Abstract
The 1918 influenza pandemic caused more than 40 million deaths and likely resulted from the introduction and adaptation of a novel avian-like virus. Influenza A virus hemagglutinins are important in host switching and virulence. Avian-adapted influenza virus hemagglutinins bind sialic acid receptors linked via α2-3 glycosidic bonds, while human-adapted hemagglutinins bind α2-6 receptors. Sequence analysis of 1918 isolates showed hemagglutinin genes with α2-6 or mixed α2-6/α2-3 binding. To characterize the role of the sialic acid binding specificity of the 1918 hemagglutinin, we evaluated in mice chimeric influenza viruses expressing wild-type and mutant hemagglutinin genes from avian and 1918 strains with differing receptor specificities. Viruses expressing 1918 hemagglutinin possessing either α2-6, α2-3, or α2-3/α2-6 sialic acid specificity were fatal to mice, with similar pathology and cellular tropism. Changing α2-3 to α2-6 binding specificity did not increase the lethality of an avian-adapted hemagglutinin. Thus, the 1918 hemagglutinin contains murine virulence determinants independent of receptor binding specificity.
The 1918-1919 “Spanish” influenza pandemic was responsible for an estimated 40 to 50 million deaths worldwide and approximately 675,000 deaths in the United States (9). The genome of the 1918 (H1N1) influenza A virus (IAV) was sequenced from viral RNA fragments retained in lung tissues collected from infected humans who died during the pandemic (35, 36). Sequence analyses suggest that the 1918 pandemic virus arose after the adaptation and introduction of an avian-like H1N1 IAV into humans (22, 36). Influenza virus pandemics occur periodically and have been associated with the introduction of new hemagglutinin (HA) subtypes, such as the 1957 (H2N2) and 1968 (H3N2) pandemic viruses (34). The emergence and spread of an antigenically novel IAV capable of causing a new pandemic are currently a matter of strong public health concern, the most notable of which is the continued circulation of Eurasian-lineage highly pathogenic avian influenza (HPAI) viruses of the H5N1 subtype capable of causing severe and unusually fatal respiratory disease in humans (21, 42). Thus, understanding of the virulence and pathogenic properties of past pandemic influenza viruses, including the 1918 virus, is crucial.
The HA protein of IAVs initiates infection by binding sialic acid (SA)-containing glycoproteins on cells (26). The specificity of HA binding to terminal SA residues is dependent on the conformation of the bond to the penultimate carbohydrate. The tissues of different host animals express different SA isomers: α2-3 linkages in the gut of waterfowl, α2-3 and α2-6 linkages on the lung and intestinal epithelium of chickens, and α2-6 linkages in the upper respiratory epithelium and α2-3 linkages in the lower respiratory epithelium of humans (1, 5, 6, 27, 32, 41). In general, avian-adapted IAVs preferentially bind SA α2-3 Gal and human-adapted IAVs have a binding preference for SA α2-6 Gal (2, 16), based on differences in the amino acid sequences in the HA receptor binding domain (RBD). The consensus sequence of the RBD of avian H1 viruses includes a Glu at position 190 and a Gly at 225 (H3 numbering); human-adapted H1 viruses generally have an Asp at both positions 190 and 225. Previous studies have shown that mutations at these positions in an avian H1 virus to the human consensus are sufficient to alter its SA binding preference from α2-3 to α2-6 (30, 31).
It has been hypothesized that E190D and G225D mutations in avian H1 viruses can lead to a host-switching event by changing its SA binding specificity (24). Intriguingly, of the five 1918 influenza virus HA genes sequenced to date, three have a D190 and a D225 with α2-6 specificity (for example, A/South Carolina/1/1918 H1N1 [SC1918]) while two have 190D and 225G with mixed α2-3 and α2-6 specificities (for example, A/New York/1/1918 H1N1 [NY1918]) (25). Given the differing receptor binding specificities of 1918 HA genes, we need to extend the hypothesis that avian-to-human IAV host switching is based on HA binding specificity to include important changes in HA outside the RBD. The factors that allow an IAV to be transmissible between humans are not well understood, but changes in the RBD are likely to be important factors in the process. It was recently demonstrated in a ferret transmission model that α2-6 SC1918 was transmitted efficiently to contact animals, α2-3/α2-6 NY1918 transmitted less well, and an “avianized” form of the 1918 virus, in which the 190 position of the RBD was mutated back to the conserved avian 190E sequence, did not transmit at all (40). Moreover, this study showed that differences in the SA binding specificity of 1918 HA proteins did not affect weight loss, viral replication, or pathogenesis in primary inoculated ferrets.
Additional studies have shown that the entire 1918 HA gene can act as a virulence factor in mouse studies in that viruses bearing the 1918 HA gene can induce lethal infections (10, 13, 20, 37, 39). However, the contributions that sequence differences in the RBD make to the virulence of the 1918 virus have not been previously examined. The presence of multiple positively charged amino acids in the cleavage domain is characteristically observed in highly pathogenic subtype H5 or H7 avian influenza viruses; however, this sequence does on appear in any 1918 HA (29, 35). To examine the relationship between influenza virus receptor binding specificity and virulence, we tested two hypotheses, (i) if changing the α2-3 SA binding of an avian-adapted HA to α2-6 would increase virulence and (ii) if altering the α2-6 SA binding specificity of the 1918 HA to α2-3 would abolish virulence in a mouse model.
MATERIALS AND METHODS
Construction and rescue of chimeric viruses.
