Abstract
Ebolavirus causes severe hemorrhagic fever, with case fatality rates as high as 90%. Currently, no licensed vaccine is available against Ebolavirus. We previously generated a replication-deficient, biologically contained Ebolavirus, EbolaΔVP30, which lacks the essential VP30 gene, grows only in cells stably expressing this gene product, and is genetically stable. Here, we evaluated the vaccine potential of EbolaΔVP30. First, we demonstrated its safety in STAT-1-knockout mice, a susceptible animal model for Ebolavirus infection. We then tested its protective efficacy in two animal models, mice and guinea pigs. Mice immunized twice with EbolaΔVP30 were protected from a lethal infection of mouse-adapted Ebolavirus. Virus titers in the serum of vaccinated mice were significantly lower than those in nonvaccinated mice. Protection of mice immunized with EbolaΔVP30 was associated with a high antibody response to the Ebolavirus glycoprotein and the generation of an Ebolavirus NP-specific CD8+ T-cell response. Guinea pigs immunized twice with EbolaΔVP30 were also protected from a lethal infection of guinea pig-adapted Ebolavirus. Our study demonstrates the potential of the EbolaΔVP30 virus as a new vaccine platform.
Ebolaviruses (EBOVs; family Filoviridae) cause severe hemorrhagic fever in humans and nonhuman primates (NHPs), with case fatality rates up to 90% (26). Since the first recorded outbreak in 1976 of EBOV in the Democratic Republic of the Congo, increasing numbers of outbreaks in Central Africa have occurred over the last decade (23). Transmission of the virus results from direct contact of infected humans and animals with body fluids; however, lethal transmission by aerosol droplets can also occur (13, 14). Due to its high pathogenicity and potential for aerosol transmission, EBOV and its sister virus, Marburgvirus (MARV), are classified as category A bioterrorism threats.
Currently, there are no licensed vaccines or antivirals available against EBOV. A vaccine against EBOV would be invaluable to those closely affected during an outbreak along with health care personnel, laboratory workers, and military personnel. Several vaccine candidates have been shown to protect NHPs: a replication-incompetent adenovirus expressing the EBOV glycoprotein (GP) (29-31), a replication-competent vesicular stomatitis virus (VSV) expressing GP (7, 15), a recombinant paramyxovirus expressing GP (4), and virus-like particles (VLPs) (38, 41). However, questions regarding acceptable vaccine doses, prior immunity to the vaccine vector, effectiveness in humans, and safety considerations still linger with these vaccine candidates (10, 25, 42). Therefore, alternative EBOV vaccine candidates continue to be sought.
We recently generated a replication-deficient, biologically contained EBOV via reverse genetics, a technique that allows the generation of infectious EBOV from cloned cDNA (21, 37). This technique provides the opportunity to introduce mutations into the EBOV genome and observe the resulting viral phenotypes (6, 11, 20, 21, 36, 37). Specifically, we generated a replication-deficient virus (EbolaΔVP30) (9) by deleting the entire open reading frame of the VP30 gene, which encodes the essential transcription factor VP30 (18, 27). EbolaΔVP30 is thus replication deficient and biologically contained unless VP30 protein is provided in trans. To allow for viral amplification, we therefore generated a Vero cell line that stably expresses VP30, designated VeroVP30 (9). EbolaΔVP30 undergoes multiple cycles of replication in VeroVP30 cells but not in parental Vero cells. More importantly, the EbolaΔVP30 genome is genetically stable over sequential passages in VeroVP30 cells (i.e., recombination between the EbolaΔVP30 genome and the VP30 cDNA present in VeroVP30 cells does not occur), thereby partially alleviating safety concerns (9). Hence, the EbolaΔVP30 virus can be grown to reasonably high titers in helper cells, expresses all viral antigens/proteins, is genetically stable, and is safe. Here, we evaluate the safety of EbolaΔVP30 as a vaccine in STAT-1-knockout (KO) mice and assess its protective efficacy in two rodent models, mice and guinea pigs.
MATERIALS AND METHODS
Cells.
VeroVP30 cells were established as previously described (9) and grown in Eagle's minimal essential medium (MEM) supplemented with 10% fetal calf serum (FCS), l-glutamine, vitamins, nonessential amino acid solution, and 5 μg/ml puromycin (Sigma, St. Louis, MO).
