259-274. [DOI] [PubMed] [Google Scholar]
- 39.Mock, M., E. Labruyere, P. Glaser, A. Danchin, and A. Ullmann. 1988. Cloning and expression of the calmodulin-sensitive Bacillus anthracis adenylate cyclase in Escherichia coli. Gene 64277-284. [DOI] [PubMed] [Google Scholar]
- 40.Paccani, S. R., F. Tonello, R. Ghittoni, M. Natale, L. Muraro, M. M. D'Elios, W. J. Tang, C. Montecucco, and C. T. Baldari. 2005. Anthrax toxins suppress T lymphocyte activation by disrupting antigen receptor signaling. J. Exp. Med. 201325-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Peterson, J. W., J. E. Comer, W. B. Baze, D. M. Noffsinger, A. Wenglikowski, K. G. Walberg, J. Hardcastle, J. Pawlik, K. Bush, J. Taormina, S. Moen, J. Thomas, B. M. Chatuev, L. Sower, A. K. Chopra, L. R. Stanberry, R. Sawada, W. W. Scholz, and J. Sircar. 2007. Human monoclonal antibody AVP-21D9 to protective antigen reduces dissemination of the Bacillus anthracis Ames strain from the lungs in a rabbit model. Infect. Immun. 753414-3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Phipps, A. J., C. Premanandan, R. E. Barnewall, and M. D. Lairmore. 2004. Rabbit and nonhuman primate models of toxin-targeting human anthrax vaccines. Microbiol. Mol. Biol. Rev. 68617-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pitt, M. L., S. F. Little, B. E. Ivins, P. Fellows, J. Barth, J. Hewetson, P. Gibbs, M. Dertzbaugh, and A. M. Friedlander. 2001. In vitro correlate of immunity in a rabbit model of inhalational anthrax. Vaccine 194768-4773. [DOI] [PubMed] [Google Scholar]
- 44.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27493. [Google Scholar]
- 45.Rhie, G. E., M. H. Roehrl, M. Mourez, R. J. Collier, J. J. Mekalanos, and J. Y. Wang. 2003. A dually active anthrax vaccine that confers protection against both bacilli and toxins. Proc. Natl. Acad. Sci. USA 10010925-10930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ristroph, J. D., and B. E. Ivins. 1983. Elaboration of Bacillus anthracis antigens in a new, defined culture medium. Infect. Immun. 39483-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Robertson, D. L., and S. H. Leppla. 1986. Molecular cloning and expression in Escherichia coli of the lethal factor gene of Bacillus anthracis. Gene 4471-78. [DOI] [PubMed] [Google Scholar]
- 48.Rossi Paccani, S., F. Tonello, L. Patrussi, N. Capitani, M. Simonato, C. Montecucco, and C. T. Baldari. 2007. Anthrax toxins inhibit immune cell chemotaxis by perturbing chemokine receptor signalling. Cell Microbiol. 9924-929. [DOI] [PubMed] [Google Scholar]
- 49.Sancar, A., and G. B. Sancar. 1988. DNA repair enzymes. Annu. Rev. Biochem. 5729-67. [DOI] [PubMed] [Google Scholar]
- 50.Sever, J. L., A. I. Brenner, A. D. Gale, J. M. Lyle, L. H. Moulton, B. J. Ward, and D. J. West. 2004. Safety of anthrax vaccine: an expanded review and evaluation of adverse events reported to the Vaccine Adverse Event Reporting System (VAERS). Pharmacoepidemiol. Drug Saf. 13825-840. [DOI] [PubMed] [Google Scholar]
- 51.Shlyakhov, E. N., and E. Rubinstein. 1994. Human live anthrax vaccine in the former USSR. Vaccine 12727-730. [DOI] [PubMed] [Google Scholar]
- 52.Sterne, M. 1939. The use of anthrax vaccines prepared from avirulent (uncapsulated) varients of Bacillus anthracis. Onderstepoort J. Vet. Sci. Anim. Ind. 13307-312. [Google Scholar]
- 53.Tippetts, M. T., and D. L. Robertson. 1988. Molecular cloning and expression of the Bacillus anthracis edema factor toxin gene: a calmodulin-dependent adenylate cyclase. J. Bacteriol. 1702263-2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tournier, J. N., A. Quesnel-Hellmann, J. Mathieu, C. Montecucco, W. J. Tang, M. Mock, D. R. Vidal, and P. L. Goossens. 2005. Anthrax edema toxin cooperates with lethal toxin to impair cytokine secretion during infection of dendritic cells. J. Immunol. 1744934-4941. [DOI] [PubMed] [Google Scholar]
- 55.Trull, M. C., T. V. du Laney, and M. D. Dibner. 2007. Turning biodefense dollars into products. Nat. Biotechnol. 25179-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Turnbull, P. C. 1991. Anthrax vaccines: past, present and future. Vaccine 9533-539. [DOI] [PubMed] [Google Scholar]
- 57.Uchida, I., K. Hashimoto, and N. Terakado. 1986. Virulence and immunogenicity in experimental animals of Bacillus anthracis strains harbouring or lacking 110 MDa and 60 MDa plasmids. J. Gen. Microbiol. 132557-559. [DOI] [PubMed] [Google Scholar]
- 58.Vodkin, M. H., and S. H. Leppla. 1983. Cloning of the protective antigen gene of Bacillus anthracis. Cell 34693-697. [DOI] [PubMed] [Google Scholar]
- 59.Welkos, S. L. 1991. Plasmid-associated virulence factors of non-toxigenic (pX01−) Bacillus anthracis. Microb. Pathog. 10183-198. [DOI] [PubMed] [Google Scholar]
- 60.Welkos, S. L., and A. M. Friedlander. 1988. Pathogenesis and genetic control of resistance to the Sterne strain of Bacillus anthracis. Microb. Pathog. 453-69. [DOI] [PubMed] [Google Scholar]
- 61.Welkos, S. L., T. J. Keener, and P. H. Gibbs. 1986. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 51795-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Welkos, S. L., N. J. Vietri, and P. H. Gibbs. 1993. Non-toxigenic derivatives of the Ames strain of Bacillus anthracis are fully virulent for mice: role of plasmid pX02 and chromosome in strain-dependent virulence. Microb. Pathog. 14381-388. [DOI] [PubMed] [Google Scholar]
- 63.Wimer-Mackin, S., M. Hinchcliffe, C. R. Petrie, S. J. Warwood, W. T. Tino, M. S. Williams, J. P. Stenz, A. Cheff, and C. Richardson. 2006. An intranasal vaccine targeting both the Bacillus anthracis toxin and bacterium provides protection against aerosol spore challenge in rabbits. Vaccine 243953-3963. [DOI] [PubMed] [Google Scholar]
- 64.Wollowitz, S. 2001. Fundamentals of the psoralen-based Helinx technology for inactivation of infectious pathogens and leukocytes in platelets and plasma. Semin. Hematol. 384-11. [DOI] [PubMed] [Google Scholar]
- 65.Xia, Z. G., and D. R. Storm. 1990. A-type ATP binding consensus sequences are critical for the catalytic activity of the calmodulin-sensitive adenylyl cyclase from Bacillus anthracis. J. Biol. Chem. 2656517-6520. [PubMed] [Google Scholar]
- 66.Zaucha, G. M., L. M. Pitt, J. Estep, B. E. Ivins, and A. M. Friedlander. 1998. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation. Arch. Pathol. Lab. Med. 122982-992. [PubMed] [Google Scholar]