A frozen stock of A/New York/312/2001 (H1N1) [NY312] was kindly provided by Sara B. Griesemer, Kirsten St. George, and Jill Taylor from the Wadsworth Center, New York State Department of Health, Albany (17). After growth in MDCK cells, viral RNA was extracted and reverse transcription and full-length segment reverse transcription-PCR were performed in accordance with previously published protocols (7). To determine the terminal portions of the untranslated regions of the A/New York/312/2001 (H1N1) gene segments, the SMART RACE (rapid amplification of cDNA ends) cDNA amplification kit (Clontech, Palo Alto, CA) was used. Viral RNA was extracted and reverse transcribed with the PowerScript reverse transcriptase, the RACE cDNA synthesis primer, and SMART II A oligonucleotide (Clontech). 5′ RACE reactions were performed with specific primers for each of the eight gene segments. The Platinum PCR high-fidelity Taq polymerase (Invitrogen, Carlsbad, CA) was used to perform 5′ RACE. After an initial denaturation of 1 cycle at 94°C for 2 min, the mixture was amplified for 40 cycles of 94°C for 30 s, 60°C for 30 s, and 72°C for 1 min. All of the RACE-derived PCR products were subcloned into the pTOPO TA vector (Invitrogen, Carlsbad, CA) and sequenced with an ABI 3130 genetic analyzer.
The eight full-length viral gene segments were subcloned in an antisense orientation into the pHH21 rescue plasmid (kindly provided by Yoshihiro Kawaoka, University of Wisconsin, Madison), and the gene segments encoding the four proteins needed for influenza virus polymerase activity (PB2, PB1, PA, and NP) were subcloned into the pCAGGS expression plasmid (kindly provided by Adolfo García-Sastre, Mt. Sinai School of Medicine, New York, NY) to generate NY312 by reverse genetics in accordance with previously published protocols (4, 18). The HA gene of A/South Carolina/1/1918, the neuraminidase (NA) gene of A/Brevig Mission/1/1918 (37), and the HA and NA genes of A/duck/Alberta/35/1976 H1N1 (31) were subcloned into pHH21. RBD mutations in the 1918 and DkAlb HA genes were generated with a site-directed mutagenesis kit by following the manufacturer's instructions (Stratagene, La Jolla, CA). Chimeric influenza viruses, each containing six genes from NY312 and the HA and NA genes from either 1918 or Dk/Alberta were produced in accordance with previously published reverse genetics protocols (4, 18).
Growth and titration of viruses.
The Dk/Alberta HA,NA:NY312 (Av-wt) and Dk/Alberta HA190,225,NA:NY312 (Av-mut) viruses were passaged once on MDCK cells. The 1918 HASC,NA:NY312 (1918-SC), 1918 HANY,NA:NY312 (1918-NY), and 1918 HA190,225,NA:NY312 (1918-NYmut) viruses were passaged twice on MDCK cells in the presence of 1.0 μg/ml N-tosyl-l-phenylalanyl chloromethyl ketone (TPCK)-treated trypsin in Dulbecco modified Eagle medium (DMEM). Viruses were harvested between 48 and 72 h after infection and then centrifuged for 10 min at 1,500 rpm. Supernatants were frozen at −80°C until further use. For virus titrations, virus stocks were serially 10-fold diluted in DMEM, and 250 μl was added to MDCK cells grown to confluence in 12-well plates. Each dilution was done in duplicate. Following incubation for 1 h at 37°C, cells were washed once with 1× phosphate-buffered saline and overlaid with 1.5 ml of agar gel (1% agar in minimal essential medium). After 2 to 3 days, the agar was removed and the cells were stained with crystal violet solution (2% [vol/vol] ethanol, 1% [wt/vol] crystal violet). Virus titers were calculated according to the method of Reed and Muench (23). All procedures involving viruses containing genes from the 1918 and Dk/Alberta influenza viruses were performed in an enhanced biosafety level 3 (BSL3) laboratory.
Mouse infection studies.
Groups of 8- to 10-week-old female BALB/c mice (Taconic Farms, Germantown, NY) were lightly anesthetized in a chamber with isoflurane supplemented with O2 (1.5 liters/min) and intranasally inoculated with between 2 × 103 and 2 × 105 PFU of IAV in a total volume of 25 to 50 μl. Viruses were diluted in sterile DMEM where appropriate. Body weights were measured daily, and mice were humanely euthanized if they lost more than 20% of their starting body weight. Lungs were collected for viral titration and pathology at 4 and 6 days postinoculation (dpi). For each virus and time point, lungs from three animals were collected for viral titration and two were collected for pathology. Lungs collected for pathology were inflated with 10% neutral buffered formalin at the time of isolation to prevent atelectasis. Lung viral titers were determined by plaque assay (described above) in 10% (wt/vol) lung suspensions prepared by homogenization in sterile 1× L15 medium. All experimental animal work was performed in an enhanced animal BSL3 laboratory at the National Institutes of Heath (NIH) following the approval of animal safety protocols by the NIH Animal Care and Use Committee.
Pathology and immunohistochemistry.
Tissue samples, including the fixed, inflated lungs, mediastinal lymph nodes, and spleen, were dehydrated and embedded in paraffin, and 5-μm sections on positively charged slides were stained with hematoxylin and eosin for histopathologic examination. Influenza virus antigen distribution was evaluated by immunohistochemistry in accordance with the manufacturer's protocol (Invitrogen Corp., Carlsbad, CA). Antigen retrieval was performed with 10 mM sodium citrate-0.05% Tween 20 buffer, pH 6.0, with a 2100 Retriever model pressure cooker by following the manufacturer's instructions (Pickcell Laboratories, Amsterdam, The Netherlands). The primary antibody was a goat polyclonal antibody to IAV (Abcam Inc., Cambridge, MA), and it was detected with biotinylated rabbit anti-goat immunoglobulin G (Invitrogen Corp., Carlsbad, CA); the chromogen was aminoethylcarbazole.
Nucleotide sequence accession numbers.
The gene segment sequences determined in this study, including the newly determined untranslated regions, have been deposited in GenBank (accession numbers FJ770051 to FJ770058).
RESULTS
Generation of avian (H1N1) and 1918 (H1N1) HA and NA chimeric viruses.