Viruses.
The EbolaΔVP30 virus was generated as previously described (9) and propagated in VeroVP30 cells in MEM as described above but supplemented with 2% FCS. The virus was harvested 6 days after infection of the cells at a multiplicity of infection of 0.1. Harvested virus was partially purified by ultracentrifugation at 27,000 rpm for 2 h over 20% sucrose. The viral pellet was resuspended in sterile phosphate-buffered saline (PBS) and stored at −80°C. Viral titers were determined by use of a focus-forming assay (visualized with antibody to the viral VP40 protein) in confluent VeroVP30 cells overlaid with MEM containing 2% FCS and 1.5% methylcellulose (Sigma).
For challenge studies in mice or guinea pigs, we used a mouse-adapted EBOV (MA-EBOV) or guinea pig-adapted EBOV (GP-EBOV), subtype Zaire, generated as previously described (3, 5). All studies involving live EBOV were carried out under biosafety level 4 conditions at the National Microbiology Laboratory of the Public Health Agency of Canada in Winnipeg, Canada.
Antibody titers.
The levels of EBOV GP-specific immunoglobulin G (IgG) antibodies in vaccinated mice were examined by using an enzyme-linked immunosorbent assay (ELISA). Briefly, wells of Immulon 2HB plates (Thermon Labsystems, Franklin, MA) were coated with purified EBOV GP (34) and blocked with PBS containing 10 mg/ml bovine serum albumin. EBOV GP-coated wells were incubated with mouse serum from nonvaccinated and vaccinated mice, and bound antibodies were detected with goat anti-mouse IgG conjugated to horseradish peroxidase (Kirkegaard & Perry Laboratories, Inc., Gaithersburg, MD) by use of an ELISA plate reader at an absorbance of 405 nm.
Intracellular staining and flow cytometry.
The number of cytokine-producing CD8+ T cells was determined by intracellular staining as described previously (19). Briefly, splenocytes were stimulated with the control peptide PB1703-711 (SSYRRPVGI, derived from influenza virus PB1) (1) or the EBOV peptide NP279-288 (SFKAALSSLA, derived from the nucleoprotein NP) (22, 28), VP40171-180 (YFTFDLTALK, derived from the matrix protein VP40), or GP161-169 (LYDRLASTV, derived from GP) (22, 39) for 5 h in the presence of brefeldin A and interleukin-2. Following activation, cells were stained for cell surface CD8 and intracellular gamma interferon (IFN-γ) by using the Cytofix/Cytoperm kit from BD Biosciences (San Jose, CA). The number of cytokine-producing CD8+ T cells was determined by using a FACSCalibur flow cytometer (BD Biosciences).
Inoculation of STAT-1-KO mice.
Six-week-old female STAT-1-KO mice (Charles River) were anesthetized with isoflurane and intraperitoneally (i.p.) inoculated with (i) wild-type EBOV (1,000 mouse 50% lethal doses [MLD50]/mouse), (ii) VeroVP30 cells (106 cells/mouse), (iii) EbolaΔVP30 virus (2 × 106 focus-forming units [FFU]/mouse), or (iv) a mixture of EbolaΔVP30 virus and VeroVP30 (106 cells and 2 × 106 FFU/mouse). Animals were observed for at least 28 days after inoculation.
Challenge studies.
Four-week-old female BALB/c mice (The Jackson Laboratory, Bar Harbor, ME) were anesthetized with isoflurane and i.p. immunized twice at 3-week intervals with 106 FFU of EbolaΔVP30 virus; nonvaccinated mice were immunized with PBS. Eight weeks after the second vaccination, mice were challenged i.p. with 1,000 MLD50 of MA-EBOV (3). Four days after challenge, viral titers were determined in the serum of three vaccinated and three nonvaccinated mice. The remaining mice were monitored for survival for 28 days. Female guinea pigs (Charles River) between 200 and 250 g in body weight were anesthetized with isoflurane and i.p. immunized twice at 3-week intervals with 107 FFU of EbolaΔVP30 virus; nonvaccinated guinea pigs were inoculated with PBS. Three weeks after the second vaccination, guinea pigs were challenged i.p. with 1,000 LD50 of GP-EBOV (5) and observed for 16 days.