To understand how changing the SA binding specificity of an avian-adapted HA would affect IAV virulence in a mouse model, we studied the growth, virulence, and pathogenicity of two recombinant influenza viruses expressing wild-type α2-3 or mutant α2-6 SA binding HA genes, created by reverse genetics, on the backbone of a contemporary low-passage human H1N1 virus (A/New York/312/2001) (Table 1). As a representative avian HA with α2-3 SA binding specificity, we used the HA and NA from Dk/Alberta/35/1976, resulting in a virus designated Av-wt. Two amino acids in the HA ligand binding domain of this virus were then mutated to E190D and G225D, resulting in a virus designated Av-mut that has been shown to have α2-6 specificity (31). To minimize the confounding effects of HA and NA function, these viruses also contained identical wild-type Dk/Alberta/35/1976 NA genes. In parallel, to test the effect of changing the α2-6 1918 HA SA specificity to an avian α2-3-only specificity, we also created three 1918 reassortant viruses. Two viruses contained an HA gene that represented one of two 1918 sequences isolated from human tissues, (i) the HA from A/South Carolina/1/18 (containing D190 and D225 and showing α2-6 specificity) or (ii) the HA from A/New York/1/18 (containing D190 and G225 and showing a blended α2-3 and α2-6 specificity) (31). These viruses were designated 1918-SC and 1918-NY, respectively, and only differ in one nucleotide that changes the D225 codon in A/South Carolina/1/18 to G225 in A/New York/1/18. A third 1918 HA chimeric virus was generated by mutating a single nucleotide in the A/New York/1/18 HA gene that recapitulated the avian consensus RBD (containing E190 and G225 and showing α2-3 specificity) and was designated 1918-NYmut. To ensure that all of the differences in the 1918 reassortant viruses were attributable to HA activity, all three 1918 reassortant viruses also contained the same 1918 NA gene.
TABLE 1.
Gene origins, cell culture replication, and MLD50s of parental and chimeric avian and 1918 influenza viruses
| Virus | HA origin | HA190 | HA225 | SA specificity | NA origin | Internal gene | Replication in MDCK cells (PFU/ml) | MLD50a | %Mouse lethalityb |
|---|---|---|---|---|---|---|---|---|---|
| NY312 | NY312 | Asp | Asp | α2−6 | NY312 | NY312 | 3.7 × 107 | >5 | 0 |
| Av-wt | Dk/Alb | Glu | Gly | α2−3c | Dk/Alb | NY312 | 8.6 × 106 | >5 | 0 |
| Av-mut | Dk/Alb | Asp | Asp | α2−6c | Dk/Alb | NY312 | 8 × 106 | >5 | 0 |
| 1918-SC | 1918 | Asp | Asp | α2−6d | 1918 | NY312 | 3.8 × 106 | 3.8 | 100 |
| 1918-NY | 1918 | Asp | Gly | α2−6 + α2−3d | 1918 | NY312 | 3.9 × 106 | 4.47 | 100 |
| 1918-NYmut | 1918 | Glu | Gly | α2−3d | 1918 | NY312 | 3.3 × 106 | >5 | 33 |
Wild-type and mutant avian HA-expressing virus mouse infection studies.
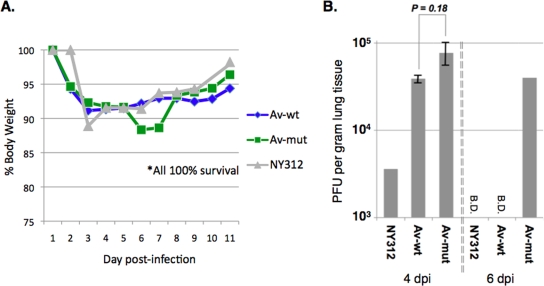
To test the virulence properties of the avian HA, NA H1N1 reassortant viruses, mice were intranasally inoculated with 2 × 105 PFU of each virus. Weight loss was measured daily, and viral lung titers and lung pathology were evaluated on different days postinfection. As shown in Fig. 1A, neither the parental NY312, the α2-3 binding Av-wt, nor the α2-6-specific Av-mut virus was lethal in mice, although mice inoculated with the Av-mut virus showed slightly more weight loss than did mice inoculated with the wild-type duck HA-expressing virus or the parental NY312 virus. The increased morbidity of the mice inoculated with the Av-mut virus was, however, associated with peak lung titers similar to those of mice inoculated with Av-wt (Fig. 1B). Interestingly, the alteration of the α2-3 SA binding specificity of the avian HA proteins to α2-6 resulted in sustained lung viral titers (at 6 dpi) that were not observed with either the parental NY312 or the Av-wt HA virus. These results showed that simply changing the SA receptor binding specificity of a representative avian HA does not in itself account for virulence, as measured by lethality for mice, but delayed viral clearance from the lungs.
FIG. 1.
Results of wild-type and mutant avian HA-expressing influenza virus infection experiments. (A) Weight loss of mice infected with rescued influenza viruses. Ten- to 12-week-old female BALB/c mice were intranasally inoculated with 2 × 105 PFU of the indicated viruses and weighed daily. Both the Av-wt and Av-mut viruses resulted in minimal weight loss (n = 5 mice per virus per group). (B) Virus titers in the lungs of infected BALB/c mice (n = 2 or 3) described in PFU per gram of lung tissue as determined by plaque assay (B.D. indicates below the detection threshold). Two-tailed P values were calculated with an unpaired t test.