All animal experiments were performed in accordance with approved animal use protocols and according to the guidelines set forth by the Canadian Council of Animal Care and the University of Wisconsin—Madison.
RESULTS
EbolaΔVP30 virus is not pathogenic in STAT-1-KO mice.
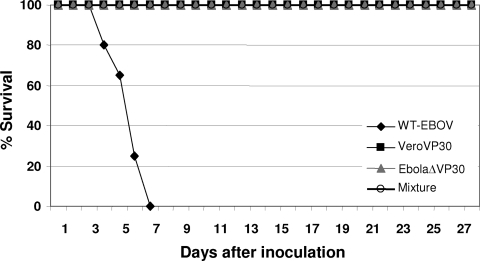
To evaluate the safety of EbolaΔVP30 virus, STAT-1-KO mice, which are susceptible to wild-type EBOV infection (2), were inoculated i.p. with wild-type EBOV (1,000 MLD50/mouse), VeroVP30 cells (106 cells/mouse), EbolaΔVP30 virus (2 × 106 FFU/mouse), or a mixture of EbolaΔVP30 virus and VeroVP30 (106 cells and 2 × 106 FFU/mouse). STAT-1-KO mice inoculated with EbolaΔVP30 virus, VeroVP30 cells, or a mixture of both showed no signs of illness and survived for the entire observation period (28 days) after inoculation (Fig. 1). In contrast, 3 days after inoculation with wild-type EBOV, STAT-1-KO mice showed signs of disease, with ruffled fur and weight loss (data not shown), and by day 6, all mice had succumbed to infection (Fig. 1). These data demonstrate the safety and lack of virulence of the EbolaΔVP30 vaccine candidate.
FIG. 1.
EbolaΔVP30 virus is not virulent in STAT-1-KO mice. Survival curves of STAT-1-KO mice inoculated i.p. with (i) 1,000 MLD50/mouse of wild-type (WT) EBOV (n = 3), (ii) 106 cells/mouse of VeroVP30 cells (n = 5), (iii) 2 × 106 FFU/mouse of EbolaΔVP30 virus (n = 5), or (iv) a mixture of EbolaΔVP30 virus and VeroVP30 (n = 5). Animals were observed for 28 days after inoculation.
Antibody response of mice immunized with EbolaΔVP30 virus.
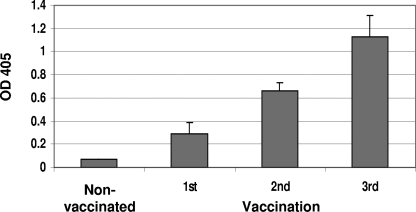
To assess EbolaΔVP30 virus as a potential vaccine candidate, we first determined its immunogenicity in mice by vaccinating mice three times at 3-week intervals. When serum samples, collected 2 weeks after each vaccination, were tested for IgG antibodies by ELISA with purified GP (Fig. 2), vaccinated animals showed elevated antibody titers against GP after the first vaccination relative to those in nonvaccinated mice (Fig. 2); these antibody titers further increased after the second and third vaccinations This finding demonstrates the ability of the biologically contained EbolaΔVP30 virus to elicit antibodies to GP.
FIG. 2.
EbolaΔVP30 virus induces an antibody response to the EBOV glycoprotein GP. Mice (n = 4) were vaccinated with EbolaΔVP30 virus three times at 3-week intervals, whereas nonvaccinated mice (n = 4) were inoculated with PBS. Serum samples were collected 2 weeks after each vaccination, and the amounts of IgG against purified EBOV GP were determined by ELISA, as described in Materials and Methods. Results are expressed as the mean absorbance (optical density [OD]) at 405 nm (± standard deviation) of samples diluted to 1:100.
CD8+ T-cell responses in vaccinated mice.
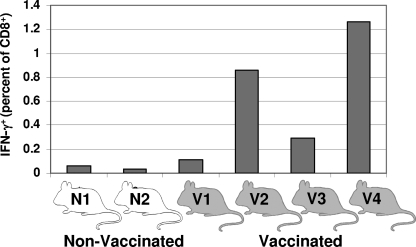
We next examined cellular immune responses to vaccination in mice. Since two vaccinations resulted in high antibody titers in mice (see above), we performed only two vaccinations for all further experiments. Eight days after the second immunization, four vaccinated and two nonvaccinated mice were euthanized and their spleens were removed. Splenocytes were isolated and stimulated with the EBOV peptide NP279-288 (SFKAALSSLA), VP40171-180 (YFTFDLTALK), or GP161-169 (LYDRLASTV), or with the influenza virus peptide PB1703-711 (SSYRRPVGI), for 5 h in the presence of brefeldin A and interleukin-2.