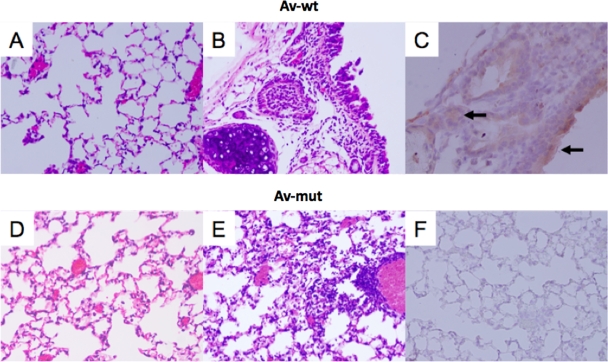
To determine the baseline pathogenic phenotype of the parental contemporary of the human-adapted H1N1 virus, we intranasally inoculated mice with the NY312 virus and observed minimal pathology in infected mice. Lung sections showed focal bronchioles with luminal necrotic epithelial debris without underlying inflammation, and a mild interstitial inflammation was seen in a few focal areas of the lung (data not shown). The Av-wt virus also induced minimal pathology in infected animals. No pathological changes or viral antigen staining was observed in the epithelium of the lower respiratory tree or in alveolar lining cells (Fig. 2A). Interestingly, sections of trachea showed an acute inflammation of the epithelium and of the submucosal glands (Fig. 2B) associated with viral antigen in the tracheal epithelium and submucosal glands (Fig. 2C). The Av-mut virus did not induce tracheal pathology and produced only minimal focal changes in the lung. A single focus of alveolitis with a mixed inflammatory infiltrate was observed, but the lung was otherwise unaffected (Fig. 2D and E). No viral antigen staining was observed in trachea or alveolar lining cells (Fig. 2F), but weak focal staining was observed in occasional alveolar ducts (data not shown).
FIG. 2.
Pathology and immunohistochemistry of avian HA-expressing virus-infected mouse lung tissue. Photomicrographs of hematoxylin-and-eosin-stained tissue sections and immunohistochemically stained sections to detect influenza viral antigen from mice infected with different influenza virus constructs at 6 dpi. Viral antigen is stained red-brown on a hematoxylin-stained background. Arrows show examples of positive cells. (A to C) Sections from an animal infected with the Av-wt virus showing no pathological changes in the lung (A, original magnification, ×20) but acute tracheitis and inflammation of the submucosal glands (B, original magnification, ×20) associated with viral antigen (C, original magnification, ×40). (D to F) Sections from an animal infected with the Av-mut virus showing only a single focus of alveolitis (E, original magnification, ×20) in an otherwise unremarkable lung (D, original magnification, ×20). No viral antigen distribution in the lung was seen (F, original magnification, ×20).
Wild-type and mutant 1918 HA-expressing influenza virus mouse infection studies.
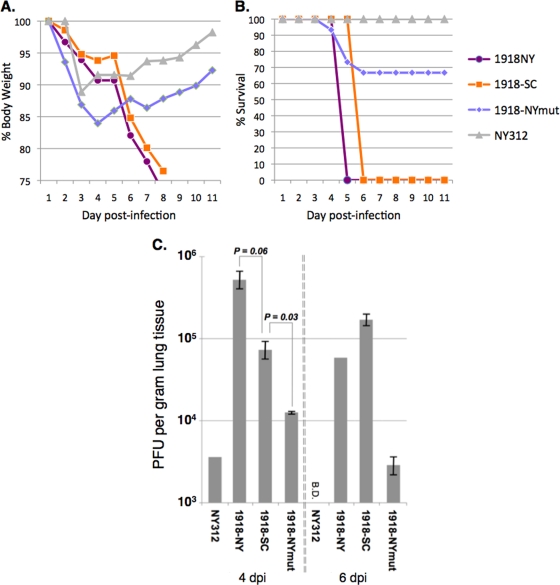
In contrast, viruses expressing 1918 HA with either α2-6 only or mixed α2-3/α2-6 SA specificity caused significant weight loss and were lethal to mice (Fig. 3A and B), produced high viral lung titers of 105 to 106 PFU per gram of lung tissue (Fig. 3C), and caused severe disease pathology. As shown in Table 1, the dose of the 1918-SC virus lethal for 50% of the mice infected (MLD50) was slightly lower (MLD50 = 103.8) than that of the 1918-NY virus (MLD50 = 104.47). To examine whether changing the SA binding specificity of the 1918 HA to α2-3 affected its phenotype in mice, we tested the α2-3-only SA binding 1918-NYmut virus (30, 31). Mice intranasally inoculated with 2 × 105 PFU of the 1918-NYmut virus showed an early weight loss that was more severe than that of mice infected with the Av-wt, Av-mut, or parental NY312 virus and was similar to that of mice infected with the 1918-SC and 1918-NY viruses. Infection with 1918-NYmut was also lethal in approximately 33% of the mice tested (n = 15); however, we were unable to determine an MLD50 of this virus, as we did not have sufficiently high titers from MDCK cell supernatants for an inoculation above 2 × 105 PFU. These results demonstrate that (i) in the first set of experiments, simply changing the SA binding specificity of an avian HA from α2-3 to α2-6 was not sufficient to induce lethal infection and (ii) in the second set of experiments, although 1918 viruses with α2-6 HA binding activity were more virulent, altering 1918 HA binding to uniquely α2-3 did not completely abolish the virulent phenotype in the mouse model.
FIG. 3.
Results of wild-type and mutant 1918 HA-expressing influenza virus infection experiments. (A) Weight loss of mice infected with rescued influenza viruses. Ten- to 12-week-old female BALB/c mice were intranasally inoculated with 2 × 105 PFU of indicated viruses and weighed daily. Only the 1918-SC- and 1918-NY-infected mice had uniform significant weight loss leading to a lethal infection (n = 5 mice per virus per group), while 1918-NYmut-infected animals showed similar early weight loss with significantly lower mortality (n = 15 mice per virus per group). (B) Kaplan-Meier survival curve of 10- to 12-week-old female BALB/c mice intranasally inoculated with 2 × 105 PFU of virus. The 1918-SC and 1918-NY viruses caused uniformly lethal infections typically by 6 dpi, while 33% of the mice infected with the 1918-NYmut virus had lethal outcomes (n = 15). (C) Virus titers in the lungs of infected BALB/c mice (n = 2 or 3) described in PFU per gram of lung tissue as determined by plaque assay (B.D. indicates below the detection threshold). Two-tailed P values were calculated with an unpaired t test.
Pathology and immunohistochemistry studies.