In vaccinated animals, stimulation with the EBOV peptide NP279-288 resulted in IFN-γ-positive CD8+ cells in the range of 0.11% to 1.26% of the total CD8+ cell population (Fig. 3). For the two nonvaccinated mice, the numbers of IFN-γ-positive CD8+ cells were appreciably lower, i.e., 0.056% and 0.032% (Fig. 3). Stimulation of cells with the influenza virus peptide PB1703-711 did not elicit a significant response in vaccinated or nonvaccinated mice (data not shown). No IFN-γ-positive CD8+ cells were detected for cells stimulated with EBOV peptide VP40171-180 or GP161-169 (data not shown).
FIG. 3.
Cellular immune response in EbolaΔVP30-vaccinated mice. Mice (n = 4) were immunized twice at 3-week intervals with EbolaΔVP30; nonvaccinated mice (n = 2) were simultaneously inoculated with PBS. Splenocytes were collected 8 days after the second vaccination and stimulated with an EBOV NP peptide. Cells were stained for the cell surface antigen CD8+ and for intracellular IFN-γ. The number of cytokine-producing CD8+ T cells was determined by using a FACSCalibur flow cytometer (BD Biosciences). N, nonvaccinated; V, vaccinated.
Protective efficacy of EbolaΔVP30 virus in mice.
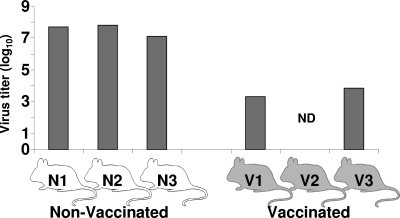
To assess the protective efficacy of EbolaΔVP30 virus, we immunized 18 4-week-old mice twice (with a 3-week interval) with 106 FFU of EbolaΔVP30 virus; 13 control mice were similarly inoculated with PBS. Mice were challenged 8 weeks after the second immunization with 1,000 MLD50 of MA-EBOV (3). After challenge, no signs of illness were seen in mice vaccinated with EbolaΔVP30 virus, whereas nonvaccinated mice began to show signs of sickness (e.g., ruffled fur) and weight loss on day 3 postchallenge (data not shown). By day 6 postchallenge, all nonvaccinated mice had succumbed to infection, whereas the vaccinated mice were fully protected (Fig. 4). All animals were observed for 21 days after challenge. On day 4 postchallenge, three vaccinated and three nonvaccinated mice were sacrificed to determine virus titers in their sera. Vaccinated mice had significantly lower titers than did nonvaccinated mice (Fig. 5), with one mouse showing no viremia by day 4. Taken together, these data demonstrate that EbolaΔVP30 virus efficiently protects mice against challenge with a lethal dose of MA-EBOV.
FIG. 4.
Protective efficacy of EbolaΔVP30 virus in mice. Mice (n = 15) were immunized twice with EbolaΔVP30 virus; nonvaccinated mice (n = 10) were inoculated with PBS. Eight weeks after the second vaccination, mice from the vaccinated and nonvaccinated groups were challenged with 1,000 MLD50 of MA-EBOV. A control group (Mock, n = 3) remained nonvaccinated and nonchallenged. Survival curves are shown.
FIG. 5.
Virus titers in immunized mice. Vaccinated and nonvaccinated mice (three per group) were euthanized on day 4 postchallenge. Virus titers in the serum were determined by use of a focus-forming assay as described in Materials and Methods. N, nonvaccinated; V, vaccinated; ND, not detectable.
Protective efficacy of EbolaΔVP30 virus in guinea pigs.
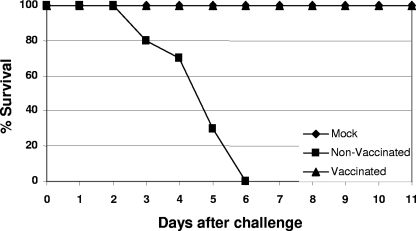
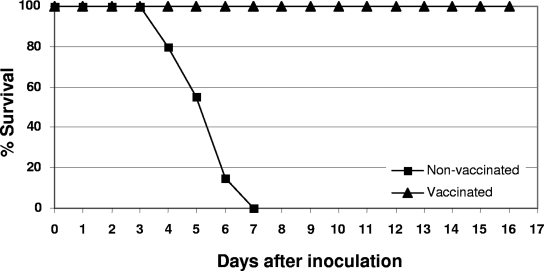
To further demonstrate the protective efficacy of EbolaΔVP30 virus, we immunized six guinea pigs twice (with a 3-week interval) with 107 FFU of EbolaΔVP30 virus; six guinea pigs were similarly inoculated with PBS. Guinea pigs were challenged 6 weeks after the second vaccination with 1,000 LD50 of GP-EBOV (5). After challenge, no signs of sickness were seen in the vaccinated guinea pigs, whereas nonvaccinated animals began loosing weight on day 3 postchallenge (data not shown). By day 7 postchallenge, all nonvaccinated guinea pigs had succumbed to infection, while all vaccinated guinea pigs showed no signs of disease and were fully protected (Fig. 6). All animals were observed for 16 days after challenge.
FIG. 6.
Protective efficacy of EbolaΔVP30 virus in guinea pigs. Survival curves of guinea pigs vaccinated twice with EbolaΔVP30 virus or inoculated with PBS (n = 6 per group). Six weeks after the last vaccination, guinea pigs were challenged with 1,000 LD50 of GP-EBOV. Animals were observed for 16 days after challenge.
DISCUSSION
Here, we assessed the potential of EbolaΔVP30 as a vaccine candidate. We found that EbolaΔVP30 is safe and does not cause disease or death in STAT-1-KO mice, in contrast to wild-type EBOV. Moreover, we found that mice and guinea pigs vaccinated with EbolaΔVP30 virus are protected against lethal challenge with MA- or GP-EBOV, respectively. In vaccinated mice, virus titers in sera were significantly lower than those in nonvaccinated mice.
Protection against EBOV infection likely requires both humoral and cellular responses. The humoral response to EBOV infection is important, as demonstrated by protection from a lethal challenge in rodent models by passive transfer of antibodies to the viral glycoprotein GP (8, 33). However, the ability of a vaccine to elicit an antibody response does not in itself correlate with protection. For example, classic vaccine approaches, such as gamma-irradiated EBOV and MARV, or GP expressed by baculovirus, elicit a moderate antibody response but fail to protect mice against lethal challenge (12, 16, 17). In contrast, EBOV and MARV VLPs that express GP and VP40 elicit both humoral and CD8+ T-cell responses and protect mice against a lethal challenge of EBOV and MARV (38-40), highlighting the importance of cellular responses for protection. Here, we demonstrate that EbolaΔVP30 virus induces both humoral and CD8+ T-cell responses (specific for an EBOV NP epitope). The next logical step is to test whether the immune responses elicited by EbolaΔVP30 are sufficient to protect NHPs from a lethal challenge with EBOV.
Three vaccine candidates, based on recombinant viral vectors expressing EBOV GP, are protective in an NHP model: adenovirus (29-31), VSV (7, 15), and paramyxovirus (4). However, none of these candidates is practical in its current form. The paramyxovirus-based vaccine does not confer full protection in the NHP model (4). The adenovirus-based vector, a replication-incompetent vector, is based on a human pathogen (adenovirus type 5), raising concerns of preexisting immunity to the vector. In addition, a large dose of this virus (1010 particles) is needed to confer protection in NHPs (29, 32, 35). A vaccine based on the VSV vector protects NHPs at reasonable doses; however, this vector is replication competent and safety is, therefore, a concern, particularly the potential for infection of the human central nervous system (24). EBOV and MARV VLPs have been shown to protect various animal models from a lethal challenge with these viruses (38, 40, 41). While VLPs are safe and preexisting immunity is not a concern for VLP vaccines, large-scale production of pure VLPs in cell culture can be an obstacle.