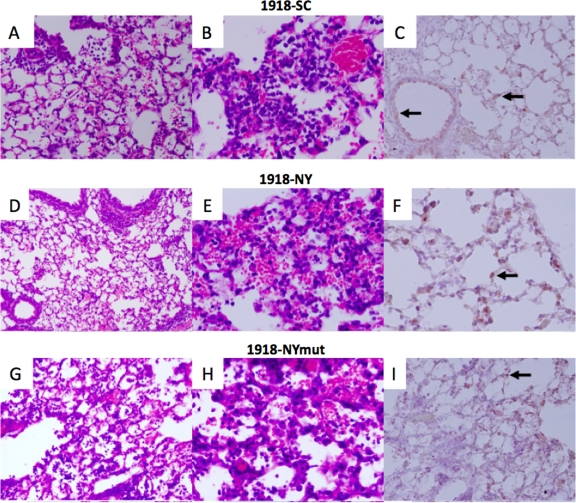
To determine how SA receptor binding specificity affected the lung pathology and cell tropism of these avian and 1918 H1N1 viruses, we compared hematoxylin-and-eosin- and viral antigen-stained lung sections from mice infected with the NY312, Av-wt, Av-mut, 1918-SC, 1918-NY, or 1918-NYmut virus. In contrast to the parental NY312, Av-wt, and Av-mut experiments, lung sections from mice infected with the three 1918 HA, NA constructs showed severe pathology. The lung sections from the 1918-SC- and the 1918-NY-infected mice had moderate-to-marked alveolitis and bronchiolitis with alveolar edema and/or hemorrhage (Fig. 4A, B, D, and E). The inflammatory infiltrate was mixed but contained many neutrophils. Widespread viral antigen was detected in both bronchiolar epithelial cells and alveolar lining cells (Fig. 4C and F). The 1918-NYmut virus-infected mice showed a similar pathology, with moderate alveolitis and bronchiolitis (Fig. 4G and H) that was less extensive than that observed in the 1918-SC- and 1918-NY-infected mouse lung sections. Viral antigen was also detected in alveolar lining cells (Fig. 4I).
FIG. 4.
Pathology and immunohistochemistry of 1918 HA-expressing virus-infected mouse lung tissue. Photomicrographs of hematoxylin-and-eosin-stained tissue sections and immunohistochemically stained sections to detect influenza viral antigen from mice infected with different influenza virus constructs at 6 dpi. Viral antigen is stained red-brown on a hematoxylin-stained background. Arrows show examples of positive cells. (A to C) Sections from an animal infected with the 1918-SC virus. Moderate-to-marked acute alveolitis and bronchiolitis were seen (A, original magnification, ×20; B, original magnification, ×40). Viral antigen was observed in alveolar lining cells and in the epithelium of terminal bronchioles (C, original magnification, ×20). (D to F) Sections from an animal infected with the 1918-NY virus. Moderate-to-marked acute alveolitis and bronchiolitis were seen (D, original magnification, ×20; E, original magnification, ×40). Viral antigen was observed in alveolar lining cells (F, original magnification, ×40). (G to I) Sections from an animal infected with the 1918-NYmut virus. Moderate acute alveolitis and bronchiolitis were seen (G, original magnification, ×20; H, original magnification, ×40). Viral antigen was observed in alveolar lining cells (I, original magnification, ×20).
DISCUSSION
In this study, we have shown that the 1918 HA RBD and associated SA binding specificity are a moderate determinant of murine virulence (as measured by viral pneumonia with marked alveolitis, weight loss, and a lethal outcome) but that additional determinants reside outside of the RBD and cleavage domains of the 1918 HA. We have also shown that mutation of a low-pathogenicity avian H1 subtype HA virus to α2-6 binding does not result in marked weight loss, severe lung pathology, or death. Severe influenza viral pneumonias in humans, particularly those caused by HPAI viruses, are often associated with significant lower respiratory tract infections (14, 15). HPAI viruses such as H5N1 have a strong α2-3 binding specificity (31), and it has been hypothesized that mutations leading to increased α2-6 binding by HPAI viruses would facilitate human-to-human transmission and lead to a new pandemic. However, this may be an oversimplification. Isolates of the 1918 pandemic influenza virus have revealed two cocirculating variant HA RBD sequences, representing α2-6 (e.g., A/South Carolina/1/18; D190, D225) and blended α2-3/α2-6 (e.g., A/New York/1/18; D190, G225) binding specificities (25). The 1918 pandemic influenza virus was thus apparently transmitted and caused severe disease with either α2-3/α2-6 or α2-6 binding activity. This suggests that 1918 HA likely encodes one or more additional unmapped virulence properties outside of the RBD. Efficient human-to-human transmission may also require changes in other viral genes that have not yet been fully elucidated. It is intriguing that some recent H5N1 influenza virus isolates that caused human infections in 2003 and 2004 showed mixed α2-3 and α2-6 binding, but these viruses were not more easily transmissible in humans (43).
The viruses used in this study contained identical internal genes, and their replication in MDCK cells was efficient (titers of 106 to 107 PFU/ml), showing that neither replacement nor mutation of the HA genes blocked infection or replication. However, we observed dramatic differences in mouse virulence and pathogenesis. Given that the 1918 reassortant viruses were isogenic, apart from the surface glycoproteins, these properties can be attributed to the different HA and NA genes (Table 1). Additionally, the 1918 and avian HA genes were isogenic outside single nucleotide changes in the codons of the RBD. The parental NY312 virus showed limited replication in the lung at 4 dpi and caused only slight weight loss with minimal pathological changes. Replacing the parental NY312 virus genes with wild-type avian HA and NA genes slightly increased weight loss but was still nonfatal. Changing avian HA α2-3 binding specificity to α2-6 led to prolonged viral replication of the Av-mut virus in the mouse lung, but with minimal pathogenic changes and a nonlethal outcome that was similar to that obtained with the Av-wt virus.