Here, we present a vaccine approach that is safe, efficacious, and highly efficient since EbolaΔVP30 virus grows to high titers in Vero VP30 cells (9). As with other EBOV vaccine candidates, our vaccine would be of value to health care personnel, laboratory workers, and military personnel, as well as to those at risk during outbreaks. Further studies are needed to establish the protective efficacy of EbolaΔVP30 in NHPs and to assess its potential for postexposure treatment.
Acknowledgments
We acknowledge membership within and support from the Region V “Great Lakes” RCE (NIH award 1-U54-AI-057153). This work was also sponsored by a contract research fund for the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases from the Ministries of Education, Culture, Sports, Science, and Technology and of Health, Labor, and Welfare of Japan; by CREST (Japan Science and Technology Agency); and by National Institute of Allergy and Infectious Diseases Public Health Service research grants and the Public Health Agency of Canada.
We also thank Susan Watson for scientific editing and Friederike Feldmann for animal care in the biosafety level 4 facility.
Footnotes
Published ahead of print on 11 February 2009.
REFERENCES
- 1.Belz, G. T., W. Xie, and P. C. Doherty. 2001. Diversity of epitope and cytokine profiles for primary and secondary influenza a virus-specific CD8+ T cell responses. J. Immunol. 1664627-4633. [DOI] [PubMed] [Google Scholar]
- 2.Bray, M. 2001. The role of the type I interferon response in the resistance of mice to filovirus infection. J. Gen. Virol. 821365-1373. [DOI] [PubMed] [Google Scholar]
- 3.Bray, M., K. Davis, T. Geisbert, C. Schmaljohn, and J. Huggins. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 178651-661. [DOI] [PubMed] [Google Scholar]
- 4.Bukreyev, A., P. E. Rollin, M. K. Tate, L. Yang, S. R. Zaki, W. J. Shieh, B. R. Murphy, P. L. Collins, and A. Sanchez. 2007. Successful topical respiratory tract immunization of primates against Ebola virus. J. Virol. 816379-6388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Connolly, B. M., K. E. Steele, K. J. Davis, T. W. Geisbert, W. M. Kell, N. K. Jaax, and P. B. Jahrling. 1999. Pathogenesis of experimental Ebola virus infection in guinea pigs. J. Infect. Dis. 179(Suppl. 1)S203-S217. [DOI] [PubMed] [Google Scholar]
- 6.Ebihara, H., A. Takada, D. Kobasa, S. Jones, G. Neumann, S. Theriault, M. Bray, H. Feldmann, and Y. Kawaoka. 2006. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feldmann, H., S. M. Jones, K. M. Daddario-DiCaprio, J. B. Geisbert, U. Stroher, A. Grolla, M. Bray, E. A. Fritz, L. Fernando, F. Feldmann, L. E. Hensley, and T. W. Geisbert. 2007. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 3e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta, M., S. Mahanty, M. Bray, R. Ahmed, and P. E. Rollin. 2001. Passive transfer of antibodies protects immunocompetent and immunodeficient mice against lethal Ebola virus infection without complete inhibition of viral replication. J. Virol. 754649-4654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halfmann, P., J. H. Kim, H. Ebihara, T. Noda, G. Neumann, H. Feldmann, and Y. Kawaoka. 2008. Generation of biologically contained Ebola viruses. Proc. Natl. Acad. Sci. USA 1051129-1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hart, M. K. 2003. Vaccine research efforts for filoviruses. Int. J. Parasitol. 33583-595. [DOI] [PubMed] [Google Scholar]
- 11.Hartman, A. L., J. E. Dover, J. S. Towner, and S. T. Nichol. 2006. Reverse genetic generation of recombinant Zaire Ebola viruses containing disrupted IRF-3 inhibitory domains results in attenuated virus growth in vitro and higher levels of IRF-3 activation without inhibiting viral transcription or replication. J. Virol. 806430-6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ignatyev, G. M., A. P. Agafonov, M. A. Streltsova, and E. A. Kashentseva. 1996. Inactivated Marburg virus elicits a nonprotective immune response in rhesus monkeys. J. Biotechnol. 44111-118. [DOI] [PubMed] [Google Scholar]