In contrast, replacement of the HA and NA genes of the parental NY312 virus with 1918 virus HA and NA genes dramatically increased pathogenicity and lethality for mice, confirming previous findings (13, 38). Both the 1918-SC and 1918-NY viruses were uniformly lethal at the highest dose, with significant lung replication that persisted until death and led to severe pathology, especially in the lower respiratory tree. The viral MLD50 and lung pathology observed for the 1918-SC virus were similar to those obtained in previous studies evaluating similar viral constructs (11, 13, 37). The increased pathogenicity of the viruses expressing the HA and NA genes representing the 1918 virus sequences was not solely due to the ability of these viruses to bind α2-6 SA. Mutation of the 1918-NY HA gene (D190, G225) to a completely avian RBD consensus (E190, G225) did not completely attenuate the virus, which still caused lethal infection with bronchiolitis and alveolitis, albeit with less severity than 1918-SC or 1918-NY. Intriguingly, we observed a similar trend of the duration of viral replication in mouse lungs between the avian and 1918 chimeric viruses. Both the Av-wt and 1918-NYmut viruses with α2-3-only binding activity were only detected at 4 dpi but were either undetectable or significantly reduced, respectively, by 6 dpi. In contrast, the Av-mut, 1918-SC, and 1918-NY viruses with α2-6 binding activity persisted in the lungs and were detected at both 4 and 6 dpi. Taken together, these studies revealed that the 1918 HA gene likely contains important determinants outside the RBD that contribute to enhanced virulence in mice. Studies are under way to identify the responsible domains and amino acid changes associated with them.
The experiments described in this report emphasize the complexity of the relationship between SA binding specificity and virulence and pathogenesis in IAV infection and highlight several important unanswered questions. Unfortunately, to date, no detailed systematic surveys of SA distribution in the respiratory tree have been performed with mice. Two limited studies that used lectin binding to determine SA isomeric distribution in the lungs have been performed. Gagneux et al. showed that α2-6 binding lectin Sambuccusnigra agglutinin (SNA) staining was not observed in the tracheas or lung airways of mice (5). Similarly, Ibricevic et al. examined SA distribution in the mouse respiratory tree with both SNA and the α2-3-specific lectin from Maackiaamurensis (MAA) (8). This study showed little SNA binding in the mouse respiratory tree and widely distributed binding of MAA. Both of these studies correlated the absence of SNA binding with the absence of α2-6 SA in mouse lungs. However, both of these studies relied upon lectin binding as a surrogate for α2-6 SA expression. The difficulty with interpreting lectin-based binding experiments is that lectins are highly specific for the terminal linkage and not for the entire glycan. For example, it has been demonstrated that the α2-3 binding lectins MAA1 and MAA2 show differential and exclusive binding to distinct α2-3 SA-containing glycans (19).
In contrast to the specific lectin binding of only the terminal carbohydrate linkages of glycans, two recent studies have shown that influenza virus HA proteins make direct contact with many subterminal carbohydrates in SA-containing glycans that contribute to their 2-3 and 2-6 binding specificity (2, 28). Thus, influenza virus HA proteins bind much more than just the terminal disaccharides of SA-terminating complex glycans. These data show that lectin binding by histochemistry with lectins like SNA and MAA is therefore not a very good surrogate for influenza virus HA binding and cellular tropism. Increasing the complexity of this binding further, Stevens et al., using glycan arrays, showed that the same influenza viral HA proteins show differential binding to a variety of branched and unbranched oligosaccharides with the same terminal disaccharide, whether α2-6 or α2-3 (30). Taken together, these diverse studies have shown a remarkable and growing understanding of the degree of complexity of the expression of SA-containing complex glycans in the respiratory tree and binding of influenza virus HA.
While α2-6 binding by 1918 HA does contribute to virulence, our study raises additional questions about the nature of the non-RBD-defined virulence of the 1918 HA protein. HA proteins from subtype H5 and H7 HPAI viruses, including recent Eurasian H5N1 lineages, possess polybasic amino acid insertional mutations near the HA1/HA2 cleavage site that have been shown to be an important virulence factor. This polybasic region broadens protease specificity and leads to enhanced HA processing and expanded cellular tropism (33). The 1918 HA protein does not possess such a cleavage site mutation and does not lead to replication outside the respiratory tree in mouse models, although it has been reported to have trypsin-independent growth properties in cell culture (37). Our analysis of viral antigen distribution in the lungs of infected mice showed that 1918 HA-expressing viruses were dominantly found in both bronchiolar and alveolar epithelial cells with a distribution that appeared to be independent of SA binding specificity. However, these studies could not rule out subtle differences in SA-mediated cellular tropism, including differences in the infection of type I and II alveolar epithelial cells or macrophages. Studies are under way to address the question of which bronchiolar and alveolar epithelial cells are infected by different 1918 HA-expressing viruses.
A possible mechanism of the virulence of the 1918 HA could be tropism for immune cells such as alveolar macrophages and dendritic cells, which might lead to inhibition of protective immune responses. Recent work showed that the 1918 PB1-F2 protein sensitized immune cells to proapoptotic stimuli (3). Thus, if the 1918 HA protein increases the infection of alveolar macrophages, effects of the 1918 PB1-F2 protein could lead to suppression of early protective immune responses that may help explain the virulence of the fully reconstructed 1918 influenza virus in mice and macaques (11, 12, 37).
The results presented in this report demonstrate that while the SA binding specificity of the 1918 HA protein plays an important role in pathogenesis in mice, additional virulence determinants must likely reside outside of the RBD. Given the differences in reported primary isolate 1918 RBD HA sequences, it will be of interest to examine the viral antigen distribution in autopsy tissue sections from human 1918 influenza cases with known differences in HA RBD amino acid sequences to determine if the pattern of infection in human alveolar lining cells is affected by changes in the HA RBD sequence and SA binding specificity. Further studies are required to identify these virulence determinants and to understand their potential roles in affecting host range, cellular tropism, replication, transmission, and pathogenesis.