- 13.Jaax, N., P. Jahrling, T. Geisbert, J. Geisbert, K. Steele, K. McKee, D. Nagley, E. Johnson, G. Jaax, and C. Peters. 1995. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet 3461669-1671. [DOI] [PubMed] [Google Scholar]
- 14.Johnson, E., N. Jaax, J. White, and P. Jahrling. 1995. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int. J. Exp. Pathol. 76227-236. [PMC free article] [PubMed] [Google Scholar]
- 15.Jones, S. M., H. Feldmann, U. Stroher, J. B. Geisbert, L. Fernando, A. Grolla, H. D. Klenk, N. J. Sullivan, V. E. Volchkov, E. A. Fritz, K. M. Daddario, L. E. Hensley, P. B. Jahrling, and T. W. Geisbert. 2005. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat. Med. 11786-790. [DOI] [PubMed] [Google Scholar]
- 16.Lupton, H. W., R. D. Lambert, D. L. Bumgardner, J. B. Moe, and G. A. Eddy. 1980. Inactivated vaccine for Ebola virus efficacious in guineapig model. Lancet ii1294-1295. [DOI] [PubMed] [Google Scholar]
- 17.Mellquist-Riemenschneider, J. L., A. R. Garrison, J. B. Geisbert, K. U. Saikh, K. D. Heidebrink, P. B. Jahrling, R. G. Ulrich, and C. S. Schmaljohn. 2003. Comparison of the protective efficacy of DNA and baculovirus-derived protein vaccines for EBOLA virus in guinea pigs. Virus Res. 92187-193. [DOI] [PubMed] [Google Scholar]
- 18.Muhlberger, E., M. Weik, V. E. Volchkov, H. D. Klenk, and S. Becker. 1999. Comparison of the transcription and replication strategies of Marburg virus and Ebola virus by using artificial replication systems. J. Virol. 732333-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murali-Krishna, K., J. D. Altman, M. Suresh, D. Sourdive, A. Zajac, and R. Ahmed. 1998. In vivo dynamics of anti-viral CD8 T cell responses to different epitopes. An evaluation of bystander activation in primary and secondary responses to viral infection. Adv. Exp. Med. Biol. 452123-142. [DOI] [PubMed] [Google Scholar]
- 20.Neumann, G., H. Ebihara, A. Takada, T. Noda, D. Kobasa, L. D. Jasenosky, S. Watanabe, J. H. Kim, H. Feldmann, and Y. Kawaoka. 2005. Ebola virus VP40 late domains are not essential for viral replication in cell culture. J. Virol. 7910300-10307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumann, G., H. Feldmann, S. Watanabe, I. Lukashevich, and Y. Kawaoka. 2002. Reverse genetics demonstrates that proteolytic processing of the Ebola virus glycoprotein is not essential for replication in cell culture. J. Virol. 76406-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olinger, G. G., M. A. Bailey, J. M. Dye, R. Bakken, A. Kuehne, J. Kondig, J. Wilson, R. J. Hogan, and M. K. Hart. 2005. Protective cytotoxic T-cell responses induced by Venezuelan equine encephalitis virus replicons expressing Ebola virus proteins. J. Virol. 7914189-14196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pourrut, X., B. Kumulungui, T. Wittmann, G. Moussavou, A. Delicat, P. Yaba, D. Nkoghe, J. P. Gonzalez, and E. M. Leroy. 2005. The natural history of Ebola virus in Africa. Microbes Infect. 71005-1014. [DOI] [PubMed] [Google Scholar]
- 24.Quiroz, E., N. Moreno, P. H. Peralta, and R. B. Tesh. 1988. A human case of encephalitis associated with vesicular stomatitis virus (Indiana serotype) infection. Am. J. Trop. Med. Hyg. 39312-314. [DOI] [PubMed] [Google Scholar]
- 25.Reed, D. S., and M. Mohamadzadeh. 2007. Status and challenges of filovirus vaccines. Vaccine 251923-1934. [DOI] [PubMed] [Google Scholar]
- 26.Sanchez, A., T. W. Geisbert, and H. Feldmann. 2007. Filoviridae: Marburg and Ebola viruses, p. 1409-1448. In D. M. Knipe, P. M. Howley, D. E. Griffin, M. A. Martin, R. A. Lamb, B. Roizman, and S. E. Straus (ed.), Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA.