Acknowledgments
We thank David Morens and Brian Murphy for helpful discussions.
This work was supported by the Intramural Research Program of the NIH and the NIAID.
Footnotes
Published ahead of print on 11 February 2009.
REFERENCES
- 1.Baum, L. G., and J. C. Paulson. 1990. Sialyloligosaccharides of the respiratory epithelium in the selection of human influenza virus receptor specificity. Acta Histochem. Suppl. 4035-38. [PubMed] [Google Scholar]
- 2.Chandrasekaran, A., A. Srinivasan, R. Raman, K. Viswanathan, S. Raguram, T. M. Tumpey, V. Sasisekharan, and R. Sasisekharan. 2008. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nat. Biotechnol. 26107-113. [DOI] [PubMed] [Google Scholar]
- 3.Conenello, G. M., D. Zamarin, L. A. Perrone, T. Tumpey, and P. Palese. 2007. A single mutation in the PB1-F2 of H5N1 (HK/97) and 1918 influenza A viruses contributes to increased virulence. PLoS Pathog. 31414-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fodor, E., L. Devenish, O. G. Engelhardt, P. Palese, G. G. Brownlee, and A. Garcia-Sastre. 1999. Rescue of influenza A virus from recombinant DNA. J. Virol. 739679-9682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gagneux, P., M. Cheriyan, N. Hurtado-Ziola, E. C. van der Linden, D. Anderson, H. McClure, A. Varki, and N. M. Varki. 2003. Human-specific regulation of alpha 2-6-linked sialic acids. J. Biol. Chem. 27848245-48250. [DOI] [PubMed] [Google Scholar]
- 6.Guo, C. T., N. Takahashi, H. Yagi, K. Kato, T. Takahashi, S. Q. Yi, Y. Chen, T. Ito, K. Otsuki, H. Kida, Y. Kawaoka, K. I. Hidari, D. Miyamoto, T. Suzuki, and Y. Suzuki. 2007. The quail and chicken intestine have sialyl-galactose sugar chains responsible for the binding of influenza A viruses to human type receptors. Glycobiology 17713-724. [DOI] [PubMed] [Google Scholar]
- 7.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 1462275-2289. [DOI] [PubMed] [Google Scholar]
- 8.Ibricevic, A., A. Pekosz, M. J. Walter, C. Newby, J. T. Battaile, E. G. Brown, M. J. Holtzman, and S. L. Brody. 2006. Influenza virus receptor specificity and cell tropism in mouse and human airway epithelial cells. J. Virol. 807469-7480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson, N. P., and J. Mueller. 2002. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull. Hist. Med. 76105-115. [DOI] [PubMed] [Google Scholar]
- 10.Kash, J. C., C. F. Basler, A. Garcia-Sastre, V. Carter, R. Billharz, D. E. Swayne, R. M. Przygodzki, J. K. Taubenberger, M. G. Katze, and T. M. Tumpey. 2004. Global host immune response: pathogenesis and transcriptional profiling of type A influenza viruses expressing the hemagglutinin and neuraminidase genes from the 1918 pandemic virus. J. Virol. 789499-9511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kash, J. C., T. M. Tumpey, S. C. Proll, V. Carter, O. Perwitasari, M. J. Thomas, C. F. Basler, P. Palese, J. K. Taubenberger, A. Garcia-Sastre, D. E. Swayne, and M. G. Katze. 2006. Genomic analysis of increased host immune and cell death responses induced by 1918 influenza virus. Nature 443578-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobasa, D., S. M. Jones, K. Shinya, J. C. Kash, J. Copps, H. Ebihara, Y. Hatta, J. H. Kim, P. Halfmann, M. Hatta, F. Feldmann, J. B. Alimonti, L. Fernando, Y. Li, M. G. Katze, H. Feldmann, and Y. Kawaoka. 2007. Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature 445319-323. [DOI] [PubMed] [Google Scholar]
- 13.Kobasa, D., A. Takada, K. Shinya, M. Hatta, P. Halfmann, S. Theriault, H. Suzuki, H. Nishimura, K. Mitamura, N. Sugaya, T. Usui, T. Murata, Y. Maeda, S. Watanabe, M. Suresh, T. Suzuki, Y. Suzuki, H. Feldmann, and Y. Kawaoka. 2004. Enhanced virulence of influenza A viruses with the haemagglutinin of the 1918 pandemic virus. Nature 431703-707. [DOI] [PubMed] [Google Scholar]
- 14.Korteweg, C., and J. Gu. 2008. Pathology, molecular biology, and pathogenesis of avian influenza A (H5N1) infection in humans. Am. J. Pathol. 1721155-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuiken, T., and J. K. Taubenberger. 2008. The pathology of human influenza revisited. Vaccine 26(Suppl. 4)D59-D66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matrosovich, M., A. Tuzikov, N. Bovin, A. Gambaryan, A. Klimov, M. R. Castrucci, I. Donatelli, and Y. Kawaoka. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 748502-8512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nelson, M. I., C. Viboud, L. Simonsen, R. T. Bennett, S. B. Griesemer, K. St George, J. Taylor, D. J. Spiro, N. A. Sengamalay, E. Ghedin, J. K. Taubenberger, and E. C. Holmes. 2008. Multiple reassortment events in the evolutionary history of H1N1 influenza A virus since 1918. PLoS Pathog 4e1000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neumann, G., T. Watanabe, H. Ito, S. Watanabe, H. Goto, P. Gao, M. Hughes, D. R. Perez, R. Donis, E. Hoffmann, G. Hobom, and Y. Kawaoka. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. USA 969345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicholls, J. M., R. W. Chan, R. J. Russell, G. M. Air, and J. S. Peiris. 2008. Evolving complexities of influenza virus and its receptors. Trends Microbiol. 16149-157. [DOI] [PubMed] [Google Scholar]