- 27.Sanchez, A., M. P. Kiley, B. P. Holloway, and D. D. Auperin. 1993. Sequence analysis of the Ebola virus genome: organization, genetic elements, and comparison with the genome of Marburg virus. Virus Res. 29215-240. [DOI] [PubMed] [Google Scholar]
- 28.Simmons, G., A. Lee, A. J. Rennekamp, X. Fan, P. Bates, and H. Shen. 2004. Identification of murine T-cell epitopes in Ebola virus nucleoprotein. Virology 318224-230. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan, N. J., T. W. Geisbert, J. B. Geisbert, D. J. Shedlock, L. Xu, L. Lamoreaux, J. H. Custers, P. M. Popernack, Z. Y. Yang, M. G. Pau, M. Roederer, R. A. Koup, J. Goudsmit, P. B. Jahrling, and G. J. Nabel. 2006. Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPs. PLoS Med. 3e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sullivan, N. J., T. W. Geisbert, J. B. Geisbert, L. Xu, Z. Y. Yang, M. Roederer, R. A. Koup, P. B. Jahrling, and G. J. Nabel. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 424681-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sullivan, N. J., A. Sanchez, P. E. Rollin, Z. Y. Yang, and G. J. Nabel. 2000. Development of a preventive vaccine for Ebola virus infection in primates. Nature 408605-609. [DOI] [PubMed] [Google Scholar]
- 32.Swenson, D. L., D. Wang, M. Luo, K. L. Warfield, J. Woraratanadharm, D. H. Holman, J. Y. Dong, and W. D. Pratt. 2008. Vaccine to confer to nonhuman primates complete protection against multistrain Ebola and Marburg virus infections. Clin. Vaccine Immunol. 15460-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takada, A., H. Ebihara, S. Jones, H. Feldmann, and Y. Kawaoka. 2007. Protective efficacy of neutralizing antibodies against Ebola virus infection. Vaccine 25993-999. [DOI] [PubMed] [Google Scholar]
- 34.Takada, A., S. Watanabe, K. Okazaki, H. Kida, and Y. Kawaoka. 2001. Infectivity-enhancing antibodies to Ebola virus glycoprotein. J. Virol. 752324-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tatsis, N., and H. C. Ertl. 2004. Adenoviruses as vaccine vectors. Mol. Ther. 10616-629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Theriault, S., A. Groseth, H. Artsob, and H. Feldmann. 2005. The role of reverse genetics systems in determining filovirus pathogenicity. Arch. Virol. Suppl. 2005(19)157-177. [DOI] [PubMed] [Google Scholar]
- 37.Volchkov, V. E., V. A. Volchkova, E. Muhlberger, L. V. Kolesnikova, M. Weik, O. Dolnik, and H. D. Klenk. 2001. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science 2911965-1969. [DOI] [PubMed] [Google Scholar]
- 38.Warfield, K. L., C. M. Bosio, B. C. Welcher, E. M. Deal, M. Mohamadzadeh, A. Schmaljohn, M. J. Aman, and S. Bavari. 2003. Ebola virus-like particles protect from lethal Ebola virus infection. Proc. Natl. Acad. Sci. USA 10015889-15894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Warfield, K. L., G. Olinger, E. M. Deal, D. L. Swenson, M. Bailey, D. L. Negley, M. K. Hart, and S. Bavari. 2005. Induction of humoral and CD8+ T cell responses are required for protection against lethal Ebola virus infection. J. Immunol. 1751184-1191. [DOI] [PubMed] [Google Scholar]
- 40.Warfield, K. L., D. L. Swenson, D. L. Negley, A. L. Schmaljohn, M. J. Aman, and S. Bavari. 2004. Marburg virus-like particles protect guinea pigs from lethal Marburg virus infection. Vaccine 223495-3502. [DOI] [PubMed] [Google Scholar]
- 41.Warfield, K. L., D. L. Swenson, G. G. Olinger, W. V. Kalina, M. J. Aman, and S. Bavari. 2007. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J. Infect. Dis. 196(Suppl. 2)S430-S437. [DOI] [PubMed] [Google Scholar]
- 42.Yang, Z. Y., L. S. Wyatt, W. P. Kong, Z. Moodie, B. Moss, and G. J. Nabel. 2003. Overcoming immunity to a viral vaccine by DNA priming before vector boosting. J. Virol. 77799-803. [DOI] [PMC free article] [PubMed] [Google Scholar]