- 20.Pappas, C., P. V. Aguilar, C. F. Basler, A. Solorzano, H. Zeng, L. A. Perrone, P. Palese, A. Garcia-Sastre, J. M. Katz, and T. M. Tumpey. 2008. Single gene reassortants identify a critical role for PB1, HA, and NA in the high virulence of the 1918 pandemic influenza virus. Proc. Natl. Acad. Sci. USA 1053064-3069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peiris, J. S., W. C. Yu, C. W. Leung, C. Y. Cheung, W. F. Ng, J. M. Nicholls, T. K. Ng, K. H. Chan, S. T. Lai, W. L. Lim, K. Y. Yuen, and Y. Guan. 2004. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet 363617-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rabadan, R., A. J. Levine, and H. Robins. 2006. Comparison of avian and human influenza A viruses reveals a mutational bias on the viral genomes. J. Virol. 8011887-11891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27493-497. [Google Scholar]
- 24.Reid, A. H., T. G. Fanning, J. V. Hultin, and J. K. Taubenberger. 1999. Origin and evolution of the 1918 “Spanish” influenza virus hemagglutinin gene. Proc. Natl. Acad. Sci. USA 961651-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reid, A. H., T. A. Janczewski, R. M. Lourens, A. J. Elliot, R. S. Daniels, C. L. Berry, J. S. Oxford, and J. K. Taubenberger. 2003. 1918 influenza pandemic caused by highly conserved viruses with two receptor-binding variants. Emerg. Infect. Dis. 91249-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rogers, G. N., and J. C. Paulson. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127361-373. [DOI] [PubMed] [Google Scholar]
- 27.Shinya, K., M. Ebina, S. Yamada, M. Ono, N. Kasai, and Y. Kawaoka. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440435-436. [DOI] [PubMed] [Google Scholar]
- 28.Srinivasan, A., K. Viswanathan, R. Raman, A. Chandrasekaran, S. Raguram, T. M. Tumpey, V. Sasisekharan, and R. Sasisekharan. 2008. Quantitative biochemical rationale for differences in transmissibility of 1918 pandemic influenza A viruses. Proc. Natl. Acad. Sci. USA 1052800-2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steinhauer, D. A. 1999. Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology 2581-20. [DOI] [PubMed] [Google Scholar]
- 30.Stevens, J., O. Blixt, L. Glaser, J. K. Taubenberger, P. Palese, J. C. Paulson, and I. A. Wilson. 2006. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J. Mol. Biol. 3551143-1155. [DOI] [PubMed] [Google Scholar]
- 31.Stevens, J., O. Blixt, T. M. Tumpey, J. K. Taubenberger, J. C. Paulson, and I. A. Wilson. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312404-410. [DOI] [PubMed] [Google Scholar]
- 32.Suzuki, Y. 2005. Sialobiology of influenza: molecular mechanism of host range variation of influenza viruses. Biol. Pharm. Bull. 28399-408. [DOI] [PubMed] [Google Scholar]
- 33.Swayne, D. E. 2007. Understanding the complex pathobiology of high pathogenicity avian influenza viruses in birds. Avian Dis. 51242-249. [DOI] [PubMed] [Google Scholar]
- 34.Taubenberger, J. K., and D. M. Morens. 2006. 1918 Influenza: the mother of all pandemics. Emerg. Infect. Dis. 1215-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taubenberger, J. K., A. H. Reid, A. E. Krafft, K. E. Bijwaard, and T. G. Fanning. 1997. Initial genetic characterization of the 1918 “Spanish” influenza virus. Science 2751793-1796. [DOI] [PubMed] [Google Scholar]
- 36.Taubenberger, J. K., A. H. Reid, R. M. Lourens, R. Wang, G. Jin, and T. G. Fanning. 2005. Characterization of the 1918 influenza virus polymerase genes. Nature 437889-893. [DOI] [PubMed] [Google Scholar]
- 37.Tumpey, T. M., C. F. Basler, P. V. Aguilar, H. Zeng, A. Solorzano, D. E. Swayne, N. J. Cox, J. M. Katz, J. K. Taubenberger, P. Palese, and A. Garcia-Sastre. 2005. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 31077-80. [DOI] [PubMed] [Google Scholar]
- 38.Tumpey, T. M., A. Garcia-Sastre, A. Mikulasova, J. K. Taubenberger, D. E. Swayne, P. Palese, and C. F. Basler. 2002. Existing antivirals are effective against influenza viruses with genes from the 1918 pandemic virus. Proc. Natl. Acad. Sci. USA 9913849-13854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tumpey, T. M., A. Garcia-Sastre, J. K. Taubenberger, P. Palese, D. E. Swayne, and C. F. Basler. 2004. Pathogenicity and immunogenicity of influenza viruses with genes from the 1918 pandemic virus. Proc. Natl. Acad. Sci. USA 1013166-3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tumpey, T. M., T. R. Maines, N. Van Hoeven, L. Glaser, A. Solorzano, C. Pappas, N. J. Cox, D. E. Swayne, P. Palese, J. M. Katz, and A. Garcia-Sastre. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315655-659. [DOI] [PubMed] [Google Scholar]
- 41.Wan, H., and D. R. Perez. 2006. Quail carry sialic acid receptors compatible with binding of avian and human influenza viruses. Virology 346278-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webster, R. G., and E. A. Govorkova. 2006. H5N1 influenza—continuing evolution and spread. N. Engl. J. Med. 3552174-2177. [DOI] [PubMed] [Google Scholar]
- 43.Yamada, S., Y. Suzuki, T. Suzuki, M. Q. Le, C. A. Nidom, Y. Sakai-Tagawa, Y. Muramoto, M. Ito, M. Kiso, T. Horimoto, K. Shinya, T. Sawada, M. Kiso, T. Usui, T. Murata, Y. Lin, A. Hay, L. F. Haire, D. J. Stevens, R. J. Russell, S. J. Gamblin, J. J. Skehel, and Y. Kawaoka. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444378-382. [DOI] [PubMed] [Google Scholar]